Abstract
Background:
Patients of chronic obstructive pulmonary disease (COPD) are at high risk for depression and anxiety. Yoga techniques are suited for promoting relaxation, psycho-emotional stability and exercise tolerance. Studies showing the effect of yoga in diffusion capacity are not available; hence this study was planned.
Materials and Methods:
The study was conducted on 60 diagnosed stable mild-to-moderate COPD patients in the age group of 30-60 years, of either sex, in the department of physiology. Patients were taken from Guru Teg Bahadur Hospital, Delhi and divided into two groups: Control and the yoga group. Both the groups were on conventional drug therapy. Subjects from the Yoga group was called to cardiopulmonary laboratory daily for 21 days and then weekly for the compliance. Yoga instructor taught them the technique of pranayama and various postures every day. They practiced yoga at home for 2 months for 45 min in the mornings. Diffusion capacity was recorded by using computerized Medisoft instrument (HYPAIR compact), in both the groups before and after 2 months.
Results:
Statistical analysis showed significant improvement in TLCO of the yoga group. Transfer factor of lung for carbon monoxide i.e. TLCO in mild COPD increased from 17.61 ± 4.55 to 19.08 ± 5.09 ml/mmHg/min, and in moderate COPD it increased from 14.99 ± 4.02 to17.35 ± 3.97 ml/mmHg/min.
Conclusion:
It was concluded that yogic breathing exercises improve diffusion capacity. They are beneficial to COPD patients and they can be used as an adjunct therapy with the conventional medical therapy.
Keywords: Chronic obstructive pulmonary disease, diffusion capacity, yoga
INTRODUCTION
According to the global burden of disease study, COPD will be the fifth leading cause of disability and the third leading cause of death in the world in the first half of the twenty-first century. For developing countries, COPD is expected to be the fourth leading cause of disability for males and the third for females in 2020.[1]
Chronic obstructive pulmonary disease (COPD) has been defined by the global initiative for obstructive lung disease (GOLD) as a disease state characterized by airflow limitation that is not fully reversible.[2]
Dyspnoea, the hallmark symptom of COPD, is the reason for which most patients seek medical attention and is a major cause of disability and anxiety associated with the disease. Chronic cough, often the first symptom of COPD, to develop.[3]
The diffusing capacity of lung for carbon monoxide (DLCO) is a measure of the ability of gas to transfer from the alveoli across the alveolar epithelium and the capillary endothelium to the RBCs. Gas exchange is impaired by parenchyma destruction, which disrupts the local matching of ventilation and perfusion.[4] The imbalance of ventilation perfusion may lead to alteration of transfer factor. It is usually due to a change in either or both the volume of blood in the alveolar capillaries and the diffusion capacity of alveolar capillary membrane. In chronic lung disease, diffusion capacity is impaired when there is a reduction in the effective surface area for gas exchange in lung, in disease of lung parenchyma in which there is loss of lung tissue or part of the lung, not ventilated.[5]
A comprehensive yoga program can have a salutary effect on general health and respiratory health and thereby help increase a person's ability to perform activities of daily living. COPD is known to increase the level of stress, emotional vulnerability, physical inactivity and muscle wasting. This yogic regimen may change the milieu at the bronchioles and the alveoli particularly at the alveolo-capillary membrane to facilitate diffusion and transport. Hence transfer factor of the lung for carbon monoxide (TLCO) has been included in this proposed study.
We have not come across any study regarding the effect of yogic exercises on transfer factor of lung for carbon monoxide; it was therefore decided to scientifically study the effects of yogic exercises in a group of COPD patients by measuring pulmonary function tests along with diffusion capacity.
MATERIALS AND METHODS
The study was conducted in University College of Medical Sciences (UCMS), Delhi on 60 diagnosed patients of mild (n=30) and moderate (n=30) COPD patients in the age group of 30-60 years, of either sex, having disease duration of more than one year. The patients were recruited from the medicine outpatient department (OPD) of Guru Teg Bahadur (GTB) hospital, Delhi. The diagnosis was based on three most common symptoms, namely, cough, sputum production and exertional dyspnoea.
Inclusion criteria for COPD patients of mild and moderate severity, according to GOLD guidelines: Mild ratio of forced expiratory volume in first second to forced vital capacity (FEV1/FVC)<70% and FEV1>80% predicted, moderate- FEV1/FVC<70% and FEV1=50-80% predicted. All patients remained on their prescribed medical treatment during the study. They were on regular conventional treatment with daily inhaled bronchodilator β2 agonist; salbutamol 100-200 μg at the interval of 6 h and inhaled anticholinergic; ipratropium bromide 40-80 μg at the interval of 6-8 h.
Subjects with a history of an exacerbation or respiratory tract infections, tuberculosis, current smokers, pregnant or lactating women, diabetes or any other disorder were excluded. The medication for COPD was kept the same throughout the study period for both control and the yoga group. The study was explained to the patients and their signed informed consent was taken. Ethical clearance was also obtained from UCMS ethical committee.
Selected patients were randomized into two groups:
![]()
Group 1 control group (n=30): This group was further subdivided according to severity:
Group 1a Mild COPD: This group was taking conventional treatment with inhaled bronchodilator β2 agonist, salbutamol 100-200 μg at an interval of 6 h.
Group 1b Moderate COPD: This group was taking conventional treatment with inhaled bronchodilator β2 agonist, salbutamol 100-200 μg at an interval of 6 h and inhaled anticholinergic, ipratropium bromide 40-80 μg at an interval of 6 h.
Group 2 Yoga group (n=30): These patients were taught pranayama and asanas and were asked to continue the same medication as group 3. This group was further subdivided according to severity.
Group 2a Mild COPD
Group 2b Moderate COPD
The training in yoga: The yoga practice given to COPD patients (for 2 months) included pranayama and asanas. Before putting the patients on yoga regimen, they were clinically examined to rule out any physical ailments. Patients were asked to perform yoga exercises for 40-50 min everyday for 2 months under the supervision and guidance of a yoga instructor. Yoga includes pranayama (30-35 min), asanas (10 min), meditation (10 min) and life style changes.
Pranayama (breathing exercises):[6]
Bhastrika: 5 min
Anulom vilom: 15 min
Kapalbhati: 10 min
Bhramari: 5 times
Asanas (postures):
Surya Namaskar
Tadasana
Sukhasana
Paschimotanasana
Shavasana: 10-20 min
Both the control group and yoga group were matched for age, sex and duration of asthma and COPD. All subjects underwent complete physical examination and clinical assessment. Routine laboratory tests (complete hemogram) were done at the time of commencement of the study. Patients were tested, instructed and followed up in cardiopulmonary laboratory of the Physiology department. Yoga group were explained about yoga and their lifestyle modifications. They were advised about the diet, in which more fruits and vegetables were included. They were instructed to avoid alcohol and smoking and to keep regular working and sleeping hours. Proper yoga training was given by yoga experts. Subsequently they performed yoga in the yoga clinic for 21 days for an average of 45 min daily. Thereafter, they were asked to practice yoga for 45 min daily at home. The subjects were followed in the cardiopulmonary laboratory, after each week, for an evaluation and compliance to see whether they were doing the yogic exercises properly. Subjects maintained daily records of their breathing exercises, asthma symptom severity during the day and night, plus activity limitations due to asthma. They were asked to note down if there was any change in the dose of their medications.
The control groups were also asked to maintain records of all events related to disease and medication use. Both the groups were regularly attended by their treating physicians during study evaluation visits. Both the groups filled the daily diary and brought it at each visit. During the follow up period, telephonic support was provided for motivating participants to improve their compliance. All the subjects were evaluated three times, first at the time of recruitment, then after one month and two months. Simultaneously they underwent either conventional treatment or conventional treatment with yogic intervention. The recorded parameters were compared, statistically analyzed and then concluded. All of the patients received the same yoga training.
Parameters
Standing height and weight of the patients were measured and body mass index (BMI) was calculated. Diffusion capacity was assessed prior to yoga training, at the end of 1 month and after 2 months of yoga therapy. It was carried out on each stable subject using computerized medisoft instrument (HYP‘AIR compact-manufacturer- PK MORGON). The patients were acclimatized to the laboratory for 10 min. The level of the mouth piece was adjusted so that the patient was comfortable. Adequate demonstration was given till the subject had comprehended the instructions. Diffusion capacity was carried out in the morning between 9:30 am and 11 am.
To make the measurement of transfer factor, the subject was seated upright in front of the apparatus; this is set so that the subject breathes air through the mouth piece. A nose clip was worn. After a few normal breaths, the subject breathed out to residual volume. Then immediately, the subjectrapidly inhaled the test gas to total lung capacity, held the breath for approximately 9-11 s and finally breathed out at a moderately fast rate. After exhalation, a sample of alveolar gas was collected for analysis.
By the method of Jones and Meade, the effective duration of breath holding is taken to include two- thirds of time of inspiration and the time of expiration up to half way through the period of sample collection.[7,8]
A total of 3 tests were performed and the best of the three fulfilling the criteria of reproducibility and vitality were considered for analysis.
The control group was told to continue the medicines, with no dietary restrictions or daily activities. They were also assessed for diffusion capacity at the time of recruitment, at the end of 1 month and after 2 months.
Data were collected, tabulated and analyzed using repeated measures of analysis of variance (ANOVA), followed by Tukey test with P<0.05 as statistically significant. Results are expressed as mean±standard deviation (SD).
RESULTS
The mean±SD for age in group 1a was 39.33±8.415 years and for group 2a was 46±9.449 years. The mean±SD for age in group 1b was 50.87±8.634 years and for group 2b was 52.47±8.911 years. The baseline parameters were comparable between the yoga and the control group of mild COPD patients and moderate patients (P>0.01 for all). Anthropometric variables (body surface area (BSA), body mass index (BMI) were found to be significantly different between group 2a and group 2b [Tables 1 and 2] (P<0.05).
Table 1.
Anthropometric variables in group 2a

Table 2.
Anthropometric variables in group 2b

Transfer factor of lung for carbon monoxide (TLCO) in group 2a and group 2b showed a statistically significant increasing trend over time from baseline to 1 month and baseline to 2 months (P<0.001) [Tables 3 and 4]. TLCO was higher in group 2a than in group 1a, but the differences were statistically not significant (P=0.443 [Table 3]. Also, TLCO was higher in group 2b than in group 1b, but the differences were statistically not significant (P=0.409) [Table 4].
Table 3.
Transfer factor of lung for carbon monoxide in group 1a and 2a
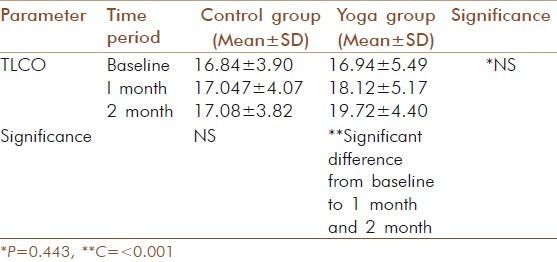
Table 4.
Transfer factor of lung for carbon monoxide in group 1b and 2b

DISCUSSION
In the present study, there was significant decrease in weight and body mass index after yoga. The values of TLCO showed a statistically significant improvement after two months of yoga training in mild as well as moderate COPD. Behera D studied the effect of yoga on COPD patients and showed that lung function parameters (forced vital capacity (FVC), forced expiratory volume in first second (FEV1)and peak expiratory flow rate(PEFR) improved after the practice of yoga.[9] COPD patients undergoing conventional drug treatment had no change in TLCO in COPD patients In the earlier stage of COPD a person's lung function may be impaired 20% to 30%. The progress of disease causes further impairment, which in turn increases inactivity. Inactivity itself may contribute to the deterioration of the lungs and the total musculature.[10] Yoga when practiced by patients with COPD results in improvement in their quality of life and lung function on a short-term basis.[11] Through proper breathing exercises more oxygen is available for the exchange at tissue level, in turn muscles throughout the body to do their job efficiently. Breathing exercises and stretching postures are used to increase respiratory stamina, relaxation of the chest muscles, expansion oflungs, raising energy levels and calming the body.[12]
Yoga improves the blood circulation; there is better perfusion of tissues also, which increases the strength of respiratory muscles. More oxygen binds with hemoglobin. So oxygen delivery increases. The further advantage of yogic breathing lies in the fact that it is more of a vertical breathing. By this vertical breathing, all the alveoli of both the lungs open up evenly. Due to the even expansion of all the alveoli, a vast expanse of alveolar membrane is available for exchange of gases. This surface is about 50 m2 in extent, which is 20 times the entire body surface. The larger the surface available for the process of diffusion, the better is the process. The purpose of yoga breathing exercises is to supply the body with oxygen and cleanse it of carbon dioxide and other toxins. Generally, a small portion of lung capacity is been utilized. This inadequate supply of oxygen results in improper waste disposal from the body. The body functions are slowed down and the cells/tissues fail to regenerate themselves due to lack of sufficient energy.[6]
With pranayama practice, there can be an increased intake of oxygen as much as five times. This means five times of carbon dioxide is gottenrid from the body. There can be great improvement in the health by doing pranayama.
The controlled breathing in yoga can ease anxiety, achieve relaxation, and provide more oxygen to the blood stream. The exercises help open blocked airways caused by bronchitis or emphysema, which are linked to COPD, and improve the function of air circulation. Simple yoga moves can even aid those with advanced COPD.
Vedanathan has observed that one of the most important aspects of yoga for asthma and COPD patients is that “they develop an increased capacity to relax and control their breathing. They learn that they don’t have to let their breathing control and that they can take charge of their breathing.” As with any technique, they emphasize that yoga requires regular practice in order to be effective.[13]
Pranayama, asana and meditation, through external signals (five sense organs) and internal signals (proprioreceptors, visceroceptors and chemoceptors) modulate the brain's cortico-limbic-hypothalamic systems and provide beneficial effects due to better functional coupling of ‘autonomic, endocrine and somatic’ responses. This could be correlated with homeostatic responses set up to negate the undesirable effects of stress.
CONCLUSION
We conclude that yoga, especially the pranayamic breathing exercises when used adjunctively with standard pharmacological treatment, can significantly improve TLCO in yoga with mild-to-moderate grades of COPD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global burden of disease study. Lancet. 1997;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 2.Bethesda, MD: National Institutes of Health; 2006. Global initiative for chronic obstructive lung disease, Global strategy for the diagnosis, management and prevention of COPD: NHLBI/WHO workshop report; pp. 5–6. [Google Scholar]
- 3.Georgopoulas D, Anthonisen NR. Symptoms and signs of COPD. In: Cherniack NS, editor. Chronic obstructive pulmonary disease. Toronto, ON, Canada: W.B. Saunders; 1991. pp. 357–63. [Google Scholar]
- 4.Boon A, Colledge R, Walker R, Hunter A, editors. Principles and Practice of Medicine. 20th ed. Edinburgh: Churchill Livingstone Publication; 2006. Davidson's Respiratory Disease; pp. 650–6. [Google Scholar]
- 5.Mc Lean A, Warren PM, Gillooly M, MacNee W, Lamb D. Microscopic and macroscopic measurements of emphysema relation to carbon monoxide gas transfer. Thorax. 1992;47:147–9. doi: 10.1136/thx.47.3.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rai L. A physiological approach to yoga. Gurgaon. India: Anubhav Rai publishers; 1996. Discovering human potential energy: Health, stress, illness, lifestyle and disease reversal. [Google Scholar]
- 7.West JB, Fowler KT, Jones P. Measurement of the ventilation perfusion ratio inequality in the lung by the analysis of a single expirate. Clin Sci. 1957;16:529–47. [PubMed] [Google Scholar]
- 8.Meade F, Pearl N, Sauders MJ. Distribution of lung function (Va/Q) in normal subjects deduced from changes in alveolar gas tension during expiration. Scand J Respir Dis. 1967;48:354–65. [Google Scholar]
- 9.Behera D. Yoga therapy in chronic bronchitis. J Assoc Physicians India. 1998;46:207–8. [PubMed] [Google Scholar]
- 10.Sharma V. Yoga and COPD. Published in yoga studies. International association of yoga. 2004 [Google Scholar]
- 11.Pomidori L, Campigotto F, Amatya TM, Bernardi L, Cogo A. Efficacy and tolerability of yoga breathing in patients with chronic obstructive pulmonary disease: A pilot study. J Cardiopulm Rehabil Prev. 2009;29:133–7. doi: 10.1097/HCR.0b013e31819a0227. [DOI] [PubMed] [Google Scholar]
- 12.Jonas WB. Alternative medicine: Learning from the past, examining the present, advancing to the future. JAMA. 1998;280:1616. doi: 10.1001/jama.280.18.1616. [DOI] [PubMed] [Google Scholar]
- 13.Vedanathan PK. Program and abstracts of the 94th International Conference of the American Thoracic Society. San Diego: 1998. Apr 23-28, Yoga breathing techniques in COPD: A preliminary study. D31; Poster A132. [Google Scholar]


