Abstract
Background & objectives:
The patterns of abused psychoactive substances change over time, and it is important to document such changes. The present retrospective study was carried out to document these changes in patients registered in a de-addiction centre in north India over three decades.
Methods:
Case notes of all patients registered in the centre from September 1978 till December 31, 2008 were reviewed. Comparisons were made among three decades (1978-1988, 1989-1998, and 1999-2008).
Results:
The number of registered subjects increased eight-fold over the decades, and age of the subjects presenting for the treatment decreased. The percentages of subjects presenting for the treatment with opioid dependence were 36.8 per cent (n=204), 42.9 per cent (n=809) and 53.2 per cent (n=2219), respectively for the three decades (P<0.001). The proportion of subjects using natural opioids decreased over the three decades (47.4, 26.5 and 18.3%; P<0.001), with a concomitant emergence and/or increase of newer and prescription opioids such as buprenorphine, codeine and dextropropoxyphene. Dependence on tobacco and sedative-hypnotics also increased, and inhalant abuse was reported especially in the third decade. Polysubstance dependence increased significantly over the decades (P<0.001).
Interpretation & conclusions:
Our results showed major shifts in the patterns of substance abuse in clinic-attending patients in north India over the three decades from 1978 till 2008. These have important implications for all the stakeholders concerned with combating the challenge of psychoactive substance abuse in our society.
Keywords: Dependence, India, opioids, pattern, substance abuse, trends
Psychoactive substance abuse in India continues to be a substantive problem for the individual as well as for the society. One of the foremost essential steps to combat this challenge is to document the extent, patterns and trends of substance abuse to appreciate the magnitude and severity of the problem. Numerous surveys have been conducted since the early 1970s at various levels and in various populations in India to assess the level of psychoactive substance abuse. The prevalence estimates ranged from 0.94 per 1000 population in the earlier studies1to 350 per 1000 population in more recent ones2,3. The focus of these studies varied from use of alcohol to use and dependence on the substances in general. In the largest general population study conducted till date, current prevalence of alcohol use was 21.4 per cent, cannabis 3.0 per cent, heroin 0.2 per cent, opium 0.4 per cent and other opiates 0.1 per cent; further, 17-29 per cent of the current users of these substances were found to be using these substances in dependent pattern4.
Substance use estimates, however, are liable to change over time, depending upon diverse factors such as availability and cost of the substances in the community, existing legislations and their implementation, social perception and attitude about use of particular substances, peer pressure and other socio-cultural factors5,6. A study published in a WHO document in 1980 remarked that “…The last point and one which deserves careful consideration is the absence of large-scale heroin or related substance abuse in India”7. Just four years later, this was contradicted by the same author in view of the rapid increase in heroin dependence in patients attending a de-addiction centre in Delhi8. This was followed by newer entrants in the substance abuse scenario: buprenorphine injection, codeine-containing cough syrups, dextropoxyphene and other opioid oral preparations, inhalants, cocaine, and the latest being several “club and rave drugs”9.
It is apparent that no single cross-sectional survey can cover this complex shift of the substance use across time, unless such surveys are repeated at regular intervals on the same defined population. In India, no such general population-based repeated survey series is available. In view of this, another important source of data that can capture the shifting patterns is from established de-addiction clinics10. These clinics serve a geographically fixed population, have uniform mode of referral and diagnostic practices, and usually have fair degree of documentation and record retrievability.
There are only two published studies on longitudinal trends in substance abuse patterns till date. In a study from north India, Sachdev et al11 compared the profile of the patients presenting to the de-addiction centre in 1998, and compared it with those reporting in 1994. There was a decrease in the use of “opium” by almost half and on increase in the use of “poppy husk” by almost double. The most glaring finding was an increase in the abuse of medications such as dextropropoxyphene, diphenoxylate, codeine, etc., from 11.08 per cent in 1994 to 28.25 per cent in 1998. However, the time period covered was only four years. In the study from south India, Venkatesan and Suresh12 compared the patients reporting to the psychiatry OPD of a general hospital for substance use over two decades (1985-1986 till 2005-2006), studied at three time-points set two decades apart (1985-1986, 1995-1996, respectively 2005-2006). The majority of the patients were dependent on alcohol across the decades but there was a significant increase in the number of patients with polysubstance use from 12.8 and 10.6 per cent in 1985-1986 and 1995-1996, respectively to 20.4 per cent in 2005-2006. They have not reported use of heroin and newer psychotropic substances in the recent years.
The Drug De-addiction and Treatment Centre (DDTC), established a 20-bedded inpatient section and an Out-Patient Department (OPD) at Postgraduate Institute of Medical Education & Research (PGIMER), Chandigarh, has earlier reported the abuse of several newer drugs over the past 20 years, such as buprenorphine13, carisoprodol14, codeine-containing cough syrups15, inhalants16,17, dextropropoxyphene18, and even opium-containing Ayurvedic and Unani herbal medicines19. However, at the end of three decades of continuous registration of patients and documentation of their substance abuse pattern, it was felt appropriate to take a stock of the situation over these three decades in a systematic manner. Thus, the present retrospective study was carried out to document the profile of the patients registered in the DDTC and any change in the overall patterns of substance abuse over the three decades (1978-2008).
Material & Methods
For the present study, case notes of the patients registered in DDTC at PGIMER, Chandigarh, since its inception in September 1978 till December 31, 2008 were reviewed. Psychoactive substance dependence was diagnosed as per the WHO International Classification of Diseases (ICD), 9th edition20 until December 1992 and later ICD-1021 by a consultant psychiatrist after direct interview with the patient and their relatives.
A semi-structured socio-demographic proforma was used to record gender, age, marital status, locality and other socio-demographic data. The clinical data for the purpose were essentially the diagnosis of substance dependence. Among opioids, the specific opioid predominantly used by the patients at the time of registration (e.g., opium and poppy husk clubbed as natural opioids, heroin, buprenorphine, dextropropoxyphene, etc.) was also noted. For a person dependent on multiple classes of substances (e.g., alcohol, opioids, cannabis) all were counted separately as well as polysubstance dependence. Accordingly, the number (and percentages) of substances was more than the number of patients.
Patients and their substance data were grouped into three decades: 1978-1988 (1st decade), 1989-1998 (2nd decade) and 1999-2008 (3rd decade). The statistical analysis was done using the SPSS software package for Windows, version 14.0 Chicago, USA. Mean values were calculated for continuous variables and frequencies were calculated for categorical variables. ANOVA with post-hoc Scheffe test was applied to compare the continuous variables and chi-square test was applied to compare the qualitative variables.
Results
The total numbers of patients registered during the entire observation period were 6608. Among these patients the complete case records sufficient for data collection were available for 6508 subjects (98.5%). On dividing the groups decade-wise, there were 555 subjects during the period 1978-1988 (1st decade, covering 10 years 4 months), 1885 in the decade 1989-1998 (2nd decade) and 4168 in the decade 1999-2008 (3rd decade).
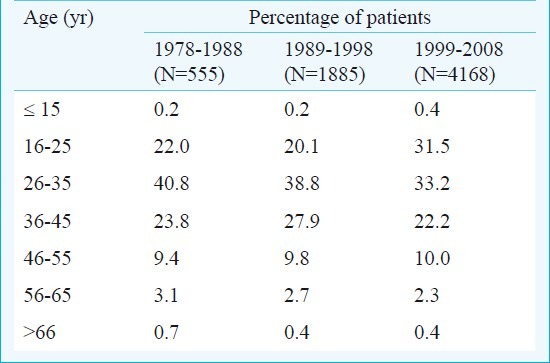
Socio-demographic profile: Majority of the subjects were males (99.5%), with no decade-wise difference. The mean ages at the time of DDTC registration were 33.75 ±10.40 yr for the first decade, 34.48 ± 10.04 for the second, and 32.68 ± 10.62 yr for the third decade. The differences in the ages were statistically significant (P<0.001). Majority (76.8%) of the subjects registered in the first decade were married at the time of registration, 74.2 per cent in the second decade and 62.5 per cent in the third decade. The difference was statistically significant (P<0.001). Age category-wise distribution of patients is given in the Table. Significantly fewer numbers of subjects were from the rural background for the second decade (first- 32.8%, second-24.4%, third- 32.7% P<0.001).
Table.
Category-wise age distribution of clinic-attending patients over three decades
Alcohol: The percentages of the subjects presenting with alcohol dependence were 57.3 per cent (n=318), 59.4 per cent (n=1120) and 47.8 per cent (n=1994) for the first, second and third decades respectively (Fig.); there was a statistically significant decrease (P<0.001) in the percentage of the subjects presenting with the alcohol dependence. The mean ages of the subjects with alcohol dependence were 35.40 ± 9.66 yr, 37.26 ± 9.22 yr and 38.08 ± 10.01 yr for the first, second and third decades, respectively. The differences in the age group were statistically significant after applying post-hoc Scheffe test, for the first vs. second decade (P<0.05) and for first vs. third decade (P<0.001) but not for the second vs. third decade. Across the decades almost equal numbers of subjects were married and there was no significant difference (83.4, 84.8 and 82.8%, respectively).
Fig.
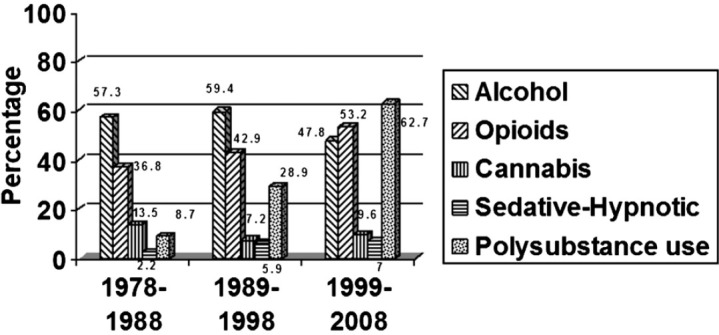
Patterns of use of major types of psychoactive substance in clinic-attending patients over three decades: decade-wise distribution.
Opioids: The percentages of subjects presenting for the treatment with opioid dependence were 36.8 per cent (n=204), 42.9 per cent (n=809) and 53.2 per cent (n=2219), respectively for the three decades (Fig.). There was a significant increase in the number of subjects presenting with opioid dependence (P<0.001). Further, the mean presenting ages of the subjects decreased significantly (P<0.001) over three decades, being 32.68 ± 11.52 yr, 30.83 ± 9.94 yr and 28.33 ± 8.37 yr, respectively. The differences were statistically significant (P<0.001), and after applying post hoc Scheffe test for the first and second decade (P<0.05), for the first and the second decade (P<0.001) and second and the third decade (P<0.001). The numbers of subjects being married were 70, 60.7 and 48.2 per cent for the three decades, respectively, with significant decrease in the percentage of the subjects being married over the decades (P<0.001). The number of subjects from the rural background fluctuated over three decades and were 35.5, 30.2 and 35.5 per cent, respectively and the difference was statistically significant (P<0.05).
Specific types of opioids: In the first decade, 47.4 per cent of the subjects were using natural opioids, 32.6 per cent heroin, 15.3 per cent injectable opioids such as morphine, pethidine, or pentazocine; 3.7 per cent of the subjects used more than one opioid, and 4.2 per cent of the subjects used other opioids (dextropropoxyphene/ diphenoxylate). There was no case of buprenorphine dependence during the first decade because buprenorphine was not available in the Indian market until 1988.
The proportion of subjects using natural opioids (47.4% in the first decade) decreased significantly (P<0.001) in the second decade to 26.5 per cent and to 18.3 per cent in the third decade. Percentage of subjects using heroin reduced to 18.2 per cent in the second decade but again increased in the third decade to 22.6 per cent. Percentage of subjects presenting for the treatment injecting either buprenorphine or pentazocine increased to 19.9 per cent in the second decade but reduced to 13.0 per cent in the third decade. Codeine containing cough syrup abuse made its entry first time in the second decade (11.9% of the subjects) compared to none in the previous decade. There was a dramatic decrease in the proportion of subjects using injection morphine or pethidine in the second decade (1.9%, compared to 12.1% in the first) and no subject reported to the de-addiction centre in the third decade with predominant morphine or pethidine dependence.
The most rapid rise was seen in the subjects presenting with dextropropoxyphene/ diphenoxylate dependence from the second to the third decade. The percentage of the subjects increased to 5.5 per cent in the second decade and to 22.2 per cent in the third decade. There was also a rapid increase in the number of subjects using more than one type of opioid – from 3.7 per cent in the first decade to 16 per cent in the second decade, which remained at almost the same level in the third decade (16.5%).
Cannabis: The percentages of subjects presenting for the treatment with cannabis dependence were 13.5, 7.2 and 9.6 per cent, respectively for the three decades (Fig.). The difference in the three groups was statistically significant (P<0.001). The mean age of the subjects were 28.30 ± 9.45 yr, 28.95 ± 7.64 yr and 26.97 ± 7.86 yr for the three decades, respectively. The difference in the ages was significant (P<0.05), subjects registered in the third decade being significantly younger than those in the earlier two decades. The difference in the percentages of married subjects in the three groups also reached significant levels (48, 62.2 and 34.8%, respectively; P<0.05).
Other substances: Overall 2714 (41.7%) had tobacco dependence. The percentages of the subjects with dependence on tobacco products have increased drastically over the three decades and increased from 6.1 per cent in 1978-1988 to 18 per cent in second and 57.2 per cent in third decade. However, tobacco dependence was co-morbid with other substance dependence in the vast majority of cases; only 2 per cent of the subjects reported exclusively with tobacco dependence and no history of any other substance use.
Six per cent of the total had dependence on sedative-hypnotics. Over the decades dependence on sedative-hypnotics had increased: 2.2, 5.9 and 7 per cent, respectively (Fig.). Stimulant abuse was rarely represented: 0.2 per cent of the total sample used stimulants: 1.4 per cent in the first decade, 0.3 per cent in the second, and in the third decade only one subject reported abusing stimulants. Inhalant substance abusing individuals was the late entrant among the subjects presenting to the treatment centre. While 0.8 per cent of the total subjects reported abusing inhalants, among them only one subject had been registered in the second decade while all others in the third decade, mostly abusing typewriter-erasing fluids.
Polysubstance dependence: The percentages of the individuals dependent on two or more substances in the three successive decades were 8.7, 28.9 and 62.7 per cent, respectively. This was a significant (P<0.001) increase. In order to ensure that this was a true reflection of the trend and not just due to changing diagnostic practices over the years, two other, progressively more conservative, strategies were adopted to analyze the data. Using a narrower and more stringent criterion for ‘polysubstance’ as three or more substances, the percentages of the subjects dependent on three or more substances were 5.8, 5.9 and 13.9 per cent, respectively. The difference in the three groups was significant (P<0.001), with an obvious increase in polysubstance dependence in the third decade compared to the earlier ones. By further removing tobacco from the consideration of polysubstance, the percentages of the same (dependence on two or more substances after excluding tobacco dependence) were 8.7, 15.4 and 20.3 per cent, respectively. This difference was also significant (P<0.001).
Discussion
The present study brought out several trends and patterns of appreciable concern. First, the numbers of subjects registered in DDTC over the decades have risen from 555 in the first decade to 4168 in the third decade, reflecting a near eight-fold increase. This increase in numbers may either reflect an increase in substance abuse problems over the decades, or more subjects attending our Centre, or, likely a combination of both factors. It is interesting to note that the study from Tamil Nadu12 did not record any such increase in the numbers recorded at the three time-points of their study; indeed, there was somewhat a decrease in the actual numbers (344, 245 and 250 in the years 1985-1986, 1995-1996 and 2005-2006, respectively).
Second, the subjects were increasingly presenting at younger age. This was particularly apparent for subjects registered in the last decade (1999-2008), when 31.5 per cent of the subjects were in the age group 16-25 yr, compared to 22 and 20 per cent of the subjects in the first and second decades, respectively. The subjects were of younger age group in the third decade compared to the Drug Abuse Monitoring System (DAMS) data22. In the study from south India, younger age of initiation of substance use has been noted12. Thus, our data document the major concern that increasingly more number of younger people is being seen in the treatment facilities in India, which may reflect the phenomenon of substance abuse making inroads into adolescents and young adults of the society.
Third, there was a significant increase in the percentage of subjects presenting for the treatment of opioid dependence over the decades. This was also seen in the study from north India11. Studies from other parts of the world have also shown increase in the number of subjects consuming opioid drugs23,24. There was a significant decrease in the age at presentation and percentage of married subjects presenting for the treatment of opioid dependence. This was similar to a study from China: 55.7 per cent of the subjects were between 26-35 yr of age and 54.7 per cent were unmarried23,25.
Fourth, our data clearly documented the shifting landscape of types of opioid abuse over 30 years. Across the three decades, there was a significant decline in the registration of dependence on natural opioids and a concomitant increase in the use of prescription drugs, a trend seen in all parts of the world26,27. The second decade recorded the entry of dependence on buprenorphine and codeine-containing cough syrups, and the third decade recorded a substantive increase in the cases of dextropropoxyphene dependence. These have been earlier reported from our Centre13,15,19, but this is the first systematic documentation of this shifting pattern of abuse of specific opioid types.
Fifth, the percentage of subjects reporting for the treatment of alcohol dependence had decreased over the decades. This is in keeping with another study from the region11. The similar trend has been observed in some other parts of the world28. This might be due to either an increased degree of tolerance of the family members towards the subjects with alcohol dependence, or because of more number of subjects presenting in the clinic with opioid dependence, thus resulting in a relative decrease in the percentage of subjects presenting with alcohol dependence. The latter possibility appears stronger, because the absolute number of subjects registered with DDTC with alcohol dependence has definitely increased though the percentage has decreased. Further, over the decades, mean age of the subjects presenting with alcohol dependence increased significantly. However, the study from Tamil Nadu12 did not find any such trend. Although the DAMS Project report22 collected data from 51 de-addiction centres from all over India, it does not provide any region-wise distribution of substance profiles. Our data suggest that there are two contrasting trends regarding the registration age of subjects: that of alcohol dependence (progressively increasing) vs. that of opioid and poly-substance dependence (progressively decreasing). The latter trend being more powerful, the net result seen was a decrease in registration age for the entire sample.
Sixth, and the most important, was the increasing trend in polysubstance dependence seen over the decades in our subject population. This has been observed in other parts of India as well12,29.
Among the other notable findings are the patterns of increase in dependence on tobacco products and sedative-hypnotics over the years. According to the National Family Health Survey-2 (1998-1999)30, 47 per cent of men older than 15 yr of age smoked or chewed tobacco. The prevalence may be underestimated by almost 11 per cent for chewing and 5 per cent for smoking because of use of household informants31. Thus, our figure for tobacco use in the third decade closely parallels the national-level data. Perhaps the lower figures for tobacco use reported in the earlier two decades were partly due to inadequate documentation as well as inadequate reporting as the DDTC is often viewed as a “drug and alcohol” treatment centre.
Last but not the least, inhalant abuse can be seen in a still small but rising trend recently16,17. Learning lessons from the past, it is imperative to be aware of the trends of newer substance abuse appearing on the horizon as a small cloud before it covers the sky13–15.
The limitations of interpretation of this study are important to consider. A clinic-based study is not meant to answer the question of true prevalence of substance abuse in the general population, simply because the data reflect on the subjects who attend (or are brought to) the clinic for seeking treatment. A further limitation is the substantive drop-out of 40-50 per cent from the first-seen screening level at the Centre (the Walk-in Clinic) to the detailed work-up (DDTC registration) level10. The essential strength of our data lies in its large size over a long period of time spanning 30 years, from a geographically large but fixed catchment area, consistent pattern of diagnosis by qualified psychiatrists as per formal diagnostic criteria, and complete and uniform documentation, coupled with high retrieval of data over 30 years (98.5%).
In conclusion, the present study highlights that there have been major shifts in the patterns of substance abuse as documented in subjects registered in a public sector drug de-addiction centre in north India over three decades from 1978 till 2008. The number of people registered in the de-addiction centre increased eight-fold. There was a significant increase in dependence on opioids as a broad class, emergence of newer substances of abuse, and a significant increase in prescription drugs and polysubstance dependence in recent years. All these have important implications for all the stakeholders concerned with combating the mounting challenge of psychoactive substance abuse in our society.
References
- 1.Nandi DN, Ajmany S, Ganguli H, Banerjee G, Boral GC, Ghosh A, et al. Psychiatric disorders in a rural community in West Bengal: an epidemiological study. Indian J Psychiatry. 1975;17:87–99. [Google Scholar]
- 2.Ghulam R, Rahman I, Naqi S, Gupta SR. An epidemiological study of drug abuse in urban population of Madhya Pradesh. Indian J Psychiatry. 1996;38:160–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Hazarika NC, Biswas D, Phukan RK, Hazarika D, Mahanta J. Prevalence and pattern of substance abuse at Bandardewa, A border area of Assam and Arunachal Pradesh. Indian J Psychiatry. 2000;42:262–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Ray R, Mondal AB, Gupta K, Chatterjee A, Bajaj P. New Delhi: United Nations Office on Drugs and Crime (UNODC) and Ministry of Social Justice and Empowerment, Government of India; 2004. The extent, pattern and trends of drug abuse in India: National Survey. [Google Scholar]
- 5.World Health Organisation. Nomenclature and classification of drug- and alcohol-related problems: a WHO Memorandum. Bull World Health Organ. 1981;59:225–42. [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma HK. Sociocultural perspective of substance use in India. Subst Use Misuse. 1996;31:1689–714. doi: 10.3109/10826089609063997. [DOI] [PubMed] [Google Scholar]
- 7.Mohan D. India: Socioeconomic development and changes in drug use. In: Edwards G, Arif A, editors. Drug problems in the sociocultural context: a basis for policies and programme planning. Public Health Papers, No.73. Geneva: World Health Organization; 1980. pp. 42–8. [Google Scholar]
- 8.Saxena S, Mohan D. Rapid increase of heroin dependence in Delhi: some initial observations. Indian J Psychiatry. 1984;26:41–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Chakraborty K, Neogi R, Basu D. Club drugs: review of the ‘rave’ with a note of concern for the Indian scenario. Indian J Med Res. 2011;133:594–604. [PMC free article] [PubMed] [Google Scholar]
- 10.Basu D, Mattoo SK. Epidemiology of substance abuse in India: methodological issues and future perspectives. Indian J Psychiatry. 1999;41:145–53. [PMC free article] [PubMed] [Google Scholar]
- 11.Sachdev JS, Yakhmi RS, Sharma AK. Changing pattern of drug abuse among patients attending de-addiction centre at Faridkot. Indian J Psychiatry. 2002;44:353–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Venkatesan J, Suresh SSD. Substance dependence: decades apart in a teaching hospital. Indian J Psychiatry. 2008;50:100–5. doi: 10.4103/0019-5545.42396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basu D, Varma VK, Malhotra AK. Buprenorphine dependence: A new addiction in India. Disabil Impair. 1990;3:142–6. [Google Scholar]
- 14.Sikdar S, Basu D, Malhotra A, Varma VK, Mattoo SK. Carisoprodol abuse: report from India. Acta Psychiatr Scand. 1993;88:302–3. doi: 10.1111/j.1600-0447.1993.tb03462.x. [DOI] [PubMed] [Google Scholar]
- 15.Mattoo SK, Basu D, Sharma A, Balaji M, Malhotra A. Abuse of codeine containing cough syrups : a report from India. Addiction. 1997;92:1783–7. [PubMed] [Google Scholar]
- 16.Basu D, Jhirwal OP, Singh J, Kumar S, Mattoo SK. Inhalant abuse by adolescents: A new challenge for Indian physicians. Indian J Med Sci. 2004;58:245–9. [PubMed] [Google Scholar]
- 17.Kumar S, Grover S, Kulhara P, Mattoo SK, Basu D, Biswas P, et al. Inhalant abuse: A clinic-based study. Indian J Psychiatry. 2008;50:117–20. doi: 10.4103/0019-5545.42399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basu D, Gaur N, Das PP, Mattoo SK. Herbal medicines: perfect garb for opioid abuse? A case series from India. Am J Addict. 2011;20:174–5. doi: 10.1111/j.1521-0391.2010.00101.x. [DOI] [PubMed] [Google Scholar]
- 19.Basu D, Banerjee A, Harish T, Mattoo SK. Disproportionately high rate of epileptic seizure in patients abusing dextropropoxyphene. Am J Addict. 2009;18:417–21. doi: 10.3109/10550490903077697. [DOI] [PubMed] [Google Scholar]
- 20.The ICD-9 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1978. World Health Organization. [Google Scholar]
- 21.The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. World Health Organization. [Google Scholar]
- 22.WHO Biennium Project. Report: Drug Abuse Monitoring System (SE/06/226877 & SE/07/117746). National Drug Dependence Treatment Centre, AIIMS, New Delhi (2006-2007) [accessed on December 4, 2010]. Available from: http://www.whoindia.org/LinkFiles/Mental_Health_&_substance_Abuse_Drug_Abuse_Monitoring_System.pdf .
- 23.Report of drug surveillance 2003. Beijing: NDASC, NIDD; 2003. National Institute on Drug Dependence (NIDD) and National Drug Abuse Surveillance Center (NDASC) [Google Scholar]
- 24.Report of drug surveillance 2004. Beijing: NDASC, NIDD; 2004. National Institute on Drug Dependence (NIDD) and National Drug Abuse Surveillance Center (NDASC) [Google Scholar]
- 25.Manchikanti L. National drug control policy and prescription drug abuse: facts and fallacies. Pain Physician. 2007;10:399–424. [PubMed] [Google Scholar]
- 26.Survey on Drug Use and Health: National Findings. (Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 064194). Rockville, MD. 2006. [accessed on December 4, 2010]. Available from: www.oas.samhsa.gov/nsduh/2k5nsduh/2k5Results.pdf .
- 27.Califano JA. High society: How substance abuse ravages American society and what to do about it. New York: Perseus Publishing; 2007. [Google Scholar]
- 28.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend. 2004;74:223–34. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Margoob MA, Majid A, Hussain A, Wani ZA, Yousf A, Malik YA, et al. Changing sociodemograhic and clinical profile of substance use disorder patients in Kashmir Valley. JK Practitioner. 2004;11:14–6. [Google Scholar]
- 30.National Family Health Survey, 1998-1999. Summary of findings. [accessed on May 22, 2012]. Available from: http://hetv.org/pdf/nfhs/india/indfctsm.pdf .
- 31.Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L. Tobacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household survey. [accessed on May 10, 2011];Tobacco Control. 2003 12:e4. doi: 10.1136/tc.12.4.e4. Available from: http://www.tobaccocontrol.com/cgi/content/full/12/4/e4 . [DOI] [PMC free article] [PubMed] [Google Scholar]


