Abstract
Background:
Complementary and alternative medicine (CAM) is a popular treatment option for many populations. The present work is aimed at studying the knowledge and attitude of health professionals in the Riyadh region, Saudi Arabia, toward CAM.
Material and Methods:
In this cross-sectional survey, a multistage random sample was taken from health professionals working in hospitals in Riyadh city and surrounding governorates. Data were collected through a self-administered questionnaire, from 306 health professionals working in 19 hospitals, on socio-demographic data, knowledge about CAM and their sources, and attitudes toward CAM practices.
Results:
Of the participants, 88.9% had some knowledge about CAM. Respondents with a doctorate degree (94.74%) and 92.53% of those with a bachelor's degree had significantly higher knowledge of CAM than subjects with a diploma, a fellowship, or a master's degree (68.75%, 76.67%, and 85.41%, respectively, P = 0.004). Mass media represented 60.1% of sources of the knowledge of CAM followed by family, relatives, and friends (29.08%) and health educational organizations (14.71%). Participants estimated that prophetic medicine including prayer, honey and bee products, medical herbs, Hijama, nutrition and nutritional supplements, cauterization, and camel milk and urine were the most commonly used CAM practices (90.5%, 85%, 76.9%, 70.6%, 61.4%, 55.9%, and 52.5%, respectively) in addition to medical massage (61.8%) and acupuncture (55%). One hundred and fifteen (80%) physicians were ready to talk with their patients on CAM.
Conclusion:
The willingness to improve knowledge and create a positive attitude in health professionals toward CAM has increased. Religious practices, especially those related to prophetic medicine, are more common in the region. Health educational organizations have to play a greater role by being the source of evidence-based knowledge of CAM. Talking on CAM with patients should be improved by rooting them on evidence-based practices.
Keywords: Alternative, complementary, prophetic medicine, health educational organizations, health institutes , health professionals, knowledge, attitude, mass media, Saudi Arabia
INTRODUCTION
Complementary and alternative medicine (CAM) is widely used both as a supplement to conventional or mainstream health care and as part of traditional health care systems and practices.[1] The definition of CAM is so diverse that it is difficult to formulate a universally accepted list of therapies and practices that fall under its ambit. The National Centre for Complementary and Alternative Medicine (NCCAM) in the USA defined CAM as a group of diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.[2]
Australian data, published in 2007, reported that 69% of the population had used one or more forms of CAM in the previous 12 months. However, the use of CAM varied with age, sex, and a range of other factors.[3] Those with chronic health issues, cancer, and/or chronic pain in particular, were found to have made greater use of CAM.[4] Exact estimates of expenditure on CAM have been difficult to determine though there is little doubt that it is enormous. In 2002, it was estimated that the amount spent on CAM in the USA was US $2.7 billion, US$ 2.4 billion in Canada, and US$ 2.3 billion in the United Kingdom.[5]
What is thought of as conventional health care varies from country to country across geographical boundaries and cultures and changes with time,[1,6] an indication that the boundary between CAM and conventional medicine is blurred and constantly shifting. Baer believes this blurring and blending has given rise to the integrative medical movement whose aim is to use the best of both CAM and conventional care.[7]
In Saudi Arabia, Tibbu Nabawi or prophetic medicine is broadly accepted and practiced by most physicians and the public. This is evidenced by the study of National Center for CAM in Saudi Arabia 2010[8] and Al-Faris et al.,[9] who recorded that more than 70% of the public in the Riyadh region had used practices related to prophetic medicine in their lifetime.
The attitude of health care providers toward the use of complementary therapies, and their exposure to education on CAM, requires careful consideration in contemporary health care. Many factors influence the use of CAM: dissatisfaction with conventional care, a desire for greater personal involvement in the maintenance of health, holistic health beliefs,[10] lack of access to adequate health care services, and ready availability of CAM services.[11] In one study, it was found that more patients were expressing their desire for CAM services.[12] It is hardly surprising therefore that several national and international studies that surveyed physicians’ practices and beliefs on CAM noted a considerable variation in responses regarding the practice of, referrals for, and safety and efficacy of specific types of CAM.[13] In line with this trend, the present study was carried out to assess the level of knowledge of CAM and measure attitudes of health professionals in the Riyadh region, Saudi Arabia, toward CAM.
MATERIAL AND METHODS
The present study was a cross-sectional descriptive survey carried out in the Riyadh region, including Riyadh city and surrounding governorates, Saudi Arabia, from January 2010 to March 2010. Health professionals working in all hospitals in the specified region formed the target of the study. According to the Saudi demographic census of 1429H (2008), the Riyadh region has 42 hospitals and 363 primary health care centers with 4924 physicians, 440 pharmacists, 5391 allied health personnel, and 1168 technicians. Of the health professionals, 380 were randomly selected using a multistage random sample technique. The plan was to include physicians (50%), allied health personnel and pharmacists (20% for each), and technicians (10%) in the sample. Four governorates were chosen randomly from all governorates around Riyadh city. One hospital was selected randomly from each governorate. From Riyadh city, 15 hospitals were chosen randomly: 5 from governmental hospitals related to Ministry of Health (MOH), 5 from governmental hospitals not related to MOH, and 5 from nongovernmental hospitals. In total, the number of hospitals included in the study was 19. From these selected hospitals, a systematic random sample was drawn to obtain a sample of physicians, pharmacists, allied health personnel, and technicians. The different health care personnel were chosen in the ratio of 5:2:2:1, respectively.
Data were collected by means of self-administered questionnaires which requested socio-demographic data, knowledge about CAM and its sources, and attitudes toward CAM especially for its integration into the health care services and medical school curricula. Of special emphasis could be the most common CAM practices in Saudi Arabia such as the prophetic medical practices and the patient-physician relationship with regard to CAM. Twenty data collectors were trained and skilled to deal with participants and expected obstacles in data collection. They distributed and collected the completed questionnaires from the respondents at the same setting. Twenty-three questionnaires were not completed. Proper consent, voluntary participation, confidentiality, and the right to withdraw were all ensured. The study was approved by the Ethical Committee of the National Center of Complementary and Alternative Medicine (NCCAM) in Riyadh.
After revising the answered questionnaires, those with incomplete or with faulty data were excluded from the study (51). The remaining questionnaires (306) were coded and the data entered into the SPSS statistical package, version 16. Data were presented and statistically analyzed using the mean and standard deviation for quantitative data and frequencies for qualitative data. The chi-square test was used to test the association of different variables with socio-demographic data of participants. The evaluation of the degree of agreement of health professionals to some aspects of CAM was done by the Likert scale. A mean score of 1–1.74 represented strongly disagree, 1.75–2.49 meant disagree; 2.49–3.24 meant agree, and a mean score of 3.25–4 represented strongly agree. The level of significance used was 5%.[14]
RESULTS
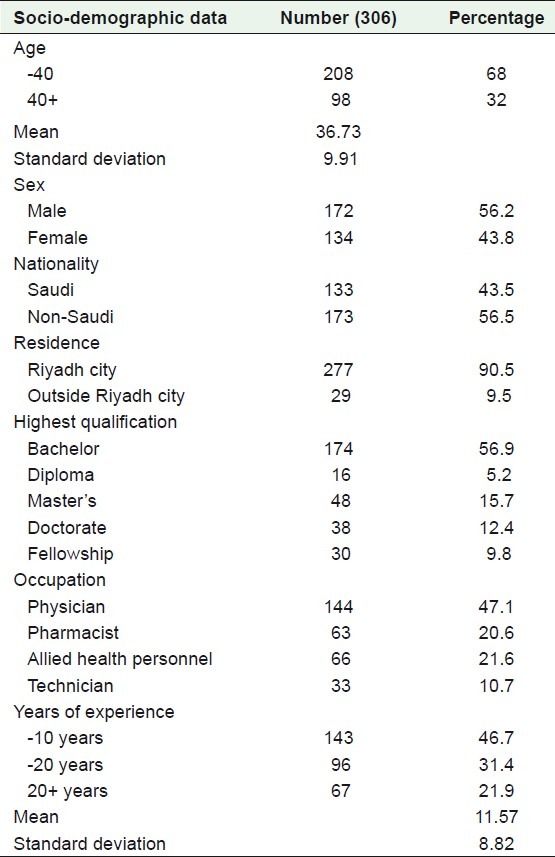
The mean age of the participants was 36.73±9.91 years with 56.2% of them were males, 43.5% Saudi and 90.5% working in the Riyadh city. Of the participants, 56.9% had bachelor's degree while only 5.2% had diploma and 12.4% had doctorate. Physicians represented 47.1%, pharmacists and allied health personnel represented about 21% for each while technicians represented 10.7%, with a mean of 11.57±8.82 years of experience [Table 1].
Table 1.
Socio-demographic data of the studied population
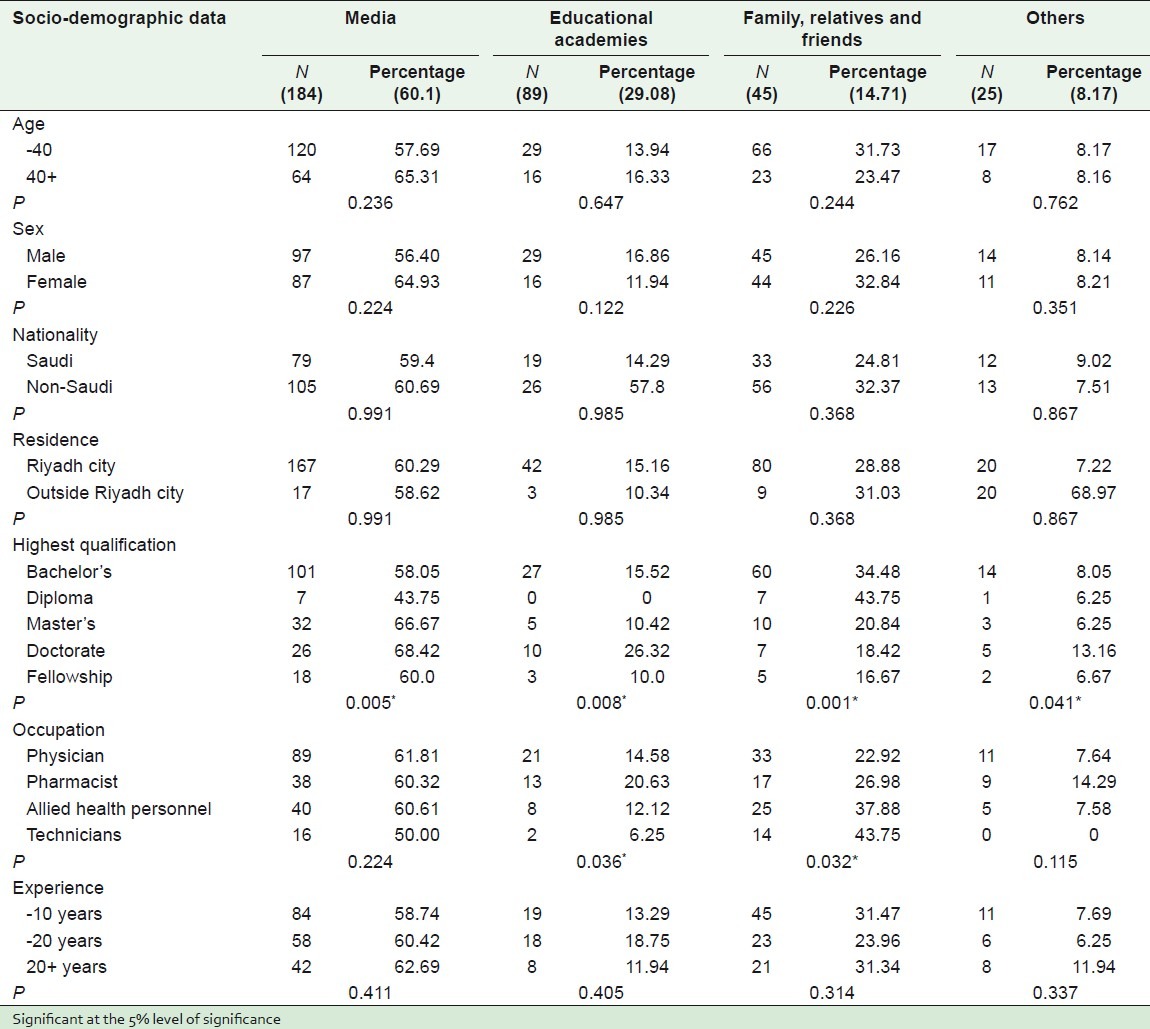
Of the participants, 88.9% reported they had some knowledge about CAM compared with 11.1% who had never heard about CAM. A total of 94.74% of those with a doctorate degree and 92.53% of those with a bachelor's degree had significantly higher knowledge than those with a diploma, master′s, and a fellowship with a statistically significant difference (P = 0.004). Media including television., newspapers, and the radio represented 60.1% of the sources of knowledge on CAM followed by family members, relatives, and friends (29.08%) and then health educational organizations (14.71%). Other not so common sources (8.17%) included the internet and books [Table 2]. Participants with a doctorate degree had educational organizations as the source of their knowledge, which was significantly higher than participants with other degrees (P = 0.008). However, the pharmacist group had the highest score with knowledge derived from health educational organizations. Next were physicians, then allied health personnel, and finally technicians with a statistically significant difference (P = 0.036; Table 3).
Table 2.
Socio-demographic data and knowledge related to CAM
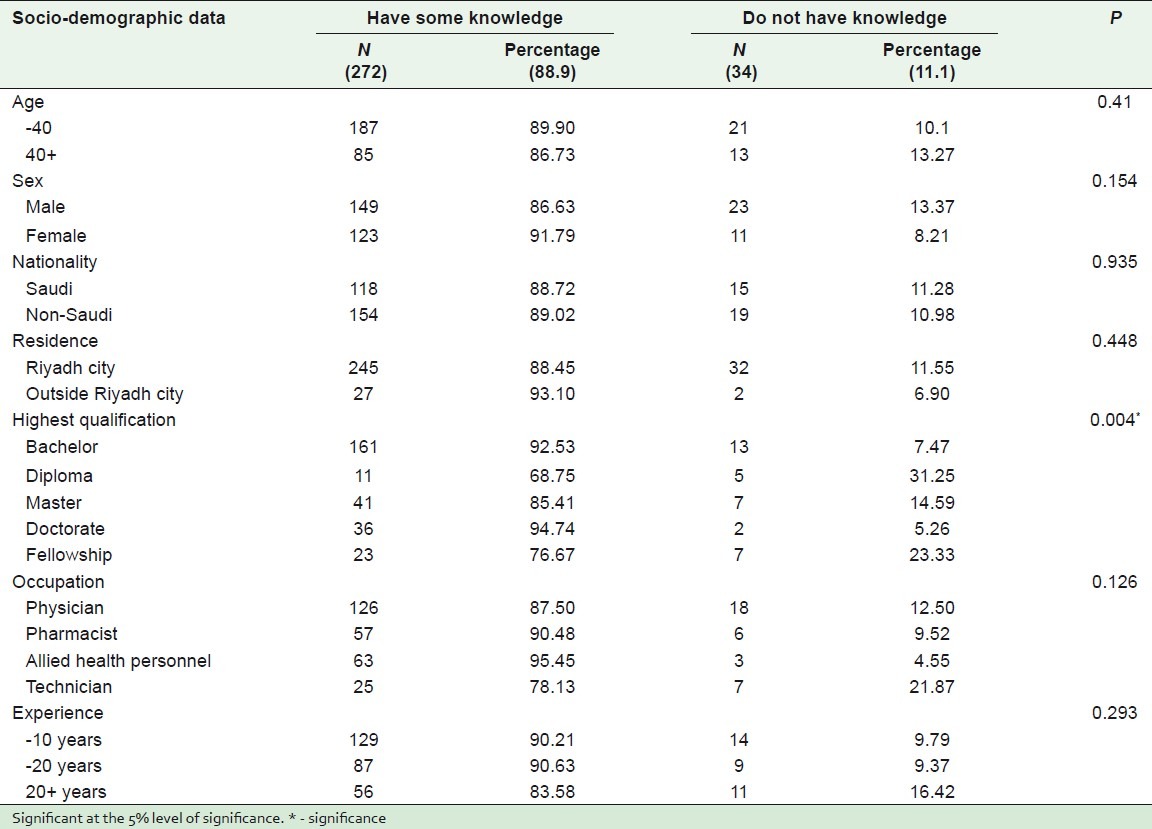
Table 3.
Sources of knowledge about CAM and socio-demographic data
The most important and commonly used CAM practices in the Kingdom from participants’ perspective were related to prophetic medicine, including prayer, honey and bee products, medical herbs, Hijama, nutrition and nutritional supplements, cauterization, and camel milk and urine (90.5%, 85%, 76.9%, 70.6%, 61.4%, 55.9%, and 52.5%, respectively) in addition to medical massage (61.8%) and acupuncture (55%; Figure 1). Of the physicians participating in the study, 115 (80%) had talked about CAM with their patients. Participants strongly agreed that there was a need for health education on the subject. There was a need for more research, more information, and internet sites for CAM. These practices have to be integrated into the health care services, and medical school curricula. Also, special centers should be set up to provide CAM [Figure 2].
Figure 1.
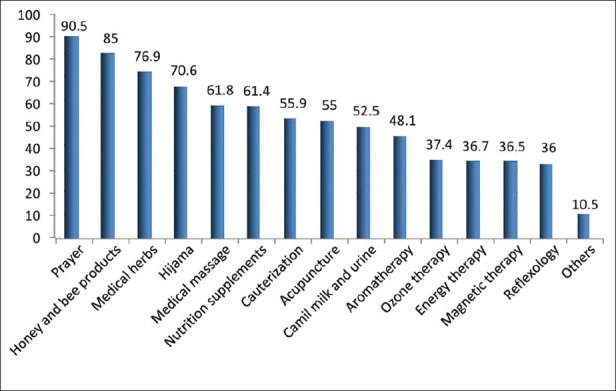
Most important used CAM practices in Saudi Arabia
Figure 2.
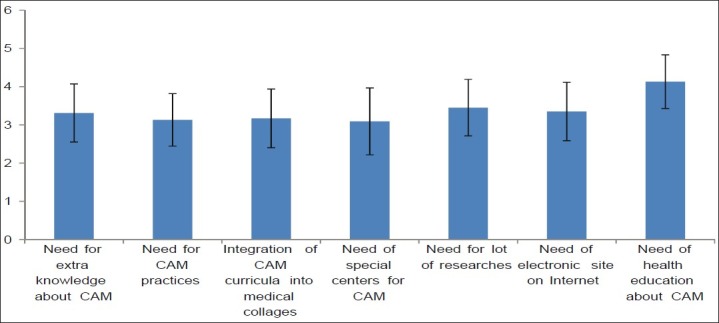
Likert score (χ± SD) of requirements related to CAM
DISCUSSION
After its recent establishment in Saudi Arabia, NCCAM made its priority to undertake a situation analysis of the position of CAM in the Kingdom, particularly with regard to current attitudes and the knowledge of health professionals. Since it was obvious that patients were reluctant to disclose their use of CAM, it was incumbent on health professionals to be proactive by initiating talking on CAM. This means they ought to be familiar with this aspect of medicine.[15]
The definition of CAM was discussed with all participants of this study to avoid confusion and misconceptions. With the use of probability sampling and a response rate of 80.53%, the results gave a fairly representative view of knowledge and attitudes of health professionals in the Riyadh region, to the subject.
Results of the present study showed that technicians were less knowledgeable (78.13%) than physicians (87.50%), pharmacists (90.48%), and allied health personnel (95.45%). Previous studies in industrialized countries[16,17] and developing ones[18,19] showed that health care givers had relatively poor knowledge of herbal medicine and supplementary foods and their possible interactions and toxic effects. Pharmacists seemed to be more knowledgeable than physicians, nurses, and technicians.[17] In a study in the United Arab Emirates carried out by Hassan et al. in 2000,[20] it was found that in spite of physicians’ lack of knowledge about different types of CAM, they did not consider it quackery. In the present study, those with a doctorate and a bachelor's degree were the most knowledgeable. This partly reflects the increased interest in CAM in the new generation and the better qualified health professionals. It also partly reflects the revision of some curricula to include CAM, as has been the case in the College of Pharmacy.
Of the health professionals in the present study, only 29.08% had acquired their knowledge from health educational institutions. This may indicate an absence of CAM in medical curricula. A total of 8.2% of the participants had acquired their knowledge from the internet or books or training courses and lectures. This was unexpected since many licensed electronic databases (e.g., Natural Medicine Comprehensive Database, http://www.naturaldatabase.com/) have been available for several years. Therefore, there should be educational campaigns with lectures, seminars, and other activities to demonstrate and explain the tools associated with these databases. However, Wahner-Roedler[21] found positive relations between the use of computer technology and the internet as a source of knowledge and self-training in addition to its use as a communication tool with peers and colleagues. Most published studies indicate that physicians agree on the need for the dissemination of more information about CAM, and 62–81% of them expressed the need for education and training on its practices.[22,23]
Health professionals in the present study stated that prophetic medicine including prayer, honey and bee products, medical herbs, Hijama, food supplements, and cauterization, as well as acupuncture and massage therapy were the most important of the CAM practices used in the region. Western researches have intimated that acupuncture was the most accepted CAM practice for physicians (43%) followed by chiropractic (40%) and massage therapy (21%).[21]
Of the physicians participating in the present study, 115 (80%) had talked on CAM with their patients. These results are in agreement with some European studies,[24,25] and with a study by Hassan et al. who found that most physicians in the United Arab Emirates talked about CAM with their patients.[20]
Many researches have indicated different perceptions of health professionals toward the use of CAM.[12,22] Those working in hospitals as well as old health professionals were less tolerant and more opposed to CAM practices. This aversion may be due to the lack of evidence on CAM and the nature of its practices.[5] Gianelli found that 42% of general practitioners in Italy did not give advice to their patients to use CAM. However, other studies have indicated the acceptance of CAM by general practitioners and specialists.[26] Studies done in Germany and Russia stated that physicians used CAM together with conventional medicine.[27,28] While Wahner-Roedler recorded that physicians in USA had got good results with CAM and 44% of these physicians referred patients to CAM practitioners.[21] In the UK[29] and Netherlands,[30] most physicians referred their patients to CAM practitioners. In Nigeria, pharmacists felt that they needed continuous training on the use of herbs and their interaction with drugs.[31]
The limitations of the present study are that since it represented the Riyadh region only, the results cannot be generalized to cover all regions in Saudi Arabia. At the same time, the absence of similar local knowledge and studies on attitudes toward CAM makes it difficult to guarantee the credibility of results. The study sampling did not take into account the different specialties of the physicians and allied health personnel.
CONCLUSION
The role played by health educational organizations, textbooks, internet, and training courses as the sources of knowledge about CAM is insignificant. The attitude toward CAM is generally positive but there is a need for more evidence-based knowledge, research, and internet sites for CAM. The integration of CAM practices into health care services and curricula of medical schools is essential. Practices related to prophetic medicine are the commonest in the region. The initiation of the talking about evidence-based CAM practices with patients should be encouraged and improved.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Bodeker G, Ong CK, Grundy C, Burford G, Shein K. WHO global atlas of traditional, complementary and alternative medicine, Text and Map Volumes World Health Organization Center for Health Development. Kobe: WHO Global Atlas of Traditional, Complementary and Alternative Medicine; 2005. [Google Scholar]
- 2.National Center for Complementary and Alternative Medicine (NCCAM) What Is CAM? 2007. [Last accessed on 2008 Sep 22]. Available from: http://nccam.nih.gov/health/whatiscam/
- 3.Xue CC, Zhang AL, Lin V, Da Costa C, Story DE. Complementary and alternative medicine use in Australia: A national population-based survey. J Altern Complement Med. 2007;13:643–50. doi: 10.1089/acm.2006.6355. [DOI] [PubMed] [Google Scholar]
- 4.Saydah SH, Eberhardt MS. Use of complementary and alternative medicines among adults with chronic disease: United States 2002. J Altern Complement Med. 2006;12:805–12. doi: 10.1089/acm.2006.12.805. [DOI] [PubMed] [Google Scholar]
- 5.MacLennan AH, Wilson DH, Taylor AW. The escalating cost and prevalence of alternative medicines. Prev Med. 2002;35:166–73. doi: 10.1006/pmed.2002.1057. [DOI] [PubMed] [Google Scholar]
- 6.Zollman C, Vickers A. ABC of complementary medicine--Complementary medicine and the doctor. Br Med J. 1999;319:1558–61. doi: 10.1136/bmj.319.7224.1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baer H. The emergence of integrative medicine in Australia: The growing interest of biomedicine and nursing in complementary medicine in a southern developed society. Med Anthropol Q. 2008;22:52–66. doi: 10.1111/j.1548-1387.2008.00003.x. [DOI] [PubMed] [Google Scholar]
- 8.AlBedah MN, El-Olemy A, Khalil MK. Knowledge, attitude and practice of public in Riyadh region, Saudi Arabia, about complementary and alternative medicine. Egypt J Community Med. 2010;28:39–52. doi: 10.4103/2230-8229.98290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Faris EA, Al-Rowais N, Mohamed AG, Al-Rukban MO, Al-Kurdi A, Al-Noor MA, et al. Prevalence and pattern of alternative medicine use: The results of a household survey. Ann Saudi Med. 2008;1:4–10. doi: 10.5144/0256-4947.2008.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bishop EL, Yardley L, Lewith GT. A systematic review of beliefs involved in the use of complementary and alternative medicines. J Health Psychol. 2007;12:851–67. doi: 10.1177/1359105307082447. [DOI] [PubMed] [Google Scholar]
- 11.Moga MM, Mowery B, Geib R. Patients are more likely to use complementary medicine if it is locally available. Rural Remote Health. 2008;8:1028. [PubMed] [Google Scholar]
- 12.Ben-Arye E, Frenkel M, Klein A, Scharf M. Attitudes toward integration of complementary and alternative medicine in primary care: Perspectives of patients, physicians and complementary practitioners. Patient Educ Couns. 2008;70:395–402. doi: 10.1016/j.pec.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Astin JA, Marie A, Pelletier KR, Hansen E, Haskell WL. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med. 1998;158:2303–10. doi: 10.1001/archinte.158.21.2303. [DOI] [PubMed] [Google Scholar]
- 14.Dawes J. “Do Data Characteristics Change According to the number of scale points used. An experiment using 5-point, 7-point and 10-point scales”? Int J Market Res. 2008;50:61–77. [Google Scholar]
- 15.Bauer BA. Herbal therapy: What a clinician needs to know to counsel patients effectively. Mayo Clin Proc. 2000;75:835–41. doi: 10.4065/75.8.835. [DOI] [PubMed] [Google Scholar]
- 16.Suchard JR, Suchard MA, Steinfeldt JG. Physician knowledge of herbal toxicities and adverse herb-drug interactions. Eur J Emerg Med. 2004;11:193–7. doi: 10.1097/01.mej.0000134721.72356.f7. [DOI] [PubMed] [Google Scholar]
- 17.Kemper KJ, Gardiner P, Gooble, Woods C. Expertise about herbs and dietary supplements among diverse health professionals. BMC Complement Altern Med. 2006;286:15. doi: 10.1186/1472-6882-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clement TN, Williams AF, Khan K, Bernard T, Bernard T, Bhola S, et al. A gap between acceptance and knowledge of herbal remedies by physicians: The need for educational intervention. BMC Complement Altern Med. 2005;185:20. doi: 10.1186/1472-6882-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adisa R, Fakeye TO. Assessment of knowledge of community pharmacists regarding common phytopharmacueticals sols in south western Nigeria. Trop J Pharm Res. 2006;5:619–25. [Google Scholar]
- 20.Hassan MY, Das M, Bahjat S. Alternative medicine and the medical profession: Views of medical students and general practitioners. East Mediterr Health J. 2000;6:25–33. [PubMed] [Google Scholar]
- 21.Wahner-Roedler D, Vincent A, Elkin PL, Loehrer LL, Cha SS, Bauer BA. Physicians’ attitude toward complementary and alternative medicine and their knowledge of specific therapies: A survey at an Academic Center. Evid Based Complement Altern Med. 2006;3:495–501. doi: 10.1093/ecam/nel036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Milden SP, Stokols D. Physicians’ attitudes and practices regarding Complementary and alternative medicine. Behav Med. 2004;30:73–82. doi: 10.3200/BMED.30.2.73-84. [DOI] [PubMed] [Google Scholar]
- 23.Hall J, Bulik R, Sierpina V. Community preceptors’ attitudes toward and practices of complementary and alternative medicine: A Texas survey. Tex Med. 2003;99:50–3. [PubMed] [Google Scholar]
- 24.Borkan JM, Neher JO, Anson O, Smoker B. Referrals for alternative therapies. J Fam Pract. 1994;39:545–50. [PubMed] [Google Scholar]
- 25.Fulder SJ, Munro RE. Complementary medicine in the United Kingdom: Patients, practitioners and consultations. Lancet. 1985;2:542–5. doi: 10.1016/s0140-6736(85)90473-8. [DOI] [PubMed] [Google Scholar]
- 26.Giannelli M, Cuttini M, Da Fre M, Buiatti E. General practitioners’ knowledge and practice of complementary/alternative medicine and its relationship with life-styles: A population-based survey in Italy. BMC Fam Pract. 2007;8:30. doi: 10.1186/1471-2296-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown S. Use of complementary and alternative medicine by physicians in St. Petersburg, Russia. J Altern Complement Med. 2008;14:315–9. doi: 10.1089/acm.2007.7126. [DOI] [PubMed] [Google Scholar]
- 28.Joos S, Musselmann B, Miksch A, Rosemann T, Szecsenyi J. The role of complementary and alternative medicine (CAM) in Germany - A focus group study of GPs. BMC Health Serv Res. 2008;8:127. doi: 10.1186/1472-6963-8-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wharton R, Lewith G. Complementary medicine and the general practitioner. Br Med J. 1986;292:1498–500. doi: 10.1136/bmj.292.6534.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Visser GJ, Peters L. Alternative medicine and general practitioners in the Netherlands: Towards acceptance and integration. Fam Pract. 1990;7:227–32. doi: 10.1093/fampra/7.3.227. [DOI] [PubMed] [Google Scholar]
- 31.Fakeye TO, Onyemadu Evaluation of knowledge base of hospital pharmacists and physicians on herbal medicines in southwestern Nigeria. Pharm Pract. 2008;6:88–92. doi: 10.4321/s1886-36552008000200005. [DOI] [PMC free article] [PubMed] [Google Scholar]


