Abstract
Context:
Physical activity of moderate intensity for 30 minutes a day, on most days substantially reduces the risk of many chronic diseases.
Aim:
To assess the effect of regular physical activity on blood pressure and blood sugar levels in a rural Indian community
Settings and Design:
This community-based study was carried out in Periakattupalayam and Rangareddipalayam in south India, with 485 subjects, aged 20 to 49 years.
Materials and Methods:
The study was done in five phases: Awareness campaign, baseline assessment of participants, intervention phase (10 weeks), interim, and final assessment. Physical activity of moderate intensity (brisk walking for 30 minutes on four days / week) was promoted by forming 30 small walking groups, in a home-based setting, with professional supervision. Village leaders and Self-Help Group members were the resource people for the promotion of physical activity.
Statistical Analysis:
Analysis was done by using paired ‘t’ test; the ‘Intention-to-Treat’ approach was utilized for the interpretation of the findings of the study.
Results:
Of the 485 subjects, 265 (54.6%) complied with walking on more than four days / week, while 156 (32.2%) walked on one to four days / week, and 64 (13.2%) dropped out during the intervention period. This study has shown that a 10-week intervention to promote physical activity was effective in significantly decreasing the population's BP by 1.56 / 0.74 mm Hg, fasting blood sugar levels by 2.82 mg%, body weight by 0.17 kg, and BMI by 0.06 kg / m2.
Conclusions:
This study has proved the functional feasibility of enabling people to undertake physical activity in a rural Indian community, and the effectiveness of using physical activity, to significantly reduce the population's mean BP and blood sugar levels.
Keywords: Blood pressure, chronic diseases, community intervention, physical activity
INTRODUCTION
An inactive lifestyle accounts for 3.3% of all deaths and 19 million Disability Adjusted Life Years (DALYs) worldwide.[1] Physical inactivity accounts for more than one-fifth of Coronary Heart Diseases (CHD) and has been identified as the fourth major modifiable risk factor of CHD.[2] It carries an increased risk of 1.2 to 2.89 times for Hypertension and Stroke, 1.05 to 2.63 for CHD, and 1.08 to 2.63 for Diabetes.[3] The World Health Assembly (2000) affirmed physical inactivity as a key risk factor, and the Global Strategy on Diet, Physical Activity, and Health (DPAS) was adopted in 2004.[4] Levels of inactivity are high in virtually all developed and developing countries. At least 60% of the world's population fail to complete the recommended amount of physical activity required to induce health benefits. The biological mechanisms responsible for the beneficial effects of physical activity are the lowering of BP, elevation in high density lipoprotein levels, increased insulin sensitivity, improved endothelial function, and reduced atherogenic cytokine production.[5] Worldwide, several public health recommendations have been put forward, based on the available evidence of health benefits of physical activity. The World Health Organization recommends at least 30 to 45 minutes of regular, moderate intensity physical activity on most days of the week for the prevention of hypertension, Cardiovascular Diseases (CVD), and Diabetes, respectively.[6]
The rise of Non-Communicable Diseases (NCDs) in developing countries is driven by increasing sedentary lifestyles due to economic development and urbanization. In contrast to developed countries, in India, the evidence base on implementing physical activity interventions is sparse. Approximately 70% of India's population lives in rural areas with resource-poor settings, where the increasing prevalence of NCDs is becoming an added burden. In India, the prevalence of hypertension was estimated to be 159.46 per thousand[7] (20 –.40% in urban adults and 12 – 17% among rural adults) affecting an estimated 118 million inhabitants in 2000.[8] This number is projected to almost double, that is, 214 million, in 2015.[9] In 2003, the prevalence of CHD was 3 – 4% in rural areas and 8 – 10% in urban areas.;[10] diabetes was 3.8% in rural areas and 11.8% in urban areas.[11] India has the largest number of people with diabetes in the world, with an estimated 19.3 million in 1995 and a projected 57.2 million in 2025.
Primary prevention of hypertension and CVD requires the understanding of a population approach to the reduction of major modifiable risk factors such as, physical inactivity. The goal of a population approach in the primary prevention of hypertension is to shift the community distribution of BP toward lower levels of ‘biological normality’. Even a small reduction in the mean BP of a population will produce a large reduction in the incidence of complications such as CHD and stroke.[12] It has been estimated that a 2 mm Hg downward shift in the entire distribution of Systolic Blood Pressure (SBP) is likely to reduce annual mortality from stroke by 6%, CHD by 4%, and all causes by 3%. The corresponding benefits for a 3 mm Hg downward shift in SBP were estimated to be 8, 5, and 4%, respectively.[13,14]
Given the epidemiological evidence of hazards of physical inactivity and the growing burden of NCDs, Operational Research is required to effectively motivate large sections of the population into health enhancing physical activity that is feasible, acceptable, and sustainable. The purpose of this study is to assess the effectiveness of the promotion of physical activity in the reduction of BP and blood sugar levels in a rural population, through community mobilization.
MATERIALS AND METHODS
This community-based intervention study followed the Social Cognitive theory, and the principles of Social marketing, like setting goals for behavior change, consumer research, segmentation of target audience, and marketing strategies.[15] The JIPMER Institute Ethics Committee approved the study.
Selection, description of participants, and baseline assessment
The villages of Periakattupalayam and Rangareddipalayam (total population of 1080) belong to Madalapattu Panchayat of Cuddalore district, Tamil Nadu. The study was done from 2008 to 2010. Initial contact and sensitization of the villagers was done through a Health camp and Health education sessions. The preparatory phase involved a meeting of village leaders and the identification of resource persons. The study was carried out in five phases: An awareness campaign, baseline assessment of participants, intervention (10 weeks), interim assessment, and final assessment. Four channels of communication were employed to create health awareness: Banners, pamphlets, group meetings, and one-to-one counseling. Subjects were recruited through village meetings and through Self-Help Groups (SHG). Subjects aged 20 to 49 years were included; those with chronic illness like asthma, arthritis, deformities that limited physical activity and pregnancy were excluded from the study.
Following informed consent, the sociodemographic details and baseline assessment of physical activity levels (short form of International Physical Activity Questionnaire – IPAQ) were collected. Height was measured to the nearest millimeter by using a Microtoise tape. Weight to the nearest 100 g was measured by UNICEF Electronic Scale 890-SECA. Using a measuring tape, the waist circumference to the nearest millimeter was measured between the costal margins and iliac crest, with the breath held at expiration. Blood pressure was recorded using a digital BP monitor (OMRONSEM-1, Japan), as recommended by the NCD Surveillance of IDSP (Integrated Disease Surveillance Project, India). After a five-minute rest, two readings were recorded three to five minutes apart. If SBP was ≥ 140 mm Hg or DBP ≥ 90 mm Hg, a third reading was taken after a 30-minute rest. An average of either two or three readings was taken to classify BP as Normal, Prehypertension, or Stage 1 or 2 Hypertension, based on the criteria given by the Joint National Committee (JNC 7). Fasting blood glucose was measured using a glucometer early in the morning (Accuchek, standardized with automated blood analyzer).
Sample size was calculated to detect a 4 mm Hg difference in SBP in the population (4 / 4 mm Hg BP reduction in normotensives) through regular physical activity.[12] Sample size was found to be 376 based on the formula 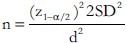 (SD of 4.2 mm Hg SBP change,[16]
(SD of 4.2 mm Hg SBP change,[16]
Precision (d) of 15%, power of 80%, and α of 0.05), Potential loss to follow-up was anticipated to be 25%, and hence, the final sample size was calculated as 470.
Intervention
‘Brisk walking (6 to 6.4 km / hour) for 30 minutes, four days / week, over and above the routine activities of daily living’[1] was set as the criteria for physical activity of moderate intensity. A cement road measuring 1500 m covered the inner circumference of the village. Participants were instructed to cover the entire cement road twice or thrice based on their activity levels and convenience, but for a minimum of 30 minutes per session. The intervention was planned for 10 weeks, as earlier studies had shown that significant reductions in BP occurred during the initial four to five weeks.[17] A physical instructor briefed the participants on brisk walking and gentle stretching exercises during baseline assessment and group meetings. Exercise of moderate intensity was explained to them in simple terms and it was modifiable to suit each individual. The physical instructor and the investigator joined the groups in their walk on most occasions, to ensure motivation and continued participation. Village leaders and youth club members were involved in periodic health education sessions, monthly meetings, and community events, to popularize physical activity.
Monitoring of exercise sessions
The study participants were divided into 30 small groups based on convenience of the timings of exercise (group size varied from 6 to 17). Members of SHGs, Youth Clubs, and other volunteers were assigned as group leaders. An attendance record of exercise sessions was maintained for each group. Four coordinators helped the investigator to monitor the intervention. Interim assessment of BP was done at six weeks, to check the compliance and sustain motivation. At the end of 10 weeks, BP, blood sugar, weight, and waist circumference were recorded. The number of exercise sessions per person was collected from the attendance records and converted into person hours of walking.
Total number of hours walked would be > 20 hours for subjects who complied with the intervention (30 minutes walking for four days / week, for 10 weeks). Similarly, the number of hours walked would be < 5 hours for subjects who walked on an average of less than one session per week, (considered as dropouts in this study). Accordingly, subjects were classified into three levels of compliance: < 5 person hours of walking (< 1 session / week, dropouts); 5 to 20 person hours of walking (one to four sessions / week), and > 20 person hours of walking (> 4 sessions / week).
Analysis
Data was analyzed using the SPSS Version 13. A level of P < 0.05 was considered as statistically significant, ‘before and after comparison (without controls) design’ was adopted in this study. Changes in BP, blood sugar, weight, BMI, and waist circumference (pre- and post-intervention values) were compared using the paired ‘t’ test. The chi square test was applied to compare differences in proportions. The efficacy of an intervention is a measure of the impact when all conditions are controlled to maximize the effect (ideal situation), and it is determined by using ‘Analysis by Protocol’ (whether or not the intervention works in those who receive it). Effectiveness is measured when the intervention is administered to subjects in the ‘real-life situation’, including dropouts.[18] Results of this study have been documented using both ‘Intention-to-Treat’ and ‘Analysis by Protocol’ methods.
RESULTS
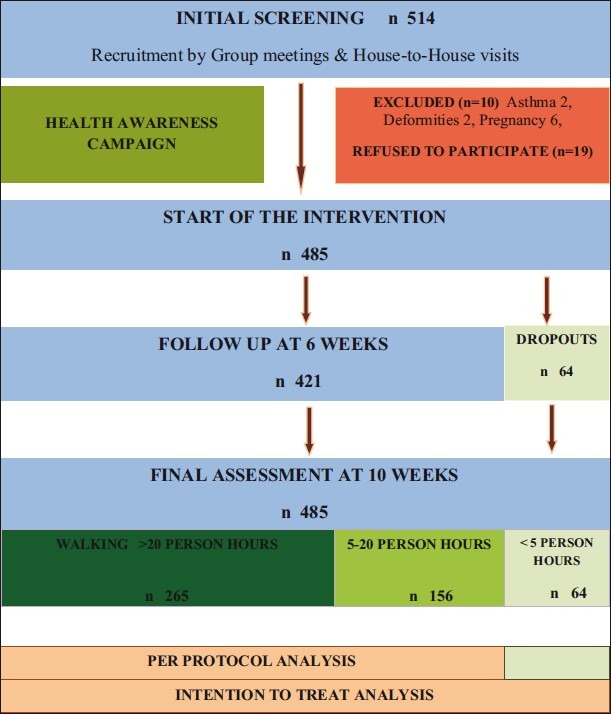
Of the total 514 age-eligible individuals screened from the study villages, 10 were excluded and 485 subjects were available and willing to participate. Participants flow through the study is depicted in Figure 1. The sociodemographic characteristics of the participants are given in Table 1. Prevalence of hypertension among the participants was 8.7%.
Figure 1.
Flow chart describing participants’ progress through the study
Table 1.
Sociodemographic characteristics of the study population at baseline
Compliance of the participants
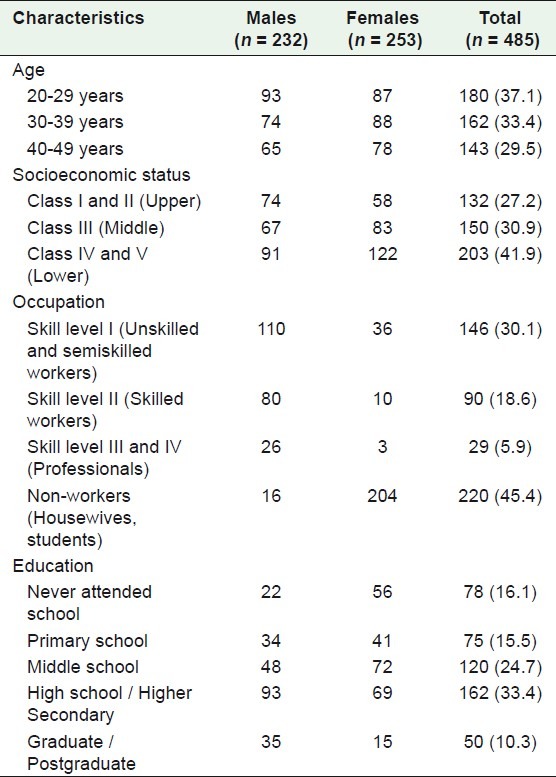
During the intervention, 421 out of 485 participants (86.8%) engaged in physical activity of moderate intensity (brisk walking). Of the 421 subjects, 265 (54.6%) engaged in more than 20 person hours of walking (walked more than four days a week), while 156 (32.2%) performed 5 to 20 person hours of walking (one to four days per week). The dropout rate was 13.2% (64 subjects) and was greatest during the first two weeks; 52 of these subjects (81%) discontinued walking within the first two weeks of the intervention. This was attributed mainly to lack of time or heavy workloads. At baseline, BP, fasting blood sugar, and anthropometric indices were similar in subjects who completed the intervention as well as dropouts (P > 0.05) [Table 2].
Table 2.
Comparison of baseline anthropometry, blood pressure, and blood sugar levels of the study population (subjects who completed intervention and dropouts)
Post-intervention changes in blood pressure
Intention-to-treat analysis was done on all 485 participants who were recruited for the intervention. Mean SBP was reduced from 122.40 mm Hg at baseline to 120.84 mm Hg at 10 weeks. A significant reduction of 1.56 mm Hg SBP (95% CI; 1.32 to 1.80) was observed (P = 0.000). The mean DBP fell from 76.81 mm Hg at baseline to 76.07 mm Hg at 10 weeks. A significant reduction of 0.74 mm Hg DBP (95% CI; 0.59 to 0.88) was observed (P = 0.000).
Per protocol analysis was done on 421 participants who engaged in physical activity and completed the intervention. Mean SBP went down from 122.06 mm Hg at baseline to 121.31 mm Hg at six weeks, during the interim assessment (P < 0.05). At the end of the 10-week intervention, the mean SBP went down to 120.24 mm Hg, resulting in a significant reduction of 1.82 mm Hg (95% CI; 1.57 to 2.08; P = 0.000) [Figure 2]. The mean DBP fell from 76.67 mm Hg at baseline to 76.37 mm Hg at six weeks, during the interim assessment (P > 0.05). After 10 weeks of intervention, the mean DBP fell to 75.80 mm Hg, resulting in a significant reduction of 0.87 mm Hg (95% CI; 0.72 to 1.03; P = 0.000) [Figure 2].
Figure 2.
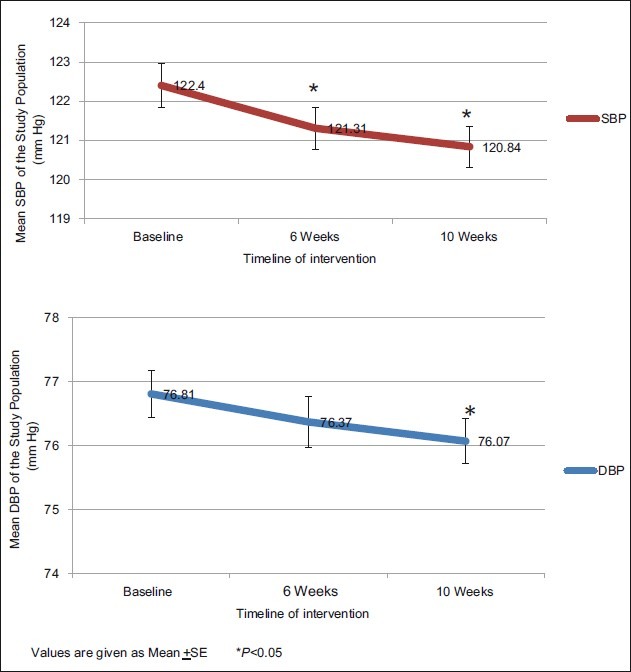
Change in population blood pressure from baseline to six weeks and 10 weeks
At the end of 10 weeks, the proportion of hypertensives in the study population fell from 7.8% to 4.5% and normotensives increased from 34 to 37% [Figure 3]. This proves that the distribution of BP can be influenced by a relatively simple non-pharmacological intervention.
Figure 3.
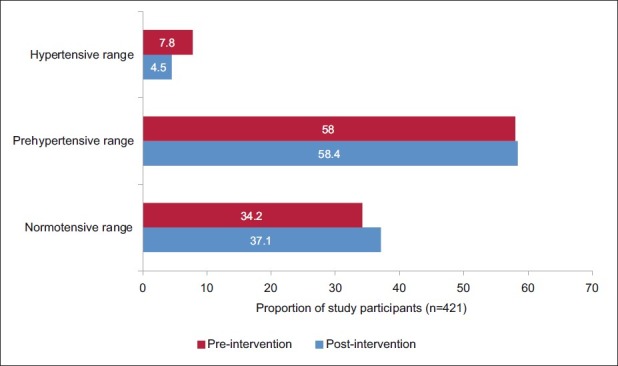
Effect of physical activity on blood pressure distribution in the study population
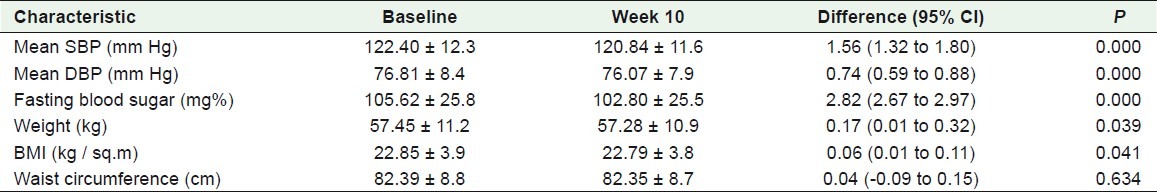
Post-intervention changes in blood sugar levels and anthropometry
The mean reduction of fasting blood sugar by 2.82 mg% (P < 0.05), body weight by 0.17 kg (P < 0.05), and BMI by 0.06 kg / m2 (P < 0.05), and a non-significant reduction of 0.04 cm in waist circumference were observed after 10 weeks of brisk walking, on the Intention-to-Treat analysis [Table 3]. On per protocol analysis, a mean reduction of blood sugar by 3.1 mg% (P < 0.05), body weight by 0.21 kg (P < 0.05), and BMI by 0.08 kg / m2 (P < 0.05), and a non-significant reduction of 0.07 cm (P = 0.309) in waist circumference were observed after 10 weeks of brisk walking.
Table 3.
Changes in blood pressure, blood sugar levels, and anthropometry after 10 weeks of intervention on the intention-to-treat analysis (n = 485)
DISCUSSION
As the adoption of physical activity is a complex behavior, varying degrees of participation were observed in the community: 54.6% of the subjects complied with walking on more than four days a week, while 32.2% engaged in brisk walking on one to four days a week; the dropout rate was 13.2%. Earlier studies on the promotion of physical activity have shown dropout rates ranging from 0 to 60% and compliance ranging from 53 to 100%.[19] Another study observed a dropout rate of 33% in the intervention group, at the end of 24 weeks.[20] The present study has demonstrated that it is feasible to motivate a community in a low resource setting to undertake a behavior-related non-pharmacological intervention.
This study has proved that a 10-week intervention to promote physical activity was effective in significantly reducing population mean BP by 1.56 / 0.74 mm Hg by the ‘Intention to Treat’ analysis and 1.82 / 0.87 mm Hg by the ‘Per Protocol’ analysis. The magnitude of BP response varied across studies, depending on the type of study (original study or meta-analysis), study setting (community or clinic based), duration of the study, type of participants (free or paid volunteers), methods of promoting physical activity, type and intensity of physical activity, techniques of monitoring compliance (investigator or group monitoring or no monitoring), reporting of physical activity (self-reported, group attendance or pedometer-based), and type of analysis (Per Protocol or Intention to Treat). Given the wide heterogeneity in study methodologies, comparison with other studies is difficult, but the public health implications of the significant BP reduction observed in this study can be illustrated as follows: It has been estimated that a 2 mm Hg downward shift in the distribution of SBP is likely to reduce annual mortality from stroke by 6%, CHD by 4%, and all causes by 3%. Mortality due to CHD, stroke, and all causes in India was 0.8[7], 0.6[7] and 7.4[21] per thousand (2008). It can be calculated that for a population of one million, the intervention effect of 1.56 mm Hg would result in an annual reduction of 25, 28, and 173 deaths due to CHD, stroke, and all causes, respectively, provided the population engages in physical activity of 30 minutes / day, four days a week.
In this study, the BP-lowering effect of brisk walking was more pronounced in hypertensives (4.5 / 2.74 mm Hg) compared to normotensives (1.55 / 0.69 mm Hg). This concurred with findings of several meta-analyses[22–24] and the World Hypertension League, which stated that BP reduced by 11 / 6 mm Hg in hypertensives and 4 / 4 mm Hg in normotensives, in response to physical activity.[12] SBP reduction of 5 mm Hg in hypertensives has the potential to reduce mortality from CHD, strokes, and all causes by 9, 14, and 7%, respectively.[25] The reduction of a 5 mm Hg SBP in hypertensives exhibited in this study proves the public health significance of the promotion of physical activity intervention in hypertensives as well. Regular exercise is also known to affect other cardiovascular risk factors favorably, such as, dyslipidemia, insulin resistance, body weight, arterial compliance, left ventricular hypertrophy, or impaired cardiovascular reflex control. Given the additional benefits and better acceptability as a lifestyle modification,[16] hypertensives should engage in regular physical activity.
However, the fact that hypertensives have higher BP reduction than normotensives does not undermine the importance of physical activity in the normal population; the significant BP reduction found in normotensives in this study is also important. Although relative risk of stroke and CHD in hypertensives is greater than in normotensives, the absolute number of deaths from these causes is greater in normotensive adults.[19] Studies have observed that the greatest absolute number of strokes occurred in individuals with DBP between 80 and 89 mm Hg.[26] The risk of stroke and CHD is directly related to the level of BP throughout the normotensive and hypertensive range.[27] This intervention reduced the proportion of hypertensives in the study population from 7.8 to 4.5% and increased the prevalence of normotensives from 34 to 37%. Therefore, the significant BP reductions observed among both hypertensive and normotensive adults in this study have public health importance in the prevention of hypertension and CVD at the population level.
The main strength of this study was the ‘Intention-to-Treat’ analysis, which facilitated an understanding of the effectiveness of the intervention. Replication of similar interventions would be possible in community settings in developing countries, as the study was conducted with minimal resources. Use of pedometers to monitor exercise sessions was not possible in this study because of cost and logistic reasons. As it was not possible to include a control population, a pre-post intervention design was adopted within the available resources. The strategy to increase walking could have included a graduated increase in the physical activity program, to allow for behavioral conditioning of the subjects, but this would have posed difficulties in understanding the effect size attributed purely to the intervention. Longer periods of study would be necessary to record changes in measurements like waist circumference or BMI and to observe attrition patterns in participation behavior. In countries such as India where there are competing demands for limited resources, evaluation of public health interventions have to be tailor-made to reduce costs involved in research. In this study, a significant mean reduction of fasting blood sugar by 2.82 mg%, body weight by 0.17 kg, BMI by 0.06 kg / m2, and a non-significant reduction of 0.04 cm in waist circumference were observed. This has to be interpreted in the light of the fact that higher exercise intensity is required to influence body weight and blood sugar (50 to 60 minutes per day on most days of the week).[6,28]
Developed countries like Canada, Finland, New Zealand, Australia, US, and Denmark have implemented comprehensive strategies to address physical inactivity. Developing countries like Iran (Isfahan Healthy Heart Project) and Pakistan (Lodharan project) have initiated demonstration projects on the promotion of physical activity. India has initiated community projects like the Ballabgarh initiative and Chandigarh Healthy Heart project. The World Health Organization states that the important characteristics of the promotion of physical activity programs are: political commitment, integration in national policies, goal setting, funding, support from stakeholders, cultural sensitivity, inter-sectoral coordination, strong leadership, and workforce development.[29] This is reflected in the National program for Prevention and Control of Diabetes, Cardiovascular Diseases, and Stroke,[30] in India, which aims at health promotion through community interventions, by targeting physical activity and diet.
In conclusion, the functional feasibility of enabling people to undertake physical activity in the natural community and its effectiveness in significantly reducing the population's mean BP and blood sugar levels, in a low resource setting, have been proven by this study. Given the burden of Hypertension and CVD in India, there is an urgent need for community-based interventions, to socially market the concept of a physically active lifestyle. The findings of this study can help secure public support and an enabling environment for comprehensive community-based lifestyle interventions, even in developing countries.
ACKNOWLEDGMENT
Dr. Gautam Roy, Professor, Department of Preventive and Social Medicine, JIPMER, Pondicherry, India
Footnotes
Source of Support: Partly funded by the Department of Preventive and Social Medicine, JIPMER, Pondicherry, India
Conflict of Interest: Nil
REFERENCES
- 1.Bhalwar R. Textbook of public health and community medicine. AFMC, Pune: WHO India country office; 2009. [Google Scholar]
- 2.Fletcher GF, Blair SN, Blumenthal J, Caspersen C, Chaitman B, Epstein S, et al. Statement on exercise. Benefits and recommendations for physical activity programs for all Americans. A statement for health professionals by the Committee on Exercise and cardiac rehabilitation of the Council of Clinical Cardiology, American Heart Association. Circulation. 1992;86:340–4. doi: 10.1161/01.cir.86.1.340. [DOI] [PubMed] [Google Scholar]
- 3.Bull FC, Armstrong TP, Dixon T, Ham S, Neiman A, Pratt M. Physical inactivity. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative quantification of health risks. Geneva: WHO; 2004. pp. 729–881. [Google Scholar]
- 4.Global strategy on diet, physical activity and health. Geneva: WHO; 2004. World Health Organisation. [Google Scholar]
- 5.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C. Physical activity and public health: A recommendation from the centers for disease control and prevention and the American college of sports medicine. J Am Med Assoc. 1995;273:402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 6.Diet, nutrition and the prevention of chronic diseases: TRS 916. Geneva: World Health Organization, Technical Report Series; 2003. Joint WHO / FAO Expert Consultation. [PubMed] [Google Scholar]
- 7.Shah B, Kumar N, Geetha R. Assessment of burden of Non-communicable diseases. Ansari Nagar and WHO India: ICMR; 2009. [Google Scholar]
- 8.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–8. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 9.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 10.Gupta R. Burden of coronary heart disease in India. Indian Heart J. 2005;57:632–8. [PubMed] [Google Scholar]
- 11.King H, Aubert RE, Herman WH. Global burden of Diabetes, 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1996;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 12.World Hypertension League. Physical exercise in the management of hypertension: A consensus statement. J Hypertens. 1991;9:283–7. doi: 10.1097/00004872-199103000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Community prevention and control of cardiovascular diseases TRS No.732. Geneva: WHO; 1986. WHO Expert Committee. [PubMed] [Google Scholar]
- 14.Stamler R. Implications of the INTERSALT study. Hypertension. 1991;17S:1017–20. doi: 10.1161/01.hyp.17.1_suppl.i16. [DOI] [PubMed] [Google Scholar]
- 15.Gordon R, McDermott L, Stead M, Angus K. The effectiveness of social marketing interventions for health improvements: What's the evidence? Public Health. 2006;120:1133–9. doi: 10.1016/j.puhe.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Saptarishi LG, Soudarssanane MB, Thiruselvakumar D, Navasakthi D, Mathanraj S, Karthigeyan M, et al. Community based randomized controlled trial of non-pharmacological interventions in prevention and control of hypertension among young adults. Indian J Community Med. 2009;34:329–34. doi: 10.4103/0970-0218.58393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper AR, Moore LAR, McKenna J, Riddoch CJ. What is the magnitude of blood pressure response to a programme of moderate intensity exercise.Randomised controlled trial among sedentary adults with unmedicated hypertension? Br J Gen Pract. 2000;50:958–62. [PMC free article] [PubMed] [Google Scholar]
- 18.Fletcher RH, Fletcher SW, Wagner EH. Clinical epidemiology: The essentials. Fourth ed. Maryland, USA: Lippincot Williams and Wilkins; 2005. [Google Scholar]
- 19.Kelley GA, Kelley KA, Tran ZV. Aerobic exercise and resting blood pressure: A meta-analytic review of randomized controlled trials. Prev Cardiol. 2001;4:73–80. doi: 10.1111/j.1520-037x.2001.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Locke CT, Bell RC, Myers AM, Harris SB, Ecclestone NA, Lauzon N, et al. Controlled outcome evaluation of the First Step Program: A daily physical activity intervention for individuals with type II diabetes. Int J Obes. 2004;28:113–9. doi: 10.1038/sj.ijo.0802485. [DOI] [PubMed] [Google Scholar]
- 21.SRS Bulletin. New Delhi: Ministry of Home Affairs, Government of India; [Last cited on 2008]. Registrar General India. Available from: http://censusindia.gov.in/Vital_Statistics/SRS_Bulletins/SRS_Bulletins_linkS/SRS_Bulletin_October_2008.pdf . [Google Scholar]
- 22.Fagard RH. Exercise characteristics and the blood pressure response to dynamic physical training. Med Sci Sports Exerc. 2001;33:S484–92. doi: 10.1097/00005768-200106001-00018. [DOI] [PubMed] [Google Scholar]
- 23.Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA, Andrews GR. The effectiveness of exercise training in lowering blood pressure: A meta-analysis of randomised controlled trials of 4 weeks or longer. J Hum Hypertens. 1997;11:641–9. doi: 10.1038/sj.jhh.1000509. [DOI] [PubMed] [Google Scholar]
- 24.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure.A meta-analysis of randomized controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 25.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic and cardiovascular risks: US population data. Arch Intern Med. 1993;153:598–615. doi: 10.1001/archinte.153.5.598. [DOI] [PubMed] [Google Scholar]
- 26.MacMahon S, Rodgers A. Blood pressure, antihypertensive treatment and stroke risk. J Hypertens. 1994;12:S5–14. [PubMed] [Google Scholar]
- 27.MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, et al. Blood pressure, stroke, and coronary heart disease. Part 1: Prolonged differences in blood pressure: Prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–74. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 28.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 29.A guide for population-based approaches to increasing levels of physical activity - Implementation of the WHO Global strategy on Diet, Physical activity and Health. Geneva: World Health Organization; 2007. World Health Organisation. [Google Scholar]
- 30.Ministry of Health and Family Welfare, GoI. Pilot phase of the National Program for Prevention and Control of Diabetes, Cardiovascular Diseases and Stroke (NPDCS) Government of India: MOHFW. Available from: http://www.mohfw.nic.in/D1.htm .


