Abstract
Background
Respiratory tract infections (RTIs) comprise the most common indication for consulting a general practitioner and obtaining an antibiotic prescription.
Objective
To study changes in the number of visits, diagnoses, and antibiotic prescriptions for RTI in primary healthcare during the period 1999–2005.
Design
A retrospective, descriptive, population-based study of electronic patient records.
Setting
County of Kalmar in southeastern Sweden.
Patients
Patients visiting primary healthcare units in Kalmar County for an RTI between 1 July 1999 and 31 December 2005.
Main outcome measures.
RTI diagnoses, antibiotic prescriptions, age groups.
Results
A total of 240 447 visits for RTI made between 1999 and 2005 were analysed. The yearly consultation rates for the diagnoses acute tonsillitis and AOM decreased by 12% and 10%, respectively (p = 0.001). Of all patients consulting for an RTI diagnosis, 45% received antibiotics. Of all prescribed antibiotics, 60% were for phenoxymethylpenicillin (PcV) and 18% doxycycline. Amoxicillin or amoxicillin + clavulanic acid was prescribed to a lesser extent. The proportion of patients obtaining an antibiotic prescription was almost constant over time (44–46%). The prescriptions of doxycycline showed increasing values (NS). The prescriptions of remaining antibiotics decreased significantly especially for patients up to middle age.
Conclusion
This large population study, comprising more than six years of observations, showed the number of primary healthcare patients receiving an RTI diagnosis decreased during the period 1999–2005, but the proportion of patients receiving an antibiotic prescription remained the same. The large seasonal variations indicate a need for further interventions to decrease antibiotic use for RTIs.
Keywords: Antibiotics, electronic patient records, family practice, general practice, phenoxymethylpenicillin (PcV), primary healthcare, respiratory tract infections
Antibiotics for respiratory tract infections are a cause of constant concern in this era of increasing bacterial resistance.
The diagnoses acute tonsillitis and AOM decreased by 10%/12% per year during the study period 1999–2005.
Independent of decreasing yearly consultation rates for RTI, the proportion of patients obtaining an antibiotic prescription was almost constant over time (44–46%).
Antibiotic prescriptions for patients below age 45 decreased significantly for all antibiotic classes except tetracycline.
The seasonal variation in antibiotic prescribing indicates that antibiotics are still used more than necessary.
Respiratory tract infections (RTIs) are the most common reason for consulting a general practitioner (GP) [1], [2]. Most antibiotics are prescribed in primary care for such symptoms despite the fact that most are caused by viruses [3], [4]. The benefit of antibiotic treatment for most RTIs is limited, only marginally affecting symptoms and recovery time [5].
Increasing use of antibiotics and the spread of multiresistant pneumococci in Sweden in the 1990s [6], [7] incited the formation of Strama (the Swedish strategic programme for rational use of antibiotics and surveillance of resistance) in 1995. Strama played a major part in the reduction of antibiotic use in Sweden between 1995 and 2005 [8] by an average of 22%, and for children by 50% [9]. In addition, new guidelines were developed for the treatment of acute otitis media in 2000 [10], acute sore throat in 2001 [11], and acute rhinosinusitis in 2005 [12], which may have influenced antibiotic prescription rates in outpatient care. Furthermore, diagnosis-prescribing studies performed in primary care during one week in the year 2000, 2002, and 2005 have shown that antibiotic prescribing can be further improved and has indicated that the visit rates for RTI have declined [8], [13]. However, the results of such short study periods may be influenced by epidemics and can be questioned.
The aim of this study was to describe changes in the number of consultations for RTI, diagnostic categories and antibiotic prescriptions in a Swedish county over a six year period.
Material and methods
Setting and population
In the middle of the study period (31 December 2002) the population of Kalmar County comprised 234 627 individuals, 118 070 women and 116 557 men [14].
Some 32 primary healthcare centres and several private healthcare providers serve the population of Kalmar County. In this study, the 21 primary healthcare centres and two private healthcare providers using the same electronic patient record (EPR) system participated from 1 January 1999 to 31 December 2005.
Material and methods
The database of the EPR system Swedestar was accessible online, allowing extraction and analysis of patient data. All patients visiting the primary healthcare centre were registered on the electronic patient data system and identified by their social security numbers. The registration of diagnoses using a primary care adapted, ICD-10 [15] based classification system, the so-called KSH 97P [16], was compulsory. The registration of diagnoses was exclusively by physicians.
When using the integrated drug-prescribing module, all drugs were automatically registered according to the Anatomical Therapeutic Chemical Classification System (ATC) [17].
All general practitioner (GP) consultations (office and out-of-office hours), receiving an RTI diagnosis according to the current classification KSH 97P were included. Rare diagnoses or combined diagnoses with a consultation frequency lower than 1000 of the 240 447 included consultations were classified as “others”. For selected analyses, common cold, pharyngitis, tonsillitis, acute otitis media, sinusitis, and laryngitis were grouped together as “upper respiratory tract infections” (URTIs) and influenza, acute bronchitis, and pneumonia as “lower respiratory tract infections” (LRTIs). Similarly, rare antibiotics and less common combinations were lumped together.
The following data were extracted from electronic patient records: date of consultation, age, gender, diagnosis, and prescribed antibiotics (ATC code). Data were extracted quarterly from July 1999 to December 2005 and further presented from July to June to avoid the influence of viral epidemics.
The study was approved by the regional ethical review board in Linköping. (Dnr M40-07)
Statistics
Most data were descriptive and units are described in figure legends and tables. Trends were analysed by linear regression analysis using logarithmic data on counts (number of visits) as the dependent variable, and quarter of years (from third quarter 1999 to last quarter 2005; n = 26) as the independent. This allows the change to be expressed in per cent per year (%Δ/yr) by multiplying the regression coefficient by 400 (quarter to year and absolute values to percent).
Results
The 23 participating healthcare centres had a total list comprising 146 454 individuals.
During the observation period, 1 July 1999 to 31 December 2005, a total of 240 447 consultations for an RTI diagnosis were registered corresponding to 257 consultations/1000 inhabitants per 12-month period. The gender distribution was 43% males and 57% females and the median age was 27 years.
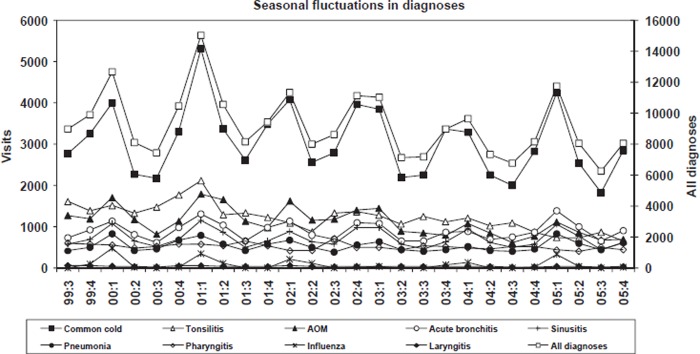
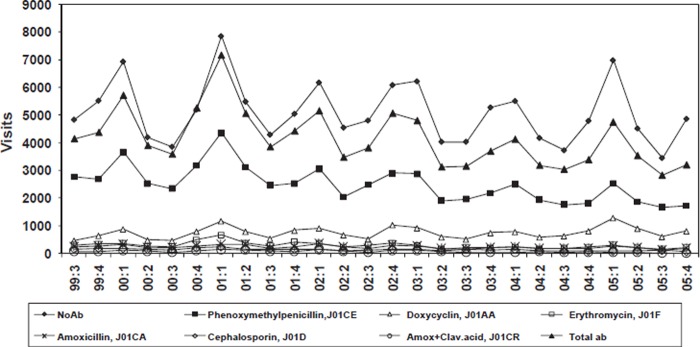
The most common RTI diagnoses are illustrated in Table I. Consultations for acute tonsillitis, AOM, pharyngitis, and laryngitis decreased significantly (p = 0.008). There were large seasonal fluctuations of consultations with peaks during the periods December to May (Figure 1). Similar fluctuations were observed for the prescribing of antibiotics (Figure 2). The proportion of patients receiving an antibiotic prescription related to number of visits was almost constant over the quartiles (44–46%). The proportion of consultations for an URTI that resulted in an antibiotic prescription was 50% in 2000 and 42% in 2005 and for a LRTI 55% in 2000 and 57% in 2005.
Table I.
Number of physician consultations for the most common diagnoses during the studied six complete infectious seasons between January 2000 and December 2005.
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | Total | %▵/yr | r | p-value | |
| Common cold | 11 813 | 14 816 | 13 448 | 11 695 | 10 418 | 11 525 | 73 715 | −3.7% | −0.26 | 0.192 |
| Tonsillitis | 6144 | 6018 | 4698 | 4751 | 4255 | 3044 | 28 910 | −11.7% | −0.81 | 0.000 |
| AOM | 4962 | 5673 | 5480 | 4076 | 3422 | 3464 | 27 077 | −10.0% | −0.65 | 0.000 |
| Acute bronchitis | 3605 | 4073 | 3788 | 3350 | 3289 | 4055 | 22 160 | −0.6% | −0.05 | 0.801 |
| Sinusitis | 3069 | 3299 | 3195 | 2774 | 2788 | 3048 | 18 173 | −2.5% | −0.17 | 0.405 |
| Pneumonia | 2486 | 2461 | 2198 | 2007 | 1944 | 2629 | 13 725 | −1.1% | −0.09 | 0.653 |
| Pharyngitis | 2181 | 2335 | 2080 | 2034 | 2033 | 1831 | 12 494 | −3.5% | −0.51 | 0.007 |
| Influenza | 543 | 493 | 363 | 152 | 159 | 402 | 2112 | −14.5% | −0.20 | 0.337 |
| Laryngitis | 189 | 201 | 195 | 198 | 146 | 171 | 1100 | −6.4% | −0.51 | 0.008 |
| Others | 3683 | 3853 | 3723 | 3333 | 3515 | 3981 | 22 088 | – | ||
| Total | 38675 | 43222 | 39168 | 34370 | 31969 | 34150 | 221554 |
Notes: Correlations shown in bold are significant at p = 0.05. %Δ/yr = relative yearly change (%) during the observation period 1999–2005. r is the correlation coefficient.
Figure 1.
Trends from July 1999 to December 2005 of number of physician visits calculated for the most common respiratory tract infections from July 1999 to December 2005. Note: The sum of all diagnoses is shown on the right-hand scale, individual diagnoses on the left.
Figure 2.
Trends from July 1999 to December 2005 of number of physician visits calculated for the most commonly used antibiotics from July 1999 to December 2005. Note: No antibiotics represents consultations where no antibiotic was prescribed.
A total of 107 990 antibiotic prescriptions were registered (Table II). Antibiotics were prescribed most frequently to patients aged 18–44. Phenoxymethylpenicillin (PcV) was the most prescribed antibiotic and accounted for 60% of all antibiotics prescriptions.
Table II.
Relative antibiotic prescription pattern calculated for each age group, including consultations where an antibiotic was not prescribed (no antibiotics).
| Age 0–6 | Age 7–17 | Age 18–44 | Age 45–64 | Age 65–74 | Age >74 | Total (%) | Total (abs) | |
| No antibiotics | 59% | 54% | 52% | 54% | 55% | 59% | 55% | 132457 |
| Phenoxymethylpenicillin (J01CE) | 29% | 35% | 30% | 20% | 16% | 14% | 27% | 64864 |
| Doxycycline (J01AA) | 0% | 1% | 8% | 17% | 21% | 19% | 8% | 19556 |
| Erythromycin (J01F) | 3% | 4% | 4% | 3% | 2% | 1% | 3% | 7763 |
| Amoxicillin (J01CA) | 4% | 2% | 2% | 3% | 3% | 3% | 3% | 6475 |
| Cephalosporin (J01D) | 1% | 2% | 2% | 1% | 1% | 2% | 2% | 3633 |
| Amoxicillin and clavulanic acid (J01CR) | 2% | 1% | 0% | 0% | 0% | 0% | 1% | 2053 |
| Others | 1% | 2% | 1% | 1% | 2% | 2% | 2% | 3646 |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | |
| Visits total (abs) | 54804 | 42575 | 69163 | 43496 | 14504 | 15905 | 240447 | |
| Antibiotics total (abs) | 22655 | 19538 | 33002 | 19791 | 6528 | 6476 | 107990 |
Note: (abs) = absolute values.
The percentage of PcV was higher in the age groups 0–6 (69%), 7–17 (77%), and 18–44 (65%) and lower in the age groups 45–64 (43%), 65–74 (35%), and ≥ 75 (34%) (see Table II). Doxycycline was the second most prescribed antibiotic with 19 556 prescriptions (18%). The percentage of prescriptions increased after 45 years of age and doxycycline dominated all antibiotic prescriptions after age 65. Amoxicillin or amoxicillin combined with clavulanic acid were most often used in the age group 0–6 (4% and 2%, respectively). Erythromycin (90% of all macrolides) and cephalosporins were prescribed less frequently for all age groups (see Table II).
During the study period, the use of all antibiotic classes except doxycycline decreased significantly particularly in patients under 44 (Table III, and see Figure 2).
Table III.
Changes over time in number of prescriptions of antibiotics in the various age groups.
| Age 0–6 |
Age 7–17 |
Age 18–44 |
Age 45–64 |
Age 65–74 |
Age >74 |
|||||||||||||
| Treatment | %Δ/yr | r | p | %Δ/yr | r | p | %Δ/yr | r | p | %Δ/yr | r | p | %Δ/yr | r | p | %Δ/yr | r | p |
| No antibiotics | −4.5 | −0.27 | 0.181 | −7.8 | −0.51 | 0.008 | −3.6 | −0.40 | 0.043 | 1.4 | 0.12 | 0.547 | 2.4 | 0.19 | 0.364 | 2.9 | 0.22 | 0.271 |
| Phenoxymethylpenicillin | −9.4 | −0.53 | 0.005 | − 12.6 | −0.75 | 0.000 | −8.8 | −0.77 | 0.000 | −4.7 | −0.46 | 0.019 | −4.1 | −0.30 | 0.134 | −1.9 | −0.15 | 0.477 |
| Doxycycline | − | − | − | 6.8 | 0.21 | 0.305 | 2.1 | 0.13 | 0.538 | 4.5 | 0.27 | 0.181 | 4.1 | 0.28 | 0.162 | 4.7 | 0.32 | 0.112 |
| Erythromycin | −12.5 | −0.47 | 0.016 | −12.0 | −0.48 | 0.013 | −11.6 | −0.72 | 0.000 | −6.2 | −0.44 | 0.025 | −0.4 | −0.02 | 0.929 | −7.4 | −0.33 | 0.100 |
| Amoxicillin | −10.7 | −0.47 | 0.015 | −14.5 | −0.70 | 0.000 | −8.0 | −0.51 | 0.007 | 1.4 | 0.16 | 0.429 | 1.5 | 0.08 | 0.686 | −0.4 | −0.02 | 0.925 |
| Cephalosporin | −22.5 | −0.79 | 0.000 | −11.7 | −0.66 | 0.000 | −15.2 | −0.80 | 0.000 | −6.6 | −0.48 | 0.013 | 5.6 | 0.18 | 0.369 | −0.4 | −0.02 | 0.922 |
| Amox + Clavul.acid | −19.2 | −0.64 | 0.000 | −13.4 | −0.53 | 0.006 | −10.9 | −0.41 | 0.039 | 5.3 | 0.13 | 0.526 | 2.2 | 0.07 | 0.757 | 5.6 | 0.21 | 0.398 |
Note: “No antibiotics” represents consultations where an antibiotic was not prescribed. Correlations shown in bold are significant at p = 0.05.%Δ/yr = Relative yearly change (%) during the observation period 1999–2005. r is the correlation coefficient. All the statistically significant trends are de facto decreasing (negative%Δ/yr values (slopes)). Doxycycline is not used in age group 0–6.
Discussion
Summary of main findings
The overall consultation rate and diagnoses of acute tonsillitis, AOM, pharyngitis, and laryngitis decreased significantly but remained unchanged for common cold, acute sinusitis, pneumonia, acute bronchitis, and influenza between 1999 and 2005.
The average number of consultations for an RTI per 1000 inhabitants was 257 and 45% of patients received an antibiotic prescription. PcV accounted for 60% of all prescribed antibiotics followed by doxycycline (18%). Antibiotic prescriptions for patients below age 45 decreased significantly for all antibiotic classes except tetracycline.
Strengths and limitations
The EPR system is well implemented in the daily routines and registration of the diagnosis (KSH 97Pcode [16]) and prescriptions is mandatory. EPRs have been suitable for describing consultation rates, diagnoses, and antibiotic prescribing in primary care [18], [19]. There are some limitations using retrospective data from EPRs. Control visits cannot be distinguished from acute visits which may overestimate the number of cases of acute otitis media and pneumonia. In addition, the criteria for diagnostic labelling used by different physicians have been shown to be variable and antibiotic treatment may also influence the choice of diagnosis.
The strength of this study was in following an entire population for six years, including all consultations for RTI (n = 240 447). The included population in Kalmar County did not change significantly from 1999 to 2005 for gender, age distribution, or size (235 391 → 233 944). The list sizes of analysed units remained constant, with only small fluctuations. We chose to present estimations based on single diagnoses. The remaining 10% of unusual diagnoses/diagnosis combinations and 3.6% of unusual antibiotics/antibiotic combinations, which statistically only slightly influenced the prescription and diagnosis changes over time, are presented in Table I and II as “others”.
Comparisons with similar studies
Our study showed that consultations for RTI decreased by 23% between 1999/2000 and 2004/2005. This finding was in accordance with studies from England [20–22], the USA [23], and the Netherlands [3], [24]. However, these studies reported data prior to 2001 while we found no studies reporting data after 2001.
The number of consultations for RTI per 1000 inhabitants and year averaged 257 in our study, nearly identical to the findings of 273 for the year 2000 in an English study [22]. There, the proportion of consultations for RTI prescribing an antibiotic was 67%, which is in contrast to an average of 45% in our study. Analysing our data from 2005, antibiotics were prescribed to 42% of upper RTIs and 57% of lower RTIs, in comparison with approximately 65% of upper RTIs and 85% of lower RTIs in the study by Ashworth in 2000 [22]. Thus, it appears as if both populations have similar consulting behaviour, but the GPs have different prescribing habits.
The total antibiotic use in outpatient care in Sweden, measured by defined daily doses, was 13.3/1000 inhabitants and day in 2002 and 13.1 in Kalmar County, and by number of prescriptions/1000 inhabitants per year 473 in 2000, and 426 in 2005 in Sweden, and 440 and 406, respectively, in Kalmar County. We consider our results to be representative of Sweden due to the size of our study population and the similarity regarding antibiotic use between Sweden and Kalmar County. In addition, the pattern of results was similar to results from Östergötland County [18] where antibiotics were prescribed in 47% of all cases of which 61% received PcV and 18% doxycycline. Decreasing consultation trends and prescribing antibiotics have also been reported in three Swedish diagnosis and prescription surveys. In these studies 56 (2000), 54 (2002), and 49% (2005) of patients consulting GPs for RTI obtained a prescription for antibiotics [13], [25], [26].
Common cold was the most common diagnosis for all years (see Table I, Figure 1). The decrease in yearly consultation rates was most evident for acute tonsillitis and AOM. This decline was probably due to the new guidelines for AOM in 2000 [10] and sore throat in 2001 [11]. In the new guidelines for AOM, it was possible to refrain from antibiotic treatment during the first three symptomatic days in children > 2 years of age. However, the new guidelines do not appear to have been implemented in the year 2000 in Kalmar County, since a decline in frequency was first noted only for the season 2003–2004 (see Table I). Instead, the decline coincided with a randomized study on AOM in the county [27] including information to all GPs and the media.
The decrease in frequency of acute tonsillitis, however, coincided with the introduction of the new guidelines for the treatment of sore throat, in Sweden equivalent to the diagnoses acute tonsillitis and acute pharyngitis in ICD 10P [11].
In this guideline, it was stressed that patients with any other viral symptoms should be diagnosed as viral infections, i.e. common cold or pharyngitis. Antibiotics should only be considered for patients with > 2 Centor criteria [28] and a rapid test indicating presence of Group A streptococci.
PcV is the drug of choice in Sweden in most RTIs and our study confirmed a high use of PcV especially for younger patients. In most other countries, amoxicillin or amoxicillin in combination with clavulanic acid and macrolides form the first-line antibiotics for RTIs, although dosage and treatment length may vary substantially [29], [30]. The observed high use of tetracycline is not supported by Swedish guidelines, but has been noted in prior studies [8], [18], [26], [31].
Low seasonal variation in antibiotic use is regarded as a quality indicator of rational antibiotic use [32]. The high seasonal variation in antibiotic prescribing in our study indicates that antibiotics are still used more than necessary for RTIs. A national study on weekly antibiotic use and incidence of influenza between 1998 and 2002 indicated similar seasonal variations in antibiotic use and a coincidental relationship between the peaks of diagnosed influenza and antibiotic utilization in 2003 [31]. In our study, diagnosed influenza cases were few but could, of course, have caused some bacterial complications in the lower respiratory tract.
Conclusions
In this six-year, population-based study, antibiotic prescriptions for RTIs decreased, as did consultation rates. The large seasonal variation indicates further possibilities to decrease antibiotic prescription. Knowledge of indications for antibiotics and changes over time is a prerequisite for interventions targeting the expectations of the population and prescribing habits of physicians.
Acknowledgements
There were no conflicts of interest.
References
- 1.Grimsmo A, Hagman E, Faiko E, Matthiessen L, Njalsson T. Patients, diagnoses and processes in general practice in the Nordic countries: An attempt to make data from computerised medical records available for comparable statistics. Scand J Prim Health Care. 2001;19:76–82. doi: 10.1080/028134301750235277. [DOI] [PubMed] [Google Scholar]
- 2.Van der Linden MW WG, de Bakker DH, et al. Second Dutch National Survey of General Practice [Tweede Nationale Studie naar ziekten en verrichtingen in de huisartspraktijk: klachten en aandoeningen in de bevolking en in de huisartspraktijk] Utrecht, Bilthoven: NIVEL, Rijksinstituut voor Volksgezondheid en Milieu; 2004. [Google Scholar]
- 3.Kuyvenhoven MM, van Balen FAM, Verheij TJM. Outpatient antibiotic prescriptions from 1992 to 2001 in the Netherlands. J Antimicrob Chemother. 2003;52:675–8. doi: 10.1093/jac/dkg412. [DOI] [PubMed] [Google Scholar]
- 4.Sampers GH, Sturm AW. Antimicrobial agents in primary health care: study of all family physicians in a medium-sized city] Nederlands Tijdschrift voor Geneeskunde. 1988;132:676–80. [PubMed] [Google Scholar]
- 5.Arroll B, Kenealy T. Antibiotics for the common cold and acute purulent rhinitis [update of Cochrane Database Syst Rev;(3):CD000247; PMID: 12137610] Cochrane Database Syst Rev. 2002;2005((3)):CD000247. doi: 10.1002/14651858.CD000247.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Ekdahl K, Hansson HB, Molstad S, Soderstrom M, Walder M, Persson K. Limiting the spread of penicillin-resistant Streptococcus pneumoniae: Experiences from the South Swedish Pneumococcal Intervention Project. Microbial Drug Resistance-Mechanisms Epidemiology & Disease. 1998;4:99–105. doi: 10.1089/mdr.1998.4.99. [DOI] [PubMed] [Google Scholar]
- 7.Olsson-Liljequist B, Kahlmeter G. Antibiotic resistance: A real threat in Sweden too. Lakartidningen. 1997;94:115–17. [PubMed] [Google Scholar]
- 8.Andre M, Eriksson M, Molstad S, Stalsbylundborg C, Jacobsson A, Odenholt I, et al. The management of infections in children in general practice in Sweden: A repeated 1-week diagnosis-prescribing study in 5 counties in 2000 and 2002. Scand J Infect Dis. 2005;37:863–9. doi: 10.1080/00365540500335207. [DOI] [PubMed] [Google Scholar]
- 9.Molstad S, Erntell M, Hanberger H, Melander E, Norman C, Skoog G, et al. Sustained reduction of antibiotic use and low bacterial resistance: 10-year follow-up of the Swedish Strama programme. Lancet Infect Dis. 2008;8:125–32. doi: 10.1016/S1473-3099(08)70017-3. [DOI] [PubMed] [Google Scholar]
- 10.Consensus Development Statement S. Treatment of Acute Inflammation of the Middle Ear 2000. 10–12 May. [Google Scholar]
- 11.Medical ProductAgency. Handläggning av faryngotonsilliter-Recommendations (Management of pharyngotonsillitis: Recommendations) Info från Läkemedelsverket. 2001;12:44–75. [Google Scholar]
- 12.Medical ProductAgency. Läkemedelsbehandling av rinosinuit–Behandlingsrekommendation (Pharmacological treatment of rhinosinusitis: Recommendations) Information from Medical Product Agency. 2005;3:7–13. [Google Scholar]
- 13.Andre M, Vernby A, Odenholt I, Lundborg CS, Axelsson I, Eriksson M, et al. Diagnosis-prescribing surveys in 2000, 2002 and 2005 in Swedish general practice: Consultations, diagnosis, diagnostics and treatment choices. Scand J Infect Dis. 2008;1:1–7. doi: 10.1080/00365540801932439. [DOI] [PubMed] [Google Scholar]
- 14.Official Statistics of Sweden. Statistiska Centralbyrån [Google Scholar]
- 15.World Health Organization. Family of International Classifications Current – June 2004. [Google Scholar]
- 16.Socialstyrelsen. 1997. Classification of diseases and related health problems. Socialstyrelsen Socialstyrelsen (The National Board of Health and Welfare); [Google Scholar]
- 17.WHO. Guidelines for ATC classification and DDD assignment. 2003. The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD ATC Index with DDDs 2003) [Google Scholar]
- 18.Engstrom S, Molstad S, Nilsson G, Lindstrom K, Borgquist L. Data from electronic patient records are suitable for surveillance of antibiotic prescriptions for respiratory tract infections in primary health care. Scand J Infect Dis. 2004;36:139–43. doi: 10.1080/00365540410019011. [DOI] [PubMed] [Google Scholar]
- 19.Engstrom S, Molstad S, Lindstrom K, Nilsson G, Borgquist L. Excessive use of rapid tests in respiratory tract infections in Swedish primary health care. Scand J Infect Dis. 2004;36:213–18. doi: 10.1080/00365540310018842. [DOI] [PubMed] [Google Scholar]
- 20.Frischer M, Heatlie H, Norwood J, Bashford J, Millson D, Chapman S. Trends in antibiotic prescribing and associated indications in primary care from 1993 to 1997 [see comment] J Public Health Med. 2001;23:69–73. doi: 10.1093/pubmed/23.1.69. [DOI] [PubMed] [Google Scholar]
- 21.Ashworth M, Charlton J, Latinovic R, Gulliford M. Age-related changes in consultations and antibiotic prescribing for acute respiratory infections, –2000. Data from the UK General Practice Research Database. J Clin Pharm Therapeut;31. 1995;2006:461–7. doi: 10.1111/j.1365-2710.2006.00765.x. [DOI] [PubMed] [Google Scholar]
- 22.Ashworth M, Latinovic R, Charlton J, Cox K, Rowlands G, Gulliford M. Why has antibiotic prescribing for respiratory illness declined in primary care? A longitudinal study using the General Practice Research Database [see comment] J Public Health. 2004;26:268–74. doi: 10.1093/pubmed/fdh160. [DOI] [PubMed] [Google Scholar]
- 23.McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents [see comment] JAMA. 2002;287:3096–102. doi: 10.1001/jama.287.23.3096. [DOI] [PubMed] [Google Scholar]
- 24.Kuyvenhoven M, van Essen G, Schellevis F, Verheij T. Management of upper respiratory tract infections in Dutch general practice: Antibiotic prescribing rates and incidences in 1987 and 2001. Fam Pract. 2006;23:175–9. doi: 10.1093/fampra/cmi122. [DOI] [PubMed] [Google Scholar]
- 25.Andre M, Odenholt I, Schwan A, Axelsson I, Eriksson M, Hoffman M, et al. Upper respiratory tract infections in general practice: Diagnosis, antibiotic prescribing, duration of symptoms and use of diagnostic tests. Scand J Infect Dis. 2002;34:880–6. doi: 10.1080/0036554021000026952. [DOI] [PubMed] [Google Scholar]
- 26.Lundborg CS. Olsson E. Molstad S Swedish Study Group on Antibiotic U. Antibiotic prescribing in outpatients: A 1-week diagnosis-prescribing study in 5 counties in Sweden. Scand J Infect Dis. 2002;34:442–8. doi: 10.1080/00365540110080647. [DOI] [PubMed] [Google Scholar]
- 27.Neumark T. Mölstad S Rosén. Persson L-G. Törngren A. Brudin L, et al. Evaluation of phenoxymethylpenicillin treatment of acute otitis media in children aged 2–16. Scand J Prim Health Care. 2007;25:166–71. doi: 10.1080/02813430701267405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE. Empirical validation of guidelines for the management of pharyngitis in children and adults [see comment] [erratum appears in JAMA 2005;294:2700] JAMA. 2004;291:1587–95. doi: 10.1001/jama.291.13.1587. [DOI] [PubMed] [Google Scholar]
- 29.Rautakorpi UM, Lumio J, Huovinen P, Klaukka T. Indication-based use of antimicrobials in Finnish primary health care: Description of a method for data collection and results of its application. Scand J Prim Health Care. 1999;17:93–9. doi: 10.1080/028134399750002719. [DOI] [PubMed] [Google Scholar]
- 30.Coenen S, Molstad S. Preferred antibiotics, dosages and length of treatments in general practice: A comparison between ten European countries. Eur J Gen Pract. 2004;10:166–8. doi: 10.3109/13814780409044306. [DOI] [PubMed] [Google Scholar]
- 31.Ganestam F, Lundborg CS, Grabowska K, Cars O, Linde A. Weekly antibiotic prescribing and influenza activity in Sweden: A study throughout five influenza seasons. Scand J Infect Dis. 2003;35:836–42. doi: 10.1080/00365540310016880. [DOI] [PubMed] [Google Scholar]
- 32.Coenen S, Ferech M, Haaijer-Ruskamp FM, Butler CC, Vander Stichele RH, Verheij TJM, et al. European Surveillance of Antimicrobial Consumption (ESAC): Quality indicators for outpatient antibiotic use in Europe. Quality & Safety in Health Care. 2007;16:440–5. doi: 10.1136/qshc.2006.021121. [DOI] [PMC free article] [PubMed] [Google Scholar]