Abstract
Purpose
The survival of patients with liver metastases from solid tumors is poor. We conducted a phase I study of hepatic arterial infusion (HAI) paclitaxel in patients with advanced cancer and predominant liver involvement.
Methods
Patients were treated with HAI paclitaxel 150–275 mg/m2 (and 15,000 IU heparin intraarterially) every 28 days. A “3 + 3” study design was used.
Results
Twenty-six patients were treated (median age, 59 years). Diagnoses were colorectal cancer (n = 10), breast cancer (n = 7), and other (n = 9). The median number of prior therapies was four (range, 0–10). The maximum tolerated dose (MTD) was HAI paclitaxel 225 mg/m2. Dose-limiting toxicities (DLTs) included Grade 3 neuropathy (1 of 5 patients) at HAI paclitaxel 275 mg/m2 and Grade 4 thrombocytopenia and neutropenia, and Grade 3 mucositis (1 of 4 patients) at 250 mg/m2. None of the eight patients treated with HAI paclitaxel 225 mg/m2 experienced a DLT. The most common toxicities were nausea and peripheral neuropathy. Of 22 patients evaluable for response, 3 (13.6%) patients had SD for ≥4 months (colorectal cancer, n = 1; thyroid cancer, n = 1; and hepatocellular carcinoma, n = 1; duration of response was 4 months, 7.1 months, and 22.2+ months, respectively).
Conclusion
The MTD of HAI paclitaxel was 225 mg/m2. This regimen was well tolerated and had antitumor activity in selected patients.
Keywords: Hepatic arterial infusion, Paclitaxel, Phase I trial
Introduction
Hepatic arterial infusion (HAI) has been used to treat hepatic metastases from all types of cancer (most commonly colorectal) and primary cancers, including hepatocellular carcinoma and biliary tract cancer. The rationale for using HAI is based on the concept that malignant lesions derive most of their blood supply from the hepatic artery, in contrast to normal hepatocytes that are supplied through the portal venous circulation [1]. Cytotoxics administered via the hepatic artery are thought to be extracted during their initial pass through the hepatic parenchyma, thereby maximizing drug concentration in the liver metastases [1].
Liver metastases from solid tumors are associated with a poor prognosis. Overall, 15 to 25% of patients with colorectal cancer present with liver metastases, and another 25 to 50% develop hepatic metastasis following resection of the primary tumor [2–4]. Although resection of liver metastases from colorectal cancer can produce long-term survival in selected patients with solitary liver metastases, the efficacy of liver resection as a solitary treatment is limited by the number of patients with resectable disease, and even after resection, most patients develop recurrent disease in the liver [5].
Paclitaxel is a broadly active, potent cytotoxic agent. It is approved by the Food and Drug Administration for breast cancer, ovarian cancer, lung cancer, and Kaposi’s sarcoma and is routinely used for other cancers, including head and neck, esophageal, gastric endometrial, and bladder cancers; lymphoma; and germ cell tumors. Paclitaxel has been used in regional arterial chemotherapy of various cancers at their primary sites (squamous cell carcinoma of the tongue through external carotid artery infusion [6], non-small-cell lung cancer through the bronchial artery [7], and breast cancer through the internal mammary artery) or at the liver metastases (breast cancer [8–12], gastric cancer [13], small cell lung cancer [14], and colorectal cancer). Furthermore, there is a very high first-phase extraction (95%) of paclitaxel in the liver, which makes it an attractive agent for HAI [14].
Based on the rationale for using HAI chemotherapy versus intravenous (IV) chemotherapy and the antitumor activity of paclitaxel in several tumor types, we conducted a Phase I clinical trial of HAI paclitaxel in patients with advanced cancer and predominant liver metastases. The primary objective was to assess the maximum tolerated dose (MTD) and dose-limiting toxicity (DLT) of HAI paclitaxel, and the secondary objective was to assess the antitumor activity of HAI paclitaxel, if any.
Patients and methods
Eligibility criteria included a histologically confirmed diagnosis of malignancy and liver involvement as the dominant site of metastasis; ECOG performance status ≤ 2; and adequate renal (serum creatinine ≤ 2.0 mg/dL), hepatic (total bilirubin < 2.0 mg/dL or ALT ≤ 5× upper normal reference value), and bone marrow function (ANC ≥ 1.5 cells/μL; PLT ≥ 100,000 cells/μL). Female patients of childbearing potential were eligible if they had a negative urine or human chorionic gonadotropin serum test. Pediatric patients were eligible at the discretion of the primary investigator. Patients were eligible to start therapy if >21 days had elapsed since prior therapy and they had complete recovery (to Grade 1) from all associated toxicities.
Exclusion criteria included clinical or radiographic evidence of ascites, pregnancy, hypersensitivity to paclitaxel or products containing polyoxyethylated castor oil or cremophor, inability to complete an informed consent process and adhere to the protocol treatment plan and follow-up requirements, untreatable bleeding diathesis, portal vein thrombosis, Grade 2 peripheral neuropathy, or untreated brain metastases.
All patients signed informed consent forms fully disclosing the investigational nature of the trial prior to enrollment. The study protocol was approved by The University of Texas MD Anderson Cancer Center Institutional Review Board.
Treatment
Patients were admitted for treatment at MD Anderson Cancer Center. A hepatic intra-arterial catheter was placed by an interventional radiologist using the femoral approach. A 5-French angiographic catheter was utilized to select the celiac and/or superior mesenteric artery and a co-axial 3-French microcatheter was advanced into the desired hepatic artery. Hepatic artery flow evaluation was then performed following the injection of 5 mCi technetium-99 m macroaggregated albumin particles through the HAI catheter used to simulate the distribution of chemotherapeutic agent. The nuclear medicine flow study was also used to identify any evidence of extrahepatic flow to reduce the risk of gastrointestinal complications. The catheter was removed at the end of the paclitaxel infusion.
Patients were treated with HAI paclitaxel ranging from 150 to 275 mg/m2 in 250 mL normal saline with 15,000 IU heparin intraarterially over 24 h on day 1. Cycles were repeated every 4 weeks. The selection of the dose was based on the recommended dose of paclitaxel (125 mg/m2 IV over 3 h every 3 weeks or 135 mg/m2 IV over 24 h every 3 weeks). In addition, other investigators have used HAI paclitaxel at 80 mg/m2 over 1 h every week for 3 weeks per month [9, 11, 13]. In a pilot study at our institution, HAI paclitaxel at 200 mg/m2 over 24 h every 4 weeks was well tolerated and was associated with a PR rate of 30% in patients with metastatic breast cancer [15]. Dose escalation of paclitaxel is shown in Table 1. Patients also received dexamethasone 10 mg IV, diphenhydramine 50 mg IV, and cimetidine 300 mg IV on day 1 prior to chemotherapy.
Table 1.
Dose escalation scheme of paclitaxel
| Dose level | Paclitaxel (mg/m2) |
|---|---|
| 0 | 150 |
| 1 | 175 |
| 2 | 200 |
| 3 | 225* |
| 4 | 250 |
| 5 | 275 |
The defined maximum tolerated dose (MTD)
Dose modification
If Grade 3 treatment-related toxicity occurred, the dose was held until resolution of toxicity to Grade ≤1 and treatment was restarted at the next lower dose. If Grade 3 or 4 toxicity occurred again, the treatment was discontinued.
Patient monitoring
Patients were monitored every 4 weeks by physical examination, complete blood counts and differential, chemistry laboratory studies, vital signs, periodic serial electrocardiograms, chest X-ray, and assessment of adverse events. Liver and renal function tests were conducted every 2 weeks. All patients had initial tumor staging and assessment after completion of every two cycles of therapy.
Endpoints and statistical considerations
The study was designed using a conventional “3 + 3” study design, followed by an expansion phase. Toxicities were assessed using the National Cancer Institute Common Terminology Criteria, version 3.0 [16]. DLTs were assessed during the first cycle and defined as follows: any Grade 4 hematologic toxicity lasting >5 consecutive days or requiring transfusion or growth factor support, Grade 4 nausea/vomiting lasting >5 days, any other Grade 3 non-hematologic toxicity, including symptoms/signs of vascular leakage or cytokine release syndrome, or any severe life-threatening complication. The use of growth factors was acceptable during the clinical study.
Best response was assessed by an MD Anderson radiologist every 2 cycles of therapy (1 cycle = 4 weeks) using the same RECIST guidelines used during the study period [17]. These criteria defined a partial response (PR) as a ≥30% decrease in the sum of the longest diameter of target lesions, excluding complete disappearance of disease (CR). Progressive disease (PD) was defined as a ≥20% increase in the sum of the longest diameter of target lesions. Stable disease (SD) was defined as small changes not meeting the criteria for a PR or PD. Waterfall plot analysis illustrated antitumor activity, if any, as previously described [18]. Responses shown in the waterfall plot were grouped according to standard RECIST criteria.
Survival was measured from start of treatment on protocol until death from any cause or last follow-up. Progression-free survival was measured from start of treatment on protocol until progression or death, whichever occurred first. A P-value < 0.05 was considered statistically significant. Statistical analyses were carried out using SAS 9.1 (SAS Institute, Cary, NC) and S-Plus, version 7.0 (Insightful Corp., Seattle, WA).
Results
Demographics
From December 2005 to April 2009, 29 patients were registered on protocol. Three patients became ineligible prior to initiation of therapy because of rapid decline in performance status (n = 1) and increased serum levels of bilirubin (n = 1) or creatinine (n = 1).
Twenty-six patients were treated. Their median age was 59 years (range, 35–77 years). There were 13 women and 13 men. The most common diagnoses were colorectal cancer (n = 10) and breast cancer (n = 7). One patient had each of the following cancers: gastric, hepatocellular, prostate, bladder, thyroid, small-cell lung, ovarian, melanoma, and cholangiocarcinoma. The median number of prior therapies was four (range, 0–12). Prior therapies are listed in Table 2.
Table 2.
Prior therapies
| 1 | FOLFOX-6 and bevacizumab; irinotecan and cetuximab; cetuximab, bevacizumab and irinotecan |
| 2 | Docetaxel; paclitaxel; anastrozole; capecitabine and gemcitabine |
| 3 | Neoadjuvant FAB; PAC with doxorubicin; TCH, vinorelbine, trastuzumab; gemcitabine, trastuzumab, nab-paclitaxel |
| 4 | FOLFOX and bevacizumab; FOLFIRI with bevacizumab; Cetuximab, irinotecan, and bevacizumab |
| 5 | Cyclophosphamide, methotrexate, and 5-FU; tamoxifen; anastrozole |
| 6 | 5-FU; leucovorin; irinotecan and cetuximab |
| 7 | 5-FU;capecitabine; FOLFOX plus bevacizumab; bevacizumab and oxaliplatin; irinotecan, cetuximab and bevacizumab |
| 8 | 5-FU and leucovorin; irinotecan; FOLFOX-6 and bevacizumab; TRAIL |
| 9 | Irinotecan, 5-FU, leucovorin; FOLFOX and bevacizumab; capecitabine; HAI cisplatin, 5-FU and leucovorin; cetuximab and irinotecan |
| 10 | Imatinib mesylate and letrozole; FEC; capecitabine with docetaxel; nab-paclitaxel and exemestane |
| 11 | Paclitaxel and carboplatin |
| 12 | Gemcitabine and cisplatin; MVAC; ifosfamide, paclitaxel and cisplatin; ATG |
| 13 | Irinotecan; capecitabine; FOLFOX 6; AEE-788; darinaparsin; irinotecan and cetuximab |
| 14 | Adriamycin, DTIC with chemoradiation; gemcitabine; docetaxel; liposomal doxorubicin; imatinib; capecitabine |
| 15 | None |
| 16 | FOLFOX and bevacizumab; FOLFIRI and bevacizumab; irinotecan and Cetuximab; irinotecan, oxaliplatin and cetuximab and bevacizumab; FOLFOX and panitumumab |
| 17 | Carboplatin and paclitaxel; carboplatin; carboplatin and paclitaxel |
| 18 | Sorafenib; gemcitabine and cisplatin; XELOX; FOLFIRI |
| 19 | Docetaxel; carboplatin and irinotecan; gemcitabine and epirubicin |
| 20 | Tamoxifen; anastrozole; exemestane; docetaxel; carboplatin; FAC; Capecitabine; vinorelbine; gemcitabine; bortezomib and bevacizumab |
| 21 | FOLFIRI and cetuximab; FOLFIRI and panitumumab; FOLFIRI and bevacizumab |
| 22 | FOLFOX; FOLFIRI and bevacizumab; cetuximab and irinotecan; FOLFOX |
| 23 | Chlorambucil; leuprolide acetate and bicalutamide; paclitaxel; docetaxel |
| 24 | Chemoembolization of the liver; sorafenib |
| 25 | Doxorubicin and cyclophosphamide; docetaxel; vinorelbine and trastuzumab; capecitabine with lapatinib; nab-paclitaxel and trastuzumab |
| 26 | Doxorubicin, cyclophosphamide, vinblastine, and methotrexate; letrozole and imatinib; docetaxel and capecitabine; vinorelbine; nab-paclitaxel; liposomal doxorubicin; dasatinib and gemcitabine; carboplatin and paclitaxel |
ATG anti-thymocyte globulin; FAC 5-fluorouracil, adriamycin, cyclophosphamide; FOLFOX 5-fluorouracil, folinic acid and oxaliplatin; FOLFIRI 5-fluorouracil, folinic acid and irinotecan; XELOX capecitabine and oxaliplatin
Dose escalation and dose-limiting toxicity
Dose escalation and DLTs are listed in Table 3. The MTD of HAI paclitaxel was 225 mg/m2 every 4 weeks. Cycles were repeated every 28 days. DLTs included Grade 3 neuropathy (1 of 5 patients) at HAI paclitaxel 275 mg/m2 and Grade 4 thrombocytopenia and neutropenia and Grade 3 mucositis (1 of 4 patients) at 250 mg/m2. None of the eight patients treated with HAI paclitaxel 225 mg/m2 experienced a DLT.
Table 3.
Distribution of patients, treatment cycles, and dose-limiting toxicities across tested dose levels
| Paclitaxel dose level (mg/m2) | No. of patients | No. of pts. who completed cycle 1 | No. of pts. with DLTs | Description of DLTs |
|---|---|---|---|---|
| 150 | 3 | 3 | 0 | |
| 175 | 3 | 3 | 0 | |
| 200 | 3 | 3 | 0 | |
| 225* | 8 | 8 | 0 | |
| 250 | 4 | 4 | 1 | Grade 4 thrombocytopenia and neutropenia, Grade 3 mucositis |
| 275 | 5 | 5 | 1 | Grade 3 neuropathy |
DLT was defined as any Grade 4 hematologic toxicity (as defined by the NCI CTC)>5 consecutive days or requiring transfusion or growth factor support, Grade 4 nausea/vomiting >5 days, any other Grade 3 non-hematologic toxicity, including symptoms/signs of vascular leakage or cytokine release syndrome, or any severe life-threatening complication. The maximum tolerated dose is shown in bold
DLT dose-limiting toxicity
Includes five patients treated in the expansion phase
Toxicity
A total of 50 cycles of HAI paclitaxel were administered. The median number of cycles administered per patient was two (range, 1–4). Toxicities are summarized in Table 4. Among 26 patients who completed cycle 1, 14 (54%) patients had no toxicity >Grade 1. The most common toxicities were peripheral neuropathy (n = 7), nausea (n = 6), anorexia (n = 5), and fatigue (n = 5) (Table 4). Two patients required treatment with granulocyte colony-stimulating factor (one patient received pegfilgrastim and one received filgrastim).
Table 4.
Toxicity
| Adverse event | Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|---|---|---|---|
| Nausea/vomiting | 6/2 | |||
| Fatigue | 5 | 2 | 1 | |
| Constipation | 2 | 1 | ||
| Anorexia | 5 | 3 | ||
| Myalgia/bone pain | 1 | 1 | ||
| Neuropathy | 7 | |||
| Abdominal pain | 1 | |||
| Diarrhea | 1 | |||
| Neutropenia | 3 | 2 | ||
| Thrombocytopenia | 1 | |||
| Infection | 1 | |||
| Mucositis | 2 | 1 | ||
| Fever | 4 | |||
| Headache | 1 | |||
| Hypertension | 1 | |||
| Rash | 1 | |||
| Dyspnea | 3 | |||
| Pruritus | 2 | |||
| Alopecia | 1 | |||
| Numbness | 1 | |||
| Night sweats | 1 |
Response
Of 26 treated patients, 22 patients reached their first restaging evaluation at 2 months. Four patients did not have CT restaging imaging studies for the following reasons: consent withdrawal (n = 1), insurance denied payment for continuation on the study (n = 1), and development of advanced cancer-related complications that were deemed to be unrelated to treatment by their treating physician (n = 2); one patient developed pulmonary embolism on cycle 1 day 42 and did not receive further therapy; the other patient experienced a fall on cycle 2 day 3 and did not return for follow-up.
Response is shown in Table 5. Of 22 patients evaluable for response, five patients had SD by RECIST, including 3 (13.6%) patients who had SD for ≥ 4 months (colorectal cancer, n = 1; thyroid cancer, n = 1; and hepatocellular carcinoma, n = 1). Of eight evaluable patients treated at the MTD, 2 (25%) had SD.
Table 5.
Characteristics of patients treated with hepatic arterial infusion of paclitaxel with stable disease
| Patient no. | Age/sex | PS | Paclitaxel mg/m2 | No. of prior Rx | No. of cycles | Type of cancer | Reason off-protocol comments | Progression-free survival, months |
|---|---|---|---|---|---|---|---|---|
| 3 | 43/F | 1 | 150 | 4 | 2 | Breast | Biliary abscess | 2.0 |
| 6 | 71/M | 1 | 175 | 3 | 4 | Colorectal | PD | 4.0 |
| 10 | 67/F | 0 | 225 | 3 | 2 | Breast | Tumor markers increased | 2.1 |
| 14 | 35/F | 1 | 250 | 7 | 4 | Thyroid | Tumor markers increased | 7.1 |
| 27 | 59/M | 0 | 225 | 3 | 3 | Hepatocellular | No evidence of PD | 22.2+ |
N/A non-applicable; PD progressive disease; PS performance status; SD stable disease
Survival
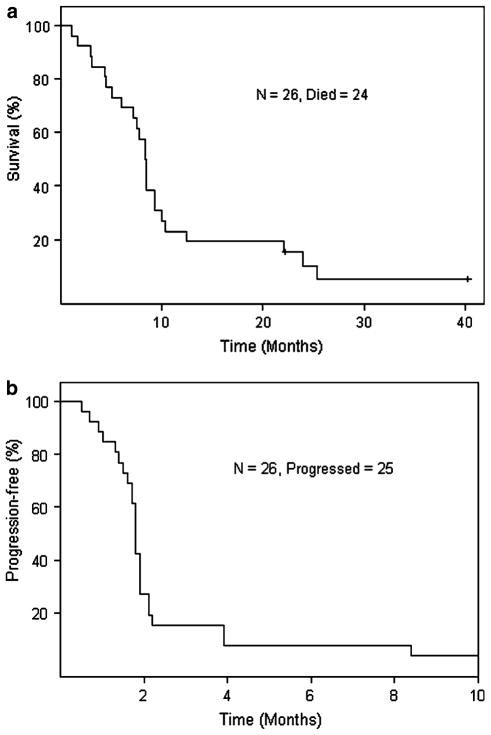
The median follow-up of surviving patients was 31 months. Twenty-four of 26 patients have died. The median overall survival was 8.3 months (95% CI, 7.2–10.3; range, 1.1–40.3+ months) (Fig. 1a).
Fig. 1.
a Kaplan–Meier plot for overall survival; median survival = 8.3 months (95% CI: 7.2–10.3). b Kaplan–Meier plot for progression-free survival; median PFS = 1.8 months (95% CI: 1.7–2.1)
Failure-free survival
Twenty-five patients had progressive disease. The median progression-free survival was 1.8 months (95% CI, 1.7–1.9; range, 0.5–22.2+ months) (Fig. 1b). A 59-year-old man with history of hepatitis C–associated metastatic hepatocellular cancer received 3 cycles of HAI paclitaxel at the 225 mg/m2 dose level, and he remains alive with SD without any further therapy 22.2+ months after initiation of treatment on protocol. This patient had undergone resection of the left lobe of the liver and chemoembolization, and he was previously treated with sorafenib.
Discussion
This study established that the MTD of HAI paclitaxel was 225 mg/m2. Overall, this regimen was well tolerated, and the most common toxicities were peripheral neuropathy, nausea, anorexia, and fatigue. Overall, 12% of patients had SD for ≥ 4 months (colorectal cancer, n = 1; hepatocellular carcinoma, n = 1; and thyroid cancer, n = 1). HAI chemotherapy–induced hepatotoxicity, including biliary sclerosis, reported in earlier trials in 6 to 25% of patients treated with FUDR, [19] was not observed in our study, probably because of premedication with corticosteroids to prevent toxicity. HAI paclitaxel was associated with an overall favorable toxicity profile. In our experience, HAI oxaliplatin is complicated with pain reaction in selected patients and HAI irinotecan may be associated with diarrhea in a few patients, suggesting that the HAI paclitaxel toxicity profile may be more favorable than that for HAI oxaliplatin or HAI irinotecan.
Other investigators have demonstrated an association of HAI paclitaxel with favorable clinical outcomes in patients with advanced gastric cancer metastatic to the liver [13]. In anecdotal cases, CR of liver metastases has been documented in breast cancer patients treated with weekly doses of HAI paclitaxel [9]. Also, docetaxel has been occasionally used in regional therapy, with some responses noted in squamous cell carcinoma of the lung [20], hypopharynx [21], head and neck, [22] and breast metastatic to the liver [8]. We previously reported that HAI oxaliplatin combination therapy has antitumor activity in patients with colorectal cancer and predominant liver metastases [23] and that HAI cisplatin and IV liposomal doxorubicin has antitumor activity in breast cancer with hepatic metastases [24].
Keeping in mind that in our clinical trial, the median number of prior therapies per patient was four, HAI paclitaxel had antitumor activity in patients with colorectal, thyroid, and hepatocellular cancer. Interestingly, the patient with hepatocellular carcinoma received 3 cycles of HAI paclitaxel at the 225 mg/m2 dose level and remains alive with SD without any further therapy 22.2+ months after initiation of treatment on protocol. This patient had undergone resection of the left lobe of the liver and chemoembolization, and he was previously treated with sorafenib.
Although pharmacokinetic analysis was not performed in the current study, other investigators have reported on the pharmacokinetics of HAI paclitaxel versus IV paclitaxel. First, it was shown that 100 mg/m2 of paclitaxel intraarterially over 4 h results in a hepatic extraction ratio of paclitaxel as high as 0.95 during the injection (paclitaxel levels were measured in serial samples of both the hepatic artery and vein) [14]. Then, other investigators measured only intravenous paclitaxel levels in two patients who were treated with IV paclitaxel the first week and, subsequently, with a 1-hour infusion of paclitaxel intraarterially. In the first 2 weeks, venous blood was sampled five times following the paclitaxel injection. The IV paclitaxel concentrations 24 h after HAI in the two patients were 45 and 33 ng/ml, which were considered high enough for cytotoxic activities. The authors presumed that the kinetics of the venous concentrations of paclitaxel following HAI were similar to those after intravenous injection in both patients and, therefore, that the hepatic extraction rate of this agent was low [25]. However, caution is warranted regarding the validity and interpretation of these results, as paclitaxel levels in the hepatic artery were not measured.
Limitations of this therapeutic strategy include the fact that although this treatment can be administered in a multidisciplinary hospital setting with the collaboration of interventional radiologists, it is costly and requires hospitalization for 2 days every 4 weeks. In addition, advances in nanotechnology have resulted in the development of albumin-bound paclitaxel (nab-paclitaxel). Results of ongoing phase I clinical trials of HAI albumin-bound paclitaxel-containing therapy may produce superior clinical outcomes compared to HAI paclitaxel in patients with advanced cancer and predominant liver metastases [26, 27].
In conclusion, the MTD of HAI paclitaxel was 225 mg/m2 and, overall, the regimen was well tolerated. Disease stabilization with HAI paclitaxel was evidenced in patients with advanced colorectal cancer, thyroid cancer, and hepatocellular carcinoma with dominant liver metastases. This approach continues to be investigational, and therefore, it should be reserved for further evaluation on a clinical trial. Most likely, in future studies, HAI paclitaxel will be replaced by the HAI nab-paclitaxel formulation. Ongoing clinical trials of HAI nab-paclitaxel may offer a therapeutic option in selected patients with advanced cancer and predominant liver metastases.
Acknowledgments
Supported in part by Grant Number RR024148 from the National Center for Research Resources, a component of the NIH Roadmap for Medical Research (http://nihroadmap.nih.gov/clinicalresearch/overview). We thank Joann Aaron for editing this manuscript.
Contributor Information
Apostolia M. Tsimberidou, Email: atsimber@mdanderson.org, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA
Katherine Letourneau, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Siqing Fu, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
David Hong, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Aung Naing, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Jennifer Wheler, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Cynthia Uehara, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Stephen E. McRae, Department of Interventional Radiology, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA
Sijin Wen, Department of Biostatistics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Razelle Kurzrock, Phase I Program, Department of Investigational Cancer Therapeutics, The University of Texas MD Anderson Cancer Center, Unit 455, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
References
- 1.Ragnhammar P, Hafstrom L, Nygren P, et al. A systematic overview of chemotherapy effects in colorectal cancer. Acta Oncol. 2001;40:282–308. doi: 10.1080/02841860151116367. [DOI] [PubMed] [Google Scholar]
- 2.Power DG, Healey-Bird BR, Kemeny NE. Regional chemotherapy for liver-limited metastatic colorectal cancer. Clin Colorectal Cancer. 2008;7:247–259. doi: 10.3816/CCC.2008.n.032. [DOI] [PubMed] [Google Scholar]
- 3.Khatri VP, Chee KG, Petrelli NJ. Modern multimodality approach to hepatic colorectal metastases: solutions and controversies. Surg Oncol. 2007;16:71–83. doi: 10.1016/j.suronc.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Pawlik TM, Choti MA. Surgical therapy for colorectal metastases to the liver. J Gastrointest Surg. 2007;11:1057–1077. doi: 10.1007/s11605-006-0061-3. [DOI] [PubMed] [Google Scholar]
- 5.Curley SA, Izzo F, Abdalla E, et al. Surgical treatment of colorectal cancer metastasis. Cancer Metastasis Rev. 2004;23:165–182. doi: 10.1023/a:1025875332255. [DOI] [PubMed] [Google Scholar]
- 6.Damascelli B, Patelli GL, Lanocita R, et al. A novel intraarterial chemotherapy using paclitaxel in albumin nanoparticles to treat advanced squamous cell carcinoma of the tongue: preliminary findings. AJR Am J Roentgenol. 2003;181:253–260. doi: 10.2214/ajr.181.1.1810253. [DOI] [PubMed] [Google Scholar]
- 7.Zhao Y, Wang SM, Zhang J. Combination chemotherapy with Taxol and cisplatin for 57 patients with non-small cell lung cancer by intraartery and intravenous infusion. Ai Zheng. 2002;21:1365–1367. [PubMed] [Google Scholar]
- 8.Chino Y, Suzuki Y, Ubukata N, et al. Hepatic infusion of docetaxel using PEIT for a patient with stage IV breast cancer. Gan To Kagaku Ryoho. 2001;28:1897–1899. [PubMed] [Google Scholar]
- 9.Iwamoto S, Gon G, Nohara T, et al. A case of liver metastasis of breast cancer successfully treated with paclitaxel infusion into the hepatic artery: an attempt of once weekly regimen. Gan To Kagaku Ryoho. 2002;29:917–920. [PubMed] [Google Scholar]
- 10.Kim SJ, Maeura Y, Ueda N, et al. A case of hepatic arterial infusion chemotherapy with docetaxel for liver metastasis from breast cancer. Gan To Kagaku Ryoho. 1999;26:1959–1962. [PubMed] [Google Scholar]
- 11.Kitagawa Y, Nakase Y, Ebihara Y, et al. A case of multiple liver metastases from breast cancer successfully treated with intra-arterial administration of paclitaxel. Gan To Kagaku Ryoho. 2001;28:2061–2064. [PubMed] [Google Scholar]
- 12.Yoon CJ, Chung JW, Park JH, et al. Transcatheter arterial chemoembolization with paclitaxel-lipiodol solution in rabbit VX2 liver tumor. Radiology. 2003;229:126–131. doi: 10.1148/radiol.2291021029. [DOI] [PubMed] [Google Scholar]
- 13.Matsui S, Tono T, Iwazawa T, et al. A case of postoperative hepatic metastasis from gastric cancer responding to hepatic arterial infusion chemotherapy of paclitaxel. Gan To Kagaku Ryoho. 2002;29:2076–2079. [PubMed] [Google Scholar]
- 14.Walton GD, Schreeder MT, Rizzo J, et al. Hepatic artery administration of paclitaxel. Cancer Invest. 1999;17:118–120. [PubMed] [Google Scholar]
- 15.Camacho LH, Kurzrock R, Cheung A, et al. Pilot study of regional, hepatic intra-arterial paclitaxel in patients with breast carcinoma metastatic to the liver. Cancer. 2007;109:2190–2196. doi: 10.1002/cncr.22672. [DOI] [PubMed] [Google Scholar]
- 16.http://ctep.cancer.gov/
- 17.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European organization for research and treatment of cancer, national cancer institute of the United States, national cancer institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 18.Ratain MJ, Eisen T, Stadler WM, et al. Phase II placebo-controlled randomized discontinuation trial of sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2006;24:2505–2512. doi: 10.1200/JCO.2005.03.6723. [DOI] [PubMed] [Google Scholar]
- 19.Kemeny NE, Ron IG. Hepatic arterial chemotherapy in metastatic colorectal patients. Semin Oncol. 1999;26:524–535. [PubMed] [Google Scholar]
- 20.Oura S, Sakurai T, Yoshimura G, et al. Recurrent squamous-cell lung cancer treated with bronchial-arterial infusion of docetaxel–case report. Gan To Kagaku Ryoho. 1998;25:2109–2113. [PubMed] [Google Scholar]
- 21.Akisada T, Harada T, Takemoto T, et al. A case of advanced hypopharyngeal carcinoma successfully treated with superselective intra-arterial infusion of docetaxel. Gan To Kagaku Ryoho. 2002;29:323–328. [PubMed] [Google Scholar]
- 22.Yabuuchi H, Kuroiwa T, Tajima T, et al. Efficacy of intra-arterial infusion therapy using a combination of cisplatin and docetaxel for recurrent head and neck cancers compared with cisplatin alone. Clin Oncol (R Coll Radiol) 2003;15:467–472. doi: 10.1016/j.clon.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Tsimberidou AM, Fu S, Ng C, et al. A phase 1 study of hepatic arterial infusion of oxaliplatin in combination with systemic 5-fluorouracil, leucovorin, and bevacizumab in patients with advanced solid tumors metastatic to the liver. Cancer. 2010 doi: 10.1002/cncr.25277. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsimberidou AM, Moulder S, Fu S, et al. Phase I clinical trial of hepatic arterial infusion of cisplatin in combination with intravenous liposomal doxorubicin in patients with advanced cancer and dominant liver involvement. Cancer Chemother Pharmacol. 2010 doi: 10.1007/s00280-010-1266-4. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tono T, Iwazawa T, Matsui S, et al. Hepatic arterial infusion of paclitaxel for liver metastasis from gastric cancer. Cancer Invest. 2004;22:550–554. doi: 10.1081/cnv-200026526. [DOI] [PubMed] [Google Scholar]
- 26.NCT00732836 A phase 1, open label, non-randomized trial of hepatic arterial infusion of Abraxane with a pharmacokinetic study in advanced solid cancer patients with predominant hepatic metastases, http://clinicaltrials.gov/ct2/show/NCT00732836?term=kurzrock+abraxane&rank=2
- 27.NCT01057264 A phase 1, open label, non-randomized trial of hepatic arterial infusion (HAI) of abraxane in combination with gemcitabine and bevacizumab for patients with advanced cancers metastatic to the liver, http://clinicaltrials.gov/ct2/show/NCT01057264?term=tsimberidou&rank=7