Abstract
Complex regional pain syndrome affects the quality of life of the patient. The aim of this study was to investigate the epidemiological features of this syndrome and evaluate its effect on the patient's working life. We demonstrated that the disease has a male preponderance and is 3 times more likely to affect the lower extremities. In this study, 11 participants (20%) retained their employment, whereas 44 (80%) became unemployed. Mean age and pain score were lower in the employment group than in the unemployment group (29.1 ± 16.8 yr vs 40.1 ± 12.6 yr, P = 0.021, and 4.5 ± 2.9 vs 7.0 ± 2.0, P = 0.002, respectively). Subjects diagnosed within 8 months (P = 0.044), those who had achieved higher levels of education (P = 0.028), and those working in white-collar jobs (P = 0.011) had higher employment-retention rates. Therefore, patients must manage their jobs (lower physical demand and decrease the number of working hours) if they are to improve their occupational life. To achieve satisfactory outcomes and a high employment-retention rate, clinicians must be aware of the importance of an early diagnosis (within 8 months), appropriate treatment, and a reduction in the patient's pain score.
Keywords: Complex Regional Pain Syndromes, Work, Employment
INTRODUCTION
Complex regional pain syndrome (CRPS) is a painful and disabling disorder, which can affect one or more of the body's extremities (1). CRPS is characterized by pain (spontaneous pain, hyperalgesia, allodynia), active and passive movement disorders (including an increased physiological tremor), abnormalities in the regulation of blood flow and sweating, edema of skin and subcutaneous tissues, temperature asymmetry, skin color changes, and trophic changes to the skin and subcutaneous tissues (2). Two recent epidemiological studies reported that the syndrome has an incidence rate of 5.5 per 100,000 persons in the USA (3) and a prevalence of 26.2 per 100,000 persons in the Netherlands (4).
Typically, CRPS is chronic in nature and resistant to the currently available treatment modalities. The disease significantly affects the quality of life and daily functioning of the patient as it causes severe pain with resultant psychosocial and socioeconomic adverse effects. Approximately 75% of patients report that the disease interferes substantially with general activity, mood, normal work capabilities, and recreational activities (5-7). Many CRPS patients, especially younger and middle-aged individuals, will be a part of the work force at the time of diagnosis. For these individuals, maintaining their work status is an important aspect of their quality of life and societal reintegration. The objective of this study was to assess the epidemiological features of CRPS and, for the first time in Korea, investigate the effects of the disease on working life.
MATERIALS AND METHODS
The study initially enrolled 63 patients who were diagnosed with CRPS and treated at our pain center from September 2010 to March 2011, although 8 patients were subsequently excluded from the analysis because they were unemployed before diagnosis. We then performed a survey and retrospective analysis of the remaining participants and categorized the participants into groups according to their employment status so that we could compare the difference between employed and unemployed patients. Patients who were continuously employed or had recently returned to work after a short period of unemployment were enrolled into the employed group.
Medical records were reviewed for each patient, and an interview was conducted to determine their current status of employment. The proposed modified International Association of the Study of Pain (IASP) research diagnostic criteria for CRPS was used to attain the diagnoses in our pain center (6). Demographical data including events, injury sites, interval between symptom onset and diagnosis, pain intensities, type of health insurance, employment status, type of occupation, level of education, and the number of workdays lost were recorded and assessed for each patient. Pain intensity was rated using an 11-point verbal numerical rating scale (VNRS; 0 = no pain and 10 = imaginarily most severe pain).
Group comparisons (employed vs unemployed) were analyzed using an independent sample t-test. A Pearson chi-square test was used to analyze categorical data such as gender, pain extremity, pain side, inciting factor, type of health insurance, level of education, type of occupation, and individual CRPS signs. Subsequently, factors that were related to an employment-retention status were analyzed with logistic regression. SPSS (version 17.0; SPSS Inc., Chicago, IL, USA) was used for statistical analysis, and a P value of less than 0.05 was considered statistically significant.
Ethics statement
This study was approved by the institutional review board of Seoul National University Hospital (IRB No. H-1008-048-326), and written informed consent was obtained from all the participants.
RESULTS
Of the 63 patients who were diagnosed with CRPS in our clinic, 55 were enrolled in the study; 32 patients (58.2%) were male and 23 (41.8%) were female. The average age of the patients was 39.2 ± 15.0 (range 14-76) yr. Of the inciting events, 43 (78.2%) were trauma-related (e.g., following a fall, crushing injury, or contusion), 11 (20.0%) were surgery-related, and 1 (1.8%) had no obvious inciting event (spontaneous). In total, 51 patients (92.7%) were diagnosed with CRPS type I, while the remaining 4 (7.3%) were diagnosed with CRPS type II. Of all the patients in the study, 38 (69.1%) complained of pain in the lower limbs, 12 (21.8%) reported pain in the upper limbs, and 5 (9.1%) experienced pain in their upper and lower limbs. The right side was affected in 20 participants (36.3%), the left side was affected in 29 participants (52.7%), and both sides were affected in the remaining 6 participants (10.9%) (Table 1). The detailed localization sites recorded for each patient were as follows: 7 were in the right upper limbs (12.7%), 6 were in the left upper limbs (10.9%), 13 were in the right lower limbs (23.6%), 19 were in the left lower limbs (34.5%), 5 were in the right and left lower limbs (9.1%), 4 were in the left upper and lower limbs (7.3%), and 1 was in the left and right upper and lower limbs (1.8%).
Table 1.
Various characteristics of CRPS patients

Data are expressed as number of cases and percentage. A percentage is a ratio of a number to each group (employed and unemployed). *P < 0.05.
Eleven patients (20.0%) retained their employment status, whereas 44 patients (80.0%) became unemployed. Of the patients who continued to work, 4 had maintained their work after the onset of CRPS and 7 had returned to work following a period of unemployment. Of note, 2 of the patients who had returned to work were employed by a different part of their company or had a new occupation, whereas 9 patients retained their position.
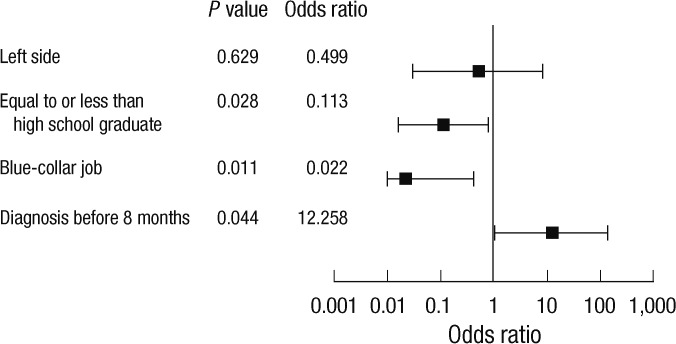
The mean duration from the diagnosis of CRPS to the time of the interview was 1,083.1 ± 743.4 (range, 252-3,710) days. The mean number of workdays lost owing to CRPS was 897.5 ± 796.5 (range, 0-3,640) days among all the patients, and the mean duration from the inciting event to unemployment was 25.5 ± 79.6 (range, 0-365) days. In 7 patients who returned to work after being unemployed, the average time taken for their employment status to change was 271.4 ± 212.9 (range, 30-660) days. The mean duration from the inciting event to the development of CRPS symptoms was 12.8 ± 21.9 (range, 0-60) days and from the developed symptoms to occur to a diagnosis of CRPS being confirmed, the mean duration was 406.7 ± 566.0 (range, 13-2,813) days. The demographical data, affected sites, and inciting factors were compared for the 2 groups (employed vs unemployed). There were no significant differences between genders, extremities, and inciting factors in both groups. Patients in whom the right side was affected were more likely to return to work (Table 1). However, after controlling for the period from onset to diagnosis (before or after 8 months) and the type of occupation of the patient, an affected right side was not an independent variable for maintaining employment (Fig. 1).
Fig. 1.
Results of logistic regression analysis. Pain site was categorized by the side that was affected, either the left or right. The level of education of the patient was defined as follows: "equal to or less than high-school graduate" or "higher than high-school graduate." Occupation was divided into 2 types: white-collar jobs and blue-collar jobs.
No significant differences were observed in the weight and height of the patients or the number of days from the diagnosis of CRPS to the time of the interview between the 2 groups. The number of daily working hours before CRPS onset was similar between the 2 groups; however, the number of days per week spent working before CRPS onset was lower in the employment group compared with the unemployment group (5.2 ± 0.5 vs 5.9 ± 1.2; P = 0.009). The mean age of the patients was significantly lower in the employment group (29.1 ± 16.8 vs 40.1 ± 12.6 yr; P = 0.021). Although pain score did not vary significantly between the 2 groups at the time of disease onset, it was relatively higher at time of interview in the unemployment group (4.5 ± 2.9 vs 7.0 ± 2.0; P = 0.002) (Table 2).
Table 2.
Various characteristics of CRPS patients
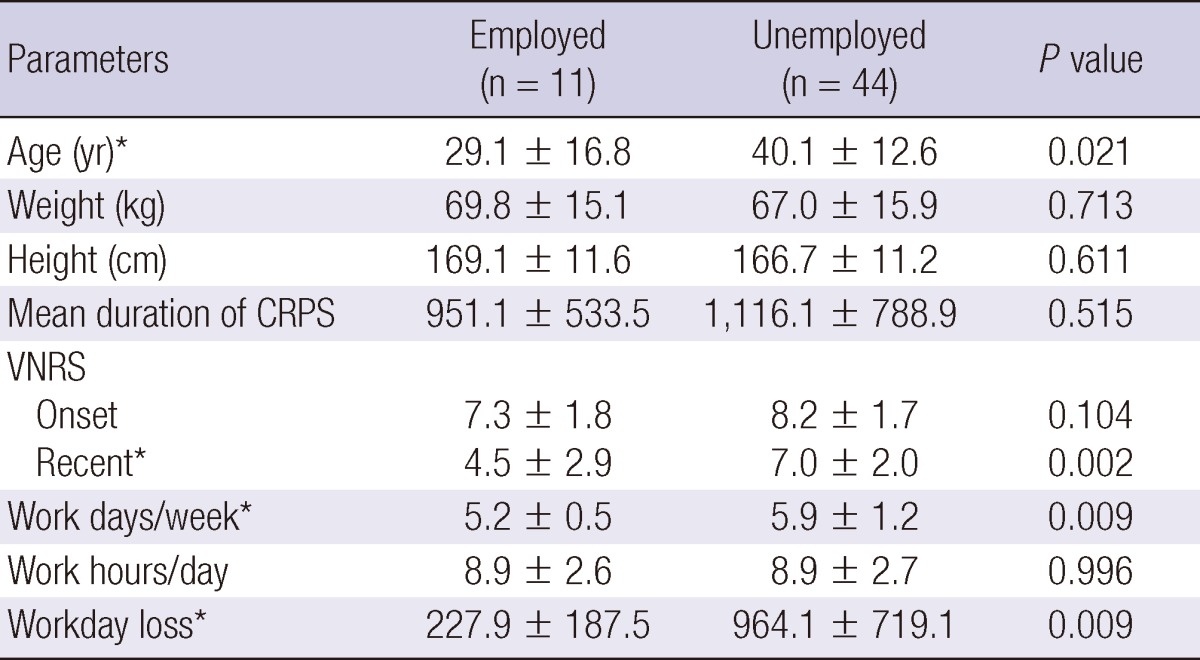
Values are given as the mean ± standard deviation. Mean duration of CRPS, the days from diagnosis of CRPS to the time of interview. VNRS, 0 = no pain, 10 = imaginarily most severe pain. Recent, at time of interview; Workday loss, the days of unemployment. *P < 0.05.
Patients who were diagnosed within 8 months (240 days) were more likely to be employed than patients diagnosed after 8 months (P = 0.014). In addition, patients with white-collar jobs were more likely to be employed than those with blue-collar jobs (P = 0.000). In this study, professions that were classified as white-collar jobs included teachers, clerical workers, financial managers, and students, whereas blue-collar jobs included manual-labor workers such as construction workers, restaurant workers, delivery men, drivers, carpenters, farmers, and housekeepers. Patients who had achieved a higher level of education also had a higher rate of employment (P = 0.006). However, the rates of employment were not related to the types of health insurance of the patients (Table 3). Finally, there were no significant differences observed in the positive signs of CRPS between the 2 groups (Table 4).
Table 3.
Duration of diagnosis, insurance, level of education, occupational characteristics of CRPS patients
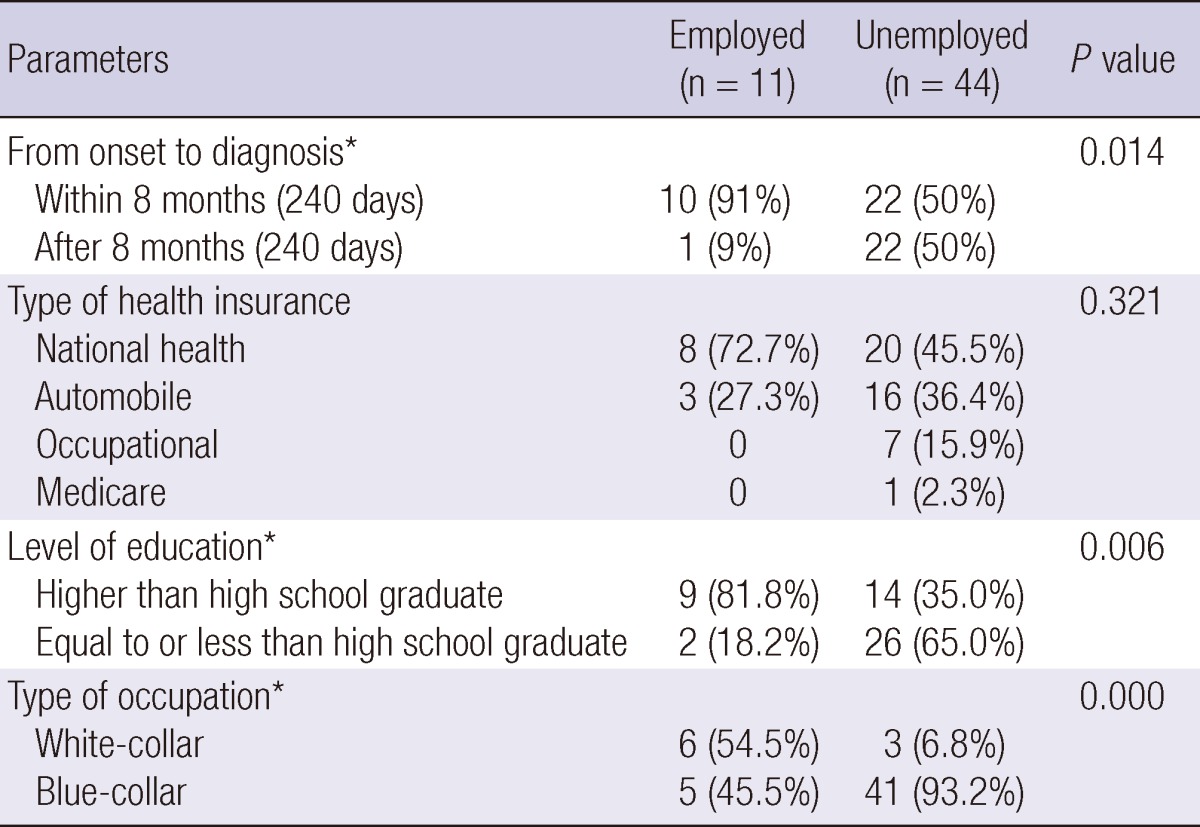
Data are expressed as number of cases and percentage. A percentage is a ratio of a number to each group (employed and unemployed). From onset to diagnosis, the days from onset of symptom to diagnosis of CRPS. *P < 0.05.
Table 4.
Signs at time of first visit of CRPS patients
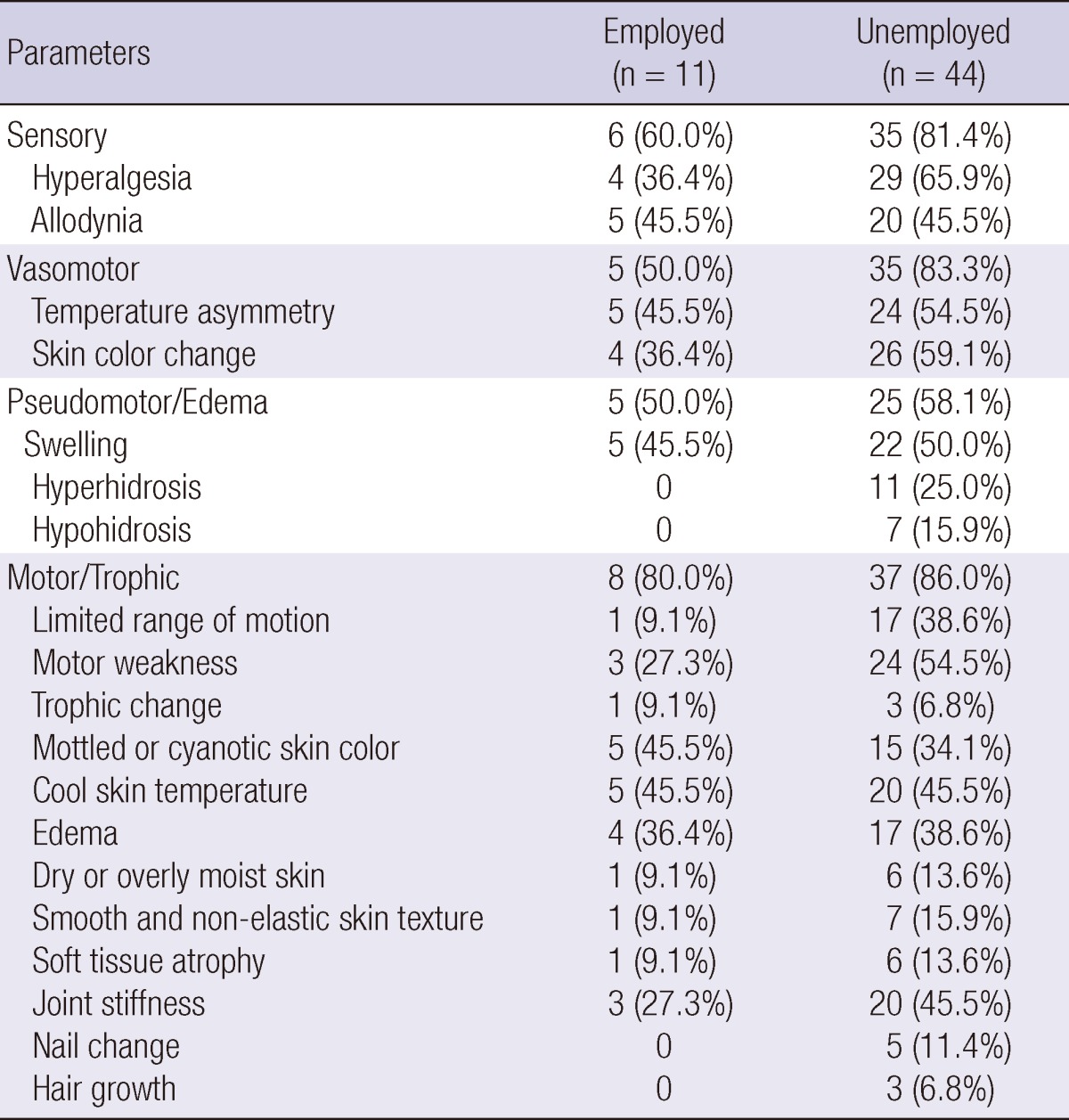
Data are expressed as number of cases and percentage. A percentage is a ratio of a number to each group (employed and unemployed).
The logistic regression analysis showed that patients had achieved a higher level of education, had a white-collar job, and were diagnosed within 8 months were more likely to be employed (Fig. 1).
DISCUSSION
The demographical data obtained by this study differed from the data that have been published in previous studies, where CRPS was reported to occur more frequently in the upper extremities and predominately affect females (3, 4, 8, 9). However, our data show a 1.3:1 male preponderance, and the lower extremities are nearly 3 times more frequently affected. These results are similar to those published by a previous study in Korea (10). Previous studies were conducted almost entirely on Caucasians, and some studies found that Caucasians are more likely to be affected by CRPS (3, 8, 11). Therefore, the different demographical results observed in our study may be attributable to racial differences. Although we wanted to compare our results with data obtained from other Asian countries, we could not find any suitable studies for comparison.
The outcomes of CRPS range from self-limiting to chronic disease with poor functioning and quality of life (4, 12). The rate of employment in our study was 20%, which is significantly lower than the rate reported in previous studies (69%-87.7%) (13-15).
In our study, good prognostic factors for employment retention were a younger age, a lower pain score after treatment, fewer days per week spent at work, a diagnosis within 8 months of onset, a higher level of education, and a white-collar occupation of the patient. Early diagnosis and management are important if positive CRPS patient outcomes are to be achieved (15-17). In our study, the average time taken for CRPS to be diagnosed was 406.7 ± 566.0 days, which is longer than the period reported by a previous study (123.0 days) (15). In addition, patients who were diagnosed after 8 months of symptom onset were less likely to be employed. The pathophysiology of CRPS is still unclear, and treatment remains largely empirical. During treatment, a clinician aims to relieve pain, accomplish functional recovery, and achieve psychological improvement in the patient. Therefore, many clinicians start early multifactorial treatment as soon as possible after CRPS has been diagnosed (18). If the diagnosis of CRPS is delayed, the patient may suffer from extreme pain and will not receive proper treatment during this time, which may lead to a poor prognosis. Prolonged pain may lead to sensitization changes in the peripheral and central nociceptive pathways. In addition, the resultant central sensitization can lead to increased pain intensity (19). Therefore, we believe that the delayed diagnosis of CRPS in some of our patients was the cause of higher rates of unemployment and was considered a poor prognostic factor.
In our study, the clinical signs of CRPS after injury, as well as pain score at the onset of the disease, did not vary between the groups. Most CRPS patients suffer from characteristic symptoms and signs. De Mos et al. (13) described that, even after treatment, there is a high prevalence rate of CRPS symptoms and signs in patients. However, the pain score after treatment was significantly lower in the employment group in this study. In other words, the curative value of this disease is related to the rate of employment. Therefore, CRPS outcome strongly influences employment status, and effective treatment should be emphasized.
MacKenzie et al. (20) reported that a higher number of patients returning to work following injury is related to many factors, including lower pain intensities, higher levels of education, higher family incomes, high levels of social support, absence of alcoholism, increased job stability and flexibility, white-collar employment, and employment by lower physically demanding jobs with good benefits. In our study, the rate of employment of patients in white-collar jobs was 45 times higher than that of patients in blue-collar jobs. In addition, the rate of employment of patients who had attended college was 9 times higher than that of other patients. MacKenzie et al. (20) demonstrated that patients had higher employment ratio if they were more aware of disease and job mobility. Furthermore, we consider their job to be of relatively lower physical demand and higher job stability. Because most patients cannot use their aching limb, most are forced to change their occupation to protect the lesion. Lower physical demand and higher job stability could lead to patients with a higher level of education and in white-collar jobs to retain their occupations.
The mean number of workdays lost among all patients was 897.5 ± 796.5 days, and among employed patients, it was 227.9 ± 187.5 days. In comparison with a previous study, this duration was relatively long (187.5 ± 107.4 days) (15). The mean duration from the inciting event to the patient resigning from their job was 25.5 ± 79.6 (range, 0-365) days, and 73.2% of patients left their job immediately after the inciting event. Medical bills may be even more financially challenging to CRPS patients, as patients may struggle to pay the medical expenses during periods of reduced income. A previous study demonstrated that family income and expenditures were greatly affected by CRPS (21), and thus, the total social and economic impact of CRPS may be significant.
In our study, the rate of employment in CRPS patients was 20%, which is significantly lower than expected. Most CRPS patients may experience unnecessary suffering due to high pain intensity, economic problems, and a poor quality of life. To improve the occupational life of a patient with CRPS, it is necessary for the patients to lower the physical demand and strain of their occupation or decrease the number hours spent working. Clinicians must be aware that a relatively early diagnosis (within 8 months), proper treatment, and minimizing the pain score of CRPS are important for obtaining satisfactory clinical outcomes and a high employment ratio.
References
- 1.de Mos M, Sturkenboom MC, Huygen FJ. Current understandings on complex regional pain syndrome. Pain Pract. 2009;9:86–99. doi: 10.1111/j.1533-2500.2009.00262.x. [DOI] [PubMed] [Google Scholar]
- 2.Jänig W, Baron R. Complex regional pain syndrome: mystery explained? Lancet Neurol. 2003;2:687–697. doi: 10.1016/s1474-4422(03)00557-x. [DOI] [PubMed] [Google Scholar]
- 3.Sandroni P. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain. 2003;103:199–207. doi: 10.1016/s0304-3959(03)00065-4. [DOI] [PubMed] [Google Scholar]
- 4.de Mos M, Debruijn A, Huygen F, Dieleman J, Stricker B, Sturkenboom M. The incidence of complex regional pain syndrome: a population-based study. Pain. 2007;129:12–20. doi: 10.1016/j.pain.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Galer BS, Henderson J, Perander J, Jensen MP. Course of symptoms and quality of life measurement in complex regional pain syndrome: a pilot survey. J Pain Symptom Manage. 2000;20:286–292. doi: 10.1016/s0885-3924(00)00183-4. [DOI] [PubMed] [Google Scholar]
- 6.Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;8:326–331. doi: 10.1111/j.1526-4637.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 7.Correll GE, Maleki J, Gracely EJ, Muir JJ, Harbut RE. Subanesthetic ketamine infusion therapy: a retrospective analysis of a novel therapeutic approach to complex regional pain syndrome. Pain Med. 2004;5:263–275. doi: 10.1111/j.1526-4637.2004.04043.x. [DOI] [PubMed] [Google Scholar]
- 8.Allen G, Galer BS, Schwartz L. Epidemiology of complex regional pain syndrome: a retrospective chart review of 134 patients. Pain. 1999;80:539–544. doi: 10.1016/S0304-3959(98)00246-2. [DOI] [PubMed] [Google Scholar]
- 9.Schwartzman RJ, Kerrigan J. The movement disorder of reflex sympathetic dystrophy. Neurology. 1990;40:57–61. doi: 10.1212/wnl.40.1.57. [DOI] [PubMed] [Google Scholar]
- 10.Choi YS, Lee MG, Lee HM, Lee CJ, Jo JY, Jeon SY, Lee SC, Kim YC. Epidemiology of complex regional pain syndrome: a retrospective chart review of 150 Korean patients. J Korean Med Sci. 2008;23:772–775. doi: 10.3346/jkms.2008.23.5.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ciccone DS, Bandilla EB, Wu W. Psychological dysfunction in patients with reflex sympathetic dystrophy. Pain. 1997;71:323–333. doi: 10.1016/s0304-3959(97)00009-2. [DOI] [PubMed] [Google Scholar]
- 12.Galer BS, Henderson J, Perander J, Jensen MP. Course of symptoms and quality of life measurement in complex regional pain syndrome: a pilot survey. J Pain Symptom Manage. 2000;20:286–292. doi: 10.1016/s0885-3924(00)00183-4. [DOI] [PubMed] [Google Scholar]
- 13.de Mos M, Huygen FJ, van der Hoeven-Borgman M, Dieleman JP. Outcome of the complex regional pain syndrome. Clin J Pain. 2009;25:590–597. doi: 10.1097/AJP.0b013e3181a11623. [DOI] [PubMed] [Google Scholar]
- 14.Duman I, Dincer U, Taskaynatan MA, Cakar E, Tugcu I, Dincer K. Reflex sympathetic dystrophy: a retrospective epidemiological study of 168 patients. Clin Rheumatol. 2007;26:1433–1437. doi: 10.1007/s10067-006-0515-8. [DOI] [PubMed] [Google Scholar]
- 15.Kiralp MZ, Dincer U, Cakar E, Dursun H. Complex regional pain syndrome: epidemiologic features, treatment approaches, workday loss and return to work/disability ratios. Turk J Rheumatol. 2009;24:1–5. [Google Scholar]
- 16.Li Z, Smith B, Smith T, Koman L. Diagnosis and management of complex regional pain syndrome complicating upper extremity recovery. J Hand Ther. 2005;18:270–276. doi: 10.1197/j.jht.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Ok SJ, Yang JY, Son JH, Jeong WJ, Lee YS, Kim WY, Park YC. Management of complex regional pain syndrome type 1 with total spinal block. Korean J Pain. 2010;23:70–73. doi: 10.3344/kjp.2010.23.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raja SN, Grabow TS. Complex regional pain syndrome I (reflex sympathetic dystrophy) Anesthesiology. 2002;96:1254–1260. doi: 10.1097/00000542-200205000-00031. [DOI] [PubMed] [Google Scholar]
- 19.Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288:1765–1768. doi: 10.1126/science.288.5472.1765. [DOI] [PubMed] [Google Scholar]
- 20.MacKenzie EJ, Morris JA, Jr, Jurkovich GJ, Yasui Y, Cushing BM, Burgess AR, DeLateur BJ, McAndrew MP, Swiontkowski MF. Return to work following injury: the role of economic, social, and job-related factors. Am J Public Health. 1998;88:1630–1637. doi: 10.2105/ajph.88.11.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kemler MA, Furnee CA. The impact of chronic pain on life in the household. J Pain Symptom Manage. 2002;23:433–441. doi: 10.1016/s0885-3924(02)00386-x. [DOI] [PubMed] [Google Scholar]