Abstract
Study Design: A randomized, double-blind, active controlled trial.
Objective: To evaluate the effectiveness of cervical interlaminar epidural injections of local anesthetic with or without steroids in the management of chronic neck pain and upper extremity pain in patients with disc herniation and radiculitis.
Summary of Background Data: Epidural injections in managing chronic neck and upper extremity pain are commonly employed interventions. However, their long-term effectiveness, indications, and medical necessity, of their use and their role in various pathologies responsible for persistent neck and upper extremity pain continue to be debated, even though, neck and upper extremity pain secondary to disc herniation and radiculitis, is described as the common indication. There is also paucity of high quality literature.
Methods: One-hundred twenty patients were randomly assigned to one of 2 groups: Group I patients received cervical interlaminar epidural injections of local anesthetic (lidocaine 0.5%, 5 mL); Group II patients received 0.5% lidocaine, 4 mL, mixed with 1 mL of nonparticulate betamethasone.
Primary outcome measure was ≥ 50 improvement in pain and function. Outcome assessments included Numeric Rating Scale (NRS), Oswestry Disability Index (ODI), opioid intake, employment, and changes in weight.
Results: Significant pain relief and functional status improvement (≥ 50%) was demonstrated in 72% of patients who received local anesthetic only and 68% who received local anesthetic and steroids. In the successful group of participants, significant improvement was illustrated in 77% in local anesthetic group and 82% in local anesthetic with steroid group.
Conclusions: Cervical interlaminar epidural injections with or without steroids may provide significant improvement in pain and function for patients with cervical disc herniation and radiculitis.
Keywords: Chronic neck pain, cervical disc herniation, upper extremity pain, cervical epidural injections, epidural steroids, local anesthetics
Introduction
Neck pain is one of the 4 most commonly reported musculoskeletal disorders 1. Chronic neck pain is common in the adult population, presenting in 60% of patients for 5 years or longer after the initial episode 2-4. The study of the prevalence of neck pain and the impact on general health showed 14% of patients reporting Grade II to IV neck pain, defined as high pain intensity with disability 4. Thus, chronic, function-limiting neck pain is not only common, but is also associated with a significant economic, social, and health impact 1,2,4. Among the multiple structures responsible for neck and upper extremity pain and headaches, cervical intervertebral discs, cervical facet joints, ligaments, fascia, muscles, and nerve root dura have been described to be commonly responsible 5. Consequently, cervical disc herniation with radiculitis is considered one of the most common conditions of neck and upper extremity pain 6,7. Even though the natural history of cervical disc herniation and cervical radicular pain is not described in detail in the literature, based on the most frequently used epidemiologic data from the Mayo Clinic, an annual incidence of cervical radiculopathy was determined to be 83 per 100,000 of those between 13 and 91 years old 7.
The economic burden of managing neck pain is second only to low back pain, with both having extensive treatment modalities and exponential growth 2,4,5,8-26. Epidural injections for managing chronic neck and upper extremity pain are one of the commonly performed interventions in the United States 5,13-19. However, the evidence for cervical interlaminar epidural injections has been a subject of debate and has been reported to be moderate. Benyamin et al 5, in a systematic review of cervical interlaminar epidural injections, determined that the evidence was moderate for managing chronic neck and upper extremity pain. Even then, the role of cervical epidural injections continues to be debated, mostly based on the evidence for lumbar epidural injections, due to multiple factors, including the design of the study (fluoroscopic versus non-fluoroscopic, placebo control versus active control, study size, outcome parameters, duration of follow-up, and bias exerted in reviews secondary to inappropriate methodology leading to inappropriate conclusions) 5,16,17,27-32. In the systematic review by Benyamin et al 5, the evidence was derived from 3 randomized trials meeting the inclusion criteria 33-35, which were all performed without fluoroscopic visualization. However, Manchikanti et al 36, in a preliminary report of a randomized, double-blind, active controlled trial studying the effectiveness of fluoroscopic cervical interlaminar epidural injections for managing chronic cervical disc herniation and radiculitis, reported significant pain relief (≥ 50%) in 77% of the patients in both groups, along with functional status improvement in 74% of the patients receiving local anesthetic and 71% of the patients receiving local anesthetics with steroids at 12 months. Utilizing strong outcome parameters, this preliminary report showed positive results.
These results are similar to the management of lumbar and thoracic disc herniations 37-39 and superior to epidural injections for axial or discogenic pain, spinal stenosis, and post surgery syndrome in the cervical or lumbar spine 40-47.
The underlying mechanism of action of epidurally administered local anesthetics and steroids is not clear, however, it has been hypothesized that the effects of neural blockade are dependent on various mechanisms for both local anesthetics and steroids, including anti-inflammatory properties. Findings in clinical and experimental studies indicate that local anesthetic injections may provide relief similar to corticosteroids 37-56.
Consequently, the current study was undertaken to evaluate the role of cervical interlaminar epidural injections in patients with chronic, function-limiting, neck and upper extremity pain secondary to disc herniation utilizing local anesthetic with or without steroids in a randomized, double-blind, active controlled design with 120 patients. This study involves assessment of patients with cervical disc herniation and radiculitis, whereas, protocol includes multiple other studies including thoracic pathologies, cervical disc related pain, cervical spinal stenosis, and cervical post surgery syndrome. The preliminary report of this study was previously published 36.
Materials & Methods
This randomized, double-blind, active controlled trial was conducted based on Consolidated Standards of Reporting Trials (CONSORT) guidelines 57. The study was performed in an interventional pain management referral center in the United States, after approval by the Institutional Review Board (IRB) and registration with the U.S. Clinical Trial Registry with an assigned number (NCT01071369). This study was conducted with internal resources of the practice without any external funding, either from industry or elsewhere.
Participants
All study patients were derived from new patients of the interventional pain management practice. They were provided with the IRB-approved protocol and informed consent, which described in detail all aspects of the study and withdrawal process.
Interventions
Study patients were assigned into one of 2 groups; Group I patients received cervical interlaminar epidural injections of local anesthetic (lidocaine 0.5% 5 mL), whereas Group II patients received cervical interlaminar epidural injections with 0.5% lidocaine, 4 mL, mixed with 1 mL or 6 mg of non-particulate betamethasone for a total of 5 mL of injectate.
Pre-Enrollment Evaluation
Prior to starting the cervical interlaminar epidural injections and after patients were selected to participate, data, including demographics, medical and surgical history with co-existing disease(s), radiological investigations (magnetic resonance imaging/or computed tomography), nerve conduction studies, findings of physical examination, numeric pain rating scores, functional status assessment using the Neck Disability Index, work status, and opioid intake information were obtained.
Inclusion Criteria
Inclusion criteria were limited to patients with cervical disc herniation or radiculitis. The age limits were 18 years or older. Patients invited to participate were those who also presented with a history of chronic, function-limiting neck and upper extremity pain of at least 6 months duration, were competent to understand the study protocol, provide voluntary written informed consent, and participate in outcome measures. Other criteria included a failure to respond to conservative treatment modalities, including, but not limited to, physical therapy, a structured exercise program, and drug therapy.
Exclusion criteria included previous cervical spine surgery; radiculitis secondary to spinal stenosis; discogenic pain without disc herniation; uncontrollable or unstable opioid use; uncontrolled psychiatric disorders; uncontrolled medical illness, either acute or chronic; any condition that could interfere with the interpretation of the outcome assessment; pregnancy and lactation; or a history of adverse reactions to local anesthetics or steroids.
Description of Interventions
Cervical interlaminar epidural procedures were performed by one physician (LM) in an Ambulatory Surgery Center (ASC), in a sterile operating room, under fluoroscopy. Patients were in the prone position with appropriate monitoring and intravenous access, and sedation with midazolam and fentanyl when indicated. After sterile preparation, the epidural space was entered with the loss of resistance technique under fluoroscopic visualization between C7 and T1 to C5 and C6 with confirmation by injection of non-ionic contrast medium. Subsequent to the confirmation of entry into the epidural space, 5 mL of lidocaine hydrochloride 0.5% preservative free, or 4 mL of lidocaine preservative free mixed with 6 mg of non-particulate betamethasone was injected.
Repeat cervical epidural injections were provided based on the response to prior cervical epidural injections. The response was assessed by improvement in physical and functional status and repeat procedures were only provided when increased levels of pain were reported with deterioration of functional status and pain relief to below 50%.
Co-interventions
No specific physical therapy, occupational therapy, or other interventions were offered other than the study intervention to all patients in both groups. However, patients continued their drug therapy with either opioids or non-opioid analgesics, therapeutic exercise program, and normal activities, including work.
Objectives
The study was designed to evaluate the effectiveness of cervical interlaminar epidural injections with or without steroids under fluoroscopy in managing chronic neck and upper extremity pain secondary to disc herniation or radiculitis.
Outcomes
The primary outcome measure was combined improvement in pain scores and functional status improvement.
The numeric rating scale (NRS), Neck Disability Index (NDI), work status, and opioid intake in terms of morphine equivalence, were assessed at baseline, 3, 6, and 12 months post-treatment.
Significant improvement was defined as at least 50% pain relief associated with at least 50% improvement in functional status measured by NRS and NDI. The NRS and NDI have been shown to be valid and reliable in patients with mechanical neck pain 58,59. Significant improvement is a robust measure compared to previous evaluations.
Based on the dosage frequency and schedule of the drug, opioid intake was converted to morphine equivalent and changes in intake were assessed 60.
Employable patients were determined based on their unemployment or employment on a part-time basis or full-time employment. However, patients who chose not to work, were retired, or were homemakers without the necessity or desire to work outside the home, but not due to pain, were not considered in the employment pool.
Sample Size
The sample size was calculated based on significant pain relief. Considering a 0.05 two-sided significance level, a power of 80%, and an allocation ratio of 1:1, 55 patients in each group were estimated 61. Allowing for a 10% attrition/ non-compliance rate, 60 patients in each group were required.
Randomization
Sixty patients were randomly assigned into each group.
Sequence Generation
Computer-generated random allocations sequence by simple randomization was utilized.
Allocation Concealment
One of the 3 coordinators of the study randomized the patients into 2 groups and prepared the drugs appropriately.
Blinding (Masking)
Appropriate blinding (masking) was achieved by blinding the group assignment to all involved, including the physician and the patients. Both solutions were clear with the inability to identify the group assignment. Further, all the study patients were mixed with other patients receiving routine treatments, and the physician performing the procedure was not informed of the nature of the patients participating in the study. At one-year follow-up, a statistician not involved in patient care (VP) collected the data on all the patients with information not being revealed to anyone else. Thus, overall the nature of blinding and masking were not interrupted.
Statistical Methods
The chi-squared statistic, Fisher's exact test, t-test, and paired t-test were used for statistical analysis.
Chi-squared statistic was used to test the differences in proportions. Fisher's exact test was used wherever the expected value was less than 5; a paired t-test was used to compare the pre- and post-treatment results of average pain scores and NDI measurements at baseline versus 3, 6, and 12 months. For comparison of mean scores between groups, t-test was performed.
The average per procedure and yearly relief were assessed by simple calculations.
Intent-to-Treat-Analysis
An intent-to-treat analysis, along with sensitivity analysis, were performed utilizing either the last follow-up data or initial data for the patients withdrawn, with the sensitivity analysis utilizing best case, worse case, and last follow-up data.
Results
Patient Flow
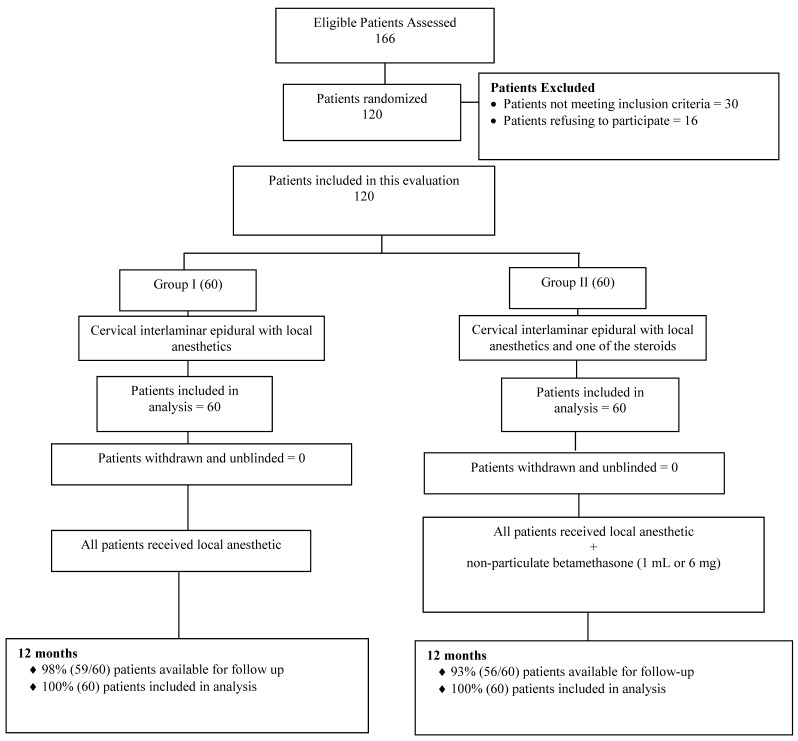
Figure 1 illustrates the patient flow. The recruitment period lasted from August 2007 through June 2010.
Fig 1.
Schematic presentation of patients flow at one-year follow-up of 120 patients.
Demographic Data
Baseline demographic and clinical characteristics of each group are illustrated in Table 1. Group I patients' mean weight was significantly more than the Group II patients' mean weight.
Table 1.
Baseline demographic characteristics.
| Group 1 (60) |
Group II (60) |
P value | ||
|---|---|---|---|---|
| Sex | Male | 47% (28) | 42% (25) | 0.581 |
| Female | 53% (32) | 58% (35) | ||
| Age | Mean ± SD | 46.2 ± 10.3 | 45.6 ± 10.4 | 0.738 |
| Weight | Mean ± SD | 208.9 ± 53.3 | 168.1 ± 35.2 | 0.000 |
| Height | Mean ± SD | 67.3 ± 4.4 | 66.3 ± 4.0 | 0.199 |
| Duration of Pain (months) | Mean ± SD | 118.3 ± 98.6 | 91.9 ± 94.5 | 0.137 |
| Onset of the Pain | Gradual | 53% (32) | 52% (31) | 0.855 |
| Injury | 47% (28) | 48% (29) | ||
| Neck Pain Distribution | Neck pain only | 15% (9) | 17% (10) | 0.975 |
| Neck pain worse than upper extremity | 57% (34) | 55% (33) | ||
| Upper extremity worse than neck pain | 8% (5) | 7% (4) | ||
| Both equal | 20% (12) | 22% (13) | ||
| Disc Herniation Levels (at multiple levels) |
C3/4 | 13% (8) | 13% (8) | NA |
| C4/5 | 30% (18) | 20% (12) | ||
| C5/6 | 50% (30) | 60% (36) | ||
| C6/7 | 40% (24) | 47% (28) | ||
| C7/T1 | 10% (6) | 12% (7) | ||
| Numeric Rating Score | Mean ± SD | 7.9 ± 1.0 | 7.9 ± 0.9 | 1.000 |
| Neck Disability Index | Mean ± SD | 29.6 ± 5.3 | 29.2 ± 6.1 | 0.678 |
Pain Relief
Table 2 illustrates the NRS scores. Pain scores significantly decreased from baseline at 3, 6, and 12 months in all groups, with no significant differences between the groups at follow-up periods.
Table 2.
Characteristics of pain relief of the numeric rating scale and proportion of patients with significant relief.
| Numeric Rating Scale | Group I (60) | Group II (60) | P value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Baseline | 7.9 ± 1.0 | 7.9 ± 0.9 | 1.000 |
| 3 months | 3.7* ± 1.4 (85%) |
3.8* ± 1.4 (75%) |
0.468 |
| 6 months | 3.5* ± 1.4 (83%) |
3.9* ± 1.5 (73%) |
0.109 |
| 12 months | 3.7* ± 1.5 (72%) |
3.9* ± 1.5 (72%) |
0.537 |
Percentages in parentheses indicate proportion of participants with significant relief (≥ 50% reduction in Numeric Rating Scale from baseline)
* indicates significant difference with baseline values (P < 0.01)
Functional Assessment
Functional assessment results assessed by the NDI are illustrated in Table 3.
Table 3.
Illustration of functional assessment scores by the Neck Disability Index and proportion of patients with significant improvement (≥ 50%).
| Neck Disability Index | Group I (60) |
Group II (60) |
P value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Baseline | 29.6 ± 5.3 | 29.2 ± 6.1 | 0.678 |
| 3 months | 14.7* ± 5.5 (85%) |
15.6* ± 6.3 (70%) |
0.394 |
| 6 months | 13.8* ± 5.4 (83%) |
15.3* ± 6.9 (73%) |
0..183 |
| 12 months | 13.8* ± 5.7 (75%) |
15.1* ± 7.0 (68%) |
0.267 |
Percentages in parentheses indicate the proportion of patients with significant relief (≥ 50% reduction in Neck Disability Index from baseline)
* indicates significant difference with baseline values (P < 0.01)
Pain Relief and Functional Assessment
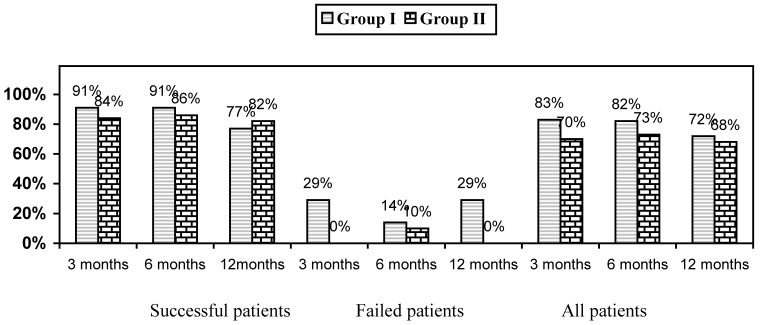
Figure 2 illustrates the proportion of patients with a significant reduction in the NRS and NDI with greater than 50% reduction from baseline. Successful patients showed better results compared to all patients with results illustrating at 12 months an improvement of 72% in Group I and 68% in Group II for all patients compared to 77% and 82% in the successful groups.
Fig 2.
Proportion of patients with significant reduction in Numeric Rating Scale and Neck Disability Index (≥ 50% reduction from baseline).
Therapeutic Procedural Characteristics
Therapeutic procedural characteristics are illustrated in Table 4. Epidural entry was performed between C7 and T1 in 28% of patients, between C6 and C7 in 60% of patients, and between C5 and C6 in 12% of patients.
Table 4.
Therapeutic procedural characteristics with procedural frequency, average relief per procedure, and average total relief in weeks over a period of one year.
| Successful Patients | Failed Patients | Combined | ||||
|---|---|---|---|---|---|---|
| Group I (53) |
Group II (53) |
Group I (7) |
Group II (7) |
Group I (60) |
Group II (60) |
|
| 1st procedure relief | 7.8 ± 8.2 | 5.7 ± 6.8 | 0.4 ± 0.8 | 0.3 ± 0.4 | 6.9 ± 8.0 | 4.8 ± 6.5 |
| 2nd procedure relief | 11.9 ± 7.1 (51) |
10.1 ± 8.8 (48) |
1.2 ± 1.3 (5) |
0.8 ± 0.8 (6) |
10.9 ± 7.4 (56) |
9.1 ± 8.8 (54) |
| 3rd procedure relief | 14.8 ± 9.1 (43) |
12.5 ± 4.4 (40) |
5.8 ± 6.3 (4) |
7.0 ± 8.5 (2) |
14.0 ± 9.2 (47) |
12.2 ± 4.6 (42) |
| 4th procedure relief | 12.3 ± 2.4 (35) |
12.6 ± 2.3 (31) |
9.5 ± 4.9 (2) |
10.0 (1) |
12.1 ± 2.5 (37) |
12.5 ± 2.3 (32) |
| 5th procedure relief | 12.6 ± 0.9 (14) |
12.3 ± 2.2 (14) |
12.0 (1) |
11.0 (1) |
12.6 ± 0.9 (15) |
12.2 ± 2.1 (15) |
| Average Number of Procedures for One Year | 3.7 ± 1.1 | 3.7 ± 1.2 | 2.7 ± 1.5 | 2.0 ± 1.2 | 3.6 ± 1.2 | 3.4 ± 1.3 |
| Average Relief per Procedure for Initial Two Procedures in Weeks | 9.8# ± 7.9 (104) |
7.8 ± 8.1 (98) |
0.8 ± 1.1 (12) |
0.5 ± 0.6 (16) |
8.8 ± 8.0 (116) |
6.8 ± 7.9 (114) |
| Average Relief per Procedure After Initial Two Procedures | 13.5 ± 6.5 (92) |
12.5 ± 3.4 (85) |
7.7 ± 5.5 (7) |
8.8 ± 5.3 (4) |
13.1 ± 6.6 (99) |
12.3 ± 3.5 (89) |
| Average Relief per Procedure | 11.5# ± 7.5 (196) |
10.0 ± 6.7 (183) |
3.3 ± 4.8 (19) |
2.1 ± 4.0 (20) |
10.8 ± 7.6 (215) |
9.2 ± 6.9 (203) |
| Average Total Relief For One Year (Weeks) | 41.4 ± 12.7 | 36.3 ± 14.6 | 9.0 ± 13.4 | 4.2 ± 10.9 | 37.6# ± 16.4 | 31.0 ± 18.5 |
# indicates significant difference with Group II (P < 0.05)
Average relief per year showed significant differences: 37.6 ± 16.4 weeks in Group I and 31.0 ± 18.5 weeks in Group II. The total number of injections per year was 3.6 ± 1.2 in Group I and 3.4 ± 1.3 in Group II. However, when patients were separated into successful and failed groups, the total number of injections per year was 3.7 ± 1.1 in Group I and 3.7 ± 1.2 in Group II in the successful groups, and 2.7 ± 1.5 for Group I and 2.0 ± 1.2 for Group II in the failed groups. Total relief of 41.4 ± 12.7 weeks was obtained in the successful group in Group I; in Group II it was 36.3 ± 14.6. In contrast, the relief was 9.0 ± 13.4 in Group I and 4.2 ± 10.9 weeks in Group II for the failed groups.
The initial therapy was considered to be successful if a patient obtained consistent relief with 2 initial injections lasting at least 3 weeks. All others were considered failures.
Employment Characteristics
Table 5 demonstrates employment characteristics in both groups.
Table 5.
Employment characteristics.
| Employment Status | Group I | Group II | ||
|---|---|---|---|---|
| Baseline | 12 Months | Baseline | 12 Months | |
| Employed part-time | 2 | 2 | 2 | 3 |
| Employed full-time | 9 | 9 | 13 | 14 |
| Unemployed (due to pain) | 0 | 2 | 1 | |
| Not Working | 2 | 2 | 5 | 4 |
| Eligible for Employment at Baseline | 13 | 13 | 22 | 22 |
| Total Employed | 11 | 11 | 15 | 17 |
| Housewife | 3 | 3 | 1 | 1 |
| Disabled | 37 | 37 | 33 | 33 |
| Retired | 7 | 7 | 4 | 4 |
| Total Number of Patients | 60 | 60 | 60 | 60 |
Opioid Intake
Table 6 illustrates opioid intake.
Table 6.
Opioid intake (morphine equivalence mg).
| Opioid Intake (Morphine Equivalence mg) |
Group I (60) | Group II (60) | P value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Baseline | 57.0 ± 46.1 | 53.8 ± 36.1 | 0.671 |
| 3 Months | 34.4* ± 21.7 | 35.2* ± 16.3 | 0.824 |
| 6 Months | 33.0* ± 22.3 | 35.5* ± 16.3 | 0.488 |
| 12 Months | 34.7* ± 23.5 | 35.5* ± 16.3 | 0.825 |
* indicates significant difference with baseline values (P < 0.05)
Changes in Weight
There were no differences in change (gain or loss) in body weight from baseline in both groups (Table 7).
Table 7.
Characteristics of changes in weight.
| Weight (lbs) | Group I (60) | Group II (60) | P value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Weight at Beginning | 208.9 ± 53.3 | 168.1 ± 35.2 | 0.000 |
| Weight at One Year | 205.4 ± 53.6 | 166.9 ± 32.7 | 0.000 |
| Change | -3.5 ± 9.9 | -1.1 ± 7.4 | 0.139 |
| Lost Weight | 57% (34) | 43% (26) | 0.311 |
| No Change | 20% (13) | 25% (15) | 0.311 |
| Gained Weight | 22% (13) | 32% (19) | 0.311 |
Adverse Events
Of the 418 procedures performed, there was one subarachnoid puncture, 3 intravascular penetrations, and one report of soreness lasting one week. No postoperative headache was reported after subarachnoid puncture.
Discussion
This randomized, active controlled, double-blind evaluation of 120 patients receiving fluoroscopically directed cervical epidural injections of local anesthetic with or without steroids demonstrated significant improvement for both groups, with 72% of the patients in the local anesthetic group and 68% patients in the local anesthetic with steroids group getting significant improvement in their pain. Significant improvement has been defined with robust outcome measures utilizing at least 50% pain relief and at least 50% improvement in functional status as measured by NRS and NDI. The results of this study illustrate that in selected patients, those judged as successful participants, that is, the ones who responded to the first 2 initial procedures, combined pain relief and improvement in functional status was observed in 77% in Group I and 82% in Group II at one-year follow-up. The improvement in the successful participants was superior to the overall improvement in all patients. This study confirms that the treatment of cervical disc herniation with radiculitis with cervical epidural injections of steroids or local anesthetics administered under fluoroscopy has clinically important effects. The overall average procedures per year was 3.6 in Group I and 3.4 in Group II, with an average total relief per year of 38 weeks for Group I patients and 31 weeks for Group II patients. Opioid intake was significantly reduced in both groups.
While the literature is replete with multiple studies and systematic reviews in favor of and against epidural injections in general, the specific literature in the cervical spine is limited with only 2 systematic reviews available 5,8. Benyamin et al 5 concluded that all 3 studies showed positive results for short-term relief, whereas only 2 were positive for long-term relief, which was defined as greater than 6 months. As illustrated in the present evaluation, cervical interlaminar epidural injections of local anesthetics with or without steroids, though they do not provide long-term relief, long-term relief can however be achieved through appropriate patient evaluation and judicious use of injection therapy, as illustrated in the successful group. This study specifically included only patients with disc herniation and radiculitis rather than a heterogenous group of patients with post laminectomy syndrome, spinal stenosis, axial discogenic pain, or radiculitis without disc herniation. In the past multiple studies have been criticized, most importantly for their design and their inability to confirm the location of the injection by not using fluoroscopy. Further, systematic reviews also have been criticized for their methodology by evaluating the studies inappropriately, reaching inaccurate conclusions.
In contrast to the previous studies, this study provides insight into successful or failed groups based on the first 2 procedures. The patients in the successful group, those who had good pain relief with the first and second procedures, constituting over 80% of the enrolled patients, showed average relief from 36.3 to 41.4 weeks out of 52 weeks. Further, the average number of procedures per year was 3.7. However, in the failed group, the average relief per procedure was 0.5 to 0.8 weeks, with overall relief of 4.2 to 9.0 weeks over a period of one year. There were no significant differences noted whether a steroid was utilized or not in the proportion of failed patients as well as the duration of relief. This is in contrast to lumbar disc herniation, which demonstrated a superiority of improvement in the steroid group 37. The results differ from caudal epidural injections in lumbar disc herniation, which showed superior results with steroids 37.
The strengths of this evaluation include its comparative evaluation, as comparative effectiveness research has been considered pivotal to evidence-based medicine 27,28,30,62. Even though this trial is limited to a single center, it is randomized, double-blind, active controlled, and designed to determine whether fluoroscopically directed cervical interlaminar epidural injections with or without steroids with the usual volumes injected in practice are effective in providing pain relief. Further, patient selection was not only practical, but it was also met with great sensitivity and included only patients with chronic, persistent neck and upper extremity pain due to disc herniation and radiculitis. The repeat procedures were provided based on principles of contemporary interventional pain management and guidelines 28, with only deterioration in relief and functional status being the criteria, rather than based on a schedule, or the number of injections, or only one procedure being offered throughout one-year. Consequently, this study meets the criteria for practical clinical trials with an active controlled group instead of a placebo group, and measures effectiveness, which is considered more appropriate than measuring efficacy.
The study may be criticized for its lack of a placebo group and also early published results after one-year instead of waiting for 2 years. In reference to placebo, most studies in the past have utilized inappropriate methodology involving placebo groups 16,17,27-30,63-67. The appropriate placebo design by Ghahreman et al 65 showed no significant effect with sodium chloride solution when injected into an inactive structure. In addition, the concepts including local anesthetic transformed into placebo are not only methodologically and conceptually inaccurate, they also result in misleading conclusions, since inactive substances injected into active structures have been shown to result in various types of effects 64-72. Further, local anesthetics have been shown to provide long-term improvement in patients both in clinical as well as experimental settings 38-50,54-56.
The present study was published with one year results, rather than waiting for 2 years, as there are no fluoroscopically performed studies, except the preliminary report of this study, and there are no large-scale reports performed in a practical setting. The only difference noted in the demographic characteristics was the weight at baseline, which failed to show any significant influence on the results.
Implications of this trial are widespread in an era of evidence-based medicine, comparative effectiveness research, and exploding health care costs. Studies with proper methodology in practical settings are crucial, but rare. Proper application of the interventions will improve patients' pain and function, reduce drug use, and may return them to the workforce. However, inappropriate interventions may incur substantial expenses and may not provide any benefit, but rather may be harmful to the patient because of the depletion of resources, resulting in denying access to patients. By the same token, inappropriately performed evaluations that lead to inaccurate conclusions may reduce health care expenditures, but will also increase patient suffering, increase drug use, and impede access to medical care.
Conclusions
This randomized, double-blind, active controlled trial of 120 patients treated with fluoroscopically guided cervical interlaminar epidural injections of local anesthetic with or without steroids for chronic neck and upper extremity pain secondary to disc herniation and radiculitis illustrated effectiveness in 77% of patients in the local anesthetic group and 82% in the steroid group, with improvement in pain and functional status in the successful groups, requiring an average of 3.5 procedures over a one-year period.
Acknowledgments
The authors wish to thank Vidyasagar Pampati, MSc, for statistical assistance, Sekar Edem for assistance in the search of the literature, Tom Prigge, MA, for manuscript review, and Tonie M. Hatton and Diane E. Neihoff, transcriptionists, for their assistance in preparation of this manuscript.
References
- 1.McLean SM, May S, Klaber-Moffett J. et al. Risk factors for the onset of non-specific neck pain: a systematic review. J Epidemiol Community Health. 2010;64:565–72. doi: 10.1136/jech.2009.090720. [DOI] [PubMed] [Google Scholar]
- 2.Enthoven P, Skargren E, Oberg B. Clinical course in patients seeking primary care for back or neck pain: a prospective 5-year follow-up of outcome and health care consumption with subgroup analysis. Spine (Phila Pa 1976) 2004;29:2458–65. doi: 10.1097/01.brs.0000143025.84471.79. [DOI] [PubMed] [Google Scholar]
- 3.Côté P, Cassidy JD, Carroll LJ. et al. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112:267–73. doi: 10.1016/j.pain.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Côté P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 1998;23:1689–98. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 5.Benyamin RM, Singh V, Parr AT. et al. Systematic review of the effectiveness of cervical epidurals in the management of chronic neck pain. Pain Physician. 2009;12:137–57. [PubMed] [Google Scholar]
- 6.Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353:392–99. doi: 10.1056/NEJMcp043887. [DOI] [PubMed] [Google Scholar]
- 7.Radhakrishnan K, Litchy WJ, O'Fallon WM. et al. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117:325–35. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 8.Peloso PMJ, Gross A, Haines T, et al; Cervical Overview Group. Medicinal and injection therapies for mechanical neck disorders. Cochrane Database Syst Rev. 2007;3:CD000319. doi: 10.1002/14651858.CD000319.pub4. [DOI] [PubMed] [Google Scholar]
- 9.Côté P, van der Velde G, Cassidy JD, et al; Bone, Joint Decade 2000-2010 Task Force on Neck Pain, Its Associated Disorders. The burden and determinants of neck pain in workers. Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33:S60–74. doi: 10.1097/BRS.0b013e3181643ee4. [DOI] [PubMed] [Google Scholar]
- 10.Leroux I, Dionne CE, Bourbonnais R. et al. Prevalence of musculoskeletal pain and associated factors in the Quebec working population. Int Arch Occup Environ Health. 2005;78:379–86. doi: 10.1007/s00420-004-0578-2. [DOI] [PubMed] [Google Scholar]
- 11.Manchikanti L, Singh V, Datta S. et al. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12:E35–70. [PubMed] [Google Scholar]
- 12.Hogg-Johnson S, van der Velde G, Carroll LJ, et al; Bone, Joint Decade 2000-2010 Task Force on Neck Pain, Its Associated Disorders. The burden and determinants of neck pain in the general population: Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33:S39–51. doi: 10.1097/BRS.0b013e31816454c8. [DOI] [PubMed] [Google Scholar]
- 13.Manchikanti L, Pampati V, Boswell MV. et al. Analysis of the growth of epidural injections and costs in the Medicare population: a comparative evaluation of 1997, 2002, and 2006 data. Pain Physician. 2010;13:199–212. [PubMed] [Google Scholar]
- 14.Manchikanti L, Pampati V, Singh V. et al. Explosive growth of facet joint interventions in the Medicare population in the United States: A comparative evaluation of 1997, 2002, and 2006 data. BMC Health Serv Res. 2010;10:84. doi: 10.1186/1472-6963-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abbott ZI, Nair KV, Allen RR. et al. Utilization characteristics of spinal interventions. Spine J. 2012;12:35–43. doi: 10.1016/j.spinee.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Manchikanti L, Datta S, Derby R. et al. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: Part 1. Diagnostic interventions. Pain Physician. 2010;13:E141–74. [PubMed] [Google Scholar]
- 17.Manchikanti L, Datta S, Gupta S. et al. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: Part 2. Therapeutic interventions. Pain Physician. 2010;13:E215–64. [PubMed] [Google Scholar]
- 18.Manchikanti L, Singh V, Boswell MV. Interventional pain management at crossroads: The perfect storm brewing for a new decade of challenges. Pain Physician. 2010;13:E111–40. [PubMed] [Google Scholar]
- 19.Benyamin RM, Datta S, Falco FJE. A perfect storm in interventional pain management: Regulated, but unbalanced. Pain Physician. 2010;13:109–16. [PubMed] [Google Scholar]
- 20.Manchikanti L, Ailinani H, Koyyalagunta D. et al. A systematic review of randomized trials of long-term opioid management for chronic non-cancer pain. Pain Physician. 2011;14:91–121. [PubMed] [Google Scholar]
- 21.Manchikanti L, Vallejo R, Manchikanti KN. et al. Effectiveness of long-term opioid therapy for chronic non-cancer pain. Pain Physician. 2011;14:E133–56. [PubMed] [Google Scholar]
- 22.Wang MC, Chan L, Maiman DJ. et al. Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine (Phila Pa 1976) 2007;32:342–47. doi: 10.1097/01.brs.0000254120.25411.ae. [DOI] [PubMed] [Google Scholar]
- 23.Manchikanti L, Singh V, Caraway DL. et al. Medicare physician payment systems: impact of 2011 schedule on interventional pain management. Pain Physician. 2011;14:E5–33. [PubMed] [Google Scholar]
- 24.Manchikanti L, Parr AT, Singh V. et al. Ambulatory surgery centers and interventional techniques: a look at long-term survival. Pain Physician. 2011;14:E177–215. [PubMed] [Google Scholar]
- 25.Manchikanti L, Fellows B, Ailinani H. et al. Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician. 2010;13:401–35. [PubMed] [Google Scholar]
- 26.Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005;57:753–58. [PubMed] [Google Scholar]
- 27.Manchikanti L, Falco FJE, Boswell MV. et al. Facts, fallacies, and politics of comparative effectiveness research: Part 1. Basic considerations. Pain Physician. 2010;13:E23–54. [PubMed] [Google Scholar]
- 28.Manchikanti L, Falco FJE, Boswell MV. et al. Facts, fallacies, and politics of comparative effectiveness research: Part 2. Implications for interventional pain management. Pain Physician. 2010;13:E55–79. [PubMed] [Google Scholar]
- 29.Manchikanti L, Boswell MV, Singh V. et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12:699–802. [PubMed] [Google Scholar]
- 30.Manchikanti L, Falco FJ, Benyamin RM. et al. The impact of comparative effectiveness research on interventional pain management: evolution from Medicare Modernization Act to Patient Protection and Affordable Care Act and the Patient- Centered Outcomes Research Institute. Pain Physician. 2011;14:E249–82. [PubMed] [Google Scholar]
- 31.Chou R, Atlas SJ, Loeser JD. et al. Guideline warfare over interventional therapies for low back pain: can we raise the level of discourse? J Pain. 2011;12:833–39. doi: 10.1016/j.jpain.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Manchikanti L, Benyamin RM, Falco FJE. et al. Guidelines warfare over interventional techniques: is there a lack of discourse or straw man? Pain Physician. 2012;15:E1–26. [PubMed] [Google Scholar]
- 33.Stav A, Ovadia L, Sternberg A. et al. Cervical epidural steroid injection for cervicobrachialgia. Acta Anaesthesiol Scand. 1993;37:562–66. doi: 10.1111/j.1399-6576.1993.tb03765.x. [DOI] [PubMed] [Google Scholar]
- 34.Castagnera L, Maurette P, Pointillart V. et al. Long term results of cervical epidural steroid injection with and without morphine in chronic cervical radicular pain. Pain. 1994;58:239–43. doi: 10.1016/0304-3959(94)90204-6. [DOI] [PubMed] [Google Scholar]
- 35.Pasqualucci A, Varrassi G, Braschi A. et al. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: single injection versus continuous infusion. Clin J Pain. 2007;23:551–7. doi: 10.1097/AJP.0b013e318074c95c. [DOI] [PubMed] [Google Scholar]
- 36.Manchikanti L, Cash KA, Pampati V. et al. The effectiveness of fluoroscopic cervical interlaminar epidural injections in managing chronic cervical disc herniation and radiculitis: preliminary results of a randomized, double-blind, controlled trial. Pain Physician. 2010;13:223–36. [PubMed] [Google Scholar]
- 37.Manchikanti L, Singh V, Cash KA. et al. A randomized, controlled, double-blind trial of fluoroscopic caudal epidural injections in the treatment of lumbar disc herniation and radiculitis. Spine (Phila Pa 1976) 2011;36:1897–1905. doi: 10.1097/BRS.0b013e31823294f2. [DOI] [PubMed] [Google Scholar]
- 38.Manchikanti L, Singh V, Falco FJE. et al. Evaluation of the effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind, controlled trial. Pain Physician. 2010;13:343–55. [PubMed] [Google Scholar]
- 39.Manchikanti L, Cash KA, McManus CD. et al. A preliminary report of a randomized double-blind, active controlled trial of fluoroscopic thoracic interlaminar epidural injections in managing chronic thoracic pain. Pain Physician. 2010;13:E357–69. [PubMed] [Google Scholar]
- 40.Manchikanti L, Cash KA, McManus CD. et al. One year results of a randomized, double-blind, active controlled trial of fluoroscopic caudal epidural injections with or without steroids in managing chronic discogenic low back pain without disc herniation or radiculitis. Pain Physician. 2011;14:25–36. [PubMed] [Google Scholar]
- 41.Manchikanti L, Singh V, Cash KA. et al. Management of pain of post lumbar surgery syndrome: one-year results of a randomized, double-blind, active controlled trial of fluoroscopic caudal epidural injections. Pain Physician. 2010;13:509–21. [PubMed] [Google Scholar]
- 42.Manchikanti L, Cash RA, McManus CD. et al. Fluoroscopic caudal epidural injections with or without steroids in managing pain of lumbar spinal stenosis: one year results of randomized, double-blind, active-controlled trial. J Spinal Disord Tech. 2012 Jun;25(4):226–34. doi: 10.1097/BSD.0b013e3182160068. [DOI] [PubMed] [Google Scholar]
- 43.Manchikanti L, Cash KA, McManus CD. et al. Preliminary results of a randomized, double-blind, controlled trial of fluoroscopic lumbar interlaminar epidural injections in managing chronic lumbar discogenic pain without disc herniation or radiculitis. Pain Physician. 2010;13:E279–92. [PubMed] [Google Scholar]
- 44.Manchikanti L, Malla Y, Cash KA. et al. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical post-surgery syndrome: preliminary results of a randomized, double-blind active control trial. Pain Physician. 2012;15:13–26. [PubMed] [Google Scholar]
- 45.Manchikanti L, Malla Y, Cash KA. et al. Fluoroscopic epidural injections in cervical spinal stenosis: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:E59–70. [PubMed] [Google Scholar]
- 46.Manchikanti L, Cash KA, Pampati V. et al. Cervical epidural injections in chronic discogenic neck pain without disc herniation or radiculitis: preliminary results of a randomized, double-blind, controlled trial. Pain Physician. 2010;13:E265–78. [PubMed] [Google Scholar]
- 47.Manchikanti L, Cash KA, McManus CD. et al. Lumbar interlaminar epidural injections in central spinal stenosis: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:51–63. [PubMed] [Google Scholar]
- 48.Manchikanti L, Singh V, Falco FJE. et al. Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci. 2010;7:124–35. doi: 10.7150/ijms.7.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Manchikanti L, Singh V, Falco FJE. et al. Comparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: a randomized, double-blind controlled trial. Pain Physician. 2010;13:437–50. [PubMed] [Google Scholar]
- 50.Manchikanti L, Singh V, Falco FJE. et al. Comparative effectiveness of a one-year follow-up of thoracic medial branch blocks in management of chronic thoracic pain: a randomized, double-blind active controlled trial. Pain Physician. 2010;13:535–48. [PubMed] [Google Scholar]
- 51.Byrod G, Otani K, Brisby H. et al. Methylprednisolone reduces the early vascular permeability increase in spinal nerve roots induced by epidural nucleus pulposus application. J Orthop Res. 2000;18:983–87. doi: 10.1002/jor.1100180619. [DOI] [PubMed] [Google Scholar]
- 52.Lee HM, Weinstein JN, Meller ST. et al. The role of steroids and their effects on phospholipase A2: an animal model of radiculopathy. Spine (Phila Pa 1976) 1998;23:1191–6. doi: 10.1097/00007632-199806010-00001. [DOI] [PubMed] [Google Scholar]
- 53.Tachihara H, Sekiguchi M, Kikuchi S. et al. Do corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation. Spine (Phila Pa 1976) 2008;33:743–7. doi: 10.1097/BRS.0b013e3181696132. [DOI] [PubMed] [Google Scholar]
- 54.Sato C, Sakai A, Ikeda Y. et al. The prolonged analgesic effect of epidural ropivacaine in a rat model of neuropathic pain. Anesth Analg. 2008;106:313–20. doi: 10.1213/01.ane.0000296460.91012.51. [DOI] [PubMed] [Google Scholar]
- 55.Pasqualucci A. Experimental and clinical studies about the preemptive analgesia with local anesthetics. Possible reasons of the failure. Minerva Anestesiol. 1998;64:445–57. [PubMed] [Google Scholar]
- 56.Arner S, Lindblom U, Meyerson BA. et al. Prolonged relief of neuralgia after regional anesthetic block. A call for further experimental and systematic clinical studies. Pain. 1990;43:287–97. doi: 10.1016/0304-3959(90)90026-A. [DOI] [PubMed] [Google Scholar]
- 57.Altman DG, Schulz KF, Moher D, et al; CONSORT GROUP (Consolidated Standards of Reporting Trials). The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134:663–94. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 58.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74. doi: 10.1016/j.apmr.2007.08.126. [DOI] [PubMed] [Google Scholar]
- 59.Pietrobon R, Coeytaux RR, Carey TS. et al. Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine (Phila Pa 1976) 2002;27:515–22. doi: 10.1097/00007632-200203010-00012. [DOI] [PubMed] [Google Scholar]
- 60.Pereira J, Lawlor P, Vigano A. et al. Equianalgesic dose ratios for opioids. A critical review and proposals for long-term dosing. J Pain Symptom Manage. 2001;22:672–87. doi: 10.1016/s0885-3924(01)00294-9. [DOI] [PubMed] [Google Scholar]
- 61.Browner WS, Newman TB, Cummings SR, et al. Estimating sample size and power. In: Hulley SB, Cummings SR, et al., editors. Designing Clinical Research: An Epidemiologic Approach 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2001. pp. 65–84. [Google Scholar]
- 62.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials. Increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–32. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- 63.Iversen T, Solberg TK, Romner B. et al. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Manchikanti L, Giordano J, Fellows B. et al. Placebo and nocebo in interventional pain management: a friend or a foe - or simply foes? Pain Physician. 2011;14:E157–75. [PubMed] [Google Scholar]
- 65.Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010;11:1149–68. doi: 10.1111/j.1526-4637.2010.00908.x. [DOI] [PubMed] [Google Scholar]
- 66.Karppinen J, Malmivaara A, Kurunlahti M. et al. Periradicular infiltration for sciatica: a randomized controlled trial. Spine (Phila Pa 1976) 2001;26:1059–67. doi: 10.1097/00007632-200105010-00015. [DOI] [PubMed] [Google Scholar]
- 67.Carette S, Leclaire R, Marcoux S. et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997;336:1634–40. doi: 10.1056/NEJM199706053362303. [DOI] [PubMed] [Google Scholar]
- 68.Manchikanti L, Singh V, Falco FJE. In: response to Smuck M, Levin JH. RE: Manchikanti L, Singh V, Falco FJE, Cash KA, Fellows B. Cervical medial branch blocks for chronic cervical facet joint pain: a randomized double-blind, controlled trial with one-year follow-up. Spine (Phila Pa 1976) 2009;34:1116–7. doi: 10.1097/BRS.0b013e3181a0a262. [DOI] [PubMed] [Google Scholar]
- 69.Pham Dang C, Lelong A, Guilley J. et al. Effect on neurostimulation of injectates used for perineural space expansion before placement of a stimulating catheter: normal saline versus dextrose 5% in water. Reg Anesth Pain Med. 2009;34:398–403. doi: 10.1097/AAP.0b013e3181b48648. [DOI] [PubMed] [Google Scholar]
- 70.Tsui BC, Kropelin B, Ganapathy S. et al. Dextrose 5% in water: fluid medium maintaining electrical stimulation of peripheral nerve during stimulating catheter placement. Acta Anaesthesiol Scand. 2005;49:1562–65. doi: 10.1111/j.1399-6576.2005.00736.x. [DOI] [PubMed] [Google Scholar]
- 71.Indahl A, Kaigle AM, Reikeräs O. et al. Interaction between the porcine lumbar intervertebral disc, zygapophysial joints, and paraspinal muscles. Spine (Phila Pa 1976) 1997;22:2834–40. doi: 10.1097/00007632-199712150-00006. [DOI] [PubMed] [Google Scholar]
- 72.Indahl A, Kaigle A, Reikerås O. et al. Electromyographic response of the porcine multifidus musculature after nerve stimulation. Spine (Phila Pa 1976) 1995;20:2652–58. doi: 10.1097/00007632-199512150-00006. [DOI] [PubMed] [Google Scholar]