Abstract
Teaching Evidence Based Medicine (EBM) helps medical students to develop their decision making skills based on current best evidence, especially when it is taught in a clinical context. Few medical schools integrate Evidence Based Medicine into undergraduate curriculum, and those who do so, do it at the academic years only as a standalone (classroom) teaching but not at the clinical years. The College of Medicine at King Saud bin Abdulaziz University for Health Sciences was established in January 2004. The college adopted a four-year Problem Based Learning web-based curriculum. The objective of this paper is to present our experience in the integration of the EBM in the clinical phase of the medical curriculum. We teach EBM in 3 steps: first step is teaching EBM concepts and principles, second is teaching the appraisal and search skills, and the last step is teaching it in clinical rotations. Teaching EBM at clinical years consists of 4 student-centered tutorials. In conclusion, EBM may be taught in a systematic, patient centered approach at clinical rounds. This paper could serve as a model of Evidence Based Medicine integration into the clinical phase of a medical curriculum.
Keywords: Clinical years, evidence based medicine, medical curriculum, medical education
INTRODUCTION
Evidence-based medicine (EBM) is a tool which aims to increase the use of high quality clinical research in clinical decision making. There is general consensus in the academic community that evidence based medicine (EBM) teaching is essential.[1] Teaching EBM becomes popular, including the incorporation of the current best evidence from research into clinical decision making. The major characteristics for teaching EBM to undergraduate medical students includes: Clinically integrated teaching is more effective than stand-alone (classroom) teaching, long-term teaching is more effective than short-term teaching, EBM should be clearly incorporated in the curriculum as part of the clinical training,[1–4] secondary EBM resources should be available, easily accessible at the point of care by medical students,[5,6] and availability of clinicians and teachers who implement EBM in their day to day practice and who are considered as models for students.[7,8] Search and critical appraisal skills can be taught early in the undergraduate medical curriculum, which proved to positively change their perceptions, knowledge, and reading habits. Students showed deterioration of their knowledge and skills over time. This is evident by the finding that their test scores were higher immediately after the course, than when tested three years later, which indicates that EBM teaching should be re-enforced as students progressed in their education.[9]
Green's literature review of approaches to teaching EBM revealed few important modalities to teachers of EBM:[10] (1) Small-group teaching which is learner-centered format (examples, small group appraisal discussion, morning meetings, ward round and EBM journal club), (2) One-on-one student-faculty opportunities, like in the out-patient clinics, task assignment and EBM workbook, (3) Immediate clinical relevance by finding any opportunity at different setting to discuss, explain, and challenge students with EBM interpretation for example relative risk, odds ratio, number needed to treat, sensitivity, specificity, likelihood ratio, how to search the secondary EBM resources and applicability of the results to a specific patient, and (4) Role modeling of EBM, when the trainer applies EBHP on his daily practice student will consider it the norm and they will follow his steps.
To our knowledge King Saud bin Abdulaziz University for Health Science (KSAU-HS) is the only medical institute in Saudi Arabia and the Gulf region to integrate EBM into the clinical rounds of medical curriculum.
We have comprehensively described our experience of integrating EBM in phase 2 (the academic years) in a separate paper[11] . The aim of this paper is to describe the integration of EBM into phase 3 (the clinical years) in a PBL medical curriculum at KSAU-HS, Riyadh, the Kingdom of Saudi Arabia.
Background
The College of Medicine (COM) at King Saud Bin Abdulaziz University for Health Sciences (KSAU-HS), Riyadh, and the KSA has adopted four-years problem-based (PBL) curriculum, the curriculum is preceded by phase 1 that could be either a two-year pre-professional program for high school student's entry or one academic semester to prepare graduate students for the curriculum. This is followed by a two-year phase 2 that integrate basic medical sciences with clinical sciences in a system based model. Students will finally pass through phase 3 which is discipline-based with the continuation of PBL model throughout two years. Medical students will spend their clinical rotations at King Abdulaziz Medical City-Riyadh, KSA, which is a tertiary-care hospital that is affiliated with the University for both Undergraduate and Postgraduate teaching and training. EBM in phase 3 will based on the clinical cases from the hospital and mostly taught by the academic staff there.
The first year of phase 2 of the curriculum includes theoretical teaching of EBM that includes: introduction to EBM, study designs, basic statistics and literature search for evidence. While the second year of phase 2, includes teaching the concept of appraisal of articles about therapy, diagnosis, prognosis, systematic reviews and guidelines. Each topic is discussed in 2 ways, a lecture and a tutorial. The lecture lasts for 45 minutes and 15 minutes discussion, while the tutorial lasts for 90 minutes.[12]
EBM in phase 3 (Clinical phase)
In the third and fourth years, medical students will rotate in discipline-based blocks with clinical attachments in different clinical departments related to the discipline (internal medicine, pediatrics, obstetrics and gynecology, surgery, family and community medicine). Within each clinical department, medical students join clinical teams which may include: A consultant, associate consultants, assistant consultants, fellows, residents, interns and medical students; consultants and associate consultants are the core members of the team. The unique aspect about phase 3 that it continues to include web-based and patient-based PBL sessions, continuation of the longitudinal themes of personal professional development and community-doctor theme, the implementation of innovative work-based assessment[13,14] which is closely evaluating the knowledge and skills of students, and the introduction of e-portfolio,[11] there is evidence of an improvement in knowledge and understanding, increased self-awareness and engagement in reflection and improved student-tutor relationships as the main benefits of portfolio use.
Another unique aspect is the adoption of PEARLS model (Presentation of Evidence Abstracted from the Research Literature for Solution),[15] a systematic teaching program that aims at integration of Evidence-Based Practice into the Clinical Rotations. Provision of a simple and efficient model for the implementation and integration of evidence into clinical practice by using a structured model that applies the principles of EBM to solve real clinical problems and to gain practical experience of short presentations and prompt specific feedback.
The following sections will describe our experience in integrating PEARLS model in the clinical phase [Table 1].
Table 1.
Evidence-based medicine sessions at third and fourth clinical years
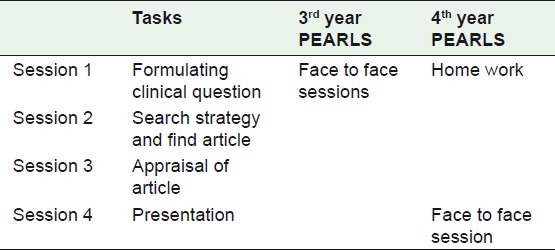
Integration of EBM in the third year clinical rotation
Tables 2 and 3 show the objective of EBM in phase 3 of the curriculum. Students attend 4 PEARLS tutorials for 8-10 weeks, each tutorial spans over 90 minutes, and is divided into segments according to the number of students [Table 1] For example: a group consisting of 6 students where each student provided with a 10-minutes segment. During the allocated 10 minutes, the student describes the stage he is at, and asks for assistance from the group, as well as the tutor. The same process is repeated for each student. Provision of a simple and efficient model for the implementation and integration of evidence into clinical practice by using a structured model that applies the principles of EBM to solve real clinical problems and to gain practical experience of short presentations and prompt specific feedback. It is usually preferable to have the same tutor facilitating all sessions.
Table 2.
Objective of evidence-based medicine in the clinical years of medical curricula
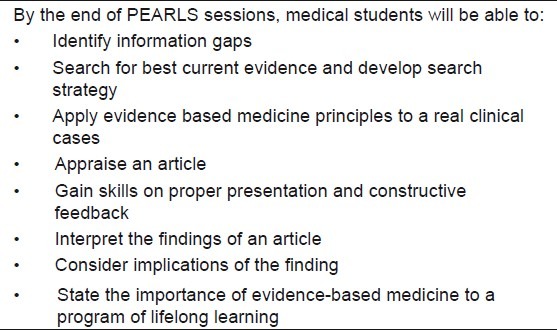
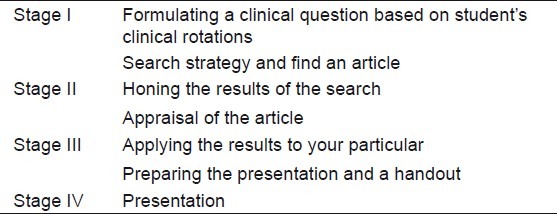
Table 3.
Integration of evidence-based medicine into third clinical year
Pre-sessions preparation
When the curriculum (block book) of the third year is distributed to medical students, a full description of EBM sessions is included and discussed with students at the start of the block. Two weeks prior to EBM sessions, a one page summarizing the whole process is posted to students. Role of students: While they were at the clinical rounds, they select one medical problem with uncertainty, they were asked to transform the uncertainty into a clinical question, develop search strategy, find the best article, appraise it, prepare the presentation and conduct the presentation.
Session 1: Medical students prepare clinical question as home work, and attend the first session with his question prepared. Each student is given 7-10 minutes to present his clinical question [Table 1]. The question should be a real clinical case that was encountered during clinical rotation. The objective of this session is to teach the student how to transform a clinical uncertainty to a clinical question. It will start with formulation of clinical focused question based on the clinical practice: Students formulate clinical focused question which was raised during the clinical interaction with medical team or patients, not a hypothetical one (example will follow). It is followed by presenting the on PICO format (P. stands for patients and their problems intervention: This may be a new drug, procedure, education programs, C. Comparison, control: Placebo (inert material), traditional drug, old procedure or educational programs, O. Outcome: Patient oriented outcome (POEM: Morbidity, mortality and the quality of life), and Process: Each student comes up with his question, presented it for peer review and faculty staff). The question is presented to the group, tutor discusses and gives his/her feedback and the peer discussion occurs as well. As homework, each student is asked to write up a search strategy and do electronic search to retrieve a relevant article. The search strategy contains: the key words, study design, the databases to be searched.
Session 2: Each student presents his search strategy, the selected article (s), and the reasons for selecting that particular article. The criteria for selecting the article are: first, to address the clinical question, second, to be recent (i.e. published within the last two years), third, to contain fewer flaws, fourth, to be randomized controlled trial or systematic review for therapy, cross-sectional or prospective for diagnosis and prospective or retrospective for prognosis.
Session 3: Students discuss their appraised articles with the faculty tutor where they discuss relevance, validity, results and applicability. By relevance, students discuss three points: is the topic common to your practice? Is the outcome patient oriented (POEM)? And the result of the study if significant will change the practice. For validity, results and applicability students apply the critical appraisal worksheets.[15] Students discuss the strengths and weaknesses of the article, and the resolution of the clinical scenario.
Session 4: Power point presentation is conducted by every medical student for 7 minutes; another 7 minutes are reserved for peer and faculty discussion. Other faculty members are invited to assess the student's project. Students present in sequence: the question, background (what is known already about the topic), search strategy, appraisal of the selected article (Validity and results), strengths and weaknesses and resolution of the case. There is an assessment sheet completed by the faculty members.
Role of tutor: An expertise in evidence based medicine faculty member run PEARLS sessions. He meets with the students, discuss with every student his task, propose corrections and assess the students’ performance.
Assessment
Assessment of students has many forms; first is the work-based format, it happens during tutorials by tutors and peers with feedback. The formative assessment occurs at the last session which is the presentation; there is a special check list which is completed by EBM tutor and content tutor who attended the presentation.
A more extended assessment need to be developed, for example a quantitative assessment to compare our students with others in understanding EBM concepts and principles, another assessment is the qualitative assessment by observing the way our students make their decision in their future career (see an example of the PEARLS session in the third year in the Appendix).
Integration of EBM into the fourth year clinical rotation
The main EBM objective for the fourth year is for medical students to apply the five steps of EBM independently as adult learning; during this year's clinical rotation, students developed the 5 skills of practicing EBM. A modified PEARLS is applied at this year. Modified PEARLS for 4th year depends on home-work and one presentation session. Each medical student comes up with a question based on his clinical rotation, converts it to PICO, develops a search strategy, retrieves and selects an article that answers the question, and appraises that article. Stages 1 to 3 which were described above in the third year's PEARLS were done independently by students. They have one session only for presentation and assessment [Table 1].
DISCUSSION
This paper is the second of the integration of EBM into undergraduate curriculum series. The first paper was addressing the integration of EBM into the academic years, which was published at Medical Education Online 2009.[11]
King Saud Abdelaziz University for Health Science (KSAU) is teaching EBM to medical students for the last 7 years, the EBM curriculum is fully integrated into the undergraduate curriculum. This is the first experience of an Arab Medical school which the authors would like to disseminate this experience to other Arab medical schools. Appropriate clinical decisions require health care providers to select the best available relevant and valid evidence and to acquire the skills to do so.[16] Teaching EBM in classes as a standalone teaching is proved to be ineffective in changing student's attitude and practice, while teaching EBM in clinical settings where patients’ problems were integrated in EBM teaching is proven to be effective, there is a hierarchy of teaching and learning activities in terms of their educational effectiveness: level 1: Interactive and clinically integrated activities, level 2(a): interactive but classroom based activities, level 2(b): didactic but clinically integrated activities, and level 3, didactic, classroom or standalone teaching,[16–20] EBM curriculum must be extended beyond the academic years to be included at the clinical years rotations, so that students gain skills of searching, assessing, applying and communicating new knowledge in clinical decision-making.[16,19,21] Al-Omari et al, and Juchi et al. found that 5% of physicians used EBM resources at their daily practice,[19,21] West at el found that the extended EBM education curriculum is shown to be effective in promoting its implementation.[21,22] The advantages of PEARLS are many, first, it is actively involving medical students in a real day to day practice, second, it educates students EBM practice in a multifaceted way, third, it translates EBM theory into practice and finally it gradually builds up the EBM skills so that medical student can practice EBM independently.[4] The key massages of the paper are, first, evidence Based Medicine can be integrated into the clinical years of medical schools; second, the real clinical question can be used to apply the 5 steps of EBM; third, medical students learn the critical thinking process; fourth, they learn and practice various skills mainly formulating focused clinical questions, developing search strategy and finding the suitable article, critically appraise published articles including picking up biases, assessing the internal validity, and interpreting the results and assessing the external validity. One of the important limitations of the study is that authors didn′t conduct a research to measure the student's decision making skills compared to other students. This paper presents the 8-year experience of a Saudi medical school experience of integrating EBM into clinical years, which may stimulate other medical schools to do the same. The next step that must be done is the evaluation of the effectiveness of PEARLS in terms of increasing knowledge, skills behavior, and satisfaction of students.
CONCLUSION
We presented King Saud bin Abdulaziz University for Health Sciences experience of a systematic, patient-centered approach of integrating EBM into clinical years at a problem based learning (PBL), medical curriculum.
APPENDIX
Example of the PEARLS session in the third year
A third year medical student doing the clinical rotation at medicine block, neurology rotation presents the following clinical scenario:
“A 41-year-old female was presented to our emergency department with twisted face and difficulty with left eye closure for 12 hours. No gait disturbances, weakness, numbness, tingling and taste disturbances were noted.”
In the first session the question was presented by a student and his colleagues were allowed to discuss issues related to it. The diagnosis was established as Bell's palsy (Lower motor neuron lesion of cranial nerve IIV). The question raised was about treatment, “would this patient improve faster if antiviral (acyclovir) was added to steroids?” PICO was formulated, P: Adult patient with Bell's palsy (lower motor neuron lesion of facial nerve), I: Steroids and acyclovir, C: Steroids alone, O: Complete recovery. In the second session student presents the search strategy: The key words used were: Bell′s, facial, palsy, steroids, prednisolone, acyclovir, and antiviral. The databases searched were:
Cochrane library, PubMed, and Clinical evidence. A student retrieved many studies but selected the following one (Early treatment with prednisolone or acyclovir in Bell's palsy). [14] The objective of this randomized controlled trial was to compare the effectiveness of steroid plus acyclovir versus steroid alone and steroid versus placebo. Patients were randomly assigned to receive prednisolone, acyclovir, both agents, or placebo for 10 days. The study outcomes were recovery of facial function, quality of life, appearance, and pain.
The third session, the students presented the appraisal of the article (validity, results and applicably). In validity he discussed the five important points, randomization, concealment, blindness, drop out and intention to treat analysis. In results, he discussed the number needed to treat and relative risk reduction. In applicability he discussed the availability, cost and side effect of acyclovir, the patient in the scenario, was he similar to patients in the study, then he discussed the patient's preference and finally he discussed the beneficial benefits versus harms. The fourth session: In presence of students, EBM and a neurologist tutors, student presented his project that summarized the three previous stages in 7 minutes in addition to the background of the topic and the resolution of the clinical question. The student concluded that the study is robust, early treatment with prednisolone significantly improves the chances of complete recovery at 3 and 9 months. There is no evidence of a benefit of acyclovir given alone or in combination with prednisolone. The formative evaluation of student presentation came from 3 parties: Peer review: At the end of the presentation, other students interact and ask the presenter about certain issues related to presentation. The neurologist: Who asks questions related to the topic itself and applicability? The EBM tutor: ask questions related to validity and results. Formal student assessment: Assessment of student presentation includes assessment of all steps of practicing EBM and is completed by both tutors which constitute 5% of the block marks.
Footnotes
Source of Support: Authors acknowledge the support of King Saud Abdelaziz University for Health services
Conflict of Interest: Authors have no conflict of interest
REFERENCES
- 1.Radack KL, Valanis B. Teaching critical appraisal and application of medical literature to clinical problem-solving. J Med Educ. 1986;61:329–31. doi: 10.1097/00001888-198604000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Wadland WC, Barry HC, Farquhar L, Holzman C, White A. Training medical students in evidence-based medicine: A community campus approach. Fam Med. 1999;31:703–8. [PubMed] [Google Scholar]
- 3.Ghali WA, Saitz R, Eskew AH, Gupta M, Quan H, Hershman WY. Successful teaching in evidence-based medicine. Med Educ. 2000;34:18–22. doi: 10.1046/j.1365-2923.2000.00402.x. [DOI] [PubMed] [Google Scholar]
- 4.Atiya AS. Teaching of evidence-based medicine to medical undergraduates. Med J Malaysia. 2002;57(Suppl E):105–8. [PubMed] [Google Scholar]
- 5.Green ML, Ruff TR. Why do residents fail to answer their clinical questions. A qualitative study of barriers to practicing evidence-based medicine? Acad Med. 2005;80:176–82. doi: 10.1097/00001888-200502000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Shuval K, Shachak A, Linn S, Brezis M, Feder-Bubis P, Reis S. The impact of an evidence-based medicine educational intervention on primary care physicians: A qualitative study. J Gen Intern Med. 2007;22:327–31. doi: 10.1007/s11606-006-0055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Isaac CA, Franceschi A. EBM: Evidence to practice and practice to evidence. J Eval Clin Pract. 2008;14:656–9. doi: 10.1111/j.1365-2753.2008.01043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tracy CS, Dantas GC, Moineddin R, Upshur RE. Contextual factors in clinical decision making: National survey of Canadian family physicians. Can Fam Physician. 2005;51:1106–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Riegelman RK. Effects of teaching first-year medical students skills to read medical literature. J Med Educ. 1986;61:454–60. doi: 10.1097/00001888-198606000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Green ML, Ellis PJ. Impact of an evidence-based medicine curriculum based on adult learning theory. J Gen Intern Med. 1997;12:742–50. doi: 10.1046/j.1525-1497.1997.07159.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tamim HM, Ferwana M, Al Banyan E, Al Alwan I, Hajeer AH. Integration of evidence based medicine into a medical curriculum. Med Educ Online. 2009;14:15. doi: 10.3885/meo.2009.F0000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilic D, Tepper K, Misso M. Teaching evidence based medicine literature searching skills to medical students during the clinical years - a protocol for a randomised controlled trial. BMC Med Educ. 2011;11:49. doi: 10.1186/1472-6920-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wanvarie S, Sathapatayavongs B, Sirinavin S, Ingsathit A, Ungkanont A, Sirinan C. Evidence-based medicine in clinical curriculum. Ann Acad Med Singapore. 2006;35:615–8. [PubMed] [Google Scholar]
- 14.Ismach RB. Teaching evidence-based medicine to medical students. Acad Emerg Med. 2004;11:e6–10. doi: 10.1197/j.aem.2004.08.037. [DOI] [PubMed] [Google Scholar]
- 15.Stockler MR, March L, Lindley RI, Mellis C. Students’ PEARLS: Successfully incorporating evidence-based medicine in medical students’ clinical attachments. Evid Based Med. 2009;14:98–9. doi: 10.1136/ebm.14.4.98-a. [DOI] [PubMed] [Google Scholar]
- 16.Coomarasamy A, Khan KS. What is the evidence that postgraduate teaching in evidence based medicine changes anything. A systematic review? BMJ. 2004;329:1017. doi: 10.1136/bmj.329.7473.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akl EA, Izuchukwu IS, El-Dika S, Fritsche L, Kunz R, Schunemann HJ. Integrating an evidence-based medicine rotation into an internal medicine residency program. Acad Med. 2004;79:897–904. doi: 10.1097/00001888-200409000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Al Omari M, Khader Y, Jadallah K, Dauod AS, Al-Shdifat AA, Khasawneh NM. Evidence-based medicine among hospital doctors in Jordan: Awareness, attitude and practice. J Eval Clin Pract. 2009;15:1137–41. doi: 10.1111/j.1365-2753.2009.01260.x. [DOI] [PubMed] [Google Scholar]
- 19.Alper BS, Vinson DC. Experiential curriculum improves medical students’ ability to answer clinical questions using the internet. Fam Med. 2005;37:565–9. [PubMed] [Google Scholar]
- 20.Juche A, Kunz R, Willich SN, Bruggenjurgen B. The implementation of evidence-based medicine in general practice-acceptance and use of external information services. Z Arztl Fortbild Qualitatssich. 2006;100:383–7. [PubMed] [Google Scholar]
- 21.West CP, Jaeger TM, McDonald FS. Extended evaluation of a longitudinal medical school evidence-based medicine curriculum. J Gen Intern Med. 2011;26:611–5. doi: 10.1007/s11606-011-1642-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.West CP, McDonald FS. Evaluation of a longitudinal medical school evidence-based medicine curriculum: A pilot study. J Gen Intern Med. 2008;23:1057–9. doi: 10.1007/s11606-008-0625-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


