Abstract
The introduction of laparoscopy to gynecologic surgery has allowed for both innovative advancements and new challenges in the field. As the complexity of laparoscopically approached gynecologic cases continues to increase, it is imperative for surgeons to be aware of the risk of ureteral injury. Although rare, ureteral complications with gynecologic surgery may be quite morbid; therefore, knowledge about their prevention, diagnosis, and management is of the utmost importance.
Key words: Ureteral injury, Laparoscopy, Hysterectomy, Intraoperative cystoscopy
The introduction of laparoscopy to gynecologic surgery has allowed for both innovative advancements and new challenges in the field. As more advanced pathology is approached via laparoscopic means, there is increasing emphasis on potential complications such as ureteral injuries. Engel and colleagues1 reported the first case of ureteral injury during a laparoscopic tubal ligation in 1971, after which the patient presented with postoperative flank pain and was diagnosed with right ureteral obstruction that necessitated ureteroneocystostomy and Boari flap repair. Since that time, much research has been devoted to prevention and management of ureteral injury during gynecologic surgery.
With regard to incidence of ureteral injury at the time of operative gynecologic laparoscopy, several large cohort studies have been performed that estimate incidence of ureteral injury during a variety of procedures at < 2%.2–4 A 2003 review of all published cases of ureteral injuries in gynecologic laparoscopy identified 70 reported cases.5 We estimate the incidence of ureteral injury (including transection, obstruction, fistula formation, and necrosis from thermal injury) during gynecologic laparoscopy as ranging from < 1% to 2%. More useful, perhaps, is to examine incidence of ureteral injury during specific cases. In 2005, Vakili and colleagues6 performed a prospective, multicenter study examining ureteral injury at the time of hysterectomy based on universal cystoscopy; ureteral injury was reported in 1.7% of cases with no differences found in incidence of ureteral injury among abdominal hysterectomy, vaginal hysterectomy, or laparoscopic hysterectomy. However, other studies have noted a higher risk of ureteral injury with a laparoscopic approach to hysterectomy when compared with an abdominal or vaginal approach.7–9 Although rare, ureteral complications of gynecologic surgery may be quite morbid; therefore, knowledge about their prevention, diagnosis, and management is of the utmost importance.
Preoperative Risk Stratification
Preoperative evaluation is useful in identifying patients who are at higher risk of ureteral injury, although it has been reported that half of all patients with ureteral injuries have no risk factors.10 Patients undergoing gynecologic surgery for malignancy may have a higher baseline risk of ureteral injury—as high as 5% to 8%.11 Other potential risk factors include sources of anatomic distortion such as previous pelvic surgery, endometriosis, pelvic adhesions, enlarged uteri, adnexal masses, cervical and broad ligament fibroids, as well as congenital anomalies. It has also been suggested that intraoperative hemorrhage is associated with ureteral injury when the visualization of the operative field is obscured.10
In cases where there is a high clinical index of suspicion of ureteral anatomic distortion, preoperative imaging of the genitourinary tract is recommended. Some experts have also suggested the prophylactic placement of ureteral stents in select cases to aid in intraoperative ureteral identification. Retrospective reviews have documented the ease and safety of prophylactic ureteral catheterization, although it may be associated with discomfort, irritated bladder symptoms, fever, and flank pain in rare instances.12–14 Results from one large randomized trial15 and a retrospective analysis16 have not documented any difference in ureteral injury rates during major gynecologic surgery with the use of prophylactic stenting. However, according to a decision analysis performed for abdominal hysterectomy cases,17 prophylactic stent placement may be cost saving in benign or radical hysterectomy, in which the injury rate is > 3.2%. As such, we recommend this in select cases as deemed appropriate by clinical judgment, taking into account surgeon experience and clinical characteristics such as prior radiation or known distorted anatomy. It is important to note that, during laparoscopic procedures, the ability to palpate ureteral stents in order to confirm location is diminished, thereby decreasing their utility. Lighted ureteral stents have been proposed as a novel method to ensure location of the ureters throughout a procedure without relying on haptic feedback.12,18
Anatomic Principles and Dissection Tips
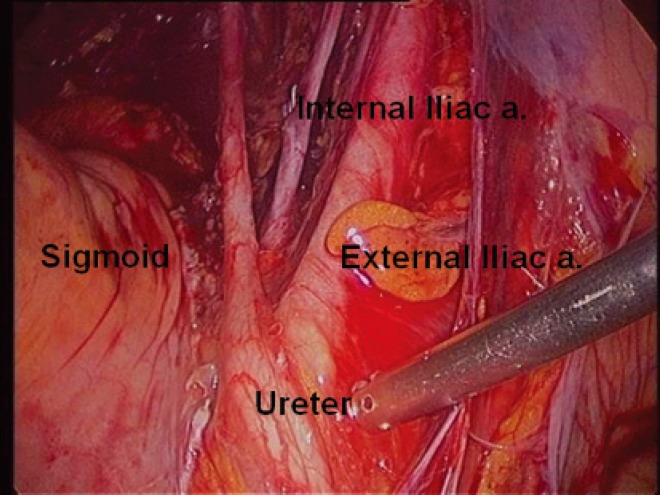
Meticulous surgical technique and attention to pelvic anatomy is paramount to the effort of decreasing ureteral injury. The ureter is divided anatomically into two major components—abdominal and pelvic—with lengths ranging from 12 to 15 cm each. The ureter descends over the pelvic brim as it courses over the iliac vessels at the bifurcation of the common iliac artery into the external and internal iliac arteries (Figure 1). Deep in the pelvis, the ureter courses along the lateral aspect of the uterosacral ligament to enter the base of the broad ligament. The ureter is found < 1.5 cm lateral to the cervix, passing under the uterine artery and then medially over the anterior vaginal fornix before entering the trigone of the bladder.14 Radiologic studies have revealed that, in 10% of cases involving cervical pathology, the ureter may be only 5 mm from the cervix.19
Figure 1.
The ureter descends over the pelvic brim as it courses over the iliac vessels at the bifurcation of the common iliac artery into the external and internal iliac arteries.
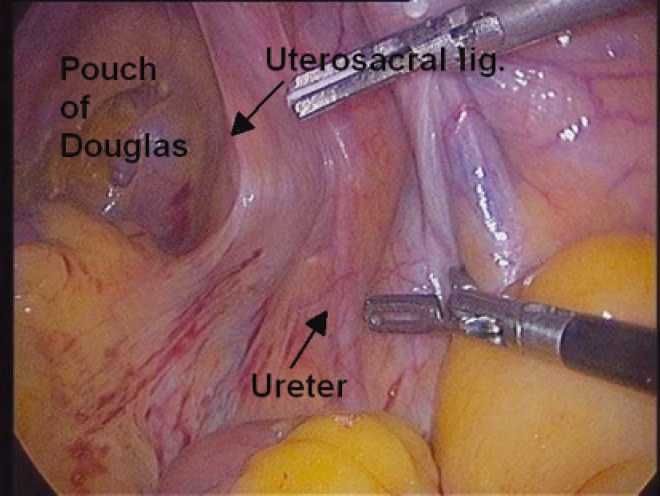
The most common locations of ureteral injury in pelvic surgery are at the cardinal ligament, where the ureter passes inferior to the uterine vessels, as well as the level of the infundibulopelvic (IP) ligament. The ureter can also be injured along the lateral border of the uterosacral ligament or along its course near the anterior vaginal wall. It has been suggested that during laparoscopic surgery specifically, the ureter is at greatest risk of injury at the IP ligament, in the ovarian fossa, and in the ureteric canal.20 A systematic Delphi procedure for the prevention of urinary tract injuries suggested that all surgeons visualize and dissect the ureter near the IP ligament and near the uterine artery in cases of distorted anatomy.21
In cases of laparoscopic adnexectomy, the ureter can be identified transperitoneally as it courses over the pelvic brim (Figure 2). The left ureter is often more challenging to view by this approach due to physiologic adhesions of the descending colon to the pelvic sidewall. This visualization may also be limited by the rectosigmoid colon or in cases involving inflammation, adhesions, and endometriosis. If the ureter is not clearly visualized at this level, a superficial incision in the peritoneum (taken parallel to the IP ligament) will allow for the initial development of the pararectal space; subsequent blunt dissection will identify the ureter. The rectosigmoid is then mobilized medially, which will enable a relatively easy identification of the left ureter at the pelvic brim. In severely distorted anatomy, it is best to find the ureter by making a peritoneal incision that begins just medial to the IP ligament and continues in the direction of the ischial spine. This way the ureter is found quicker than if the incision is continued parallel to the suspected course of the ureter. After ensuring that the ureter is sufficiently distant from the IP ligament, the blood supply to the ovary can be controlled. In cases of benign pathology, we recommend incising the vascular pedicle very close to the ovary, as this pedicle will shorten with retraction into the pelvic sidewall; subsequent bleeding can be easier to control with a longer IP pedicle. It is important to note that identification of the ureter at the pelvic brim is not adequate in cases involving significant deep pelvic adhesions, such as in severe endometriosis with rectovaginal involvement. In these cases, the ureters are often deviated more medially and the ureterolysis needs to be carried all the way down to the cardinal ligament.
Figure 2.
In cases of laparoscopic adnexectomy, the ureter can be identified transperitoneally as it courses over the pelvic brim.
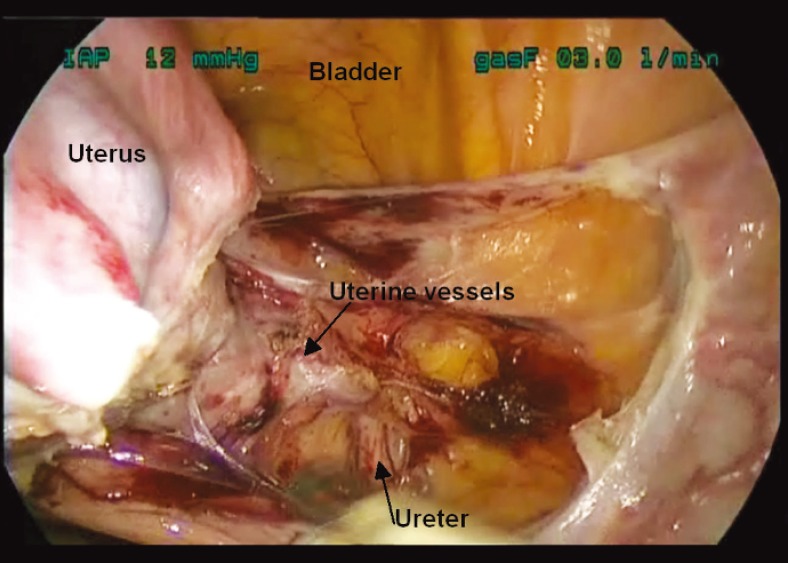
When approaching the cardinal ligament dissection during laparoscopic hysterectomy, a few techniques can help ensure that the ureter is sufficiently lateralized. First, sufficient skeletonization of the uterine vasculature will ensure that any peritoneal attachments involving the ureter are released. Second, it is important to maintain cranial deviation of the uterus with firm upward pressure on the uterine manipulator before cauterizing or incising the uterine vessels. Some surgeons prefer to use upward traction on the uterine specimen with a laparoscopic tenaculum in lieu of a uterine manipulator. Either approach will ensure the distance from the ureter adnexectomy, the ureter can be identified transperitoneally as it courses over the pelvic brim. (Figure 3). We prefer to take the ascending uterine vessels at the level of the internal cervical os when performing a total laparoscopic hysterectomy and then create a pedicle that lateralizes the uterine vessels away from the colpotomy cup. This has proven to be a very effective method to avoid ureteral injury at the time of a laparoscopic hysterectomy.22
Figure 3.
Some surgeons prefer to use upward traction on the uterine specimen with a laparoscopic tenaculum in lieu of a uterine manipulator. Either approach will ensure the distance from the ureter to the ascending uterine artery is increased substantially and the vascular pedicle can be safely controlled. increased substantially and the vascular pedicle can be safely controlled.
Other procedures that necessitate special consideration regarding ureteral location include apical prolapse repairs (laparoscopic sacropexy or uterosacral suspension) and management of severe endometriosis or adhesive disease involving the pelvic sidewall or uterosacral ligaments. It is imperative that the ureter be identified along its entire course in these cases; ureterolysis should be performed as needed to ensure visualization or appropriate distance from the intended operative field.
Intraoperative Ureteral Evaluation
When injury is suspected intraoperatively, approaches to investigate ureteral integrity include the use of intravenous dye injection or retrograde bladder/ureteral dye injection using indigo carmine or methylene blue, in addition to further surgical dissection of the ureter.20 Cystoscopy to assess urine efflux from the ureteral orifices, with or without ureteral catheterization, may also be employed but may not detect partial transection or thermal injury. In certain instances, intraoperative fluoroscopy with urography using a radio-opaque contrast agent may also be useful to characterize ureteral stricture, obstruction, or leak.
Even when a high risk of ureteral injury is not suspected, some advocate the practice of universal cystoscopy during major gynecologic cases to improve injury detection. The results of a systematic review suggest that higher injury detection rates are seen when intraoperative cystoscopy is employed, and it has been suggested that intraoperative markers such as peristalsis and visualization of ureteral caliber may be unreliable to detect injury.6,8 Furthermore, in a prospective clinical study of 839 hysterectomy cases, Ibeanu and associates23 found that universal intraoperative cystoscopy detected 97.4% of ureteral injuries. It is important to note, however, that a negative cystoscopy result does not guarantee lack of ureteral or bladder injury, as there may be partial obstruction or injury with residual patency.24
At the Brigham and Women’s Hospital (Boston, MA), we have undertaken a retrospective study (Sandberg EM, Cohen SL, Hurwitz S, Einarsson JI; article in press) regarding the use of cystoscopy during hysterectomy at our institution. A total of 1982 patients who underwent a hysterectomy of any type during the years 2009 to 2010 were included. Within this hysterectomy cohort, no ureteral injuries were detected intraoperatively whether cysto scopy was performed or not. Five patients were subsequently diagnosed with ureteral injury postoperatively (0.25% of cases); all five cases of ureteral injury were associated with laparoscopic or robotic hysterectomy and none underwent cystoscopy at the time of surgery. Risk factors for ureteral injury that were identified in this study include adhesive disease, prior surgery, oncology cases, and low operator case volume. Due to low absolute risk of complications, we recommend selective rather than universal cystoscopy during hysterectomy. However, the threshold to perform a cystoscopy should be low, and in cases involving low-volume surgeons and/or significant pelvic pathology, cystoscopy should be performed routinely. We also strongly recommend that all gynecologic surgeons who perform advanced pelvic surgery be trained in and have privileges for performing diagnostic cystoscopy.
Postoperative Ureteral Evaluation
Patients with ureteral injury may develop postoperative vaginal drainage, fevers, flank pain, rising creatinine levels, or frank peritonitis. In addition to physical examination and laboratory investigations, imaging studies can detect ascites, hydronephrosis, or ureteral obstruction/leakage. Recommended imaging modalities include renal ultrasound, computed tomography urogram with intravenous contrast (if patient has normal renal function), and/or retrograde pyelogram. Renal scans can be particularly useful in detecting obstruction and/or urinary leak. The use of color Doppler ultrasonography for ureteral jets has also been investigated as a mode of ureteral assessment.25
Regarding the timing of ureteral injury detection, Wu and colleagues26 described their series of over 4950 laparoscopic hysterectomies and reported that early injury detection, by either intraoperative cystoscopy or postoperative jet ultrasonography, conferred a better prognosis. Thermal injury led to delayed necrosis and partial obstruction of the ureteral wall that was not initially detected with immediate intraoperative cystoscopy or early postoperative jet ultrasonography; these patients presented 10 to 14 days postoperatively.
Management of Ureteral Injury
Urologic consultation is recommended for management of ureteral injuries. Treatment may range from a conservative approach with stent placement to a more extensive repair with re-anastomosis or re-implantation of the ureter to the bladder.27 Factors that impact the mode of management include timing of injury recognition and mechanism of injury. For example, an injury that is recognized intraoperatively is more likely to be treated with immediate repair. For postoperatively recognized ureteral injuries, particularly if there is tissue edema and inflammation or poor general condition of the patient, it is advised to postpone surgical treatment 6 weeks or longer with the intervention of percutaneous nephrostomy tubes during the interval to allow the patient’s general health and tissue quality to improve. Regarding mechanism of injury, a partial ureteral ligation can often be managed with temporary placement of a ureteral stent. A complete ureteral ligation, crush injury or thermal injury, however, typically requires resection of the involved segment. In cases of ureteral transection, interval percutaneous nephrostomy tube placement with drainage of ascites is employed; the patient then undergoes delayed repair of the transected segment of the ureter.
The location of an injury also impacts the decision regarding the mode of repair. A ureteroureterostomy is typically the preferred method to repair injuries to the upper third of the ureter. The middle third of the ureter is often repaired with ureteroureterostomy with tensionfree anastomosis, or with a Boari flap if anastomosis cannot be repaired without tension. The pelvic ureter can be repaired via ureteroneocystostomy with the addition of a psoas hitch to add length to the ureter. Transureteroureterostomy is rarely performed due to concerns about putting both ureters—and therefore both kidneys—at risk; however, it is occasionally necessary. Construction of an ilial ureter, wherein a piece of small bowel is used to bridge a ureteral defect, is typically reserved for cases that fail a prior surgical procedure. Finally, a nephrectomy is sometimes necessary if a repair cannot safely be performed or the kidney has marginal function.
In addition to a traditional open approach to ureteral repair, laparoscopic repair is a safe and effective option for the patient. In 1991, Gomel and James28 published the first case of ureteral injury repaired laparoscopically, and in 1992 Nezhat and Nezhat29 followed with a report on a laparoscopic ureteral injury and subsequent repair during an operation for excision of endometriosis. In appropriate hands, laparoscopic ureteral repair can be undertaken in a manner consistent with the principles of open repair without the morbidity of laparotomy.30
Conclusions
As the complexity of gynecologic cases approached laparoscopically continues to increase, it is imperative that surgeons be aware of the risk of ureteral injury. Patients should be appropriately counseled preoperatively regarding baseline and individualized risks. Although the overall incidence of ureteral injury is low in gynecologic laparoscopy, the potential morbidity for the patient merits vigilance. Prevention of injury can be achieved by careful attention to the location of the ureter at all times during the procedure.31 To this end, a solid foundation in pelvic anatomy will be an asset in surgeries where there is a distortion of the anatomy. Prophylactic ureteral stenting may be helpful in select circumstances, and intra- or postoperative evaluation should be undertaken whenever suspicion arises of potential ureteral damage. Knowledge of ureteral anatomy and familiarity with avenues for assessment throughout the operative process can empower a surgeon to prevent or reduce potential ureteral complications.
Main Points.
Although rare, ureteral complications with gynecologic surgery may be quite morbid; therefore, knowledge about their prevention, diagnosis, and management is of the utmost importance.
Preoperative evaluation is useful in identifying patients who are at higher risk of ureteral injury. Potential risk factors include sources of anatomic distortion such as previous pelvic surgery, endometriosis, pelvic adhesions, enlarged uteri, adnexal masses, cervical and broad ligament fibroids, and congenital anomalies.
Meticulous surgical technique and attention to pelvic anatomy is paramount to the effort of decreasing ureteral injury. The most common locations of ureteral injury in pelvic surgery are at the cardinal ligament, where the ureter passes inferior to the uterine vessels, as well as the level of the infundibulopelvic (IP) ligament. It has been suggested that during laparoscopic surgery specifically, the ureter is at greatest risk of injury at the IP ligament, in the ovarian fossa, and in the ureteric canal.
When injury is suspected intraoperatively, approaches to investigate ureteral integrity include the use of intravenous dye injection or retrograde bladder/ureteral dye injection using indigo carmine or methylene blue, in addition to further surgical dissection of the ureter. Gynecologic surgeons who perform advanced pelvic surgery should also be trained in diagnostic cystoscopy.
References
- 1.Engel T, Reid RA, Thompson HE. Laparoscopy in gynecology. Rocky Mt Med J. 1971;68:11–16. [PubMed] [Google Scholar]
- 2.Tamussino KF, Lang PF, Breinl E. Ureteral complications with operative gynecologic laparoscopy. Am J Obstet Gynecol. 1998;178:967–970. doi: 10.1016/s0002-9378(98)70532-0. [DOI] [PubMed] [Google Scholar]
- 3.Saidi MH, Sadler RK, Vancaillie TG, et al. Diagnosis and management of serious urinary complications after major operative laparoscopy. Obstet Gynecol. 1996;87:272–276. doi: 10.1016/0029-7844(95)00411-4. [DOI] [PubMed] [Google Scholar]
- 4.Gao JS, Leng JH, Liu ZF, et al. Ureteral injury during gynecological laparoscopic surgeries: report of twelve cases. Chin Med Sci J. 2007;22:13–16. [PubMed] [Google Scholar]
- 5.Ostrzenski A, Radolinski B, Ostrzenska KM. A review of laparoscopic ureteral injury in pelvic surgery. Obstet Gynecol Surv. 2003;58:794–799. doi: 10.1097/01.OGX.0000097781.79401.0B. [DOI] [PubMed] [Google Scholar]
- 6.Vakili B, Chesson RR, Kyle BL, et al. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol. 2005;192:1599–1604. doi: 10.1016/j.ajog.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Härkki-Sir’en P, Sjöberg J, Tiitinen A. Urinary tract injuries after hysterectomy. Obstet Gynecol. 1998;92:113–118. doi: 10.1016/s0029-7844(98)00146-x. [DOI] [PubMed] [Google Scholar]
- 8.Gilmour DT, Das S, Flowerdew G. Rates of urinary tract injury from gynecologic surgery and the role of intraoperative cystoscopy. Obstet Gynecol. 2006;107:1366–1372. doi: 10.1097/01.AOG.0000220500.83528.6e. [DOI] [PubMed] [Google Scholar]
- 9.Garry R, Fountain J, Mason S, et al. The eVALuate study: two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ. 2004;328:129. doi: 10.1136/bmj.37984.623889.F6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan JK, Morrow J, Manetta A. Prevention of ureteral injuries in gynecologic surgery. Am J Obstet Gynecol. 2003;188:1273–1277. doi: 10.1067/mob.2003.269. [DOI] [PubMed] [Google Scholar]
- 11.Te Linde RW, Thompson JD, Rock JA. Te Linde’s Operative Gynecology. Philadelphia, PA: Lippincott-Raven; 1997. [Google Scholar]
- 12.Redan JA, McCarus SD. Protect the ureters. JSLS. 2009;13:139–141. [PMC free article] [PubMed] [Google Scholar]
- 13.Tanaka Y, Asada H, Kuji N, Yoshimura Y. Ureteral catheter placement for prevention of ureteral injury during laparoscopic hysterectomy. J Obstet Gynaecol Res. 2008;34:67–72. doi: 10.1111/j.1447-0756.2007.00686.x. [DOI] [PubMed] [Google Scholar]
- 14.Fröber R. Surgical anatomy of the ureter. BJU Int. 2007;100:949–965. doi: 10.1111/j.1464-410X.2007.07207.x. [DOI] [PubMed] [Google Scholar]
- 15.Chou MT, Wang CJ, Lien RC. Prophylactic ureteral catheterization in gynecologic surgery: a 12-year randomized trial in a community hospital. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:689–693. doi: 10.1007/s00192-008-0788-3. [DOI] [PubMed] [Google Scholar]
- 16.Kuno K, Menzin A, Kauder HH, et al. Prophylactic ureteral catheterization in gynecologic surgery. Urology. 1998;52:1004–1008. doi: 10.1016/s0090-4295(98)00382-3. [DOI] [PubMed] [Google Scholar]
- 17.Schimpf MO, Gottenger EE, Wagner JR. Universal ureteral stent placement at hysterectomy to identify ureteral injury: a decision analysis. BJOG. 2008;115:1151–1158. doi: 10.1111/j.1471-0528.2008.01757.x. [DOI] [PubMed] [Google Scholar]
- 18.Pedro RN, Kishore TA, Hinck BD, et al. Comparative analysis of lighted ureteral stents: lumination and tissue effects. J. Endourol. 2008;22:2555–2558. doi: 10.1089/end.2008.0278. [DOI] [PubMed] [Google Scholar]
- 19.Gemer O, Simonocsky A, Huerta M, et al. A radiological study on the anatomical proximity of the ureters and the cervix. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:991–995. doi: 10.1007/s00192-006-0269-5. [DOI] [PubMed] [Google Scholar]
- 20.Hurt WG, Jones CM., III . Intraoperative ureteral injuries and urinary diversion. In: Nichols DH, editor. Gynecologic and Obstetric Surgery. Baltimore, MD: Mosby; 1993. pp. 900–910. [Google Scholar]
- 21.Janssen PF, Brölmann HA, Huirne JA. Recommendations to prevent urinary tract injuries during laparoscopic hysterectomy: a systematic Delphi procedure among experts. J Minim Invasive Gynecol. 2011;18:314–321. doi: 10.1016/j.jmig.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Einarsson JI, Suzuki Y. Total laparoscopic hysterectomy: 10 steps toward a successful procedure. Rev Obstet Gynecol. 2009;2:57–64. [PMC free article] [PubMed] [Google Scholar]
- 23.Ibeanu OA, Chesson RR, Echols KT, et al. Urinary tract injury during hysterectomy based on universal cystoscopy. Obstet Gynecol. 2009;113:6–10. doi: 10.1097/AOG.0b013e31818f6219. [DOI] [PubMed] [Google Scholar]
- 24.Dandolu V, Mathai E, Chatwani A, et al. Accuracy of cystoscopy in the diagnosis of ureteral injury in benign gynecologic surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:427–431. doi: 10.1007/s00192-003-1095-7. [DOI] [PubMed] [Google Scholar]
- 25.Lojindarat S, Suwkrom S, Puangsa-art S. Postoperative color Doppler sonography of the ureteral jets to detect ureteral patency in laparoscopic hysterectomy. J Med Assoc Thai. 2011;94:1169–1174. [PubMed] [Google Scholar]
- 26.Wu HH, Yang PY, Yeh GP, et al. The detection of ureteral injuries after hysterectomy. J Minim Invasive Gynecol. 2006;13:403–408. doi: 10.1016/j.jmig.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 27.Han CM, Tan HH, Kay N, et al. Outcome of laparoscopic repair of ureteral injury: follow-up of twelve cases. J Minim Invasive Gynecol. 2012;19:68–75. doi: 10.1016/j.jmig.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 28.Gomel V, James C. Intraoperative management of ureteral injury during operative laparoscopy. Fertil Steril. 1991;55:416–419. doi: 10.1016/s0015-0282(16)54138-7. [DOI] [PubMed] [Google Scholar]
- 29.Nezhat C, Nezhat F. Laparoscopic repair of the ureter resected during operative laparoscopy. Obstet Gynecol. 1992;80:543–544. [PubMed] [Google Scholar]
- 30.Cholkeri-Singh A, Narepalem N, Miller CE. Laparoscopic ureteral injury and repair: case reviews and clinical update. J Minim Invasive Gynecol. 2007;14:356–361. doi: 10.1016/j.jmig.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 31.Gastillo-Ashby AM, Jelovsek JE, Barber MD, et al. Incidence of ureteral obstruction and the value of intraoperative cystoscopy during vaginal surgery for pelvic organ prolapse. Am J Obstet Gynecol. 2006;194:1478–1485. doi: 10.1016/j.ajog.2006.01.064. [DOI] [PubMed] [Google Scholar]