Abstract
Background & objectives:
Traditionally, rabies diagnosis is made by demonstration of rabies viral antigen by direct immunofluorescence (DIF) and mouse inoculation test (MIT). The present study was carried out to evaluate the role of reverse transcriptase-polymerase chain reaction (RT-PCR) in comparison with these conventional techniques for the diagnosis of rabies.
Methods:
Skin biopsies, corneal impression smears and saliva sample were collected ante-mortem and brain tissue and CSF were collected post-mortem from ten clinically suspected rabies patients. DIF, Seller staining, MIT and RT-PCR were performed on the patients’ samples for the diagnosis of rabies. The ability of RT-PCR to detect rabies virus earlier as compared to other assays was tested both for reference virus as well as clinical isolates.
Results:
All samples taken ante-mortem were negative for DIF test. Six of 10 post-mortem brain tissues of the clinically suspected patients were positive both by RT-PCR and MIT, of these six, five were positive by DIF test and four were positive by Seller stain. RT-PCR could detect the rabies virus earlier as compared to DIF, both from clinical isolates and fixed rabies virus.
Interpretation & conclusions:
The present results showed 100 per cent sensitivity and specificity of RT-PCR as compared to 83.3 per cent of DIF and 66.7 per cent of Sellers stain for diagnosis of rabies. RT-PCR also detected rabies viral infection earlier as compared to conventional tests and can also be used on ante-mortem samples. Thus, the present study shows the usefulness of RT-PCR as an alternative to MIT for the confirmation of rabies diagnosis.
Keywords: Ante-mortem diagnosis, MIT, rabies, RT-PCR
Rabies is responsible for approximately 50,000 to 100,000 deaths per year worldwide1. Although preventable by vaccination, this deadly disease is still not controlled and its true impact is largely underestimated2. Exact data on magnitude of human rabies in India are not available as surveillance mechanism for rabies hardly exists. However, India contributes a major chunk to global rabies mortality. Central Bureau of Health Investigation (CBHI) records about 500 deaths due to rabies annually which has though come down below 300 in recent years3. This is still a serious concern when safe and effective anti-rabies treatment is available.
An early confirmation of rabies is extremely important to prevent the spread of infection by timely institution of proper immunization or the unnecessary use of post-exposure prophylaxis if found negative. Traditionally, ante-mortem diagnosis of rabies is made by demonstration of rabies virus antigen by direct immunofluorescence (DIF) in corneal/conjunctival smears and skin biopsies4. DIF of corneal scrapings and skin biopsies has a sensitivity of 20- 50 per cent5,6. The confirmatory diagnosis of rabies is the mouse inoculation test (MIT) using patient brain tissue obtained at autopsy. Though MIT has a sensitivity of more than 98.3 per cent and specificity of 100 per cent it is laborious, takes 2 to 3 wk time and requires many experimental mice7. Recently, molecular techniques such as the reverse transcriptase polymerase chain reaction (RT-PCR)8–10 and nucleic acid sequence based amplification assay (NASBA)11,12 have been tried by various workers to improve the sensitivity and specificity of ante- as well as post-mortem diagnosis of rabies. The present study was carried out to evaluate the role of RT-PCR in comparison with conventional techniques like DIF and MIT for the diagnosis of rabies.
Material & Methods
The study was conducted over a period of three years in the Department of Virology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. Fifteen patients attending PGIMER, Chandigarh, with clinical features suspected of rabies encephalitis were included in the study. Ten of them died within 4 to 10 days of hospital admission while five left the hospital against medical advice and hence were not included in the study. Thus both ante-mortem and post-mortem samples of ten patients were analyzed in the study.
Skin biopsies and corneal impression smears were collected ante-mortem according to the standard protocol7. An additional saliva sample was collected with the consent of the patient or the attendants. In case of patient's demise, brain tissue and CSF were collected at autopsy. All samples were collected after obtaining the written informed consent from the patient's attendants. The study protocol was approved by the Institute's ethics committee.
DIF test: This was performed on the nuchal skin biopsies, corneal impression smears and brain tissue. Five different sections of skin tissue containing at least 8-10 follicles per smear were examined for the presence rabies antigen. The acetone fixed smears were stained with sheep antirabies serum conjugated with fluorescein isothiocyanate (FITC) [Central Research Institute (CRI), Kasauli] at 1:8 dilution and examined under the epifluorescence microscope (Nikon, Japan) to look for the apple-green fluorescence exhibited by the rabies viral antigen in the perifollicular nerve plexus.
Seller stain: Smears made from the brain tissue were examined for the presence of the characteristic Negri bodies by Seller stain7.
MIT: This was performed according to the standard protocol described by Koprowski et al13 by inoculating homogenized patient brain tissue intracerebrally in to two litters of 1-3 days old Swiss albino mice, each consisting of 6- 8 mice per litter.
To determine the earliest appearance of rabies virus RNA in the mouse tissues reference rabies fixed virus suspension (obtained from CRI, Kasauli) was also inoculated intracerebrally into two litters of mice. Two newborn mice were sacrificed per day and their brains and muzzle skins were harvested on alternate days (day 1- day 8 in case of reference virus and day 5 till death in case of clinical sample). This schedule was decided considering the short duration of the fixed rabies virus and routine observation on development of symptoms with clinical samples. Brain tissue and muzzle skin were subjected to DIF, Seller's staining and RT-PCR. The observations were recorded independently from two sets of such experiments and by two observers separately.
RT-PCR: Saliva, post-mortem brain tissue, CSF, infected mouse brain and muzzle skin samples preserved at -70°C were subjected for RT-PCR to detect the rabies virus RNA. The primer sequence was derived from the nucleocapsid gene of Pasteur virus strain as described previously14. cDNA synthesis was done by annealing 1μg of total RNA with 50 pmol each of the outer pair of primers for the nucleocapsid gene, 5’-CTA CAA TGG ATG CCG AC- 3’(66-82) and 5’-GAG TCA CTC GAA TAT GTC- 3’ (1402-1419) at 70°C for 5 min, and the product was chilled on ice. The reaction mixture was completed to a final volume of 20 μl containing murine leukaemia virus -RT and 10mM dNTP (MBI, Fermentas, USA) and incubated for 1 h at 42°C.
RNAcDNA hybrid was added to make 50 μl to PCR buffer containing 1.25 U of Taq DNA polymerase and 2 mM dNTP. The mixture was subjected to 40 cycles of PCR (94°C, 1 min; 43°C, 2 min; 72°C, 2.5 min) on a DNA thermal cycler (Techne, UK). Then 2μl of the primary amplified product was added to a 23 μl mixture that contained 2mM dNTP and 20 pmol each of the inner primer pair, 5’- GAC ATG TCC GGA AGA CTGG-3’ (319-337) and 5’-GTA TTG CCT CTC TAG CGG TG- 3’ (823-842) and 1U of Taq DNA polymerase. These were subjected to 40 cycles of PCR (94°C, 1 min; 43°C, 2 min; 72°C, 2.5 min). The final amplification product of 563 base pair was visualized in 1.2 per cent agarose gel electrophoresis and ethidium bromide staining.
Sensitivity of RT-PCR was determined by quantitating the extracted RNA from fixed virus inoculated MIT positive brain sample diluted in log dilutions from 10-1 to 10-6 and then amplified by the polymerase chain reaction.
Japanese encephalitis virus (JEV) infected mouse brain, measles virus infected tissue culture supernatant and normal mouse brain was subjected to RT-PCR to check the specificity of the primers.
Results
The age group of the clinically suspected rabies patients was in the range of 4 to 60 yr including both children and adults. Of the 15 rabies patients, six belonged to less than 15 yr age group. All had a history of dog bite in the preceding 1-6 months. Ten of them died within 4 to 10 days of hospital admission while five left the hospital against medical advice.
The clinical presentation, duration of illness and course of illness in the 10 patients were consistent with features of human rabies. Hydrophobia, the most characteristic and widely known feature of the disease, was present in 100 per cent of patients followed by parasthesias (80%), agitation and confusion (60%).
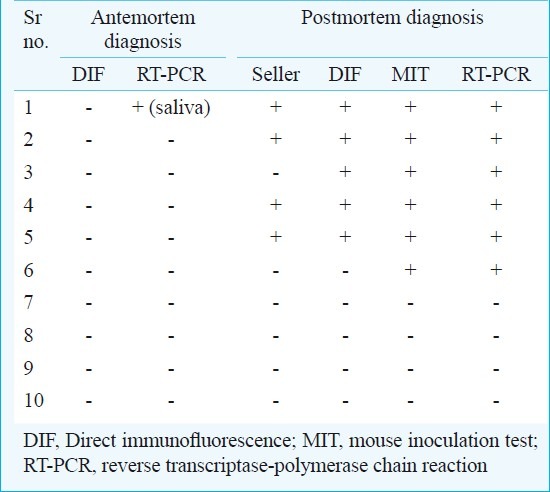
None of the samples taken ante-mortem, i.e., skin tissues, corneal/conjunctival smears were found to be positive for rabies viral antigen by DIF test. None of the CSF and serum samples and one of the 10 saliva samples collected was positive by RT-PCR. In six of the 10 post-mortem brain tissues of the clinically suspected patients, both RT-PCR and MIT were positive. Five of these six post-mortem brain tissues were positive by DIF test and four by Seller stain (Table I).
Table I.
Comparison of Seller, DIF, MIT and RT-PCR in antemortem and postmortem samples in clinically suspected rabies cases
RT-PCR was consistently positive both in muzzle skin and brain tissue when examined day 5 onwards, whereas DIF showed marginal fluorescence on day 7 and became convincingly positive from day 9 onwards (Table II). Negri body detection by Seller stain became positive on day 9 post-inoculation. Rabies viral RNA could be detected as early as 3rd day of infection by RT-PCR (Figs 1, 2) followed by rabies viral RNA antigen by DIF on day 5 whereas symptoms developed on day 7.
Table II.
Results of inoculation of clinical isolate by Seller stain, DIF test and RT-PCR in mice brain and skin on different post-inoculation days
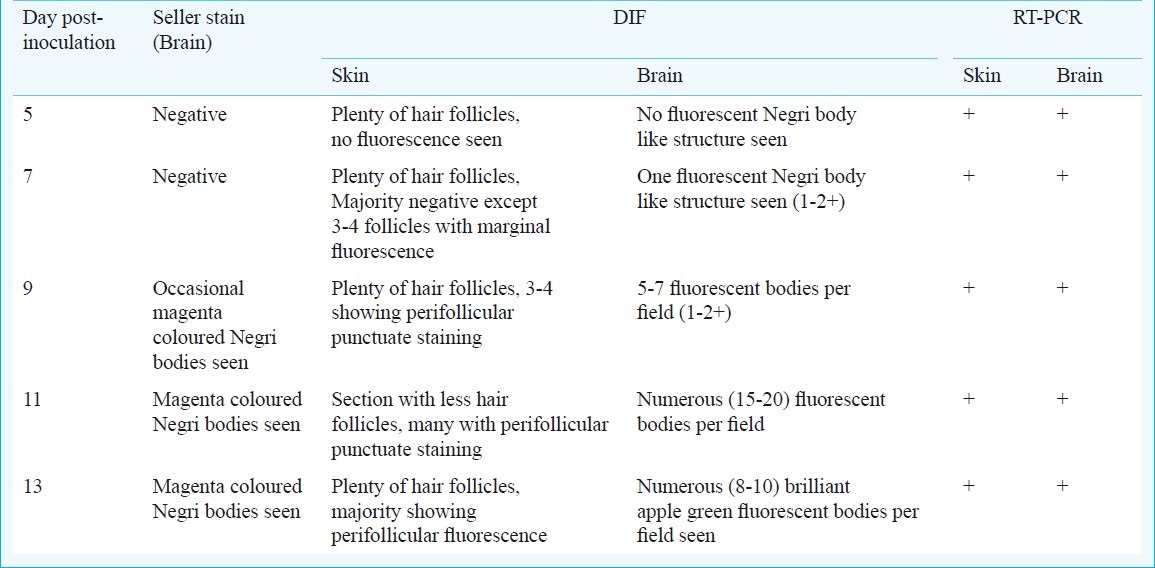
Fig. 1.
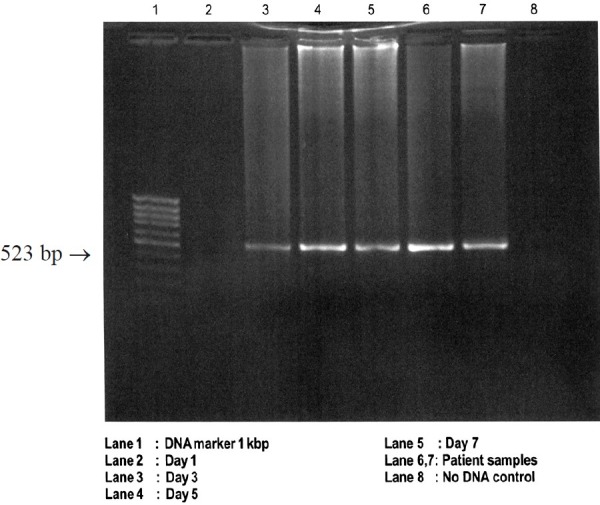
Detection of viral RNA by RT-PCR on different days post-inoculation of fixed rabies virus and patients’ samples in newborn mice brain.
Fig. 2.
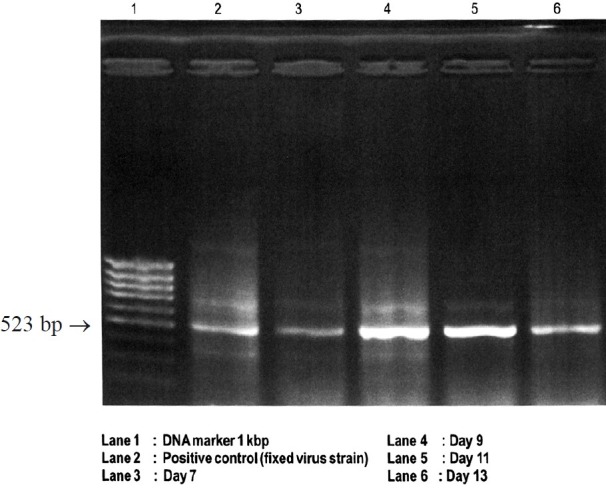
Detection of viral RNA by RT-PCR in mouse muzzle skin on different days post-inoculation of postmortem human brain sample in newborn mice.
Discussion
Rabies is a major public health problem in India. In a National multicentric rabies survey carried out by the Association of Prevention and Control of Rabies in India (APCRI) in collaboration with the WHO, the projected figure of deaths due to rabies per year was 20,56515.
In the present study, the direct immunofluorescence test of all the corneal smears and nuchal skin biopsies failed to demonstrate rabies viral antigen. The corneal smear used for viral antigen detection by IF has been extensively studied and shown to be poorly sensitive, besides being a cumbersome technique and having the danger of leaving an abraded cornea16,17. In various studies the sensitivity of skin biopsy positivity by DIF has varied between 25-50 per cent depending on several variables like the site of biopsy, number of sections examined and the amount of viral antigen18,19. It is necessary to sample the proper areas of the skin to include the maximum number of hair follicles and at a level of the epidermis which has the highest concentration of perifollicular nerve fibres. Crepin and colleagues9 reported that in routine laboratory testing, examination of a minimum number of 20 sections was needed to ensure the observations of several hair follicles.
In the present study 100 per cent sensitivity and specificity of RT-PCR were observed as compared to 83.3 per cent of DIF and 66.7 per cent of sellers stain, for diagnosis of rabies in post-mortem brain samples. The sensitivity of the Seller stain in the present study was in agreement with the sensitivity of 50-85 per cent reported by other workers4,20. It has been suggested that the development of these cytoplasmic inclusions depends on the length of survival after the onset of symptoms and cases with a fulminant course with shorter survival are unlikely to show these. Histology alone, therefore, does not confirm the diagnosis in all cases.
The direct immunofluorescence test could detect rabies viral antigen in 83.3 per cent cases of rabies positive patients proven by virus isolation method MIT. Our findings were in agreement with the study conducted by the California Department of Health in which a sensitivity of 99.4 per cent has been reported in 363 brains examined7. We have earlier detected rabies-specific antigen in 80.7 per cent cases21. In addition to the false negative results in the beginning phase of the illness, the efficiency of the DIF depends upon technical competency and expertise22,23. In MIT proven 95 rabid dog brains and three human brains, RT-PCR results were reported as 100 per cent concordant with MIT results8.
Besides the higher sensitivity, RT-PCR also showed the potentiality to detect rabies viral infection earlier as compared to DIF and Seller staining. It is to be emphasized that though both DIF and RT-PCR were positive in mice infected with rabies virus positive sample from day 7 onwards, the degree of positivity (i.e., the number of fluorescing antigen particles in brain tissue) was minimal by DIF, which could easily be missed, unless carefully looked for. The situation was similar with negri bodies by Seller stain on 9th day post-inoculation, whereas the results of RT-PCR were consistent from day 7 onwards.
The kinetics of rabies virus shedding in saliva is not well-defined. The present study observed RT-PCR positivity in only 10 per cent of the saliva samples as has been reported earlier in 30 per cent saliva samples9. A study has demonstrated a sensitivity of 100 per cent using a heminested RT-PCR to diagnose rabies from multiple saliva samples24. Therefore, the diagnosis of rabies can be made ante-mortem by RT-PCR. The negativity of PCR in CSF and serum samples could be due to inadequate amount of virus in sample or insufficient sample amount. Kamolvarin et al8 also quoted a similar poor sensitivity of 9 per cent. The low titres and the late appearance of virus in the CSF could to be the most likely cause for the negativity as the sampling was done only once.
In conclusion, our results demonstrated the potential of RT-PCR for the detection of rabies RNA in brain and saliva of infected humans.
References
- 1.Leung AK, Davies HD, Hon KL. Rabies: epidemiology, pathogenesis, and prophylaxis. Adv Ther. 2007;24:1340–7. doi: 10.1007/BF02877781. [DOI] [PubMed] [Google Scholar]
- 2.Coleman PG, Fevre EM, Cleaveland S. Estimating the public health impact of rabies. Emerg Infect Dis. 2004;10:140–2. doi: 10.3201/eid1001.020744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. http://cbhidghs.nic.in .
- 4.Plotkin SA. Rabies. Clin Infect Dis. 2000;30:4–12. doi: 10.1086/313632. [DOI] [PubMed] [Google Scholar]
- 5.Warrell DA. The clinical picture of rabies in man. Trans R Soc Trop Med Hyg. 1976;70:188–95. doi: 10.1016/0035-9203(76)90037-7. [DOI] [PubMed] [Google Scholar]
- 6.Vishawapoka U, Hemachudha T, Tepsumethanon W, Polsuwan C, Tirawatnpong S, Phanuphak P. Detection of rabies antigen in canine parotid glands by dot-blot technique. Lancet. 1988;1:881. doi: 10.1016/s0140-6736(88)91625-x. [DOI] [PubMed] [Google Scholar]
- 7.Jhonson HN. Rabies virus. In: Lennette EH, Schmidt NJ, editors. Diagnostic procedures for viral, rickettsial and chlamydial infections. 5th ed. American Public Health Association, Inc; 1979. pp. 843–78. [Google Scholar]
- 8.Kamolvarin N, Tirawatnpong T, Rattanasiwamoke R, Tirawatnpong S, Panpanich T, Hemachudha T. Diagnosis of rabies by polymerase chain reaction with nested primers. J Infect Dis. 1993;167:207–10. doi: 10.1093/infdis/167.1.207. [DOI] [PubMed] [Google Scholar]
- 9.Crepin P, Audry L, Rotivel Y, Gacoin A, Caroff C, Bourhy H. Intravitam diagnosis of human rabies by PCR using saliva and cerebrospinal fluid. J Clin Microbiol. 1998;36:1117–21. doi: 10.1128/jcm.36.4.1117-1121.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith J, McElhinney L, Parsons G, Brink N, Doherty T, Agranoff D, et al. Rapid ante-mortem diagnosis of a human case of rabies imported into the UK from the Philippines. J Med Virol. 2003;69:150–5. doi: 10.1002/jmv.10253. [DOI] [PubMed] [Google Scholar]
- 11.Wacharapluesadee S, Hemachudha T. Urine samples for rabies RNA detection in the diagnosis of rabies in humans. Clin Infect Dis. 2002;34:874–5. doi: 10.1086/338872. [DOI] [PubMed] [Google Scholar]
- 12.Wacharapluesadee S, Hemachudha T. Nucleic-acid sequence based amplification in the rapid diagnosis of rabies. Lancet. 2001;358:892–3. doi: 10.1016/S0140-6736(01)06041-X. [DOI] [PubMed] [Google Scholar]
- 13.Koprowski H. The mouse inoculation test. In: Kaplan MM, Koprowski H, editors. Laboratory techniques in rabies. 3rd ed. Geneva: WHO Publication; 1973. pp. 85–93. [PubMed] [Google Scholar]
- 14.Biswal M, Ratho R, Mishra B. Usefulness of reverse transcriptase-polymerase chain reaction for detection of rabies RNA in archival samples. Jpn J Infect Dis. 2007;60:298–9. [PubMed] [Google Scholar]
- 15.Sudarshan MK. Assessing the burden of rabies in India. WHO sponsored national multi-centric survey (May 2004) Assoc Prev Control Rabies India J. 2004;6:44–5. [Google Scholar]
- 16.Smith JS, Neill SU. Rabies virus. In: Lennette EH, Smith TF, editors. Laboratory diagnosis of viral infections. 3rd ed. New York: Marcel Dekker, Inc; 1999. pp. 745–60. [Google Scholar]
- 17.Noah DL, Drenzek CL, Smith JS, Krebs JW, Orciari L, Shaddock J, et al. Epidemiology of human rabies in the United States, 1980 to 1996. Ann Intern Med. 1998;128:922–30. doi: 10.7326/0003-4819-128-11-199806010-00012. [DOI] [PubMed] [Google Scholar]
- 18.Blenden DC, Creech W, Torres-Anjel MJ. Use of immunofluorescence examination to detect rabies virus antigen in the skin of humans with clinical encephalitis. J Infect Dis. 1986;154:698–701. doi: 10.1093/infdis/154.4.698. [DOI] [PubMed] [Google Scholar]
- 19.Blenden DC, Bell JF, Tsao AT, Umoh JU. Immunofluorescent examination of the skin of rabies-infected animals as a means of early detection of rabies virus antigen. J Clin Microbiol. 1983;18:631–6. doi: 10.1128/jcm.18.3.631-636.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jogai S, Radotra BD, Banerjee AK. Immunohistochemical study of human rabies. Neuropathology. 2000;20:197–203. doi: 10.1046/j.1440-1789.2000.00332.x. [DOI] [PubMed] [Google Scholar]
- 21.Ratho R, Grover R, Mahajan RC. Experience of human rabies in north India. Indian J Pathol Microbiol. 2001;44:41–4. [PubMed] [Google Scholar]
- 22.WHO Expert Consultation on rabies. World Health Organ Tech Rep Ser. 2005;931:1–88. [PubMed] [Google Scholar]
- 23.Chhabra M, Bhardwaj M, Ichhpujani RL, Lal S. Comparative evaluation of commonly used laboratory tests for post-mortem diagnosis of rabies. Indian J Pathol Microbiol. 2005;48:190–3. [PubMed] [Google Scholar]
- 24.Dacheux L, Reynes JM, Buchy P, Sivuth O, Diop BN, Rousset D, et al. A reliable diagnosis of human rabies based on analysis of skin biopsy specimens. Clin Infect Dis. 2008;47:1410–7. doi: 10.1086/592969. [DOI] [PubMed] [Google Scholar]


