Abstract
Chronic obstructive pulmonary disease (COPD) includes pulmonary components with increased comorbidity rates, as well as being a systemic disease. Comorbidities may frequently occur in COPD patients over 40 yr old. We report the comorbidities of patients with COPD, diagnosed by spirometry, in a population-based epidemiologic survey in Korea. Data were derived from the fourth Korean Health and Nutrition Examination Survey in 2008, a stratified multistage clustered probability design survey of a sample representing the entire population of Korea. Results of spirometry and various health-related questionnaires were analyzed in 2,177 subjects aged ≥ 40 yr. The prevalence of COPD (FEV1/FVC < 0.7) in subjects ≥ 40 yr of age was 14.1%. Multivariate analysis showed that underweight (odds ratio [OR] 3.07, 95% confidence interval [CI] 1.05-8.98), coronary heart disease (OR, 0.43; 95% CI, 0.20-0.93) and dyslipidemia (OR, 0.61; 95% CI, 0.45-0.82) were significantly associated with COPD, whereas allergic rhinitis, anemia, arthritis, chronic renal failure, depression, diabetes mellitus, hypertension, gastrointestinal ulcer, and osteoporosis were not. Underweight might be more prevalent but coronary heart disease and dyslipidemia are less prevalent in Koreans with than without COPD in population setting.
Keywords: Chronic Obstructive Pulmonary Disease, Comorbidity, Population-Based Survey
INTRODUCTION
COPD is characterized by chronic airway inflammation causing obstruction, as well as by lung parenchymal destruction causing emphysema. The prevalence of COPD is increasing at a greater rate than is the case for other chronic diseases, and COPD is predicted to be the third most frequent cause of deaths worldwide by 2020 (1). In addition to generating high healthcare costs, COPD and comorbidities are associated with disability and impaired quality of life.
COPD has been considered part of a "chronic systemic inflammatory syndrome", with several comorbidities of COPD associated with systemic inflammatory responses (2). Among the principal comorbidities of COPD are weight loss, skeletal muscle dysfunction, osteoporosis, progression of atherosclerosis, coronary artery disease, anxiety, depression, and a higher rate of lung cancer (3, 4). These comorbidities, however, may also be associated with gender, age, income, cigarette smoking and other factors. However, there have been few population-based studies of COPD comorbidities especially for Asian.
We therefore evaluated the nationwide incidence of COPD comorbidities, after controlling for sex, age, smoking and other factors, using data from the fourth Korean Health and Nutrition Examination Survey (4th KNHANES).
MATERIALS AND METHODS
Study design
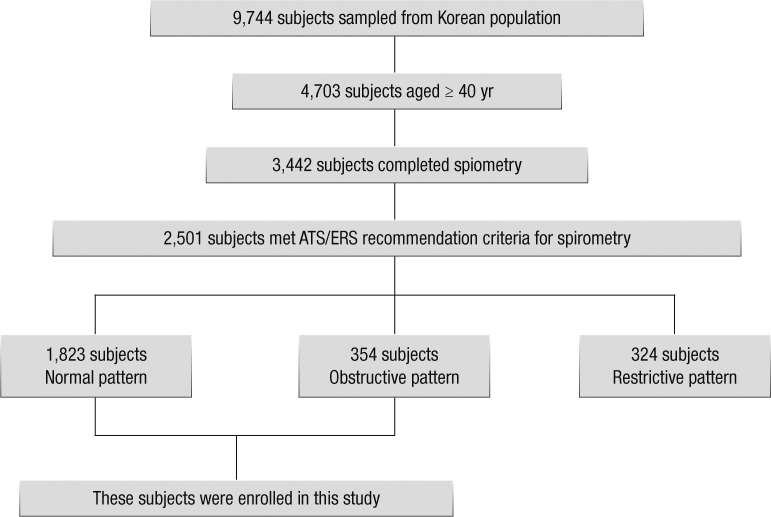
We retrospectively analyzed the database of the fourth Korean Health and Nutrition Examination Survey, a cross-sectional, nationally representative survey with stratified random sampling, performed by the Statistics Korea during 2008 (5). The survey involved 9,744 subjects selected from the Korean population; of these, 4,703 were aged ≥ 40 yr. The incidence of COPD and the comorbidities were evaluated in these latter subjects.
Data collection and spirometry
Trained interviewers administered standardized questionnaires on comorbidities associated with COPD, including allergic rhinitis, anemia, arthritis, coronary heart disease, chronic renal failure, depression, diabetes mellitus, dyslipidemia, hypertension, gastrointestinal ulcer, lung cancer, osteoporosis, and history of pulmonary tuberculosis; the questionnaires also included information on income and history of cigarette smoking. Spirometry was performed using dry rolling seal spirometers (Model 2130; SensorMedics, Yorba Linda, CA, USA) by well trained technicians, thus controlling for the quality of pulmonary function tests, as recommended by the American Thoracic Society/European Respiratory Society (ATS/ERS). Only data that met the criteria for acceptability and reproducibility were analyzed.
Definition of COPD and comorbidities
Airflow obstruction was defined as a ratio of forced expiratory volume in 1 second (FEV1) divided by forced vital capacity (FVC) < 0.7, with COPD defined as airflow obstruction in persons aged 40 yr and older.
Income was classified by ranking according to gender and age group. Household income was divided into quartiles. Subjects who had consumed less than 5 packs of cigarettes during their lifetime were defined as never-smokers, whereas those who had consumed more than 5 packs were defined as smokers. The database of the 4th KNHANES included the results of various health-related questionnaires and laboratory tests. Patients were defined as having a chronic disease (allergic rhinitis, arthritis, coronary heart disease, depression, GI ulcer, history of pulmonary tuberculosis, lung cancer, or osteoporosis) if they answered affirmatively to the question, "Have you had [name of chronic disease] lasting 6 months or more that was diagnosed by a health professional?" Anemia in men, nonpregnant women, and pregnant women was defined as hemoglobin concentrations less than 13 g/dL, 12 g/dL, and 11 g/dL, respectively. Underweight was defined as a body mass index (BMI) < 18.5 kg/m2, and overweight as a BMI ≥ 25 kg/m2. Subjects taking glucose lowering medication or with a fasting blood glucose concentration ≥ 126 mM/L were defined as having diabetes mellitus; subjects taking lipid-lowering medication or with a low density lipoprotein cholesterol (LDL-C) concentration ≥ 130 mg/dL were defined as having dyslipidemia; and subjects taking anti-hypertensive medication or with a diastolic blood pressure ≥ 90 mmHg were defined as having hypertension.
Data analysis
Categorical variables were analyzed using the chi-square test, and means were compared using Student's t-tests. All values are presented as means ± standard deviations. We constructed a logistic regression model with COPD as the dependent variable and age, sex, economic status, and smoking history as independent variables. Results are reported as odds ratios (ORs) with 95% confidence intervals (CIs). A P value less than 0.05 was defined as statistically significant. All statistical analyses were performed with SPSS version 18.0 software (SPSS Inc, Chicago, IL, USA).
Ethics statement
This study was approved by the institutional review board of the Korea Centers for Disease Control and Prevention (approval number, 2008-01EXP-01-C). Informed consent was obtained from each study participant.
RESULTS
Prevalence and severity of COPD subjects
We assessed 4,703 subjects aged ≥ 40 yr (mean age, 54.4 yr); of these 3,442 (73.2%) were assessed by spirometry, and 2,501 (53.2%) met the ATS/ERS criteria for acceptability and reproducibility. Of these 2,501 subjects 1,823 (71.9%; 36.9% male; 63.1% female) were normal and 354 (10.4%; 67.2% male; 32.8% female) had COPD, defined as FEV1/FVC < 0.7, most of mild to moderate severity (Fig. 1).
Fig. 1.
Flow of inclusion and exclusion.
Comorbidities in COPD subjects
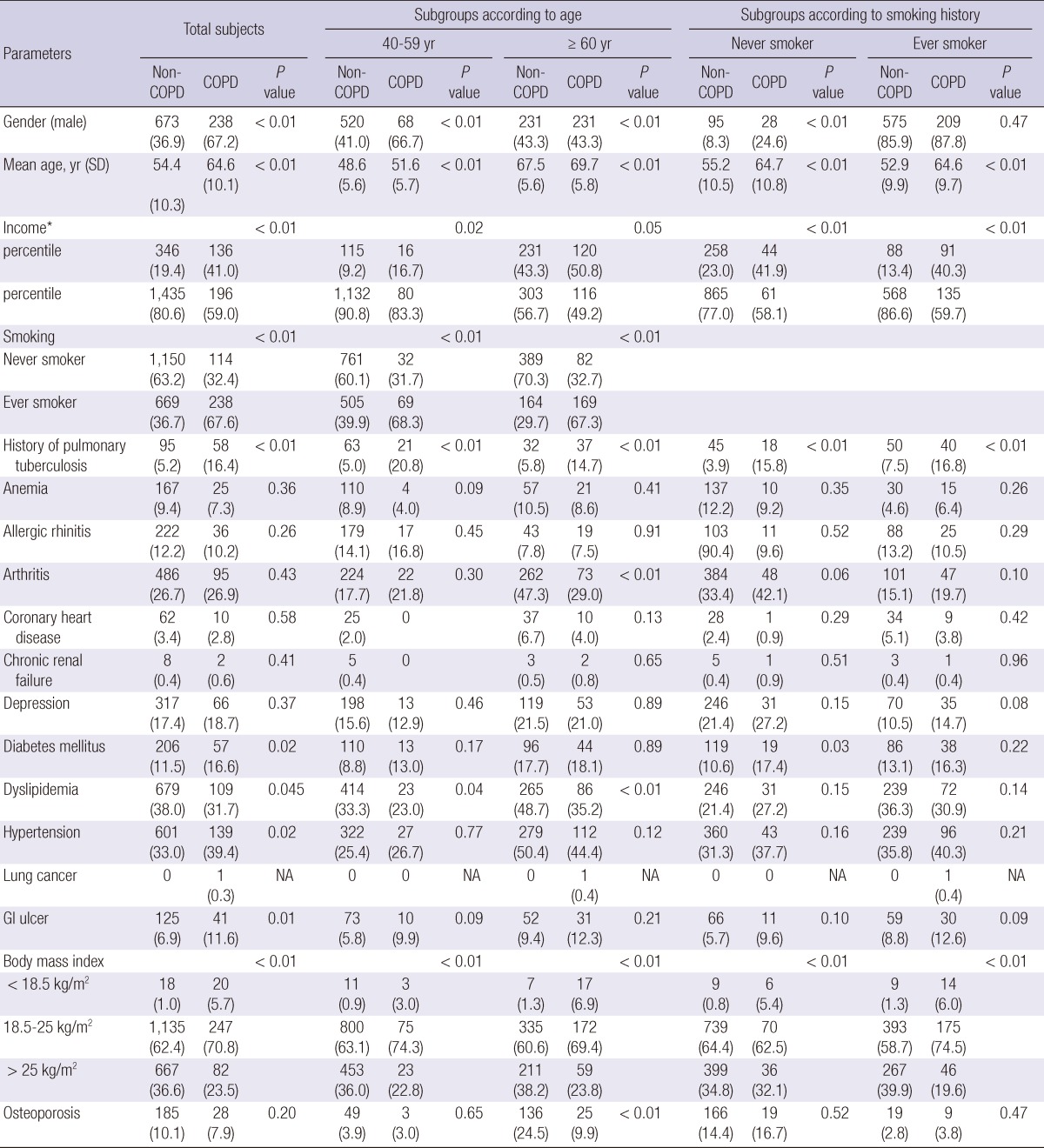
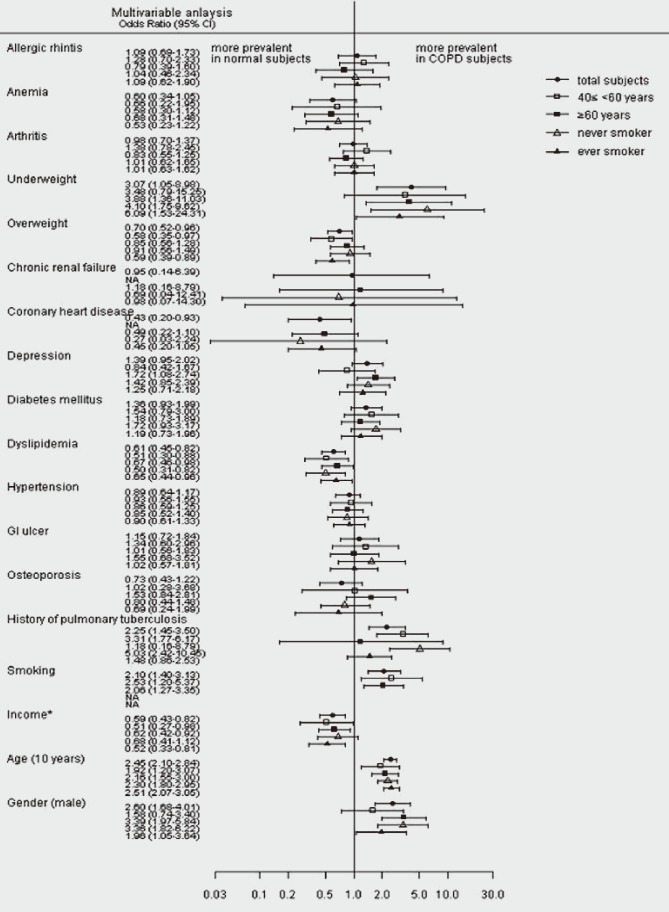
Table 1 compares the characteristics of normal and COPD subjects. The rates of diabetes, hypertension, gastrointestinal ulcers and underweight were higher, and the rate of dyslipidemia was lower, in COPD than in normal subjects. A multivariate analysis, after adjustment for gender, age, income, smoking and other comorbidities, to identify comorbidities independently associated with COPD showed that underweight (OR, 3.07; 95% CI, 1.05-8.98) was significantly more prevalent, and coronary heart disease (OR, 0.43; 95% CI, 0.20-0.93) and dyslipidemia (OR, 0.61; 95% CI, 0.45-0.82) were significantly less prevalent in COPD than in non-COPD subjects. Male sex, older age, lower income and smoking were also independently associated with COPD (Fig. 2).
Table 1.
Characteristics of subjects
Individuals aged ≥ 40 yr and a forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio < 0.7 (airflow obstruction) were retrospectively selected from the database of the 4th Korean National Health and Nutrition Examination Survey. *House income was divided into quartiles, with income compared with the lowest quartile. Patients who had consumed fewer than 5 packs of cigarettes during their lifetime were defined as never-smokers; those who had consumed more than 5 packs were defined as smokers. Patients with allergic rhinitis, arthritis, coronary heart disease, GI ulcer, depression, osteoporosis, and a history of pulmonary tuberculosis were defined as having the respective disease for ≥ 6 months after diagnosis by a health professional. Anemia was defined as subjects on medication or meeting the criteria of hemoglobin < 13 g/dL (men), < 12 g/dL (nonpregnant women), < 11 g/dL (pregnant women). Underweight and overweight were defined as body mass indexes (BMI) < 18.5 kg/m2 and ≥ 25 kg/m2, respectively; diabetes as fasting blood glucose ≥ 126 mg/dL, dyslipidemia as low density lipoprotein cholesterol ≥ 130 mg/dL, and hypertension as diastolic blood pressure ≥ 90 mmHg. Data are presented as number of subjects, with percentages in parentheses, except for age, which is presented as mean and standard deviationin parentheses. P value comparing individuals with normal and obstructive spirometry results, using the chi-square test. NA, not available; GI, gastrointestinal.
Fig. 2.
Odds ratios of comorbidities for COPD. Odds ratios for COPD were calculated for males (vs females), age in 10 yr intervals, and income relative to the lowest quartile. Results are reported as odds ratios and 95% confidence intervals from a logistic regression model fully adjusted for gender, age, income, cigarette smoking and comorbidities as dependent variables. Patients who had consumed fewer than 5 packs of cigarettes during their lifetime were defined as never-smokers; those who had consumed more than 5 packs were defined as smokers. Patients with allergic rhinitis, arthritis, coronary heart disease, GI ulcer, depression, osteoporosis, and a history of pulmonary tuberculosis were defined as having the respective disease for ≥ 6 months after diagnosis by a health professional. Anemia was defined as subjects on medication or meeting the criteria of hemoglobin < 13 g/dL (men), < 12 g/dL (nonpregnant women), < 11 g/dL (pregnant women). Underweight and overweight were defined as body mass indexes (BMI) < 18.5 kg/m2 and ≥ 25 kg/m2, respectively; diabetes as fasting blood glucose ≥ 126 mg/dL, dyslipidemia as low density lipoprotein cholesterol ≥ 130 mg/dL, and hypertension as diastolic blood pressure ≥ 90 mmHg. • Odds ratios of total COPD subjects compared with normal subjects, □ Odds ratios of middle-aged COPD subjects (40 ≤ and < 60 yr) compared with normal subjects, ▪ Odds ratios of older COPD subjects (≥ 60 yr) compared with normal subjects, ▵ Odds ratios of COPD of never smoker compared with normal subjects, ▴ Odds ratios of COPD with ever smoker compared with normal subjects. NA, not available; GI, gastrointestinal.
Comorbidities in COPD subjects aged 40-59 and ≥ 60 yr
Underweight was more prevalent and dyslipidemia was less prevalent in COPD subjects aged 40 to 59 yr than in non-COPD subjects after adjustment for gender, age, income, smoking and other comorbidities. Underweight and depression were more prevalent and dyslipidemia was less prevalent in COPD than non-COPD subjects aged ≥ 60 yr (Fig. 2).
COPD comorbidities in subgroups of never smokers and smokers
Underweight was more prevalent and dyslipidemia was less prevalent in both smokers and never smokers with than without COPD, after adjustment for gender, age, income and other comorbidities (Fig. 2).
Comorbidities in COPD according to the lower limits of normal criteria and non-asthmatic subjects
We analyzed the comorbidities of COPD using the lower limit of normal (LLN) criteria in the Korean population. COPD (LLN) was diagnosed after adjustment for gender, age, height, weight and other risk factors and comorbidities. Using these criteria, we found that underweight was significantly more prevalent and dyslipidemia was less prevalent in COPD than non-COPD subjects.
We also analyzed the comorbidities of COPD in subjects with airflow obstruction but without asthma as diagnosed by a physician. Underweight was more prevalent and dyslipidemia was less prevalent in COPD than non-COPD subjects after adjustment for gender, age, income and other comorbidities.
DISCUSSION
Our findings showed that underweight was significantly more prevalent, whereas coronary heart disease and dyslipidemia were less prevalent, in Korean subjects with than without COPD. To our knowledge, this study is the first population based-survey to identify the associations between COPD and its comorbidities, after adjustment for gender, age, income and other comorbidities, in an Asian population.
We found that the incidence of underweight might be higher in Asian than in Western COPD subjects (6). The mean BMI of COPD subjects in China and the Philippines was 23.3 kg/m2 and 24.9 kg/m2, respectively, whereas the mean BMI of COPD subjects in Western countries, including Austria, Germany, Canada and the USA, was over 25 kg/m2. These differences are likely due to differences in race and environmental and nutritional factors, suggesting the need for additional epidemiologic studies in Asian populations (7).
Cardiovascular heart disease is an important cause of death and hospitalization in COPD patients. Sin et al. have shown that moderate and severe COPD is associated with increased occurrence of ischemic changes on electrocardiogram (8). In the Towards a Revolution in COPD Health (TORCH) clinical trial, 27% of all deaths in subjects with moderate to severe COPD (FEV1 < 60%) were directly attributable to cardiovascular events (9). Risk factors for COPD-associated atherosclerotic cardiovascular effects include older age, male sex, smoking, dyslipidemia and hypertension, with low grade systemic inflammation being the most prominent link between COPD and cardiovascular disease.
However, in our study coronary heart disease was less prevalent in COPD than non-COPD subjects and this was true even after adjustment for age, sex, smoking and comorbidities. This result might be due to the different characteristics of study subjects who were randomly selected from a Korean population and among whom most showed milder airflow obstruction, with only 22 (6.6%) having an FEV1 below 50%.
Being similar to our result a study reported that COPD with mild and moderate airflow obstruction was not associated with ischemic heart disease (10). In China, cardiovascular disease was less prevalent in asymptomatic COPD subjects with less severe obstruction than in symptomatic COPD subjects (11).
Previous studies have reported that the prevalence of dyslipidemia was higher in COPD than non-COPD subjects (12). Although the mechanism has not been determined, it may be similar to that of cardiovascular disease. In the Kaiser Permanente Medical Care Program of Northern California, coronary artery disease and dyslipidemia diagnosed with International Classification of Disease, ninth revision is prevalent in COPD subjects having hospitalization than control subjects (13).
However, in our study dyslipidemia was less prevalent in COPD than non-COPD subjects and this was true even after adjustment for gender, age, income and other comorbidities, a finding similar to that in a Canadian study of COPD (14). The negative association between dyslipidemia and COPD in our population might be also due to the mild severity of airway obstruction in our subjects or/and due to racial/ethnic differences (10).
We compared severe to very severe COPD subjects with FEV1 of predicted below 50% with normal subjects (data not shown in the result section). The mean LDL-C level of severe to very severe COPD subjects was higher than that of normal subjects. A univariate analysis, dyslipidemia was more prevalent in severe to very severe COPD subjects than normal subjects, while dyslipidemia was less prevalent in mild to moderate COPD subjects with FEV1 predicted above 50% than normal subjects. We did a similar comparison for the coronary heart disease (data not shown). We could not find the relation between severity of COPD and coronary heart disease probably because there were very few subjects who had both severe to very severe COPD and coronary heart disease in this study. Because this survey represented the general population in Korean, the proportion of COPD subjects with severe airflow obstruction is small. It was known that dyslipidemia is strongly associated with coronary heart disease. It can explain the negative of association between coronary heart disease and COPD in this population-based study. The large-scaled population based survey was needed including the medical record of subjects to analyze relation the severity of COPD and coronary heart disease.
We also performed subgroup analyses of older (≥ 60 yr) COPD subjects and never-smokers. We found that depression was significantly more prevalent in COPD than non-COPD subjects (≥ 60 yr) after adjustment for gender, age, income and other comorbidities. Among never-smokers, a history of pulmonary tuberculosis was significantly more prevalent in COPD than non-COPD subjects after these adjustments. Studies of patients with chronic diseases, such as coronary heart disease, diabetes mellitus and hypertension, have found that depression has adverse effects on poor functional performance and mortality (15). COPD has also been associated with depression in older subjects (16). Inflammatory cytokines such as IL-6 can affect the central nervous system, and TNF-α was found to be a biomarker for the association between systemic inflammation and depression in subjects with COPD (17).
Systemic inflammation may underlie the mechanism of comorbidities of COPD. Cigarette smoke can cause lung and systemic inflammation, systemic oxidative stress, marked changes in vasomotor and endothelial function and enhanced circulating concentrations of several pro-coagulant factors. Animal and in vitro models have shown that pulmonary inflammation can lead to systemic inflammation (18). Moreover, serum concentrations of markers of systemic inflammation, such as high-sensitivity C-reactive protein, were found to be higher in patients with COPD than in normal subjects (19).
Pulmonary tuberculosis remains one of the most important pulmonary diseases in Asia. This disease can destroy the lung parenchyma, causing airflow obstruction (20). In addition, bronchial stenosis may result from endobronchial involvement of tuberculosis. Damage to the parenchyma and airways due to pulmonary tuberculosis can result in airflow limitation. We therefore analyzed comorbidities of COPD after adjustment for a history of pulmonary tuberculosis.
Our study had several strengths, including its use of data from a nationwide survey, which was designed systematically using a stratified random sampling of the Korean population and was performed by well-trained interviewers and medical professionals. In addition, our use of criteria for acceptability and reproducibility resulted in high quality control in the performance of spirometry. We also analyzed the comorbidities of COPD by multivariate regression analysis after adjustment for gender, age, income and other comorbidities. This likely minimized the effects of confounders and interactions with other chronic diseases.
Nevertheless, this study had some limitations. First, its cross-sectional design limited our ability to establish causal relationships between variables. Second, we did not obtain results of chest radiography. Because airflow obstruction may be caused by other diseases, such as bronchiectasis and pulmonary tuberculosis, we may have overestimated the number of subjects with COPD. Third, we utilized data from pre-bronchodilator tests to diagnose COPD and its severity. The fifth KHANES is being conducted using of bronchodilator and airflow obstruction defined by the relative lower limits of normal. So the comorbidities could be defined more clearly with the future analysis of the fifth KHANES data.
In conclusion, underweight might be more prevalent but coronary heart disease and dyslipidemia are less prevalent in Koreans with than without COPD in population setting.
Footnotes
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health and Welfare, Republic of Korea (A102065) in 2011.
References
- 1.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 2.Fabbri LM, Rabe KF. From COPD to chronic systemic inflammatory syndrome? Lancet. 2007;370:797–799. doi: 10.1016/S0140-6736(07)61383-X. [DOI] [PubMed] [Google Scholar]
- 3.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163:1256–1276. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 4.Yoo JW, Hong Y, Seo JB, Chae EJ, Ra SW, Lee JH, Kim EK, Baek S, Kim TH, Kim WJ, et al. Comparison of clinico-physiologic and CT imaging risk factors for COPD exacerbation. J Korean Med Sci. 2011;26:1606–1612. doi: 10.3346/jkms.2011.26.12.1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hwang YI, Yoo KH, Sheen SS, Park JH, Kim SH, Yoon HI, Lim SC, Lee SY, Park JY, Park SJ. Prevalence of chronic obstructive pulmonary disease in Korea: the reasult of fourth Korean National Health and Nutrition Examination Survey. Tuberc Respir Dis. 2011;71:328–334. doi: 10.1111/j.1440-1843.2011.01951.x. [DOI] [PubMed] [Google Scholar]
- 6.Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, Menezes AM, Sullivan SD, Lee TA, Weiss KB, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370:741–750. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 7.Tan WC, Ng TP. COPD in Asia: where East meets West. Chest. 2008;133:517–527. doi: 10.1378/chest.07-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sin DD, Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003;107:1514–1519. doi: 10.1161/01.cir.0000056767.69054.b3. [DOI] [PubMed] [Google Scholar]
- 9.McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax. 2007;62:411–415. doi: 10.1136/thx.2006.072348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Izquierdo JL, Martinez A, Guzman E, de Lucas P, Rodriguez JM. Lack of association of ischemic heart disease with COPD when taking into account classical cardiovascular risk factors. Int J Chron Obstruct Pulmon Dis. 2010;5:387–394. doi: 10.2147/copd.s14063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu M, Yao WZ, Zhong NS, Zhou YM, Wang C, Chen P, Kang J, Huang SG, Chen BY, Wang CZ, et al. Asymptomatic patients of chronic obstructive pulmonary disease in China. Chin Med J (Engl) 2010;123:1494–1499. [PubMed] [Google Scholar]
- 12.Nussbaumer-Ochsner Y, Rabe KF. Systemic manifestations of COPD. Chest. 2011;139:165–173. doi: 10.1378/chest.10-1252. [DOI] [PubMed] [Google Scholar]
- 13.Sidney S, Sorel M, Quesenberry CP, Jr, DeLuise C, Lanes S, Eisner MD. COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest. 2005;128:2068–2075. doi: 10.1378/chest.128.4.2068. [DOI] [PubMed] [Google Scholar]
- 14.Curkendall SM, DeLuise C, Jones JK, Lanes S, Stang MR, Goehring E, Jr, She D. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann Epidemiol. 2006;16:63–70. doi: 10.1016/j.annepidem.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Wells KB, Rogers W, Burnam MA, Camp P. Course of depression in patients with hypertension, myocardial infarction, or insulin-dependent diabetes. Am J Psychiatry. 1993;150:632–638. doi: 10.1176/ajp.150.4.632. [DOI] [PubMed] [Google Scholar]
- 16.Yohannes AM, Baldwin RC, Connolly MJ. Depression and anxiety in elderly outpatients with chronic obstructive pulmonary disease: prevalence, and validation of the BASDEC screening questionnaire. Int J Geriatr Psychiatry. 2000;15:1090–1096. doi: 10.1002/1099-1166(200012)15:12<1090::aid-gps249>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 17.Al-shair K, Kolsum U, Dockry R, Morris J, Singh D, Vestbo J. Biomarkers of systemic inflammation and depression and fatigue in moderate clinically stable COPD. Respir Res. 2011;12:3. doi: 10.1186/1465-9921-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mukae H, Vincent R, Quinlan K, English D, Hards J, Hogg JC, Van Eeden SF. The effect of repeated exposure to particulate air pollution (PM10) on the bone marrow. Am J Respir Crit Care Med. 2001;163:201–209. doi: 10.1164/ajrccm.163.1.2002039. [DOI] [PubMed] [Google Scholar]
- 19.Pinto-Plata VM, Mullerova H, Toso JF, Feudjo-Tepie M, Soriano JB, Vessey RS, Celli BR. C-reactive protein in patients with COPD, control smokers and non-smokers. Thorax. 2006;61:23–28. doi: 10.1136/thx.2005.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med. 1989;83:195–198. doi: 10.1016/s0954-6111(89)80031-9. [DOI] [PubMed] [Google Scholar]