Abstract
Objective:
To assess the efficacy of a short-term comprehensive yoga-based lifestyle intervention in reducing anxiety, improving subjective well-being and personality.
Materials and Methods:
The study is a part of an ongoing larger study at a tertiary care hospital. Participants (n=90) included patients with chronic diseases attending a 10-day, yoga-based lifestyle intervention program for prevention and management of chronic diseases, and healthy controls (n=45) not attending any such intervention.
Primary Outcome Measures:
Change in state and trait anxiety questionnaire (STAI-Y; 40 items), subjective well-being inventory (SUBI; 40 items), and neuroticism extraversion openness to experience five factor personality inventory revised (NEO-FF PI-R; 60 items) at the end of intervention.
Results:
Following intervention, the STAI-Y scores reduced significantly (P<0.001) at Day 10 (66.7 ± 13.0) versus Day 1 (72.5 ± 14.7). Also, positive SUBI scores (F1– F6) improved significantly (P<0.01) at Day 10 versus Day 1. Similarly NEO-FF PI-R scores improved significantly (P<0.001) at Day 10 versus Day 1. Control group showed an increase in STAI-Y while SUBI and NEO-FF PI-R scores remained comparable at Day 10 versus Day 1.
Conclusions:
The observations suggest that a short-term, yoga-based lifestyle intervention may significantly reduce anxiety and improve subjective well-being and personality in patients with chronic diseases.
Keywords: Anxiety, personality, short-term yoga-based lifestyle intervention, stress, subjective well-being
INTRODUCTION
Anxiety, stress, diminished feeling of well-being and altered personality are associated with most of the chronic diseases including diabetes, heart diseases, respiratory diseases, and psychiatric disorders, and often result in a compromised treatment and poor quality of life.[1–7] Recent reports have demonstrated that mental health is an important predictor of health outcomes, and hence maintaining a good mental health and positive personality is of prime concern in patients with chronic diseases.[8,9] Yoga[10] and psychoneuroimmunology are two such potential intervention modules of alternative and complementary medicine that are emerging as foundations of mind-body medicine.[11] We have previously shown that this short-term lifestyle intervention is effective in reducing oxidative stress,[12] fasting glucose, and improving lipid profile as early as 10 days.[13]
Though health-related quality of life is generally used to measure overall well-being of an individual, a self-evaluation of health status, levels of anxiety[5] and personality traits[14] can also predict mortality and treatment outcomes, sometimes better than that predicted by current health status or other risk factors.[15–17] This might be important, especially in case of lifestyle-related diseases[18] and may provide important clinical information. However, only a few studies have evaluated the association between lifestyle and self-rated mental and physical health in a general population[19–22] or patients with other lifestyle-related diseases. Therefore, we conducted the current study with an aim to assess the improvement in state and trait anxiety, subjective well-being, and personality traits in patients with various chronic diseases following a pretested short-term, yoga-based lifestyle intervention program.
MATERIALS AND METHODS
Participants
Subjects (n=90, 46 male and 44 female; mean age 41.37 ± 13.91 years) with diabetes, hypertension, asthma, musculoskeletal-pain, mental stress, mild psychiatric disorders (depression, anxiety) visiting the outpatient clinics and overweight subjects who wished to join the program for weight loss and fitness were included in the study. The main inclusion criteria were that subjects were able to perform basic yoga postures and were willing to comply with the study intervention program at Integral Health Clinic (IHC), Department of Physiology, All India Institute of Medical Sciences, New Delhi, India. Physically challenged subjects were excluded from the study. The control group included 45 healthy subjects (24 male, 21 female; mean age 39.26 ± 9.38 years) who had not attended any such program in the last one year, and were recruited from amongst the hospital staff and patients’ attendants. The aim of including a control group was only to see the natural variation in anxiety levels, subjective well-being and any change in personality traits within 10 days and was therefore not age- and sex-matched.
Study design
All the participants attended a 10-day lifestyle-intervention program as an outpatient facility and were not required to be admitted. State and trait anxiety, subjective well-being, and personality traits were assessed at baseline, i.e. Day 1 and at the end of intervention i.e. Day 10. The same assessments were also done for control group within the 10-day window period in order to see the natural variation occurring in these parameters without any intervention.
The study was conducted in accordance with the Declaration of Helsinki and was approved by the appropriate local ethics committee and Institutional Review Board. All patients provided their informed consent. The trial was registered at Clinical Trial Registry India (CTRI), CTRI/2009/091/000727.
Lifestyle intervention program
This was a comprehensive, yoga-based intervention program, 2 h each day for 10 days. It consisted of an integrated and pretested intervention[12,13] comprising of theory and practice sessions. To ensure the quality of the program and to ensure that participants get enough time with the experts, only 6-8 participants were assigned to the program at a time. A typical day in the program started with a set of simple asanas (physical postures) and pranayama (breathing exercises) for approximately 1 h. This was followed by lectures and group discussions regarding disease-specific lifestyle measures, efforts to minimize or eliminate substance abuse and basics of calming practices. Special focus was laid on coping with stress and anxiety. Nutrition awareness program was also included; however, providing meals was not a part of the program. Questions and unstructured discussions were encouraged among the participants. Each day's program ended with relaxation through either shavasana (a relaxation technique) or meditation. Spouse and other members of the participant's family were encouraged to attend the program in order to facilitate compliance. The structure of this lifestyle intervention program has been published previously.[13]
Assessment of state and trait anxiety
The state and trait anxiety was assessed by using “State and Trait Inventory-Y 1 and 2” (STAI-Y), which is a validated tool devised by Spielberger.[23] This is a self-report assessment device which includes separate measures of state and trait anxiety. State anxiety reflects a transitory emotional state characterized by subjective, consciously perceived feelings of tension and apprehension, and heightened autonomic nervous system activity. State anxiety may fluctuate over time and can vary in intensity. In contrast, trait anxiety denotes a relatively stable individual difference in anxiety proneness and refers to a general tendency to respond with anxiety to perceive threats in the environment.
Assessment of subjective well-being
The subjective well-being was assessed using a validated ‘subjective well-being inventory’[24] (SUBI). This is a self-report assessment device, which measures the degree of subjective well-being of an individual in various day-to-day life concerns.
Assessment of change in personality
The personality was assessed by using neuroticism extraversion openness to experience five factor personality inventory revised (NEO-FF PI-R), a validated tool.[25] The shortened 60-item NEO-FF PI-R provides a quick reliable and accurate measure of the five domains of adult personality. It is a concise measure of the five domains of personality and the six traits or facets that define each domain: Neuroticism (anxiety, hostility, depression, self-consciousness, impulsiveness, vulnerability); extraversion (gregariousness, assertiveness, activity, excitement-seeking, positive emotions); openness (openness to experience, feelings, actions, ideas, values); agreeableness (trust, modesty, compliance, straightforwardness, tender-mindedness); conscientiousness (competence, self-discipline, achievement, dutifulness, deliberation).
Statistical analysis
The STAI-Y scores, SUBI scores and NEO-FF PI-R scores on Day 1 and Day 10 were compared by Student's t-test for paired observations. As a part of exploratory analysis, control group was included to see the natural variation in subjective well-being, anxiety levels and personality traits; however, a comparison between the two groups was not done.
RESULTS
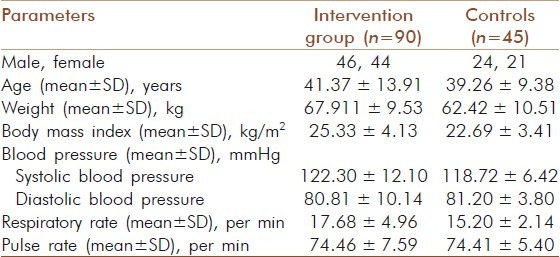
The study included 90 participants (46 male, 44 female; age 41.37 ± 13.91 years) in the intervention group and 45 subjects (24 male, 21 female; age 39.26 ± 9.38 years) in the control group [Table 1]. Of these 90 participants, 27 were overweight, 15 had diabetes, 17 had psychological disorders, 14 had hypertension, 9 had musculoskeletal pain, and 4 each had asthma and constipation.
Table 1.
Baseline parameters
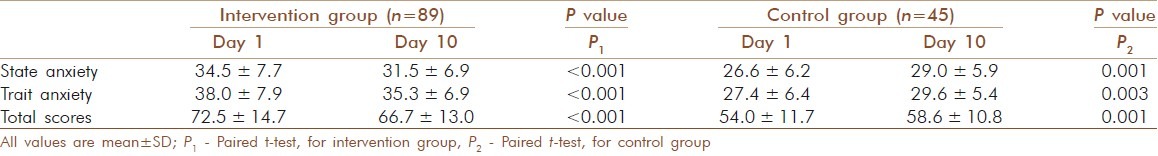
The level of state and trait anxiety, both decreased significantly (P<0.001) following the lifestyle intervention, and the overall anxiety scores were also significantly lower at Day 10 versus Day 1 [Table 2]. However, in the control group, the state and trait anxiety scores increased significantly by Day 10 as compared to Day 1 [Table 2].
Table 2.
State and trait anxiety questionnaire scores in the intervention and control groups at day 1 and day 10
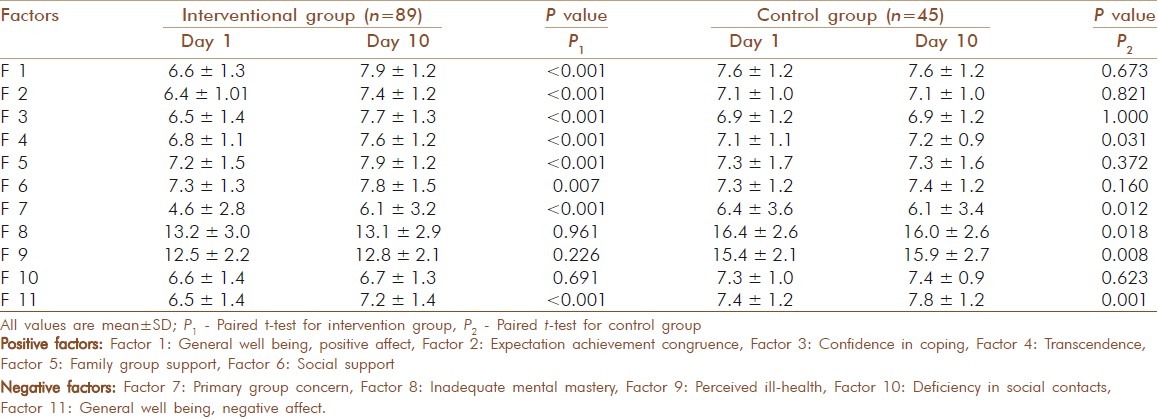
Regarding the SUBI scores, following the lifestyle intervention, participants showed a significant improvement in all the positive factors (F1 to F6) from Day 1 to Day 10 [Table 3]. For the negative factors, Factor 11 (general well-being negative affect) showed a significant decrease from Day 1 to Day 10 following lifestyle intervention while there was no notable change in Factors 8, 9 and 10. Surprisingly primary group concern (Factor 8) showed a further worsening [Table 3]. In the control group, the positive factors remained comparable except for Factor 4, which showed significant improvement. Regarding the negative factors, in a 10 day period, Factors 7 and 8 showed significant decrease while Factors 9 and 11 showed significant increase [Table 3].
Table 3.
Subjective sense of well.being inventory scores in the intervention and control groups at day 1 and day 10
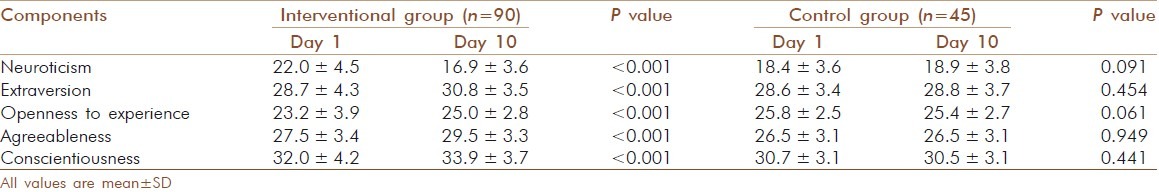
The NEO-FF PI-R personality assessment showed a significant improvement in personality by decreased scores for neuroticism (P<0.001), and increased (P<0.001) scores for extraversion, openness to experience, agreeableness, and conscientiousness [Table 4]. The control group did not show any changes in personality within 10 days.
Table 4.
Neuroticism extraversion openness to experience five factor personality inventory revised (NEO.FF PI.R) scores in the intervention and control groups at day 1 and day 10
DISCUSSION
The intervention in this study was a comprehensive short-term, yoga-based lifestyle intervention comprised of simple physical exercises, relaxation techniques, stress management, diet and other aspects of lifestyle. The results showed that even a short-term lifestyle intervention reduced anxiety levels, improved personality and to an extent enhanced subjective well-being. This benefit, especially when achieved within a short time frame, appears promising because patient compliance becomes higher with shorter period of their engagement with the hospital/clinic and hence increases the clinical utility of the intervention. These benefits were spread over a wide range of chronic diseases, which implies that lifestyle intervention has an efficacy regardless of specific diagnosis as shown previously by other studies.[26–29]
Anxiety is known to aggravate ill health and also reduces the efficacy of medical or surgical treatment.[1–7] Therefore, reducing anxiety in these patients may not only improve the quality of life but also improve the treatment efficacy. The present study demonstrated a significant reduction in anxiety following a simple yoga-based lifestyle intervention. These findings are similar to those observed in previous studies that showed a significant decrease in the trait anxiety scores following meditation[30–36] and breathing exercises as the relaxation techniques; and in state anxiety following muscle relaxation techniques and listening to music.[37] Further, there was a clinical improvement in patients with chronic neck pain following a yoga-based intervention.[38] Together these findings suggest that reducing anxiety is beneficial in improving clinical profile as well as enhancing the efficacy of treatment offered to these patients.
Regarding subjective well-being, all individual factors of the SUBI scoring system, the general well-being (F1), expectation achievement congruence (F2), confidence in coping (F3) and transcendence (F4) showed improvement in these patients as well as those who were overweight. These factors together indicate an improvement in feeling of success, satisfaction for achievements in life, and confidence in coping with crisis. Other parameters of SUBI scores like family group support, and social support also showed an improvement. Consistent with these findings, the negative factors of SUBI scores like general well-being negative effect (F11) showed a reduction, indicating a positive effect of intervention. These results are in-line with previous studies where a beneficial effect of yoga was observed on various physiological and psychological parameters.[39] However, the subjective well-being is largely culturally oriented and the results of the present study can be therefore compared to the studies in Indian patients only. A previous study which evaluated change in SUBI scores after four months of yogic practices in healthy subjects did not show any significant changes for family group support and social group support (Factors 5 and 6).[40] We observed a significant improvement in the general well-being negative affect (Factor 11), which is contradictory to a previous study with a yogic intervention.[41] The results of current study support our previous findings where this short-term lifestyle intervention was effective in reducing oxidative stress,[12] and also improved serum lipid profile and fasting plasma glucose.[13] This study therefore re-emphasizes the benefits of a short-term, yoga-based lifestyle intervention program.
Though alteration of personality is most marked in psychological disorders,[42] other chronic diseases also result in altered personality traits[43,44] and personality has a known effect on managing self-rated health[45] as well as clinical outcome.[46] Further, high neuroticism and low conscientiousness are known to be associated with inflammation and interleukin-6.[47] This suggests that a reduction in neuroticism not only improves the personality but may also reduce inflammation, which is a hallmark of these lifestyle-related diseases. The “Five Factor” model used to assess personality in this study is known to provide a valid assessment, captures the major axes of psychological and behavioral variation in humans and is associated with an array of important health behaviors and outcomes.[48,49] Overall, the present study demonstrated that there was a positive change in the personality of these subjects, which may reflect not only a better quality of life, but also a positive outlook, improved self-rated health and a possible enhancement of medical treatment as shown in a previous study including patients with diabetes.[50] In the control group, it was observed that anxiety increased significantly, subjective well-being changes remained inconclusive while personality traits remained unaffected at Day 10 versus Day 1.
There were certain limitations in this study. Firstly, this was not a randomized controlled trial. The control group was included with an intention to see if there is any measurable difference in a time period as short as 10 days without any intervention. Secondly, the medical treatment outcome could not be related to the reduction in anxiety, improvement in subjective well-being and personality. Thirdly, the intervention group was a heterogeneous group of patients with different chronic diseases. Despite these, the results of this study are in line with the previous studies where lifestyle and stress management programs were beneficial irrespective of the diagnosis.[22] This further supports the importance and efficacy of a short-term, yoga-based lifestyle intervention as we have shown in our previous studies.[12,13]
Overall, the results of the present study suggest that the yoga-based lifestyle intervention program caused a significant reduction in state and trait anxiety levels, had a favorable effect on subjective well-being and significantly improved the five facets of personality even in a short-time period. Since lifestyle is an integrated entity, a yoga-based intervention, which aims at influencing the total lifestyle, has much in favor as compared to changing only one aspect of lifestyle at a time hence resulting in an increased efficacy and compliance.
ACKNOWLEDGMENT
The authors are thankful and grateful to Drs. R. Sharma and A Talwar for their contribution and support to run the regular programs at the Integral Health Clinic, Department. of Physiology, AIIMS, New Delhi, India.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Huang CJ, Chiu HC, Lee MH, Wang SY. Prevalence and incidence of anxiety disorders in diabetic patients: A national population-based cohort study. Gen Hosp Psychiatry. 2011;33:8–15. doi: 10.1016/j.genhosppsych.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Sanz J, García-Vera MP, Espinosa R, Fortún M, Magán I, Segura J. Psychological factors associated with poor hypertension control: Differences in personality and stress between patients with controlled and uncontrolled hypertension. Psychol Rep. 2010;107:923–38. doi: 10.2466/09.15.20.PR0.107.6.923-938. [DOI] [PubMed] [Google Scholar]
- 3.Fiedorowicz JG, He J, Merikangas KR. The association between mood and anxiety disorders with vascular diseases and risk factors in a nationally representative sample. J Psychosom Res. 2011;70:145–54. doi: 10.1016/j.jpsychores.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martínez-Rivera C, Vennera MD, Cañete C, Bardagí S, Picado C. Psychological profile of patients with bronchial asthma and functional dyspnea: A comparison with a non-asthmatic population and impact on the disease. Arch Bronconeumol. 2011;47:73–8. doi: 10.1016/j.arbres.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Mertens MC, Roukema JA, Scholtes VP, De Vries J. Trait anxiety predicts unsuccessful surgery in gallstone disease. Psychosom Med. 2010;72:198–205. doi: 10.1097/PSY.0b013e3181cb65b4. [DOI] [PubMed] [Google Scholar]
- 6.Huffman JC, Smith FA, Blais MA, Januzzi JL, Fricchione GL. Anxiety, independent of depressive symptoms, is associated with in-hospital cardiac complications after acute myocardial infarction. J Psychosom Res. 2008;65:557–63. doi: 10.1016/j.jpsychores.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Ryu YJ, Chun EM, Lee JH, Chang JH. Prevalence of depression and anxiety in outpatients with chronic airway lung disease. Korean J Intern Med. 2010;25:51–7. doi: 10.3904/kjim.2010.25.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boe HJ, Holgersen KH, Holen A. Mental health outcomes and predictors of chronic disorders after the North Sea oil rig disaster: 27-year longitudinal follow-up study. J Nerv Ment Dis. 2011;199:49–54. doi: 10.1097/NMD.0b013e31820446a8. [DOI] [PubMed] [Google Scholar]
- 9.Möller-Leimkühler AM, Mädger F. Personality factors and mental health outcome in caregivers of first hospitalized schizophrenic and depressed patients: 2-year follow-up results. Eur Arch Psychiatry Clin Neurosci. 2010;261:165–72. doi: 10.1007/s00406-010-0155-5. [DOI] [PubMed] [Google Scholar]
- 10.Barrows KA, Jacobs BP. Mind-body medicine.An introduction and review of the literature. Med Clin North Am. 2002;86:11–31. doi: 10.1016/s0025-7125(03)00069-5. [DOI] [PubMed] [Google Scholar]
- 11.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annu Rev Psychol. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- 12.Yadav RK, Ray BR, Vempati R, Bijlani RL. Effect of a comprehensive yoga-based lifestyle modification program on lipid peroxidation. Indian J Physiol Pharmacol. 2005;49:358–62. [PubMed] [Google Scholar]
- 13.Bijlani RL, Vempati RP, Yadav RK, Ray RB, Gupta V, Sharma R, et al. A brief but comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med. 2005;11:267–74. doi: 10.1089/acm.2005.11.267. [DOI] [PubMed] [Google Scholar]
- 14.Auerbach SM, Clore JN, Kiesler DJ, Orr T, Pegg PO, Quick BG, et al. Relation of diabetic patients’ health-related control appraisals and physician-patient interpersonal impacts to patients’ metabolic control and satisfaction with treatment. J Behav Med. 2002;25:17–31. doi: 10.1023/a:1013585617303. [DOI] [PubMed] [Google Scholar]
- 15.Idler EL, Kasl S. Health perceptions and survival: Do global evaluations of health status really predict mortality? J Gerontol. 1991;46:S55–65. doi: 10.1093/geronj/46.2.s55. [DOI] [PubMed] [Google Scholar]
- 16.McGee HM, Hevey D, Horgan JH. Psychosocial outcome assessments for use in cardiac rehabilitation service evaluation: A 10-year systematic review. Soc Sci Med. 1999;48:1373–93. doi: 10.1016/s0277-9536(98)00428-6. [DOI] [PubMed] [Google Scholar]
- 17.Halford C, Ekselius L, Anderzen I, Arnetz B, Svärdsudd K. Self-rated health, life-style, and psychoendocrine measures of stress in healthy adult women. Ups J Med Sci. 2010;115:266–74. doi: 10.3109/03009734.2010.496910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benjamins MR, Hummer RA, Eberstein IW, Nam CB. Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Soc Sci Med. 2004;59:1297–306. doi: 10.1016/j.socscimed.2003.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Kruger J, Bowles HR, Jones DA, Ainsworth BE, Kohl HW., 3rd Health-related quality of life, BMI and physical activity among US adults (>/=18 years): National Physical Activity and Weight Loss Survey, 2002. Int J Obes (Lond) 2007;31:321–7. doi: 10.1038/sj.ijo.0803386. [DOI] [PubMed] [Google Scholar]
- 20.Riise T, Moen BE, Nortvedt MW. Occupation, lifestyle factors and health-related quality of life: The Hordaland Health Study. J Occup Environ Med. 2003;45:324–32. doi: 10.1097/01.jom.0000052965.43131.c3. [DOI] [PubMed] [Google Scholar]
- 21.Van Dijk AP, Toet J, Verdurmen JE. The relationship between health-related quality of life and two measures of alcohol consumption. J Stud Alcohol. 2004;65:241–9. doi: 10.15288/jsa.2004.65.241. [DOI] [PubMed] [Google Scholar]
- 22.Wendel-Vos GC, Schuit AJ, Tijhuis MA, Kromhout D. Leisure time physical activity and health-related quality of life: Cross-sectional and longitudinal associations. Qual Life Res. 2004;13:667–77. doi: 10.1023/B:QURE.0000021313.51397.33. [DOI] [PubMed] [Google Scholar]
- 23.Spielberger CD, Gorusch RL, Lushene RE. Palo Alto, CA: Consulting Psychologists Press; 1970. STAI Manual for State-Trait Anxiety Inventory. [Google Scholar]
- 24.Sell H, Nagpal R. New Delhi: World Health Organization; 1992. Assessment of subjective well-being. [Google Scholar]
- 25.Costa PT, Jr, McCrae RR. Odessa, FL: Psychological Assessment Resources Inc; 1992. NEO PI-R Professional Manual: Revised NEO Personality Inventory and NEO Five-Factor Inventory. [Google Scholar]
- 26.Dongbo F, Fu H, McGowan P, Shen Y, Zhu L, Yang H, et al. Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: Randomized controlled trial. Bull World Health Organ. 2003;81:174–82. [PMC free article] [PubMed] [Google Scholar]
- 27.Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomised controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease. Br J Gen Pract. 2005;55:831–7. [PMC free article] [PubMed] [Google Scholar]
- 28.Lorig KR, Sobel DS, Stewart AL, Brown BW, Jr, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Med Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Swerissen H, Belfrage J, Weeks A, Jordan L, Walker C, Furler J, et al. A randomised control trial of a self-management program for people with a chronic illness from Vietnamese, Chinese, Italian and Greek backgrounds. Patient Educ Couns. 2006;64:360–8. doi: 10.1016/j.pec.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 30.Eppley KR, Abrams AI, Shear J. Differential effects of relaxation techniques on trait anxiety: A meta-analysis. J Clin Psychol. 1989;45:957–74. doi: 10.1002/1097-4679(198911)45:6<957::aid-jclp2270450622>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 31.Telles S, Gaur V, Balkrishna A. Effect of a yoga practice session and a yoga theory session on state anxiety. Percept Mot Skills. 2009;109:924–30. doi: 10.2466/pms.109.3.924-930. [DOI] [PubMed] [Google Scholar]
- 32.Brown RP, Gerbarg PL. Sudarshan kriya yogic breathing in the treatment of stress, anxiety, and depression part 1-neurophysiological model. J Altern Complement Med. 2005;11:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 33.Gupta N, Khera S, Vempati RP, Sharma R, Bijlani RL. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50:41–7. [PubMed] [Google Scholar]
- 34.Gross CR, Kreitzer MJ, Thomas W, Reilly-Spong M, Cramer-Bornemann M, Nyman JA, et al. Mindfulness-based stress reduction for solid organ transplant recipients: A randomized controlled trial. Altern Ther Health Med. 2010;16:30–8. [PMC free article] [PubMed] [Google Scholar]
- 35.Subramanya P, Telles S. Effect of two yoga-based relaxation techniques on memory scores and state anxiety. Biopsychosoc Med. 2009;3:8. doi: 10.1186/1751-0759-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rao MR, Raghuram N, Nagendra HR, Gopinath KS, Srinath BS, Diwakar RB, et al. Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: A randomized controlled trial. Complement Ther Med. 2009;17:1–8. doi: 10.1016/j.ctim.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 37.Stoudenmire JA. Comparison of muscle relaxation training and music in the reduction of state and trait anxiety. J Clin Psychol. 1975;31:490–2. doi: 10.1002/1097-4679(197507)31:3<490::aid-jclp2270310328>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 38.Yogitha B, Nagarathna R, John E, Nagendra H. Complimentary effect of yogic sound resonance relaxation technique in patients with common neck pain. Int J Yoga. 2010;3:18–25. doi: 10.4103/0973-6131.66774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Udupa KN, Singh RH, Yadav RA. Certain studies on psychological and biochemical response to the practice of Hatha Yoga in young normal volunteers. Indian J Med Res. 1973;61:237–44. [PubMed] [Google Scholar]
- 40.Malathi A, Damodaran A, Shah N, Patil N, Maratha S. Effects of yogic practices on subjective well being. Indian J Physiol Pharmacol. 2000;44:202–6. [PubMed] [Google Scholar]
- 41.Sharma R, Gupta N, Bijlani RL. Effect of yoga based lifestyle intervention on subjective well being. Indian J Physiol Pharmacol. 2008;52:123–31. [PubMed] [Google Scholar]
- 42.Gurrera RJ, Nestor PG, O’Donnell BF, Rosenberg V, McCarley RW. Personality differences in schizophrenia are related to performance on neuropsychological tasks. J Nerv Ment Dis. 2005;193:714–21. doi: 10.1097/01.nmd.0000185938.30783.6b. [DOI] [PubMed] [Google Scholar]
- 43.Fernandes L, Fonseca J, Rodrigues J, Vaz M, Almeida J, Winck C, et al. Personality characteristics of asthma patients. Rev Port Pneumol. 2005;11:7–34. doi: 10.1016/s0873-2159(15)30481-5. [DOI] [PubMed] [Google Scholar]
- 44.Tanum L, Malt UF. Personality and physical symptoms in nonpsychiatric patients with functional gastrointestinal disorder. J Psychosom Res. 2001;50:139–46. doi: 10.1016/s0022-3999(00)00219-1. [DOI] [PubMed] [Google Scholar]
- 45.Jerant A, Chapman B, Duberstein P, Franks P. Effects of personality on self-rated health in a 1-year randomized controlled trial of chronic illness self-management. Br J Health Psychol. 2010;15:321–35. doi: 10.1348/135910709X464353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Auerbach SM, Clore JN, Kiesler DJ, Orr T, Pegg PO, Quick BG, et al. Relation of diabetic patients’ health-related control appraisals and physician-patient interpersonal impacts to patients’ metabolic control and satisfaction with treatment. J Behav Med. 2002;25:17–31. doi: 10.1023/a:1013585617303. [DOI] [PubMed] [Google Scholar]
- 47.Sutin AR, Terracciano A, Deiana B, Naitza S, Ferrucci L, Uda M, et al. High neuroticism and low conscientiousness are associated with interleukin-6. Psychol Med. 2010;40:1485–93. doi: 10.1017/S0033291709992029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychol Bull. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- 49.Chapman B, Duberstein P, Lyness JM. Personality traits, education, and health-related quality of life among older adult primary care patients. J Gerontol B Psychol Sci Soc Sci. 2007;62:343–52. doi: 10.1093/geronb/62.6.p343. [DOI] [PubMed] [Google Scholar]
- 50.Lane JD, McCaskill CC, Williams PG, Parekh PI, Feinglos MN, Surwit RS. Personality correlates of glycemic control in type 2 diabetes. Diabetes Care. 2000;23:1321–5. doi: 10.2337/diacare.23.9.1321. [DOI] [PubMed] [Google Scholar]


