Abstract
Falls are among the most common problems affecting older adults. At least 50% of those over the age of 80 fall annually. The goal of this pilot study was to assess the safety and feasibility of structured yoga in an elderly population with fall risk. Seniors at risk for falls were identified and enrolled in a single arm pilot trial. A chair based yoga program was provided twice a week for 8 weeks. The program was designed from previously published pilot data. A battery of validated instruments was administered at baseline and week eight and was used to identify which instruments may be sensitive to change as a result of a yoga program. Among sixteen seniors (median age of 88) with a previous history of falls, 87% provided data for assessment at the end of the intervention. Two patients withdrew, one due to a fall outside the institution and the other due to lack of time and interest. There were no adverse events during the yoga sessions. Paired-t tests compared pre-post changes and gains were noted in Fear of Falling (5.27 to 2.60; P = 0.029) and SPPB sit to stand subscale (0.31 to 1.00; P =.022). Improved trends were noted in anxiety and the timed up and go assessments. We found the modified chair-yoga program is safe and recruitment is feasible. Our data suggests that yoga may be beneficial in improving mobility and reducing fear of falling which warrants additional research via randomized controlled trial.
Keywords: Balance, fear of falling, function, seniors, yoga
INTRODUCTION
Falls are a leading cause of fatal and non-fatal injuries in older adults. At least 50% of those over the age of 80 fall annually.[1] Following a fall, an individual will present with an increased fear of falling and decrease in self-efficacy, often resulting in a sedentary lifestyle due to avoidance of activities that may lead to falling. Lack of exercise and daily activity leads to a decrease in balance proficiency, which has been identified as a key risk factor for falling.[2]
Physical activity and regular exercise have been shown to improve balance, prevent falls, and maintain physical function in older individuals.[3] Physical and social activity has been found to have emotional benefits, such as decreased fear of falling, increased confidence and independence in leaving their residence and partaking in more overall activity.[4] Given the benefits resulting from daily exercise in older adults, it is crucial to find safe and effective forms of activity.
Hatha yoga is a gentle form of exercise that has positive impact on physical, mental and emotional well being and also is a promising intervention for managing fear of falling and improving balance in older adults.[1] Research in this area is preliminary with few studies investigating the correlation between yoga, improvement of balance and the fear of falling in adults over the age of 65.[1] In order to bring this intervention to assisted living environments where many older adults are at risk for falls, an understanding of the safety and feasibility is critically needed before launching larger scale research. Thus, our research aimed at assessing the safety and feasibility of a structured yoga program in an elderly population with fall risk.
MATERIALS AND METHODS
Study patient population
The protocol for this study was approved by the Institutional Review Board at Richard Stockton College of New Jersey. Eligible participants were over 65 years of age from an assisted living community, who experienced a fall in the past 6 months and an increased fear of falling as a result, had an increased risk of falls identified by the physical therapy or nursing staff, and gave written consent to adhere to all study procedures. Participants were excluded if they had a diagnosis of Alzheimer's disease or were unable to weight bear on upper extremities.
Study intervention
This protocol was designed with mobility and balance concerns in mind, thus the yoga centered on asanas (postures) that benefit the musculoskeletal system. Mirrored from previous research in the use of yoga for osteoarthritis,[5] the protocol includes particular asanas performed under the instruction of certified yoga instructors.
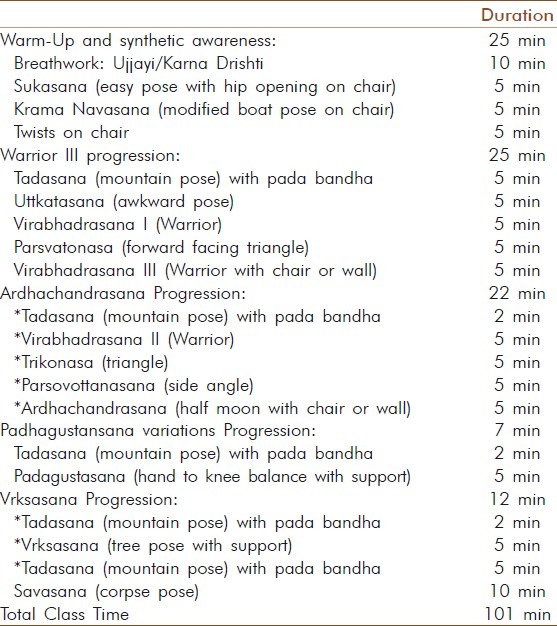
Yoga classes met twice per week for 8 weeks at the assisted living facility. Residents participated in the yoga sessions from a chair and were given the appropriate props when indicated. Participants received 60minutes of structured yoga as shown in Table 1. Yoga was the only intervention the participants received during the 8 week period for balance and fall reduction.
Table 1.
Yoga class structure and components
Data collection and outcome measurement
Rater assessed functional outcomes:
Timed Up and Go (TUG)[6] and the Short Physical Performance Battery (SPPB)[7] were used to evaluate the mobility and function of the participants in this study. The TUG score of less than 12 s or less is a normal value for healthy elderly individuals.[8] In recent studies, participants’ TUG scores increased significantly with decreasing mobility.[8] Participants with times more than 12 s may warrant interventions directed at improving their strength, balance, and/or mobility.[6] The subscales of the SPPB test were scored individually. A composite SPPB score is the sum of each subscale score.[9] A score on the SPPB of 0 to 4 at hospital discharge increases risk of re-hospitalization or death. A score of 8 to 12 has shown to be predictive of a higher quality of life.[7]
The Berg Balance Scale (BBS), Functional Reach (FR),[10] and modified Sit and Reach (SR)[11,12] were intended to measure flexibility and balance. The Berg Balance Scale (BBS) is a commonly used scale to determine risk of falls in older adults.[13] If participants have a change in eight points, a genuine alteration in the balance of older people can be noted in their function.[14] For the FR, the participants who reach, at least 25.4cm are at lowest risk for falls, 15.2 to 25.4cm are two times more likely to fall than those beyond 25.4cm, and less than 15.2cm are four times more likely to fall than those beyond 25.4cm. People with no reach ability are eight times more likely to fall than those with a reach over 25.4cm.[15] The SR normative values for the age range of our population were -13.97cm to 1.27cm for males and -5.08cm to 6.35cm for females.[16] The risk for falls increases in males with a measurement greater than -10.16cm and for females greater than -5.08cm.[16]
Patient reported outcomes
Tinetti's Falls Efficacy Scale (TFES),[17] Hospital Anxiety and Depression Scale (HADS),[18] and Brief Pain Inventory (BPI)[19] were patient self-reported outcomes used to measure pre and post effects of the yoga intervention. Surveys were administered at baseline and at the end of the 8-week intervention. The TFES score greater than 80 suggests an increased risk of falling and a score greater than 70 suggests a fear of falling.[17] A HADS score of 0 to 7 for either the anxiety or depression subscale is within the normal range, a score of 8 to 10 is suggestive of the presence of anxiety or depression and a score of 11 or higher indicates probable presence of anxiety or depression.[20] The BPI scores range from mild to severe with 1-4 corresponding to “mild”, 5 -6 corresponding with “moderate”, and 7-10 corresponding with “severe”. These scores correlate with functional abilities in such a way that when the score increases so does the amount of functional activity that is affected.[19]
Statistical analysis
Data analysis was performed using SPSS 19.0. Descriptive statistics were performed in order to find trends among the findings. The functional and quality of life (QOL) outcomes measured at baseline and the completion of 8 week yoga intervention were analyzed using the paired t-test.
RESULTS
Patient characteristics
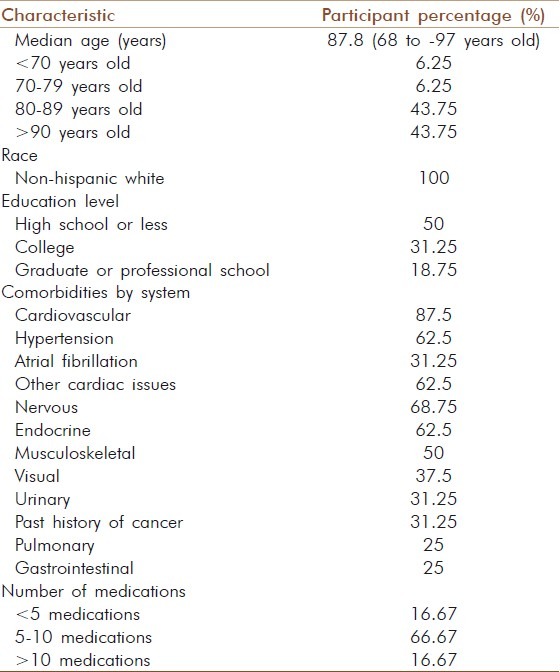
Twenty individuals with fall risk were offered participation in the yoga sessions. Sixteen seniors, four males and twelve females, were enrolled in the study (four required additional family consent not attained by the start of the study). Demographic and participant characteristics are noted in Table 2. Two patients withdrew, one due to a fall outside the institution and the other due to lack of time and interest. The mean age of the participants was 87.8 years old (68 to 97 years old). With the exception of one participant who is 68, all were in their ninth or tenth decade of life. They were all non-Hispanic white residents and retired with a high school or college education. At baseline, all participants were reliant on various types of assistive devices. Participants attended 50-90% of the yoga sessions.
Table 2.
Demographic and clinical characteristics of trial participants (N=16)
No adverse events took place during the yoga intervention; however there were falls outside the study. One participant fell outside of the assisted living facility, causing damage to vision and balance resulting in a slight regression from the baseline while another fell in his room.
Change in function and psychological perspectives
Table 3 provides the changes in mean scores in the various measures. Even with a small sample size, the scores fulfilled the normality assumptions for the paired t-test. From baseline to the end of the study, the participants improved in SPPB Sit to Stand Scale (0.31 to 0.93, P = .021) and reduction in TUG (22.57 to 18.97, P = 0.052) which indicate improved trends in mobility.
Table 3.
Change in function and other symptom outcomes (N = 16)
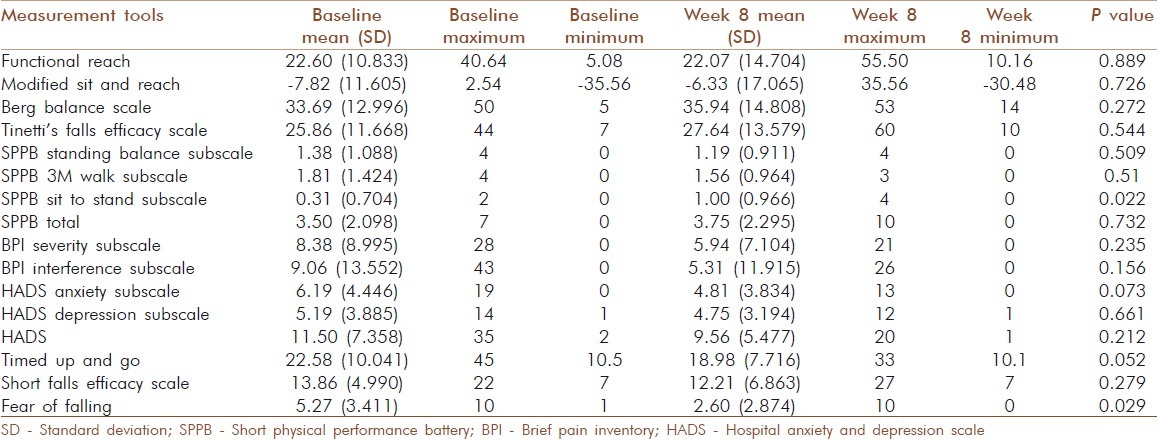
The HADS anxiety subscale showed a reduction from baseline (6.10 to 4.86, P=.072) and fear of falling (FOF) improved (5.27 to 2.60, P = 0.029). These trends are encouraging and may point to improved confidence in participants’ self efficacy in activities of daily living.
With these functional and psychological trends, less reliance on assistive devices for mobility in the community was noted. Three participants were able to eliminate the use of their assistive devices completely. However, while improved trends were noted in the FR, the seniors on average were below 25 cm for FR at the completion of the yoga intervention which indicates continued fall risk.
DISCUSSION
This preliminary research of a chair yoga based program in an assisted living community among 80 to 90 year old seniors is both feasible and safe. There is promising effects related to improved balance and mobility in this population that warrant additional research in randomized controlled trials. Ultimately, a critical examination of whether this intervention will prevent falls is needed to provide evidence for its integration into assisted living facilities and promote functional independence and healthy aging. The study duration deserves special attention since the FR scale indicated this population was still “at fall risk”. Future studies of greater than 8 weeks alongside a maintenance yoga based program may be indicated to foster sustainability of gains made in the acute yoga intervention.
A variety of studies have shown that exercise increases balance and QOL in seniors.[1–3,21] This study offers chair-based yoga as a potential intervention to increase balance and self efficacy, as noted by the SPPB sit to stand scale and FOF. Functional balance is an important characteristic as it represents the ability of the individual to complete activities of daily life. These may be measures that are of greater importance than those that measure stationary balance such as the FR.
There are several limitations to this study. The sample size of this pilot study was intended to develop the body of evidence to support further studies. The lack of a control group negates the ability to exclude the argument that the findings were caused by placebo, hawthorne effects or regression to the mean effect. It would be important to include a control group, utilize a larger sample size, and continue to develop sensitive measures that fit populations in assisted living communities.
There are potential benefits of mind-body techniques on function as yoga and meditation involves an active attentional or mindfulness component.[22] Research using Hatha yoga to determine impact on cognitive function, fatigue, mood and quality of life in seniors 65-85 years of age were randomized to yoga, exercise, and wait-list control groups. The yoga intervention produced improvements in physical measures as well as a number of quality-of-life measures related to sense of well-being, energy and fatigue compared to controls.[22] Our study suggests yoga may be a safe intervention with potential functional benefit for those in their 80's and 90's.
While the FR was difficult to administer to this population, it appears that FOF and SBBP may be most sensitive to change in older seniors. Octogenarians and nonagenarians represent a growing sector of the population and are increasingly drawn to yoga. This presents both an extraordinary opportunity and a serious challenge for yoga instructors who must be both resources and guardians of safety for this uniquely vulnerable group.[23] In any given class of seniors at this age level, various comorbidities and a diverse mix of abilities may be present. The majority will have at least one chronic health condition and half will have at least two. In our study each participant had on an average 3-5 health issues that required concurrent management and use of several medications [Table 2]. Our yoga sessions were based on principles of The Therapeutic Yoga for Seniors program and fulfill a critical need to help yoga instructors work safely and effectively with this population coming to yoga classes.[23] To provide a skillful framework for teaching yoga to seniors, specific principles of practice are important to ensure safety of this intervention.
CONCLUSION
This pilot study is the first to demonstrate that yoga is a feasible and safe intervention for elderly seniors who may be at risk for falls in their ninth and tenth decades of life. A randomized clinical trial is needed to establish the definitive efficacy of yoga for objective functional improvement in seniors with fall risk.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Schmid AA, Van Puymbroeck M, Koceja DM. Effect of a 12-week yoga intervention on fear of falling and balance in older adults: A pilot study. Arch Phys Med Rehabil. 2010;91:576–83. doi: 10.1016/j.apmr.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 2.Arnold CM, Sran MM, Harrison EL. Exercise for fall risk reduction in community-dwelling older adults: A systematic review. Physiother Can Fall. 2008;60:358–72. doi: 10.3138/physio.60.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lord SR, Castell S, Corcoran J, Dayhew J, Matters B, Shan A, et al. The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: A randomized, controlled trial. J Am Geriatr Soc. 2003;51:1685–92. doi: 10.1046/j.1532-5415.2003.51551.x. [DOI] [PubMed] [Google Scholar]
- 4.Kim S, Lockhart T, Roberto K. The effects of 8-week balance training or weight training: For the elderly on fear of falling measures and social activity levels. Qual Ageing. 2009;10:37–48. doi: 10.1108/14717794200900030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bukowski EL, Conway A, Glentz LA, Kurland K, Galantino ML. The effect of Iyengar yoga and strengthening exercises for people living with osteoarthritis of the knee: A case series. Int Q Community Health Edu. 2007;26:287–305. doi: 10.2190/IQ.26.3.f. [DOI] [PubMed] [Google Scholar]
- 6.Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29:64–8. doi: 10.1519/00139143-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Volpato S, Cavalieri M, Sioulis F, Guerra G, Maraldi C, Zuliani G, et al. Predictive value of the short physical performance battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011;66:89–96. doi: 10.1093/gerona/glq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bischoff HA, Stahelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, et al. Identifying a cut-off point for normal mobility: A comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32:315–20. doi: 10.1093/ageing/32.3.315. [DOI] [PubMed] [Google Scholar]
- 9.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 10.Wang CY, Sheu CF, Protas EJ. test-retest reliability and measurement errors of six mobility tests in the community-dwelling elderly. Asian J Gerontol Geriatr. 2009;4:8–13. [Google Scholar]
- 11.Tsang YL, Mak MK. Sit-and-reach test can predict mobility of patients recovering from acute stroke. Arch Phys Med Rehabil. 2004;85:94–8. doi: 10.1016/s0003-9993(03)00377-0. [DOI] [PubMed] [Google Scholar]
- 12.Baltaci G, Un N, Tunay V, Besler A, Gerceker S. Comparison of three different sit and reach tests for measurement of hamstring flexibility in female university students. Br J Sports Med. 2003;37:59–61. doi: 10.1136/bjsm.37.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kornetti DL, Fritz SL, Chiu YP, Light KE, Velozo CA. Rating scale analysis of the Berg Balance Scale. Arch Phys Med Rehabil. 2004;85:1128–35. doi: 10.1016/j.apmr.2003.11.019. [DOI] [PubMed] [Google Scholar]
- 14.Conradsson M, Lundin-Olsson L, Lindelof N, Littbrand H, Malmqvist L, Gustafson Y, et al. Berg balance scale: intrarater test-retest reliability among older people dependent in activities of daily living and living in residential care facilities. Phys Ther. 2007;87:1155–63. doi: 10.2522/ptj.20060343. [DOI] [PubMed] [Google Scholar]
- 15.Chevan J, Atherton HL, Hart MD, Holland CR, Larue BJ, Kaufman RR. Nontarget- and target-oriented functional reach among older adults at risk for falls. J Geriatr Physical Therapy. 2003;26:22–5. [Google Scholar]
- 16.Jones CR. Measuring functional fitness for older adults. J Active Aging. 2002;2:24–30. [Google Scholar]
- 17.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:P239–43. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 18.van Haastregt JC, Zijlstra GA, van Rossum E, van Eijk JT, Kempen GI. Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. Am J Geriatr Psychiatry. 2008;16:186–93. doi: 10.1097/JGP.0b013e3181591c1e. [DOI] [PubMed] [Google Scholar]
- 19.Wang XS, Cleeland CS, Mendoza TR, Engstrom MC, Liu S, Xu G, et al. The effects of pain severity on health-related quality of life: A study of Chinese cancer patients. Cancer. 1999;86:1848–55. [PubMed] [Google Scholar]
- 20.Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim S, Lockhart T, Roberto K. The effects of eight-week balance training or weight training for the elderly on fear of falling measures and social activity levels. Qual Ageing. 2009;10:37–48. doi: 10.1108/14717794200900030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, Haas M, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med. 2006;12:40–7. [PMC free article] [PubMed] [Google Scholar]
- 23.Krucoff C, Carson K, Peterson M, Shipp K, Krucoff M. Teaching yoga to seniors: Essential considerations to enhance safety and reduce risk in a uniquely vulnerable age group. J Altern Complement Med. 2010;16:899–905. doi: 10.1089/acm.2009.0501. [DOI] [PubMed] [Google Scholar]


