Abstract
Antibiotic resistance is now recognized as a major, global threat to human health and the need for the development of novel antibacterial therapies has become urgent. Lytic bacteriophages (phages) targeting individual bacterial pathogens have therapeutic potential as an alternative or adjunct to antibiotic use. Bacteriophage therapy has been used for decades, but clinical trials in this field are rare, leaving many questions unanswered as to its effectiveness for many infectious diseases. As a consequence bacteriophage therapy is not used or accepted in most parts of the world. The increasing need for new antimicrobial therapies is driving the development of bacteriophage therapies for a number of diseases but these require the successful completion of large-scale clinical trials in accordance with US FDA or European EMA guidelines. Bacteriophages are considered as biological agents by regulatory authorities and they are managed by biological medicinal products guidelines for European trials and guidelines of the division of vaccines and related product applications in the USA. Bacteriophage therapy is typically an ‘active’ treatment requiring multiplication in the bacterial host and therefore the factors that govern its success are different from those of conventional antibiotics. From the pharmacokinetic and pharmacodynamic points of view, time of treatment, dosage depending on the site of infection and the composition of the bacteriophage formulation (single vs multiple strains) need careful consideration when designing clinical trials. Scientific evidence regarding inflammatory effects, potential for gene transfer and phage resistance, need to be evaluated through such trials. However purity, stability and sterility of preparations for human use can be addressed through Good Manufacturing Practises to reduce many potential safety concerns. In this review we discuss the potential for the development of bacteriophage therapy in the context of critical aspects of modern, regulated clinical trials.
Keywords: Bacteriophage, active therapy, clinical trials, regulatory issues, safety, efficacy
INTRODUCTION
With the rising prevalence of antibiotic resistant-bacteria and the serious concerns raised by the World Health Organisation (Levy and Marshall, 2004; Cars et al, 2008; WHO 2011), new approaches to deal with bacterial infections have become an urgent need. Bacteriophage therapy has been applied for decades as a means of treating bacterial infections in some parts of the world and encouraging results have been documented (as reviewed in Kutter et al, 2010; Abedon et al, 2011; and described in Marza et al, 2006). To date very few human clinical trials have been conducted to modern standards in either the European Medicines Agency (EMA) or United States FDA jurisdictions. A few phase I studies have been conducted and published (Bruttin and Brüssow, 2005; Merabishvili et al, 2009; Rhoads et al, 2009;) while others have not been published to date. In 2009, a US Food and Drug Administration (FDA) approved bacteriophage phase I clinical trial was reported, evaluating a bacteriophage cocktail targeting Staphylococcus aureus, Pseudomonas aeruginosa and Escherichia coli in venous ulcers (Rhoads et al, 2009). The results of this trial showed this multi-bacteriophage preparation to be safe in trial subjects. Also in 2009, Biocontrol Ltd (UK), reported a double-blind placebo-controlled, randomized phase I/II clinical trial targeting chronic otitis caused by antibiotic-resistant P. aeruginosa. This was the first, and to date only, regulated efficacy trial of bacteriophage therapy. A positive result was reported showing decreasing levels of P. aeruginosa in the ear and improvement of clinical condition with a single input dose of 600,000 bacteriophages (Wright et al, 2009). These trials, alongside earlier, less well reported studies, indicate that phage therapy shows considerable promise for treating infectious diseases caused by antibiotic-resistant bacteria.
Despite numerous encouraging case studies, bacteriophage treatment has not been brought to mainstream medicine due to a lack of robust scientific evidence generated through systematically planned, controlled and regulated clinical trials. Recently, however, an increasing number of papers, reviews and books appearing on bacteriophage therapy, as well as the emergence of specifically dedicated commercial bacteriophage companies indicates an increasing appetite among the scientific community and industry for developing bacteriophage therapy as part of mainstream medicine (Waldor, 2005; Górski et al, 2007; Harper and Kutter, 2008; Kutter et al, 2010; Burrowes et al, 2011).
Current biomedical technology is vastly superior to that available during the early days of bacteriophage therapy. Our understanding of the biological properties of bacteriophages and the mechanisms of phage-bacterial host interactions has also improved dramatically. Although, our knowledge of the biology, genetics and bactericidal efficacy of bacteriophages in vitro are impressive, less is known about their behaviour in vivo, in particular in the human body.
Fully controlled clinical trials under the supervision of ethical committees and in compliance with the highest regulatory standards of leading Western jurisdictions need to be performed in order to develop robust, reliable data to answer the key clinical questions and to establish the safety and efficacy profile of bacteriophage therapy. The gold standard will be double blind, randomised controlled trials (RCTs) to avoid any bias, and extension to (international) multi-centre studies would also be crucial. This will provide the necessary scientific evidence for safe and effective bacteriophage therapeutics. Furthermore, comparative studies involving direct comparison with existing therapies will also be needed to answer some of today's questions.
This review is intended to highlight the critical aspects of regulated clinical trials in developing bacteriophage therapies.
REGULATORY CHALLENGES
Bacteriophage therapeutic products have already been marketed in Eastern European countries, such as the Republic of Georgia. In Poland, the Ethics Committee of Wroclaw Medical University approved a medical experiment now being conducted at the Phage Therapy Unit, a Healthcare Center affiliated with the Institute of Immunology and Experimental Therapy (IIET) in Wroclaw to treat drug-resistant bacterial infections (www.clinicaltrials.gov).
Several other clinical trials and case studies known to use bacteriophage therapy have been carried out under different jurisdictions. Individual countries have their own regulators, and levels of regulation can be highly variable. However, the current standard bacteriophage therapies used in Eastern Europe are unlikely to receive approval in the rest of Europe or USA without further work to prove therapeutic claims using regulated clinical trials.
The EMA considers bacteriophages as biological agents and although bacteriophage therapy falls under the existing European regulatory framework on biological medicinal products (Commission Directive 2001/83/EC) the directive does not fully cover aspects which are specific to bacteriophages. However, products such as vaccines (some of which are live viruses) that do not have specific regulatory guidelines have been approved by EMA and have shown great success in mainstream medicine.
Verbeken et al (2007) argued that bacteriophage should be considered as advanced therapy medicinal products (Commission Directive 2003/63/EC), which covers gene therapy, somatic cell therapy and tissue engineered products; however the European Commission has indicated that, as a “biological”, the existing regulatory framework is adequate for bacteriophage therapy. Therefore, the current European regulation framework on medicinal products may be the way forward for bacteriophage therapy in the European Union.
In the US, similar to the situation in Europe, no bacteriophage therapeutics guidelines for human use have been published by the FDA. Nevertheless, bacteriophage applications are handled by the Division of Vaccines and Related Product Applications of the Center for Biologicals Evaluation and Research (CBER).
While waiting for bacteriophage therapy to be fitted into the regulatory framework, a short term interim solution in Europe is to use bacteriophages as a therapy within the responsibility and supervision of medical ethical committees under the umbrella of the World Medical Association Declaration of Helsinki (Verbeken et al, 2007; WMA Declaration of Helsinki, 2008). However, this provisional solution is not a substitute for fully regulated clinical trials and consequently fails to move the product forward efficiently.
The FDA and the United States Department of Agriculture Food Safety and Inspection Service (USDA, FSIS) currently recognise commercial bacteriophage preparations against common bacterial pathogens such as Listeria monocytogenes and E. coli as safe and approved their use in food consumed by humans (71 Fed. Reg. 47729; 2006).
The first bacteriophage-based product formally approved by the United States government regulatory agency was AgriPhageTM, in 2005 (US EPA 2005), to treat crop diseases (targeting bacterial speck on crops, with specific formulations for strains of Xanthamonas campestris pv. Vesicatoria or P. syringae pv. Tomato). However, the first approved food safety-related bacteriophage product was ListShield™ (LMP-102™), from Intralytix Inc, a phage cocktail that targets L. monocytogenes contaminants on ready to eat (RTE) foods containing meat and poultry products (Bren, 2007). Approval was granted in 2006 and marks the first time that the FDA accepted the use of a phage preparation as a food additive. Similar food safety applications and other non-human applications in the agricultural, animal husbandry, veterinary and diagnostics sectors appear to be progressing well with an increasing number of products becoming available. Such products include AgriPhage, BioTector, EcoShield, Finalise, ListShield, LISTEXTM P100 (Monk et al, 2010; Ryan et al, 2011). Approval of these products should help to support acceptance of the application of bacteriophage therapeutics for humans.
However, a serious limitation for small-to-medium scale biotech companies seeking to carry out clinical trials is to find adequate funding. The lack of regulatory guidelines specific to bacteriophage does not currently provide assurance for potential investors that a finished product can be licensed (Skurnik et al, 2007). Also, there is little incentive for regulators to develop schemes when no marketed product exists. Nevertheless, going forward, the investigators and sponsors may need to have regular meetings with the regulatory agencies to discuss and review the trial strategy alongside the existing regulatory guidelines. It is also important to elicit expert knowledge of critical aspects of the trial in the absence of published data.
Bacteriophages are naturally occurring organisms. They have been used as therapeutic agents for almost a century and the basic technology is well established, therefore basic concepts are not patentable (Clark and March, 2006). This situation is similar to that of monoclonal antibodies, where a large number of potential agents exist and the basic technology lies in the public domain. However, with monoclonal antibodies a number of patent-protected technical developments, along with the progression of individual agents through advanced testing underpin expanding markets worth of tens of billions of dollars annually. As with monoclonal antibodies, individual bacteriophages are patentable since they can be deposited in an approved collection under the Budapest treaty (http://www.wipo.int). But, again as with monoclonal antibodies, there are always other bacteriophages in the environment that may be isolated and used to formulate a competing phage preparation. In consequence, it is both progression through clinical trials and individual technical developments (whether patented or as proprietary knowledge) that can underpin the commercialisation of bacteriophages, rather than more sweeping patent claims.
Early uses of relatively crude mixtures of antibodies as anti-infectives have largely been replaced by more precise technologies. Key to this was the ability to purify high levels of individual antibodies. This was achieved by the purification of individual producer cells, hence the use of the term “monoclonal”. Similarly, early bacteriophage preparations used poorly characterised mixtures, while newer work uses high purity, well characterised and fully defined bacteriophages. It is these clonally purified bacteriophages that will form the basis of future applications which are compliant with regulatory processes. It is perhaps appropriate to refer to these new generation therapeutics by a distinct name, perhaps even as “monoclonal bacteriophages” (since that is what they actually are) in order to differentiate them from earlier approaches.
The practical considerations on the development of regulatory compliance in formulations of bacteriophages will be discussed in more detail below.
CLINICAL TRIAL DESIGN CONSIDERATIONS
The trial design aspects of a bacteriophage clinical trial will not be vastly different to any other clinical trial design. However, there are a few unique differences in bacteriophage therapy compared to a standard drug or vaccine particularly due to its self-replicating ability as well as due to specificity of the bacteriophage.
PK/PD data and dose finding
Bacteriophages are typically used as an active (self-replicating) treatment, and more often as a topical rather than a systemic treatment. Hence, conventional pharmacokinetic (PK) investigational methodologies may not be applicable. However, the clinical information on bacteriophage concentrations at the site of action and subsequent elimination are crucial in designing the dosing schedule when more than one dose is deemed necessary. Also, the dose for one application (e.g., skin) may not be suitable for another (e.g., gastro-intestinal diseases where the bacteriophage need to be ingested and act inside the body). The bacteriophage concentration at the infection site, bodily distribution and rate of clearance (Parisien et al, 2008) of the bacteriophages after application will provide useful information for the clinician's understanding of a given bacteriophage application. For an effective treatment, as a rule of thumb, the product of the number of bacteriophages (PFU) and the host bacteria (CFU) ranges from 109 to 1011. Thus, for a lower concentration of bacteria, a higher number of bacteriophages is needed, and vice versa.
From a pharmacodynamics (PD) point of view, efficacy of the therapy depends on a few key parameters that are not familiar in chemo-based pharmaceutical products (Payne et al, 2000). The primary mode of action of bacteriophage is bacteriolysis, which requires adsorption of the phage tail to a specific receptor on the bacterial cell wall and there should be a sufficient number of bacterial cells (proliferation threshold) for bacteriophages to sustain their numbers at the initial stage of the application. Mathematically, number of encounters between bacteria and bacteriophage in a fixed volume of liquid is defined as:
k*t*V*P*N
where, k = adsorption constant; t = time; V = volume; P = bacteriophage density (constant); N = bacterial density (constant)
This assumes free circulation and does not allow for restricted access, bacterial mortality or masking by other substances. The adsorption constant (k), was empirically defined by Stent (1963) for T4 Myophage as 2.5x109. It appears that it is correlated with the proliferation threshold. There are several other mathematical models to describe the interaction between bacteriophage and bacteria (Payne and Jansen, 2003; Levin and Bull, 2004), however more empirical data are needed to validate these models.
A number of previous reports (Marza et al, 2006; Wright et al, 2009; Hawkins et al, 2010) indicate that a bacteriophage count of 102-103 plaque forming unit (PFU) is sufficient to initiate a therapeutic replication with a 106-109 CFU per ml proliferation threshold of bacteria in vivo. Trials to date have used between 105 and 109 PFU of individual bacteriophages (Bruttin and Brüssow, 2005; Merabishvili et al, 2009; Rhoads et al, 2009; Wright et al, 2009).
Some studies have addressed the issue of the replication threshold in vitro; with estimates ranging from 104-106 CFU per ml in combination with 102-103 PFU (Wiggins and Alexander, 1985) depending on the experimental situation. This is somewhat lower than equivalent numbers in vivo, which may reflect the more complex situation in the latter setting. At the same time, some researchers deny that a replication threshold is relevant (Kasman et al. 2002).
The proliferation onset time (the time required for the bacteria to reach proliferation threshold) is another key efficacy parameter that influences the success of bacteriophage treatments. However, the timing of treatment is crucial for acute infections but is less crucial in chronic infections where the infectious bacterial population is found in abundance (Maura and Debarbieux, 2011). To combat this problem in a clinical trial setting for an acute or premature stage of infection repeat dosing or use of higher titers of bacteriophages may be necessary, as is seen in some animal models of acute infections (Debarbieux et al, 2010; Morello et al, 2011).
Workers are thus faced with a range of challenges to provide robust clinical data on these efficacy parameters for different types of infections when applying for approved bacteriophage therapeutics.
Monotherapy vs combination therapy
In standard chemo-therapeutic approaches, mono and combination therapy refers to use of a single drug compared to use of multiple drugs at a given time. An analogous treatment strategy exists with bacteriophage when using a single bacteriophage compared to the use of a “cocktail” of multiple bacteriophage strains. However, use of cocktails as a combined therapy poses some challenges in proving the specificity or the role of individual viruses. On the positive side the cocktails will minimise the disadvantages of bacteriophages being specific to a limited number of strains. That is to say, in an unknown infection it is more likely that a bacteriophage combination therapy will be successful compared to bacteriophage monotherapy with the possible exception of broad spectrum bacteriophages such as S. aureus bacteriophage K (O'Flaherty et al, 2005). Moreover, properly selected cocktails can minimise the potential for resistance arising in the target bacteria, since one mutation could provide resistance to a single phage, no matter how broad its spectrum of activity. Unsurprisingly, cocktails have been used in the majority of clinical trials reported to date.
Study population
It is an absolutely critical aspect of a trial to define the patient population and the disease stage (acute, chronic, etc.) that the final regulatory-approved therapeutic label is based upon. If the claim of the bacteriophage therapy is associated with treating antibiotic resistant patients with chronic disease, the study eligibility criteria should be set accordingly. In other words, there should be clear guidelines to identify the antibiotic resistant patients who are suffering from a specified chronic disease the trial is intended to treat.
Efficacy and safety study parameters
Efficacy
The common efficacy parameters of bacterial infective disease for registrational trials are of two types:
Patient/physician reported outcomes of the patient (typically primary endpoint)
Population dynamics of the infective bacteria (typically secondary endpoint)
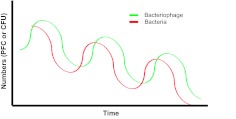
In addition, bacteriophage population dynamics could also be used to complement the above data and provide additional information on the efficacy of bacteriophage therapy (Figure 1). These biological endpoints will be primary in pre-clinical or early phase trials.
Figure 1.
Population dynamics of bacteria (CFU) during an “active” bacteriophage (PFU) therapy with a single dose of agent. Bacteriophage multiplies in vivo, and clears when infection resolves.
Although the patient/physician reported outcomes are of high value and reflect the tangible results to the patients it is also important to acknowledge the subjectivity in these outcomes. Therefore, defining a more profound, clinically meaningful quantitative outcome or an objective definition for the cure rate for bacteriophage therapy might be an area where scientists and clinicians will have to work together to provide convincing evidence to the regulatory bodies on the performance of bacteriophage therapeutics.
Safety
Safety aspects of the therapy are associated with the potential toxicities that can result directly or indirectly and the impact on non-target tissues. However, bacteriophage-associated side effects are uncommon since bacteriophages and their products do not affect eukaryotic cells (Matsuzaki et al, 2005). Although claims for safety are supported by the exposure of humans to high levels of ubiquitous bacteriophages via everyday activities (Harper and Enright, 2011), there are at least three safety concerns the controlled clinical trials need to consider:
The presence of bacterial materials, including toxins, pyrogens and other debris (Brüssow et al, 2004). This has to be addressed at the bacteriophage preparatory stage, and with current technological developments a high degree of purity can be achieved at laboratory scales (Denou et al, 2009). To address this, bacteriophage production for clinical trials under FDA or EMA supervision is required to follow specific Good Manufacturing Practice (GMP) guidelines with appropriate quantity controls (Gill and Hyman, 2010), and to meet specific standards for purity and sterility.
The Herxheimer effect due to unusually high levels of endotoxins liberated by rapid bacteriolysis or bacteriophage-carrying endotoxins. This phenomenon was observed with some bactericidal antibiotics (Rac, 2010) when used to treat severe bacterial infections (such as, spirochetal infections) where high numbers of bacteria are present. The near-simultaneous lysis of the target bacteria can release high levels of toxins (endotoxins), produce an autoimmune response to the toxins. Despite some concerns (Dixon, 2004) no such phenomenon has been reported with bacteriophages, even when this has been the intention of the study (Soothill, 2004). It is likely that the sequential multiplication of bacteriophages produces a longer duration of bacteriolytic effect, reducing the effects of such release. However, this is an area to monitor in trials of bacteriophage therapeutics.
The ability of at least some lytic bacteriophages to mediate low-level generalised transduction, possibly resulting in the transfer of bacterial genes, with the potential to result in a more pathogenic or antibiotic-resistant bacterial hosts (Waddell et al, 2009). From a clinical perspective, obligate lytic bacteriophages are highly desirable and are generally regarded as safe (Burdock and Carabin, 2004). These reduce the potential for transduction via rapid killing.
Overall, in terms of risk benefit, when viewed in comparison with antibiotic treatments where long lasting or serious adverse events may occur in some cases (Hamilton, 2011), phage therapy may be seen as acceptable (Sulakvelidze et al, 2001).
Standardization and quality control of bacteriophage therapies
Despite the absence of specific guidelines for therapeutic bacteriophage products, in the current medicinal product regulations (Verbeken et al, 2007), some of the existing requirements for live viral vaccines can be used as a guide for bacteriophage-based clinical products. Also, the guidelines for biotechnological/biological products, hygiene products and bacteriophage based food-use product approved by regulatory agencies can be used as a basis for evaluating bacteriophage preparations for therapeutic purposes.
According to International Conference on Harmonisation (ICH) guideline Q5C (Quality of Biotechnological/Biological Products) the manufacturer should propose a stability indicating profile to ensure that changes in identity, purity and potency of the product will be detected. The same requests will apply to assure the identity, biological activity, purity and quality of bacteriophage-drug products when used for humans. In achieving this objective, standardization and validation of the techniques used for purification, removal of endotoxins and stability should be prioritised.
Whether the bacteriophage therapeutic product is a single phage with broad specificity or a phage cocktail, it is recommended that all components in the product should be individually characterised (both genomically and phenotypically) and analysed. Bacteriophage being a biological agent, the natural variations of the organism is an important factor to be considered. One of the main reasons for individual characterisation is that any possible shifts could be detected more easily.
Therefore in order to achieve a successful therapeutic bacteriophage preparation to be used as a clinical product, standardisation and specific protocols for the following parameters would be very important:
Bacteriophage identification
Potency and biological activity of bacteriophage preparations
Product purity
Stability and storage conditions of phage preparations
Control of sterility
Manufacturing process considerations
Suitable identification and monitoring of bacteriophage preparations for use in clinical trials is crucial. Each bacteriophage should be identified to make sure the preparation contains only well-defined bacteriophages. After manufacture, to produce the drug substance they can be mixed together to produce the bacteriophage cocktail product for application (drug product). The product should also be monitored after multiple bacteriophages have been mixed in a cocktail product.
All bacteriophage species used in human clinical trials should be obligately lytic (virulent) as a minimum requirement to ensure the safety of the product. The morphological types of bacteriophages used should be identified. Table 1 summarises the techniques used for characterisation of high quality bacteriophage preparations for therapeutic applications.
Table 1.
Quality parameters of bacteriophage-drug substances and assessment methods
| Specification | Test Method | Acceptance Criteria |
|---|---|---|
| Identity | DNA sequencing | Lytic (absence of lysogenic cassettes) |
| Absence of toxins or other undesirable genes | ||
| Transmission electron microscopy with negative staining (TEM) | Morphological classification (i.e., Myoviridae, Siphoviridae, Podoviridae). | |
| PCR (primers) can be developed for known genes | Absence of transduction (toxins or lysogenic genes); and taxonomical classification | |
| Host activity and Identity“ | Cross-plate”technique | Phage sensitivity profile compared with standard |
| Potency (titre) | Agar overlay plaque assay technique | Bacteriophage concentration (titration) of each bacteriophage particles (pfu) in a volume of 1ml |
| Biofilm models vs Plaque assay | Bacteriophage concentration (amplification) in biofilms, enhanced in vitro activity in some systems | |
| OD measurement at 600nm | Evaluation of bacterial lysis by measuring the optical density at 600nm in comparison to control cultures. | |
| DNA fingerprinting (Purity) | RFLP, PFGE, PCR, RAPD* | RFLP - conformation to reference standards |
| Protein content (residual or host-cell protein content) | Protein assays i.e. Bio-Rad Bradford | Protein content (>0.7µg/ml) |
| Protein fingerprinting (purity) | SDS-Page** and/or Western blots | Measure relative amounts of protein and reveals proteins of interests |
| Endotoxin | LAL***assay EP <2.6.14> LAL*** assay USP <85> |
<0.5 EU/mg**** |
| Sterility | EP test for sterility <2.6.1> USP test for sterility <71> |
Product sterile |
Restriction fragment length polymorphism (RFLP), Pulsed field gel electrophoresis (PFGE), polymerase chain reaction (PCR), random amplified polymorphic DNA (RAPD)
sodium dodecyl sulphate (SDS) polyacrylamide gel electrophoresis
Limulus amoebocyte lysate (LAL)
Maximum level of endotoxin for intravenous applications of pharmaceutical and biologic product is set to 5 endotoxin units (EU) per kg of body weight per hour by European and US pharmacopoeias.
Stability and storage of phage preparations
The stability data on bacteriophage-based clinical products is important because the preparations must have a shelf-life long enough for the duration of the study or to support commercial applications (Withington, 2001). Any change with the potential to alter the bacteriophage concentration or profiles should be evaluated for its impact on stability. Temperature, pH and buffer/gel compositions are some stability parameters. However, the optimal conditions for phage preservation can vary for each strain. Some bacteriophages are very stable and can be stored in wide-ranging conditions while others are fragile and need special attention (Ackermann et al, 2004; Merabishvili et al, 2009; Yang et al, 2010; Jończyk et al, 2011). If a bacteriophage cocktail is to be used in a clinical study, each individual strain should be tested. The testing program should define test intervals for each storage condition investigated and the tests to be performed at each interval.
Control of sterility
All products to be used in a clinical trial should be sterilized by processes that are properly validated. For example, the guidelines for sterility testing of biologics are addressed in the various worldwide pharmacopeias (e.g., USP, EP and JP), Section 21 of the Code of Federal Regulations (CFR), ICH and FDA Points to Consider (PTC) documents. The same guidelines will need to be applied to test bacteriophage preparations.
Manufacturing process considerations
All pharmaceutical products used in clinical trials must be manufactured according to GMP guidelines and these are equally applicable for bacteriophage formulations in order to ensure that bacteriophage products are effective, safe and pure. Moreover, all manufacturing process details, including growth media composition, conditions of fermentation, filtration methods, purification processes, and the methods employed for the evaluation of the bacteriophage preparations will be important components of the regulatory filing for marketing approval.
CONCLUSIONS
Concerns over the increased incidence of antibiotic resistance and lack of effective novel antibiotics have revived interest in bacteriophage therapeutics as an approach to controlling bacterial infections. Despite the modern knowledge on the genetics and physiology of bacteriophages, there is a lack of formal, well-controlled, large scale clinical studies on their safety and efficacy as therapeutic agents. Industry and regulatory bodies (FDA and EMA) are actively working towards this goal, using the Biological Medicinal Products guidelines for European trials, and the guidelines of the Division of Vaccines and Related Product Applications in the USA, as a starting point.
Standardised protocols to evaluate safe and efficacious bacteriophage products are necessary. The mode of action of bacteriophage is unique and different to any pharmaceutical product in current use. Hence, conventional methodologies have little use in understanding many aspects of their use, for example their PK and PD. Well-designed clinical trials are needed to ensure the highest standards of data and data collection. It has been suggested that bacteriophages may be considered safe on the grounds that bacteriophages are naturally occurring ubiquitous viruses to which humans are widely exposed. However, researchers need to generate systematic information on potential safety issues to verify this claim.
There are some practical issues such as purity, stability and sterility to be addressed via GMP before entering bacteriophage formulations into clinical trials. Appropriate procedures will reduce the chance of impure product or of contamination with bacteriophages carrying genes encoding toxins or factors that enhance bacterial pathogenicity in order to assure therapeutic safety.
The industry is faced with challenges to find sponsors for bacteriophage trials as there is still perceived to be uncertainty on obtaining marketing approval. Going forward, industry and the regulatory bodies should work closely to bridge the gaps and find mutually acceptable solutions to overcome the barriers. Experts in the field have a crucial role to play in guiding the industry in places where not much knowledge is available.
LIST OF ABBREVIATIONS
- CBER
Center for Biologics Evaluation and Research
- CFU
Colony forming units
- EMA
European Medicines Agency
- EP
European Pharmacopoeia
- FDA
Food and Drug Administration
- FSIS
Food Safety and Inspection
- GMP
Good manufacturing practice
- ICH
International conference on harmonisation
- LAL
Limulus amoebocyte lysate
- PD
Pharmacodynamics
- PFGE
Pulsed field gel electrophoresis
- PFU
Plaque-forming units
- PK
Pharmacokinetics
- RAPD
Random amplified polymorphic DNA
- RCTs
Randomised controlled trials
- RFLP
Restriction fragment length polymorphism
- USDA
United States Department of Agriculture
- USP
United States Pharmacopeia
COMPETING INTERESTS
The authors are employed by AmpliPhi Biosciences Corporation (DR Harper) and/or by its wholly owned subsidiary Biocontrol Limited (DR Harper, HMRT Parracho, BH Burrowes, MC Enright, ML McConville). DR Harper is a director of Biocontrol Limited and a shareholder in AmpliPhi Biosciences Corporation. All authors hold or are anticipating holding share options in AmpliPhi Biosciences. The authors have no other relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from the disclosed. No writing assistance was utilised in the production of this manuscript.
REFERENCES
- Abedon ST, Kuhl SJ, Blasdel BG, Kutter EM. Phage treatments of human infections. Bacteriophage. 2011;1:66–85. doi: 10.4161/bact.1.2.15845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerman H-W, Tremblay D, Moineau S. Long-term bacteriophage preservation. World Federation for culture Collections Newsletter. 2004;38:35–40. [Google Scholar]
- Bren L. Bacteria-eating virus approved as food additive. FDA Consum. 2007;41:20–22. [PubMed] [Google Scholar]
- Brüssow H, Canchaya C, Hardt WD. Phages and the evolution of bacterial pathogens: from genomic rearrangements to lysogenic conversion. Microbiol Mol Biol Rev. 2004;68:560–602. doi: 10.1128/MMBR.68.3.560-602.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruttin A, Brüssow H. Human volunteers receiving Escherichia coli phage T4 orally: a safety test of phage therapy. Antimicrob Agents Chemother. 2005;49:2874–2878. doi: 10.1128/AAC.49.7.2874-2878.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdock GA, Carabin A. Generally recognized as safe (GRAS): history and description. Toxicol Lett. 2004;150:3–18. doi: 10.1016/j.toxlet.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Burrowes B, Harper DR, Anderson J, McConville M, Enright MC. Bacteriophage therapy: potential uses in the control of antibiotic-resistant pathogens. Expert Rev Anti Infect Ther. 2011;9:775–85. doi: 10.1586/eri.11.90. [DOI] [PubMed] [Google Scholar]
- Cars O, Högberg LD, Murray M, et al. Meeting the challenge of antibiotic resistance. BMJ. 2008;337:726–728. doi: 10.1136/bmj.a1438. [DOI] [PubMed] [Google Scholar]
- Clarck JR, March JB. Bacteriophages and biotechnology: vaccines, gene therapy and antibacterials. Trends Biotechnol. 2006;24:212–218. doi: 10.1016/j.tibtech.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Debarbieux L, Leduc D, Maura D, et al. Bacteriophages can treat and prevent Pseudomonas aeruginosa lung infections. J Infect Dis. 2010;201:1096–1104. doi: 10.1086/651135. [DOI] [PubMed] [Google Scholar]
- Denou E, Bruttin A, Barretto C, Ngom-Bru C, Brüssow H, Zuber S. T4 phages against Escherichia coli diarrhea: Potential and problems. Virology. 2009;388:121–130. doi: 10.1016/j.virol.2009.03.009. [DOI] [PubMed] [Google Scholar]
- Dixon B. New dawn for phage therapy. Lancet Infect Dis. 2004;4:186. doi: 10.1016/S1473-3099(04)00951-X. [DOI] [PubMed] [Google Scholar]
- Gill JJ, Hyman P. Phage choice, isolation, and preparation for phage therapy. Curr Pharm Biotechnol. 2010;11:2–14. doi: 10.2174/138920110790725311. [DOI] [PubMed] [Google Scholar]
- Górski A, Borysowski J, Miedzybrodzki R, Weber-Dabrowska B. Caister Academic Press; Norfolk, UK: 2007. Bacteriophages in medicine. In: McGrath S and van Sinderen D (Eds) Bacteriophage: Genetics and Molecular Biology; pp. 126–158. [Google Scholar]
- Hamilton RJ. Jones & Bartlett Publishers; Massachusetts, USA: 2011. Tarascon Pharmacopoeia 2011 Library Edition. [Google Scholar]
- Harper DR, Enright MC. Bacteriophages for the treatment of Pseudomonas aeruginosa infections. J Appl Microbiol. 2011;111:1–7. doi: 10.1111/j.1365-2672.2011.05003.x. [DOI] [PubMed] [Google Scholar]
- Harper DR, Kutter E. The Encyclopedia of Life Sciences. John Wiley & Sons; Chichester, UK: 2008. Bacteriophage: therapeutic uses. [Google Scholar]
- Jończyk E, Klak M, Miedzybrodzki R, Górski A. The influence of external factors on bacteriophages – review. Folia Microbiol (Praha) 2011;56:191–200. doi: 10.1007/s12223-011-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasman LM, Kasman A, Westwater C, Dolan J, Schmidt MG, Norris JS. Overcoming the phage replication threshold: a mathematical model with implications for phage therapy. J Virol. 2002;76:5557–5564. doi: 10.1128/JVI.76.11.5557-5564.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutter E, De Vos D, Gvasalia G, et al. Phage therapy in clinical practice: treatment of human infections. Curr Pharm Biotechnol. 2010;11:69–86. doi: 10.2174/138920110790725401. [DOI] [PubMed] [Google Scholar]
- Levin BR, Bull JJ. Population and evolutionary dynamics of phage therapy. Nat Rev Microbiol. 2004;2:166–173. doi: 10.1038/nrmicro822. [DOI] [PubMed] [Google Scholar]
- Levy SB, Marshall B. Antibacterial resistance worldwide: causes, challenges and responses. Nat Med. 2004;10:S122–9. doi: 10.1038/nm1145. [DOI] [PubMed] [Google Scholar]
- Marza JA, Soothill JS, Boydell P, Collyns TA. Multiplication of therapeutically administered bacteriophages in Pseudomonas infected patients. Burns. 2006;32:644–666. doi: 10.1016/j.burns.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Matsuzaki S, Rashel M, Uchiyama J, et al. Bacteriophage therapy: a revitalized therapy against bacterial infectious diseases. J Infect Chemother. 2005;11:211–219. doi: 10.1007/s10156-005-0408-9. [DOI] [PubMed] [Google Scholar]
- Maura D, Debarbieux L. Bacteriophages as twenty-first century antibacterial tools for food and medicine. Appl Microbiol Biotechnol. 2011;90:851–859. doi: 10.1007/s00253-011-3227-1. [DOI] [PubMed] [Google Scholar]
- Merabishvili M, Pirnay J-P, Verbeken G, et al. Quality-controlled small-scale production of a well-defined bacteriophage cocktail for use in human clinical trials. PLoS ONE. 2009;4:e4944. doi: 10.1371/journal.pone.0004944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk AB, Rees CD, Barrow P, Hagens S, Harper DR. Bacteriophage applications: where are we now? Lett Appl Microbiol. 2010;51:363–9. doi: 10.1111/j.1472-765X.2010.02916.x. [DOI] [PubMed] [Google Scholar]
- Morello E, Saussereau E, Maura D, Huerre M, Touqui L, Debarbieux L. Pulmonary bacteriophage therapy on Pseudomonas aeruginosa cystic fibrosis strains: first steps towards treatment and prevention. PLoS One. 2011;6:e16963. doi: 10.1371/journal.pone.0016963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Flaherty S, Ross RP, Meaney W, Fitzgerald GF, Elbreki MF, Coffey A. Potential of the polyvalent anti-Staphylococcus bacteriophage K for control of antibiotic-resistant staphylococci from hospitals. Appl Environ Microbiol. 2005;71:1836–1842. doi: 10.1128/AEM.71.4.1836-1842.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parisien A, Allain B, Zhang J, Mandeville R, Lan CQ. Novel alternatives to antibiotics: bacteriophages, bacterial cell wall hydrolases, and antimicrobial peptides. J Appl Microbiol. 2008;104:1–13. doi: 10.1111/j.1365-2672.2007.03498.x. [DOI] [PubMed] [Google Scholar]
- Payne RJ, Jansen VA. Pharmacokinetic principles of bacteriophage therapy. Clin Pharmacokinet. 2003;42:315–25. doi: 10.2165/00003088-200342040-00002. [DOI] [PubMed] [Google Scholar]
- Payne RJ, Phil D, Jansen VA. Phage therapy: the peculiar kinetics of self-replicating pharmaceuticals. Clin Pharmacol Ther. 2000;68:225–30. doi: 10.1067/mcp.2000.109520. [DOI] [PubMed] [Google Scholar]
- Rac MW, Greer LG, Wendel GD., Jr Jarisch Herxheimer reaction triggered by group B streptococcus intrapartum antibiotic prophylaxis. Obstet Gynecol. 2010;116(Suppl 2):552–556. doi: 10.1097/AOG.0b013e3181e7d065. [DOI] [PubMed] [Google Scholar]
- Rhoads DD, Wolcott RD, Kuskowski MA, Wolcott BM, Ward LS, Sulakvelidze A. Bacteriophage therapy of venous leg ulcers in humans: results of a phase I safety trial. J Wound Care. 2009;18:237–243. doi: 10.12968/jowc.2009.18.6.42801. [DOI] [PubMed] [Google Scholar]
- Ryan EM, Gorman SP, Donnelly RF, Gilmore BF. Recent advances in bacteriophage therapy: how delivery routes, formulation, concentration and timing influence the success of phage therapy. J Pharm Pharmacol. 2001;63:1253–1264. doi: 10.1111/j.2042-7158.2011.01324.x. [DOI] [PubMed] [Google Scholar]
- Skurnik M, Pajunen M, Kiiljunen S. Biotechnology challenges of phage therapy. Biotechnol Lett. 2007;29:995–1003. doi: 10.1007/s10529-007-9346-1. [DOI] [PubMed] [Google Scholar]
- Soothill J, Hawkins C, Anggård E, Harper D. Therapeutic use of bacteriophages. Lancet Infect Dis. 2004;4:544–545. doi: 10.1016/S1473-3099(04)01127-2. [DOI] [PubMed] [Google Scholar]
- Stent GS. WH Freeman and Co; San Francisco, CA, USA: 1963. Molecular Biology of Bacterial Viruses. [Google Scholar]
- Sulakvelidze A, Alavidze Z, Morris JG., Jr Bacteriophage therapy. Antimicrob. Agents Chemother. 2001;45:649–659. doi: 10.1128/AAC.45.3.649-659.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Environmental Protection Agency Xanthomonas campestris pv. vesicatoria and Pseudomonas syringae pv. tomato specific bacteriophages: exemption from the requirement of a tolerance. http://www.epa.gov/EPA-PEST/2005/December/Day-28/p24540.pdf. Federal Register. 2005;70:76700–76704. Available from. Accessed October 31, 2011. [Google Scholar]
- Verbeken G, De Vos D, Vaneechoutte M, Merabishvili M, Zizi M, Prinay J-P. European regulatory conundrum of phage therapy. Future Microbiol. 2007;2:485–491. doi: 10.2217/17460913.2.5.485. [DOI] [PubMed] [Google Scholar]
- Waddell TE, Franklin K, Mazzocco A, Kropinski AM, Johnson RP. Clokie MRJ, Kropinski AM. Bacteriophages: Methods and protocols, Volume 1: Isolation, characterisation, and interactions. Humana Press; New York, USA: 2009. Generalized transduction by lytic bacteriophages; pp. 293–303. (Eds) [DOI] [PubMed] [Google Scholar]
- Waldor MK, Friedman DI, Adhya SL. ASM Press; Washington DC, USA: 2005. Phages: their role in bacterial pathogenesis and biotechnology. [Google Scholar]
- Wiggins BA, Alexander M. Minimum bacterial density for bacteriophage replication: implications for significance of bacteriophages in natural ecosystems. 1985;49:19–23. doi: 10.1128/aem.49.1.19-23.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Withington R. Regulatory issues for phage-based clinical products. J Chem Technol Biotechnol. 2001;76:673–676. [Google Scholar]
- WMA Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. Adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964 and amended by the: 59th WMA General Assembly; Seoul, Korea. October 2008. paragraph 32. [Google Scholar]
- World Health Organization Race against time to develop new antibiotics. Bull World Health Organ. 2011;89:88–89. doi: 10.2471/BLT.11.030211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright A, Hawkins CH, Anggård EE, Harper DR. A controlled clinical trial of a therapeutic bacteriophage preparation in chronic otitis due to antibiotic-resistant Pseudomonas aeruginosa; a preliminary report of efficacy. Clin Otolaryngol. 2009;34:349–57. doi: 10.1111/j.1749-4486.2009.01973.x. [DOI] [PubMed] [Google Scholar]
- Yang H, Liang L, Lin S, Jia S. Isolation and characterisation of a virulent AB1 of Acinetobacter baumanii. BMC Microbiol. 2010;10:131. doi: 10.1186/1471-2180-10-131. [DOI] [PMC free article] [PubMed] [Google Scholar]