Abstract
Background
Telestroke has been effective in the management of acute ischemic stroke (AIS). This study characterizes and compares Stroke Specialist (SS) and Emergency Physician (EP) perceptions of telestroke and identifies barriers preventing increased implementation.
Methods
A survey was developed and distributed nationwide to 382 SSs via an online survey-system and in paper form to 226 EPs attending the 2008 American College of Emergency Physicians (ACEP) national conference.
Results
Stroke specialists perceived themselves to be more knowledgeable about telemedicine and telestroke (p<0.001 and p=0.010). A large majority of physicians in both specialties either strongly agreed or agreed that telestroke will reduce geographical differences in stroke management and that it is superior to telephone consultation. EPs perceived patient preference (p<0.001), rt-PA side effects (p<0.001), level of technology (p=0.005), and rt-PA not the standard of care (p<0.001) to be more significant obstacles to increased implementation of telestroke than SSs. However, SSs found increased personal work to be a greater barrier than EPs (p<0.001).
Conclusion
SSs and EPs report positive beliefs regarding telestroke, however perceived obstacles exist to implementation. Differences between barriers perceived by EPs and SSs need to be addressed to enhance AIS treatment.
Keywords: Stroke Care, Telemedicine, Telestroke, Emergency Medicine, Acute Stroke
Introduction
Telestroke, real-time audio and visual communication between a stroke specialist (SS) and emergency physicians (EP), has been proposed as a solution to low rt-PA administration rates in acute ischemic stroke (AIS)1,2. The technology is currently used by a number of hospital systems, both within the United States and internationally3,4. Studies show its advantages over traditional telephone consults4. Yet, despite its demonstrated safety and effectiveness in increasing rt-PA administration rates, the technology has not been implemented in many hospitals that stand to benefit.
We characterize and compare the attitudes, beliefs and perceived barriers of SSs and EPs regarding the broader implementation of telestroke.
Materials and Methods
A standardized survey was developed based on a literature review and interviews with community and academic SSs and EPs. As limited research is available regarding physician perceptions of telestroke, literature focusing on telemedicine generally was reviewed5,6.
The survey was piloted at our institution and subsequently distributed nationwide via an online system to 382 SS identified through a review of SSs at academic centers. SSs had 4 weeks to respond to the survey, with a reminder after 2 weeks. The survey was distributed in paper form at the American College of Emergency Physicians (ACEP) conference (Chicago, Il. October 27th-30th 2008) and was available to all physicians attending the conference. Physicians were encouraged to watch a video of an actual telestroke consult to ensure a base level of familiarity with the technology7. The survey required approximately 20 minutes to complete.
All results and statistics were compiled using SPSS (SPSS Inc. version 15.0, Chicago, Il). Non-parametric Mann-Whitney scores were used to compare SSs and EPs to account for the deviations from a normal distribution. p values of < 0.05 were considered significant.
Results
One hundred and thirty five (35%) of the 382 SS surveyed and 226 EPs completed the survey. The average age (yrs) of the SSs and EPs were 47±9 and 41±10 (p<0.001). Fifty-five percent of the EPs were attendings > five years, compared to 82% of SSs (p <0.001). 10.7% of EPs indicated rural practice. Forty-three (31.6%) of the SS were familiar with telestroke from personal use, as compared to 17 (7.5%) of EPs surveyed (p<0.001).
Tables 1-3 summarize the data. SSs spent less time using the internet (p=0.008), but indicated more knowledge regarding telemedicine and telestroke (p<0.001 and p=0.010). Of the SSs, most (89.6% and 87.4% respectively) either strongly agreed or agreed that telestroke will reduce geographical differences in stroke management and that it is superior to telephone consultation. Similarly, the majority of EPs (91.9% and 97.2% respectively) responded optimistically regarding the above items. SSs perceived ambiguity in reimbursement and medical liability as the greatest barriers. EPs reported medical liability and time/cost of installation as the most significant obstacles. EPs perceived patient preference for physical visits (p<0.001), management of rt-PA sideeffects(p<0.001), level of technology (p=0.005), and rt-PA not the standard of care for AIS (p<0.001) as more significant obstacles. SSs found increased personal work to be a greater barrier than EPs (p<0.001).
Table 1.
Technology, Telemedicine,and Telestroke
| ITEM | Emergency Physician | Stroke Specialist |
P-Value |
|---|---|---|---|
| Mean (SD) Scale |
Mean(SD) | Mann-Whitney U | |
| Daily internet use | 2.16 (0.94) 1(< 1 hour) to 4 (> 3 hours) |
1.90 (0.93) | 0.008 |
|
Knowledge of technology
is higher than colleagues |
2.27 (0.97) 1(strongly disagree) to 4(strongly agree) |
2.36 (0.99) | 0.365 |
|
First in specialty to adopt
technologies |
2.44 (0.86) 1 (strongly disagree) to 4 (strongly agree) |
2.46 (0.90) | 0.967 |
|
Knowledge of
Telemedicine |
2.64 (0.71) 1 (no knowledge) to 4 (very knowledgeable) |
3.08 (0.73) | <0.001 |
| Knowledge of Telestroke | 2.88 (0.78) 1 (no knowledge) to 4 (very knowledgeable) |
3.11 (0.72) | 0.010 |
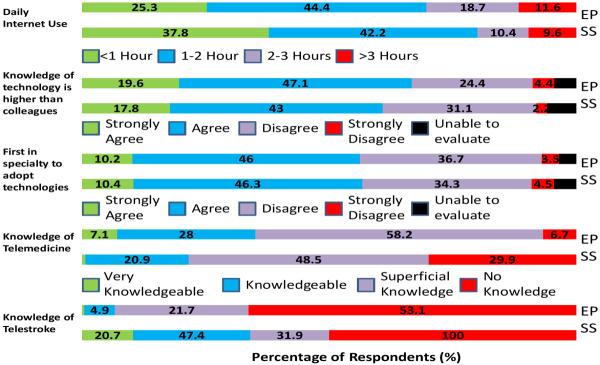
| |||
Table 3.
Perceived Barriers
| Barrier | Emergency Physician | Stroke Specialist | P-Value |
|---|---|---|---|
|
Mean (SD) 1 (very significant barrier) to 5 (no barrier) |
Mean (SD) | Mann-Whitney U | |
| Level of technology | 2.83 (1.17) | 3.13 (0.99) | 0.005 |
| Time and cost of installation | 2.43 (1.05) | 2.36 (1.03) | 0.625 |
|
Perception that rtPA not
considered “standard of care” |
2.90 (1.21) | 3.43 (1.10) | <0.001 |
| Increased personal work | 3.11 (1.12) | 2.52 (1.17) | <0.001 |
|
Management of rt-PA side-
effects |
2.50 (1.21) | 2.94 (1.10) | <0.001 |
| Medical liability | 2.34 (1.16) | 2.26 (1.14) | 0.528 |
|
Patients prefer physical
visits |
3.00 (1.28) | 3.55 (1.08) | <0.001 |
|
Safety/Confidentiality of
online data |
3.53 (1.19) | 3.78 (0.99) | 0.073 |
| Adequacy of reimbursement | NA | 1.96 (0.99) | N/A |
|
Time taken away from care
of patients in the ED |
3.14 (1.18) | NA | N/A |
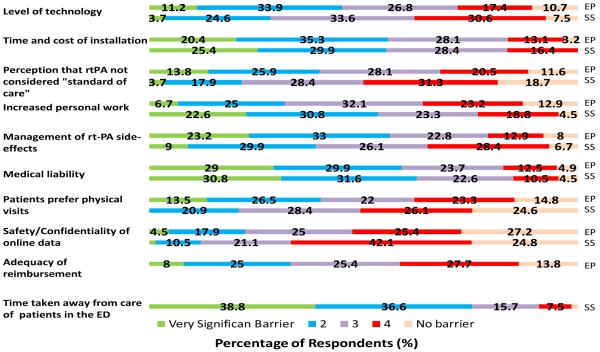
| |||
There were no significant differences between EPs indicating rural versus non rural practices.
Discussion
Telemedicine for remote diagnosis and management of AIS is a feasible solution to low rt-PA administration rates8,9,10. We have shown that telemedicine is viewed favorably by SSs and EPs. However, while SS and EPs agree on the potential of telestroke, concerns regarding medico-legal guidelines, reimbursement, and time/cost of installation impede implementation.
It is important to note that many of these concerns have been informally recognized by leaders in the telestroke field2,11,12. Educating potential users with regards to progress in these areas is critical in increasing physician buy-in.
EPs viewed rt-PA not being the standard-of-care in AIS and management of rt-PA complications to be more significant obstacles than SSs. With regards to these concerns, studies have shown that EPs are less comfortable with rt-PA as the standard of care13. This may be driving the differences observed here.
Limitations of this study included the use of an online survey for SS and paper for EPs. A large non-response rate from SSs, the inability to calculate the non-response rate of EPs, and the use of a convenience sample of EPs at a national conference limits generalizability and may have contributed to a selection bias as those with increased familiarity with telemedicine/telestroke may have been more or less likely to respond. Due to the low percentage of EPs indicating a rural practice in this sample, additional studies regarding this population are warranted. Finally, this survey did not differentiate between web-based and ‘work-station’ models of telestroke.
Table 2.
Beliefs and Expectations
| ITEM | Emergency Physician | Stroke Specialist |
P-value |
|---|---|---|---|
|
Mean (SD) 1 (strongly agree) to 4 (strongly disagree) |
Mean (SD) | Mann-Whitney U | |
|
Improve the diagnosis
and treatment of AIS |
1.83 (0.58) | 1.55 (0.63) | <0.001 |
|
More effective than
telephone consultation |
1.69 (0.54) | 1.64 (0.86) | 0.040 |
|
Reduce geographical
differences in regional stroke care |
1.85 (0.57) | 1.78 (0.87) | 0.019 |
|
Number of EDs using
Telestroke will increase |
1.88 (0.52) | 1.87 (0.91) | 0.061 |
|
Telestroke will be useful
in research of emerging stroke medications |
1.87 (0.54) | 2.02 (0.89) | 0.376 |
|
Telestroke will be useful
in physician and community stroke education |
1.86 (0.60) | 2.17 (0.87) | 0.002 |
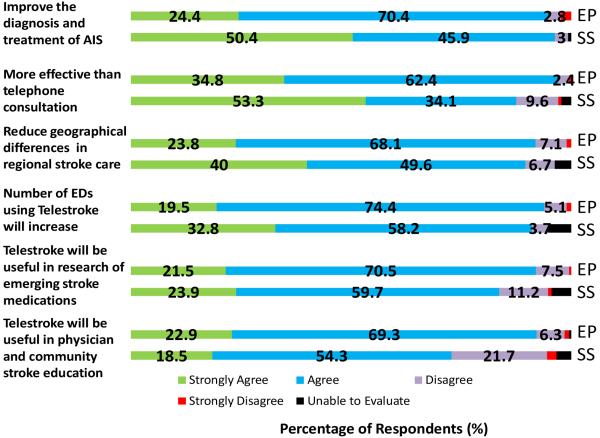
| |||
Acknowledgements
Supported by NIH-NINDS T32 NS051147, The Gaisman Foundation, and Mount Sinai Medical Student Research Office
Presented as an abstract at the 2009 International Stroke Conference, San Diego, California and at the 2009 American College of Emergency Physicians, Boston, Mass.
Footnotes
Conflicts of Interest/Disclosures: No conflicts
The authors acknowledge the assistance of Sean I. Savitz M.D. in collecting contact information of Stroke Specialists
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Levine SR, M Gorman. “Telestroke”: The Application of Telemedicine for Stroke. Stroke. 1999;30(2):464–9. doi: 10.1161/01.str.30.2.464. [DOI] [PubMed] [Google Scholar]
- 2.Switzer J, Levine SR, Hess D. Telestroke 10 Years Later - ‘Telestroke 2.0’. J Stroke Cerebrovasc Dis. 2009;28(4):323–330. doi: 10.1159/000229550. [DOI] [PubMed] [Google Scholar]
- 3.Demaerschalk BM, Miley ML, Kiernan TE, Bobrow BJ, Corday DA, Wellik KE, Aguilar MI, Ingall TJ, Dodick DW, Brazdys K, Koch TC, Ward MP, Richemont PC. STARR Coinvestigators. Stroke Telemedicine. Mayo Clin Proc. 2009;84(1):53–64. doi: 10.4065/84.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer BC, Raman R, Hemmen T, Obler R, Zivin JA, Rao R, Thomas RG, Lyden PD. Efficacy of site-independent telemedicine in the STRokE DOC trial: a randomised, blinded, prospective study. Lancet Neurol. 2008;7(9):787–95. doi: 10.1016/S1474-4422(08)70171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Segura J, Roldán C, Galera J, Naval J. What Do Spanish physicians believe and expect about telemedicine? Results of a Delphi-based survey. Telemed J E Health. 2008;14(1):42–8. doi: 10.1089/tmj.2007.0018. [DOI] [PubMed] [Google Scholar]
- 6.Barton PL, Brega AG, Devore PA, Mueller K, Paulich MJ, Floersch NR, Goodrich GK, Talkington SG, Bontrager J, Grigsby B, Hrincevich C, Neal S, Loker JL, Araya TM, Bennett RE, Krohn N, Grigsby J. Specialist Physicians’ Knowledge and Beliefs about Telemedicine: A Comparison of Users and Non users of the Technology. Telemed J E Health. 2007;13(5):487–500. doi: 10.1089/tmj.2006.0091. [DOI] [PubMed] [Google Scholar]
- 7.Graham S. [27 May 2007]; [1 May 2008];Diagnosis at a Distance. New York Times. < http://health.nytimes.com/health/guides/disease/stroke/overview.html>.
- 8.Hess DC, Wang S, Gross H, Nichols FT, Hall CE, Adams RJ. Telestroke: extending stroke expertise into underserved areas. Lancet Neurol. 2006;5(3):275–8. doi: 10.1016/S1474-4422(06)70377-5. [DOI] [PubMed] [Google Scholar]
- 9.Schwamm LH, Holloway RG, Amarenco P, Audebert HJ, Bakas T, Chumbler NR, Handschu R, Jauch EC, Knight WA, 4th, Levine SR, Mayberg M, Meyer BC, Meyers PM, Skalabrin E, Wechsler LR. American Heart Association Stroke Council; Interdisciplinary Council on Peripheral Vascular Disease. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40(7):2616–34. doi: 10.1161/STROKEAHA.109.192360. [DOI] [PubMed] [Google Scholar]
- 10.Switzer JA, Hall C, Gross H, Waller J, Nichols FT, Wang S, Adams RJ, Hess DC. A web-based telestroke system facilitates rapid treatment of acute ischemic stroke patients in rural emergency departments. J Emerg Med. 2009;36(1):12–8. doi: 10.1016/j.jemermed.2007.06.041. [DOI] [PubMed] [Google Scholar]
- 11.Stanberry B. Legal and ethical aspects of telemedicine. J Telemed Telecare. 2006;12(4):166–175. doi: 10.1258/135763306777488825. [DOI] [PubMed] [Google Scholar]
- 12.de Bustos EM, Moulin T, Audebert H. Barriers, Legal Issues, Limitations and Ongoing Questions in Telemedicine Applied to Stroke. J Stroke Cerebrovasc Dis. 2009;27(4):36–9. doi: 10.1159/000213057. [DOI] [PubMed] [Google Scholar]
- 13.Meschia JF, Williams LS. Views on the use of tissue plasminogen activator in acute ischemic stroke: A state-wide survey among neurologists and emergency medicine physicians in Indiana. J Stroke Cerebrovasc Dis. 1999;8(4):207–10. doi: 10.1016/s1052-3057(99)80068-8. [DOI] [PubMed] [Google Scholar]


