Abstract
The goal of this study was to determine how much the formation of tetanus antibody is influenced after a single injection of tetanus vaccine (Td) and the simultaneous injection of tetanus vaccine with tetanus immunoglobulin (TIG). All of the healthy adult volunteers were divided into two groups: group 1 (Td only) and group 2 (Td plus TIG). Two hundred thirty seven volunteers were enrolled. When the baseline antibody titer, gender and age were adjusted, the geometric mean titers (GMTs) of the tetanus antibody (group 1 vs group 2) was 0.8438 IU/mL vs 0.5684 IU/mL at 4 weeks (P = 0.002), 0.4074 IU/mL vs 0.3217 IU/mL at 6 months (P = 0.072) and 0.3398 IU/mL vs 0.2761 IU/mL at 12 months (P = 0.140) after injection, respectively. The formation of tetanus antibody after tetanus vaccination is not influenced by TIG at the late period and in adults below the age of 50 yr, but there are significant differences between the two groups at the early period of 4 weeks after vaccination and for the patients over 60 yr.
Keywords: Tetanus, Tetanus Toxoid, Immunoglobulins
INTRODUCTION
Despite efforts paid by the World Health Organization and the government of developing countries, tetanus persists as a global health problem. Tetanus prophylaxis after injury had been introduced in US Immunization Practices Advisory Committee (ACIP) guideline and this guideline has been used in emergency departments (EDs) (1). However, some studies have shown that physician compliance with the guideline for tetanus prophylaxis according to the past vaccination history and the kind of wound is very low and their decisions were sometimes incorrect (2-4). The reasons for physician noncompliance with the ACIP guideline are likely due to a lack of familiarity with the guideline or failure to document the appropriate history (3).
In a busy and overcrowded ED, many emergency physicians are unable to get sufficient medical information of patients on the past tetanus vaccination history and individual immunity. When an injured patient visits the ED, unnecessary injection of tetanus immunoglobulin (TIG) may cause side effects and also increase the medical expense (5). Further, the opportunity of assessing a rising tetanus antibody titer may be missed after simultaneous injection of tetanus-diphtheria vaccine (Td) and TIG. According to age, the elevation of the tetanus antibody titer after tetanus prophylaxis might be not equivalent because of different levels of basal immunity and the time-interval of the last tetanus vaccination. Therefore, we wanted to determine whether TIG influences the level of tetanus antibody after simultaneous tetanus vaccination according to age and the time-interval of the last tetanus vaccination.
MATERIALS AND METHODS
Vaccine and immunoglobulin
Tetanus and diphtheria toxoid vaccine (Td-pur, Norvatis, Marburg, Germany) and tetanus immunoglobulin (Hypertet; Green Cross, Seoul, Korea) were used in this study. The Td vaccine was the licensed formulation that has been used for over 5 yr and it contains not less than 20 international unit (IU) per 0.5 mL dose. TIG has anti-tetanus human immunoglobulin 250 IU per 1 mL.
Participants
A total of 237 healthy adult volunteers who were over 20 yr old were enrolled and immunized in one emergency center of an academic teaching hospital. All the participants made lists of answers to questionnaire about the variables of age, gender, previous vaccination or a prophylaxis history, and military service.
Study design and procedures
This study was a randomized, controlled clinical trial. The participants were divided into different age groups: twenties (20-29 yr), thirties (30-39 yr), forties (40-49 yr), fifties (50-59 yr) and over sixty (60 yr). Some of the subjects, typically those in their twenties, already had high tetanus titers on account of previous tetanus at the beginning of military service, and a relatively short time-interval from the last child vaccination, and those subjects who had a high or adequate tetanus antibody titer might be disaffiliated in the case of a positive result after a field examination with a tetanus quick stick (TQS). The TQS is semiquantitative test of the tetanus antibody by using immunochromatography. The detection threshold asserted by the manufacturer is 0.2 international units (IU)/mL in the whole blood. For each age, all the subjects were allocated into two groups by using a computer-generated list of random numbers. Group 1 was composed of the subjects who had a single injection of Td vaccine and Group 2 was composed of the subjects who had a simultaneous injection of Td vaccine plus TIG. Blood samples (3 mL) were obtained just before and at 4 weeks, 6 months and 12 months after immunization, respectively. All the blood samples were centrifuged and serum was separated immediately, and stored at -70℃.
Serological assays
The tetanus antibody titers were determined by enzyme-linked immunosorbent assay (ELISA kit; Novalisa™, NovaTec, Dietzenbach, Germany) in accordance with the manufacturer's recommendation. The results were reported in IU/mL, and they were standardized by comparing them to calibrated World Health Organization (WHO) reference sera. The cutoff of these positive results was 0.1 IU/mL.
Statistical analysis
Statistical analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, North California, USA). Since, the distribution of tetanus antibody titers was skewed to the right, log-transformation for geometric mean titer (GMT) was done for its normality. The distribution of the demographic data between the two groups was compared using the independent t-test for the continuous numeric data and the chi-square test for the categorical data. The linear mixed model was used to evaluate the effect of simultaneous tetanus vaccination on the log (GMT). Fixed effects were baseline GMTs, time, group, age, gender, the interactions between group and age, group and gender and group and time, while study subjects were treated as random effect. Even though the distribution of age and gender between the two groups were not significantly different, they were adjusted in the model. In the model, age was categorized: 20s, 30s, 40s, 50s and over 60. The interactions which were not statistically significant were excluded from the model. The adjusted means of log (GMT) were obtained from the model. The adjusted geometric means were calculated by taking anti-log of the mean of log (GMT). The adjusted P values were calculated by the Hochberg's method to keep from inflation of type I error.
Ethics statement
The study protocol was approved by the institutional review board of Seoul Metropolitan Government Seoul National University Boramae Medical Center (number 20080720/06-2008-47/74). We explained study protocol and obtained the written consent from all the subjects. Exclusions to enrollment included the persons who were immunocompromised, febrile, and those who had allergy to vaccine constituents, they had received tetanus immunization within 5 yr and rejection to enrollment. The medical and non-medical employees in our hospital were excluded. This trial was registered (clinical trial registration number NCT01338688).
RESULTS
A total 252 subjects first participated in this study and were immunized. We could not obtain follow up samples in fifteen subjects in their twenties group at 4 weeks after vaccination. These 15 subjects were excluded from the analysis. A totally of 237 subjects was enrolled and analyzed in this study.
Characteristics of the subjects
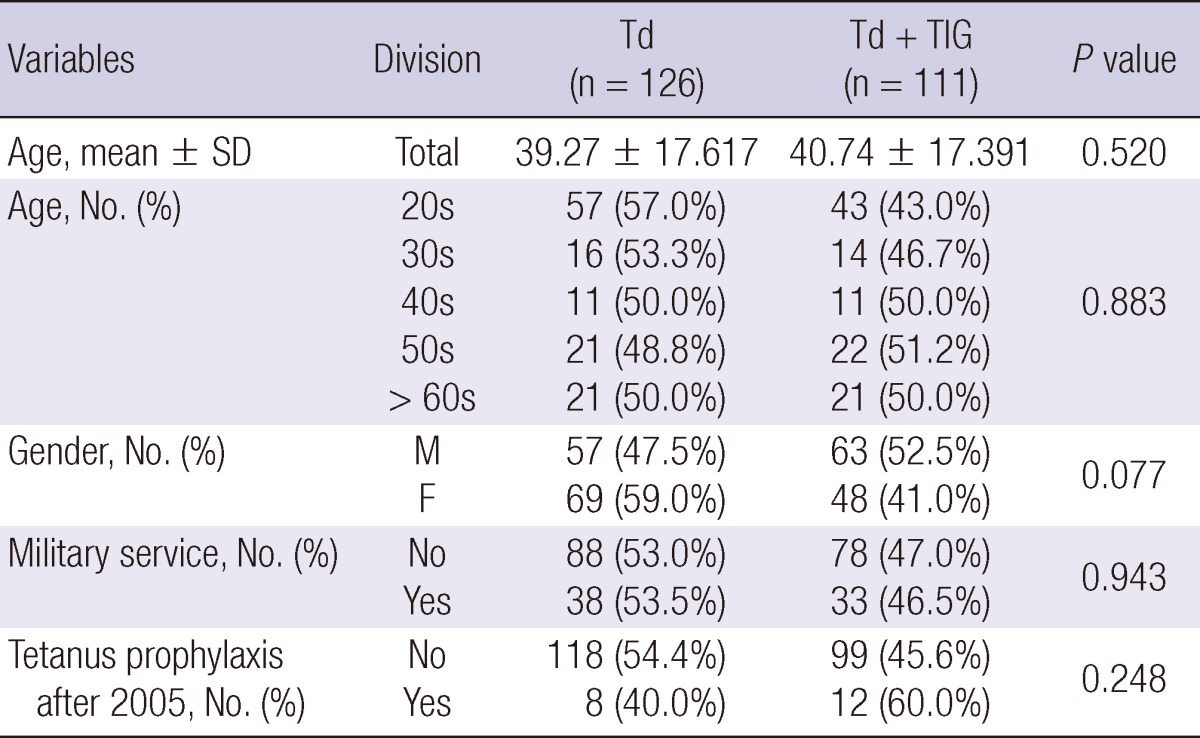
The numbers of subjects who were followed uphad blood sampling done (group 1 vs group 2) were 126 vs 111 subjects at 4 weeks, 96 (76.2%) vs 89 (80.2%) subjects at 6 months and 67 (53.2%) vs 59 (52.2%) subjects at 12 months (Table 1). There were some subjects who were not participated in our study of one's will at 6 months and 12 months. There were no statistical significant differences between the groups for the mean age, the number of subjects who were enrolled in specific age groups, gender, military service and a tetanus prophylaxis history. However the distribution of gender between the groups had a marginal significant difference (P = 0.077), so the variable of gender needed adjustment in this study. The number of group 1 subjects in their twenties was more than that in group 2, so the distribution of the subjects in their twenties also needed adjustment (Table 2).
Table 1.
Subjects' disposition
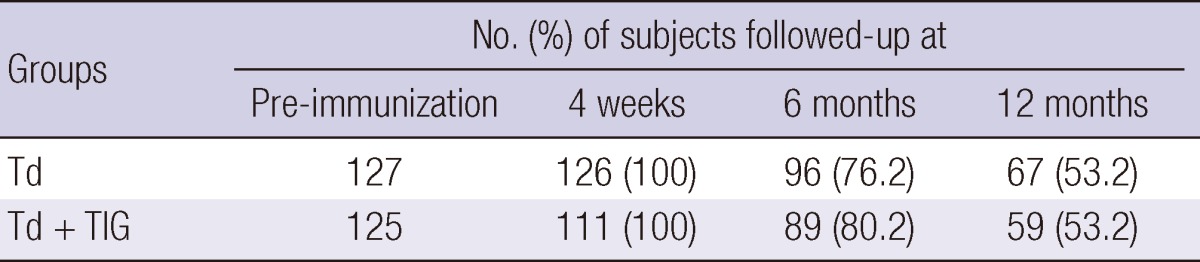
Td, tetanus-diphtheria vaccine group; TIG, tetanus immunoglobulin.
Table 2.
Baseline characteristics of the subjects
Comparison of GMTs between the groups
When the interaction between time and groups, gender and groups, and age and groups were included in the fixed factors analysis using the mixed model after adjustment of the baseline GMTs, time, age and gender, the interaction effects of time and age between the groups did not show statistically significant differences, but the interaction effect between gender and the groups was significantly different (P = 0.021). The GMTs between the groups for the males had a statistically significant difference, which was higher in group 1 than that in group 2, but the females did not show a significant difference (Table 3).
Table 3.
Comparison of the GMTs tetanus antibody level between the groups by gender
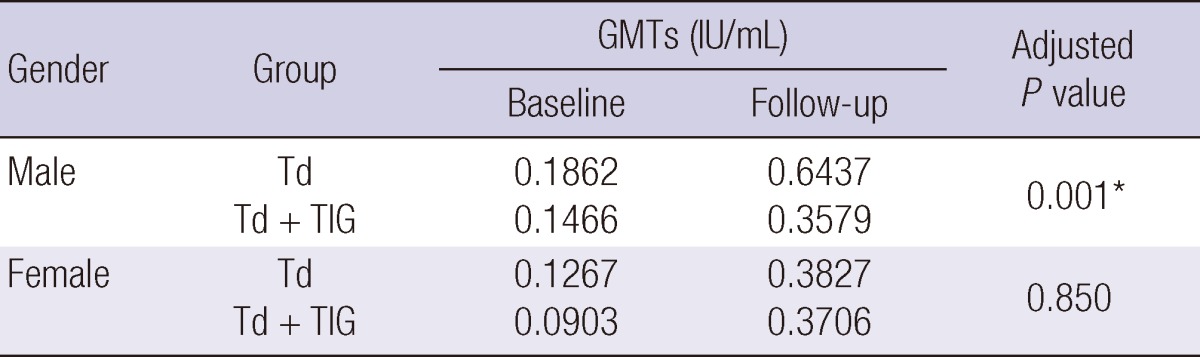
*P < 0.05 at adjusted GMTs. GMTs, geometric mean titers.
Results according to times and ages between the groups
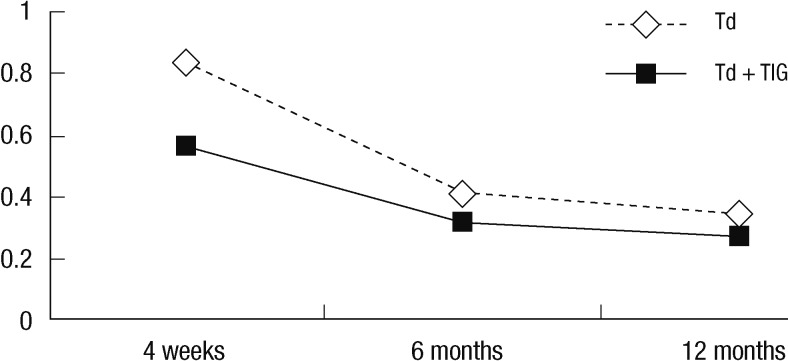
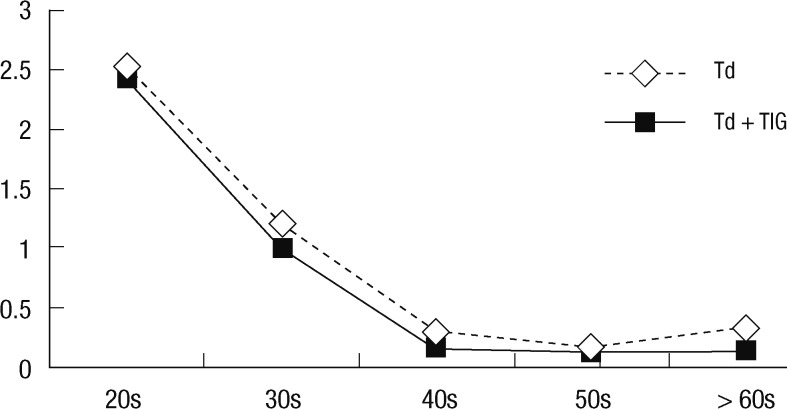
The baseline GMTs of the two groups were 0.1497 IU/mL and 0.1189 IU/mL, respectively (P = 0.122). When the baseline GMTs, gender and age were adjusted, the GMTs according to time between the two groups had statistical significant differences at 4 weeks (P = 0.005), but there were no significant differences at 6 and 12 months (P = 0.140 and 0.140, respectively) (Table 4, Fig. 1). When the baseline GMTs of tetanus antibody, gender and time were adjusted, the GMTs according to age between the two groups did not show statistically significant differences for the subject in their 20s, 30s, 40s, and 50s, but there were significant differences for the subjects over 60 yr (P = 0.006) (Table 5, Fig. 2).
Table 4.
Changes of the GMTs between the groups according to time after adjustment of gender and age
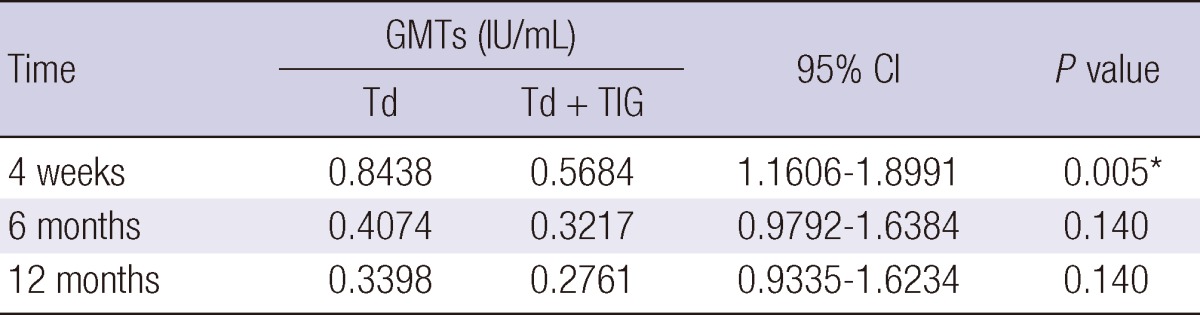
*P value < 0.05. GMTs, geometric mean titers; CI, confidence interval.
Fig. 1.
Comparison of the GMTs between the groups according to time after adjustment of gender and age. GMTs, geometric mean titers.
Table 5.
Changes of the GMTs of tetanus antibody level between the groups according to age after adjustment of gender and time
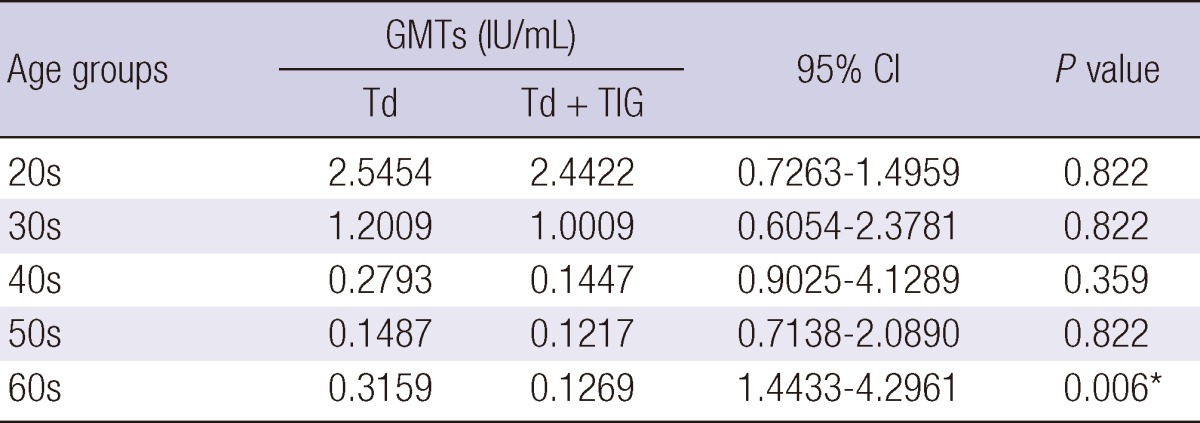
*P value < 0.05. GMTs, geometric mean titers; CI, confidence interval.
Fig. 2.
Changes of the GMTs between the groups according to age after adjustment of gender and time. GMTs, geometric mean titers.
Effects of military service and tetanus prophylaxis after 2005
When the baseline GMTs, age, gender, group, time and the interaction between gender and groups were adjusted in the mixed model by the fixed effects, the GMTs according to military service and tetanus prophylaxis after 2005 were not significantly different between the groups (P = 0.076, P = 0.878, respectively).
DISCUSSION
In Korea, Td vaccine has been available after 2004 (6). Before that year, tetanus prophylaxis should be done by only TIG at the ED or at a general hospital. Nevertheless, there have been approximately 10 tetanus patients have been reported each year, even after complete vaccination during childhood and tetanus prophylaxis with TIG at ED after injury. Though Td has recently been available for immunization and prophylaxis, Td and Td vaccination in adults are not covered by the national health insurance in Korea. Td and Td vaccination are expensive, so most adults' vaccination have been done with Td only at the ED after injury and the adults who had not received previous tetanus vaccination with Td after childhood generally were not vaccinated according to the adult tetanus vaccination schedule. Male adults entering the military service after 1975 must be vaccinated with tetanus toxoid. Tetanus vaccinations at the time of military service and at the ED after injury have been almost the only chance to elevate the tetanus antibody titer in adults. Therefore tetanus prophylaxis at the ED after injury would be very important immunization opportunity for elevating an individual tetanus antibody titer. Most emergency physicians in Korea have been directed to perform tetanus prophylaxis with Td and TIG for injured adult patients because of their low tetanus antibody titer and the low rate of previous tetanus active immunization. In our study, simultaneous injection of Td and TIG did not diminish on tetanus immunity.
The tetanus antibody level after simultaneous administration of Td and TIG was lower than that after a Td single injection in a previous study (7), which provoke some controversies. First, in group 2 (Td + TIG) the basal GMTs were lower than that of group 1 (Td), and statistical significant differences were not shown in the basal GMTs between the groups, but adjustment of the basal GMTs might have been needed. Second, the enrolled subjects were young with a mean age of 26 yr, so a limitation of the adult age distribution existed. Third, follow-up of this study was done for only 4 months and additional follow-up was not done. Significant differences of the GMTs between the groups existed at 4 weeks, but these were not seen at 4 months after immunization. In our study, the GMTs at 4 weeks were significantly different between the groups, but there were no significant differences at 6 and 12 months follow-up. Also, time and age were not meaningful factors for the change of the tetanus antibody level after tetanus prophylaxis in our study by using the mixed model after adjustment of other factors.
There were significant differences of the GMTs in the male subjects between the groups after adjustment of the baselines GMTs and age, but these differences did not exist in the female subjects. However, there was not an exact explanation about these differences between male and female subjects. There were also significant differences of the GMTs in the patients over 60 yr between the groups after adjustment, but not for the patients below 60 yr. In Korea, complete child vaccination had started in 1956 and vaccination at the beginning of military service had started in 1975; therefore, now most the subjects who were over 60 yr might not have been immunized at childhood and during military service when they were young adults (8). Further study and investigation are needed to determine and explain the significantly high GMTs in the males and the people over sixty in our country.
There have been some studies about the simultaneous administration of hepatitis immunoglobulin and vaccine (9, 10). Those studies showed that the hepatitis antibody titers were not significantly different when comparing between the injection of vaccine alone group and the simultaneously injecting vaccine plus immunoglobulin group. The antibody titers in the recipients of vaccine alone were slightly but significantly higher than those of the subjects who received both hepatitis immunoglobulin and vaccine during the several months. In the late months, however, these differences were no longer statistically significant. These hepatitis researches were very similar to our results that tetanus immunoglobulin did not interfere with the development of an active antibody response to the vaccine during a relatively long time. When live attenuated vaccine is injected to humans according to the vaccination schedule, the simultaneous injection of immunoglobulins is usually not recommended because the simultaneous administration of immunoglobulin with vaccines could reduce the immunogenicity for protective antibody production. Yet for inactivated vaccines, the simultaneous administration of immunoglobulins and vaccines is considered feasible (11). The tetanus vaccine is an inactivated vaccine, so co-administration with immunoglobulin is possible.
According to the general guideline of tetanus vaccination to inoculators who had not been immunized as adults, a three shot booster schedule is recommended at 0, 1 and 6 months or at 0, 1 and 12 months. Because no statistical significant difference existed between a single injection of Td and the simultaneous injection of Td plus TIG in this study, if the first vaccination was done by co-administration of vaccine and immunoglobulin at the ED for the first time during adulthood, then the next vaccination may be followed according to the recommended schedule.
In summary, the level of tetanus antibody after tetanus vaccination is not influenced by TIG as observed at 6 and 12 months, and in adults below 50 yr, but are significantly different between the two groups at 4 weeks and for the patients over 60 yr.
ACKNOWLEDGMENTS
We thank Medical Research Collaborating Center in Seoul National University for the statistical analysis.
References
- 1.Center for Disease Control. Diphtheria, tetanus and pertussis: recommendations for vaccine use and other preventive measures recommendations of the immunization practices advisory committee (ACIP) MMWR Recomm Rep. 1991;40:1–28. [PubMed] [Google Scholar]
- 2.Talan DA, Abrahamian FM, Moran GJ, Mower WR, Alagappan K, Tiffany BR, Pollack CV, Steele MT, Dunbar LM, Bajani MD, et al. Tetanus immunity and physician compliance with tetanus prophylaxis practices among emergency department patients presenting with wounds. Ann Emerg Med. 2004;43:305–314. doi: 10.1016/j.annemergmed.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 3.Alagappan K, Pulido G, Caldwell J, Abrahamian FM. Physician compliance with tetanus guidelines for admitted versus discharged patients. South Med J. 2006;99:234–238. doi: 10.1097/01.smj.0000202705.51101.e3. [DOI] [PubMed] [Google Scholar]
- 4.Abbate R, Di Giuseppe G, Marinelli P, Angelillo IF Collaborative Working Group. Appropriate tetanus prophylaxis practices in patients attending emergency departments in Italy. Vaccine. 2008;26:3634–3639. doi: 10.1016/j.vaccine.2008.04.072. [DOI] [PubMed] [Google Scholar]
- 5.Giangrasso J, Smith RK. Misuse of tetanus immunoprophylaxis in wound care. Ann Emerg Med. 1985;14:573–579. doi: 10.1016/s0196-0644(85)80783-6. [DOI] [PubMed] [Google Scholar]
- 6.Lee SY, Kwak GY, Nam CH, Kim JH, Hur JK, Lee KY, Park JS, Kim HM, Kang JH. Immunogenicity and safety of diphtheria-tetanus vaccine in pre-adolescent and adolescent South Koreans. Vaccine. 2009;27:3209–3212. doi: 10.1016/j.vaccine.2009.03.037. [DOI] [PubMed] [Google Scholar]
- 7.Dal-Ré R, Gil A, González A, Lasheras L. Does tetanus immune globulin interfere with the immune response to simultaneous administration of tetanus-diphtheria vaccine? J Clin Pharmacol. 1995;35:420–425. doi: 10.1002/j.1552-4604.1995.tb04083.x. [DOI] [PubMed] [Google Scholar]
- 8.Shin DH, Yu HS, Park JH, Shin JH, Kim SJ. Recently occurring adult tetanus in Korea: emphasis on immunization and awareness of tetanus. J Korean Med Sci. 2003;18:11–16. doi: 10.3346/jkms.2003.18.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lelie PN, Reesink HW, Grijm R, de Jong-van Manen ST, Reerink-Brongers EE. Simultaneous passive and active immunization against hepatitis B: noninterference of hepatitis B immune globulin with the anti-HBs response to reduced doses of heat-inactivated hepatitis B vaccine. Hepatology. 1986;6:971–975. doi: 10.1002/hep.1840060527. [DOI] [PubMed] [Google Scholar]
- 10.Wagner G, Lavanchy D, Darioli R, Pecoud A, Brulein V, Safary A, Frei PC. Simultaneous active and passive immunization against hepatitis A studied in a population of travellers. Vaccine. 1993;11:1027–1032. doi: 10.1016/0264-410x(93)90128-k. [DOI] [PubMed] [Google Scholar]
- 11.National Health and Medical Research Council. Immunoglobulins. Canberra Australian Government Publishing Service; 1991. [Google Scholar]