Abstract
Objectives.
The purpose of the current study was to prospectively test the utility of a social cognitive theory (SCT) model of physical activity behavior over an 18-month period in middle-aged and older adults (N = 321; M age = 63.8 years).
Methods.
Participants completed measures of self-efficacy, disability limitations, goals, outcome expectations, and physical activity at baseline and follow-up. Self-efficacy was hypothesized to influence physical activity both directly and indirectly through goals and outcome expectations. Relationships were examined using panel analysis within a covariance modeling framework.
Results.
The model provided an excellent fit to the data (χ2 = 36.16, df = 30, p = .20; comparative fit index = 1.00; root mean square error of approximation = .03). At baseline, self-efficacy was directly related to outcome expectations, disability limitations, goals, and physical activity and indirectly related to physical activity through physical outcome expectations. Changes in self-efficacy were significantly related to residual changes in outcome expectations, disability limitations, goals, and physical activity and indirectly related to residual changes in physical activity through changes in physical and social outcome expectations.
Discussion.
These results provide further support for the use of SCT to physical activity behavior in middle-aged and older adults. Self-efficacy influenced physical activity both directly and indirectly via outcome expectations, suggesting that these variables should be targeted in physical activity interventions for middle-aged and older adults.
Keywords: Middle aged, Older adults, Physical activity, Social cognitive theory
OLDER adults are not only one of the fastest growing segments of the U.S. population (U.S. Census Bureau, Population Division, 2008), they are also one of the most inactive with only approximately 31.5% of adults aged 65–74 years and 17.6% of adults aged 75 years and older meeting the public health physical activity guidelines (U.S. Department of Health and Human Service, Centers for Disease Control and Prevention, 2009). The high level of inactivity in this population is especially alarming as both age and physical inactivity are primary risk factors for a multitude of diseases/conditions, disability, and decreased quality of life (Brown et al., 2003; Rejeski & Mihalko, 2001). As the “baby boomer” generation enters the 65 years and older age range, it is critical to develop a better understanding of physical activity behavior in middle-aged and older adults in order to increase physical activity rates and significantly improve public health, reduce health care cost, and increase the likelihood of these individuals maintaining their ability to live independently. Social cognitive theory (SCT; Bandura, 1986, 1997, 2004) may be a particularly useful framework for understanding physical activity behavior in middle-aged and older adults and for developing and designing programs geared toward the initiation and maintenance of physical activity in this population.
SCT (Bandura, 1986, 1997, 2004) specifies a core set of psychosocial determinants (i.e., self-efficacy, outcome expectations, goals, and impediments and facilitators) for effectively understanding a broad range of health behaviors, including physical activity. SCT has been one of the most frequently applied theoretical models for understanding physical activity behavior in the general population and in older adults (McAuley & Blissmer, 2000). Self-efficacy reflects one’s beliefs in one’s capabilities to successfully complete a course of action and has generally been shown to be the “active agent” in SCT models. Bandura (2004) specified the pathways through which social cognitive constructs influence health behavior. Specifically, self-efficacy operates both directly and indirectly, through outcome expectations, goals, and facilitators and impediments, to influence behavioral outcomes. These factors are proposed to interact such that individuals with higher levels of self-efficacy have more positive expectations about what the behavior will bring about, set higher goals for themselves, and are more likely to take the view that they are capable of overcoming barriers resulting in a greater likelihood of engaging and maintaining specific behaviors (Bandura, 2004). Overall, the existing evidence supports both a direct and an indirect relationship between self-efficacy and physical activity (McAuley & Blissmer, 2000). However, the vast majority of the literature examining the relationship of SCT constructs to physical activity has adopted a piecewise approach, often only examining one- or two-model constructs at a time. Furthermore, self-efficacy has been the focus of the majority of this research with the other SCT constructs receiving far less attention. In order to better understand physical activity behavior and design more effective interventions and programs, it is important to examine self-efficacy in conjunction with the other SCT constructs.
As noted, self-efficacy has been consistently associated with physical activity behavior (Trost, Owen, Bauman, Sallis, & Brown, 2002) across an array of populations (Dishman et al., 2004; McAuley et al., 2007; Rogers, McAuley, Courneya, & Verhulst, 2008; Steele et al., 2000). It is well established that the relationship between self-efficacy and physical activity is reciprocal such that higher levels of self-efficacy have been associated with greater participation in physical activity and greater participation in physical activity has been associated with higher levels of self-efficacy (McAuley & Blissmer, 2000). Self-efficacy has also been shown to mediate the relationship between physical activity and improvements in well-being in older adults (Netz, Wu, Becker, & Tenenbaum, 2005). Although much of the research to date has focused on self-efficacy in isolation of the other model constructs, evidence exists to support its indirect relationship to physical activity via outcome expectations and goals.
Outcome expectations reflect individual beliefs about what will result from engaging in specific behaviors. Bandura (2000, 2004) identified three classes of outcome expectations: physical, social, and self-evaluative. Physical outcome expectations reflect beliefs about physical experiences resulting from engagement in physical activity (e.g., exercise will aid in weight control). Social outcome expectations reflect beliefs regarding increased opportunities for socialization (e.g., exercise will provide companionship). Finally, self-evaluative outcome expectations capture beliefs relative to the feelings of satisfaction and self-worth (e.g., exercise will provide me with a sense of accomplishment). Higher outcome expectations have been shown to be related to greater physical activity participation (Son, Kerstetter, Mowen, & Payne, 2009; Stewart & King, 1991; Williams, Anderson, & Winett, 2005; Wójcicki, White, & McAuley, 2009). Additionally, evidence exists to suggest that individuals with stronger self-efficacy for exercise exhibit higher outcome expectations for physical activity and that the three different types of outcome expectations may be differentially related to physical activity participation depending on the population of interest (Wójcicki et al., 2009). However, the evidence supporting the relationship between outcome expectations and physical activity is somewhat equivocal and can be attributed to either outcome expectations being reduced to a redundant predictor due to the strength of the self-efficacy and physical activity relationship (Bandura, 1997) or previous studies collapsing all three types of outcome expectations into a single variable, thereby attenuating the independent influence of each type of outcome expectation on physical activity behavior (Wójcicki et al., 2009).
Goal setting can be a useful self-regulating resource to assist individuals in adopting and maintaining regular physical activity patterns as it directs effort and guides behavior (Bandura, 2004). Increased frequency of goal setting has been shown to be related to increased use of physical activity self-monitoring techniques (Nothwehr & Yang, 2007), and individuals who set higher goals have been shown to exhibit greater increases in physical activity participation (Dishman, Vandenberg, Motl, Wilson, & DeJoy, 2009). Self-regulation, or the ability to monitor behavior in order to achieve goals, has also been associated with regular exercise participation in older adults (Son et al., 2009; Umstattd & Hallam, 2007). Individuals with higher levels of self-efficacy have also been shown to engage in more frequent goal setting, planning, and monitoring of their behavior, which has resulted in increased participation in physical activity (Rovniak, Anderson, Winett, & Stephens, 2002).
Finally, Bandura (2004) has suggested that a host of factors can act as impediments and facilitators to participation in health behaviors. Although many of these may be common across all adults, in the context of aging, impediments may take on a particularly salient role. Indeed, perceived poor health and symptoms of physical disabilities associated with chronic disease are often reported as major barriers to physical activity participation in older adults (Trost et al., 2002).
Only a few studies have attempted to incorporate more than one SCT construct into models predicting physical activity behavior. For example, Rovniak and colleagues (2002) found a longitudinal SCT model incorporating outcome expectations, self-efficacy, and self-regulation with social support acting as a moderator accounted for 55% of the variance in physical activity. In another study by Anderson, Winett, Wojcik, and Williams (2010), their SCT model testing the relationship of all model constructs (self-regulation, outcome expectations, and social support) to each other and physical activity explained 36% of the effect of an online intervention on physical activity behavior. Plotnikoff, Lippke, Courneya, Birkett, and Sigal (2008) tested the effect of baseline SCT variables on 6-month physical activity behavior using the paths specified by Bandura (2004) in individuals with type I and type II diabetes, independently. These models accounted for 14% and 9% of the variance in physical activity in type I and type II diabetes, respectively, and exhibited support for all the specified relationships except for the direct effect of baseline outcome expectations on 6-month physical activity.
The present study was designed to test the utility of Bandura’s (2004) social cognitive model for explaining physical activity behavior in a sample of community-dwelling middle-aged and older adults. We used an 18-month prospective panel design to determine whether changes in the model constructs were related over time. It was hypothesized that self-efficacy at baseline would be directly associated with more positive physical, social, and self-evaluative outcome expectations, enhanced goals, fewer disability limitations, and greater levels of physical activity and indirectly associated with physical activity level through these social cognitive constructs. It was also hypothesized that more positive outcome expectations would be directly associated with higher goals and physical activity participation, fewer disability limitations would be directly associated with higher goals and physical activity participation, and stronger goals would be directly associated with increases in physical activity. Additionally, we hypothesized that changes in self-efficacy over the 18-month period would be directly associated with changes in physical, social, and self-evaluative outcome expectations, disability limitations, goals, and physical activity and indirectly associated with changes in physical activity through changes in outcomes expectations, disability limitations, and goals. We also hypothesized that changes in outcome expectations would be directly associated with changes in goals and physical activity participation and that changes in disability limitations would be directly associated with changes in goals. Finally, we hypothesized that changes in goals would be directly associated with changes in physical activity.
METHODS
Participants and Recruitment
As previously reported (Wójcicki et al., 2009), 349 individuals were recruited to participate in the current study at baseline. Data were collected from an initial sample of 321 of those men and women (M age = 63.8 years) with 227 (70.7% of total sample) available for follow-up 18 months later. All study procedures were approved by a University Institutional Review Board, and each participant completed a written informed consent prior to study entry. Briefly, participants were required to be at least 50 years of age and were recruited via paper advertisements (e.g., fliers and community postings) and a mass E-mail solicitation to all university employees. Further study inclusion criteria, recruitment methods, and baseline characteristics have been reported elsewhere (Wójcicki et al., 2009). All individuals who participated in the study at baseline were contacted via the E-mail address or telephone number provided at baseline a minimum of two times for recruitment into the 18-month follow-up study. Reasons for attrition at follow-up included failure to respond to repeated recruitment efforts (n = 35; 10.9%), invalid contact information/change of address (n = 21; 6.5%), failed to return 18-month questionnaire packet (n = 14; 4.3%), no longer interested (n = 23; 7.2%), and deceased (n = 1; 0.3%). Baseline analyses comparing individuals who did not participate in the follow-up with those who did on all study variables were nonsignificant.
Measures
Demographics.—
A brief questionnaire assessed basic demographic information, including sex, race, education, and income.
Self-efficacy.—
The six-item Exercise Self-Efficacy Scale (McAuley, 1993) was used to assess participants’ beliefs in their ability to exercise five times per week, at moderate intensities, for 30 or more minutes per session at 2-week increments over the next 12-week period. This scale is scored on a 100-point percentage scale comprised 10-point increments, ranging from 0% (not at all confident) to 100% (highly confident). A total scale score is derived by summing the responses to each item and dividing by the total number of items in the scale. This measure has been used widely in the social cognitive literature in understanding physical activity (e.g., Duncan & McAuley, 1993; McAuley, Jerome, Elavsky, Marquez, & Ramsey, 2003). This scale demonstrated excellent internal consistency in this sample (α = .99).
Outcome expectations.—
The fifteen-item Multidimensional Outcome Expectation for Exercise Scale (Wójcicki et al., 2009) was used to assess participants’ social (four items), self-evaluative (five items), and physical (six items) outcome expectations for exercise. This scale instructs participants to indicate how strongly they agree with each statement on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). Responses from items on each scale are summed to provide a total subscale score (i.e., scale range from 4 to 20 for social outcome expectations; 5 to 25 for self-evaluative outcome expectations; and 6 to 30 for physical outcome expectations). This scale has been shown to be valid and demonstrates high internal consistency (Wójcicki et al., 2009). The internal consistency in this sample was high for the self-evaluative (α = .84), physical (α = .82), and social (α = .81) outcome expectation subscales.
Physical activity.—
The Physical Activity Scale for the Elderly (PASE; Washburn, Smith, Jette, & Janney, 1993) was used to assess physical activity. PASE is a 10-item instrument designed to assess physical activity levels in older adults over a 1-week time period. PASE assesses activity counts based upon the frequency, duration, and metabolic equivalent value of self-reported leisure, household, and occupational activity. PASE is a valid and reliable self-report measure frequently used to assess physical activity in older adults (Washburn & Ficker, 1999; Washburn, McAuley, Katula, Mihalko, & Boileau, 1999). Higher scores on the PASE reflect greater participation in physical activity.
Goals.—
Goals were assessed using a modified version of a four-item scale developed by Rise, Thompson, and Verplanken (2003). We modified it to be specific to leisure-time walking as this is the most common type of physical activity reported by middle-aged and older adults. Participates were asked to indicate the extent to which they agreed that they had made plans relative to “when,” “where,” “what,” and “how” they were going to engage in regular leisure-time walking over the next 2 months. Participants indicated their responses on a scale from 1 (strongly disagree) to 7 (strongly agree). Items responses were summed to achieve a total goals score ranging from 4 to 28. The internal consistency of this measure was high in the current sample (α = .96).
Impediments.—
We used the eight-item disability limitations subscale of the abbreviated Late Life Function and Disability Instrument (McAuley, Konopack, Motl, Rosengren, & Morris, 2005) as a potential barrier to physical activity participation in this sample. The measure is scored on a scale of 1 (completely limited) to 5 (not at all limited), with total scores ranging from 15 to 40 (higher scores reflect fewer limitations). This measure had good internal consistency in the present sample (α = .83).
Procedure
At baseline, participants were recruited through university E-mail lists and fliers posted around the community. At follow-up, participants were contacted via telephone or E-mail and asked if they would be interested in participating in a follow-up study. Study staff attempted to contact individuals to assess interest in participation a minimum of two times. If individuals were interested in participating, their contact information was verified and updated. All study materials, including two copies of an institutional review board–approved informed consent, were then sent to participants via the U.S. Postal Service. Participants were asked to complete and return all materials within a 2-week period. Up to three follow-up contacts were made to individuals failing to return study materials. Participants returning completed follow-up study materials were automatically entered into a lottery to win one of twenty $50.00 cash prizes.
Data Analysis
In order to examine the hypothesized relationships between self-efficacy, outcome expectations, goals, and physical activity, a panel analysis within a covariance modeling framework was conducted using Mplus v5.2 (Muthén & Muthén, 1998–2007). The panel model analysis allows the dynamics of relationship changes across time to be examined.
The full-information maximum likelihood (FIML) estimator was used as a result of the presence of missing data. The FIML estimator is well documented as an excellent approach to the analysis of missing data in structural equation modeling and has yielded accurate parameter estimates and fit indices with simulated missing data (Arbuckle, 1996; Enders, 2001; Enders & Bandalos, 2001). Preliminary analyses of the data were conducted to confirm the missing at random assumption, therefore justifying use of FIML estimation. The extent of missing data at baseline was physical outcome expectations (1.6%), self-evaluative outcome expectations (1.2%), social outcome expectations (1.2%), PASE (5.9%), disability limitations (0.6%), and goals (0.6%). There were no missing data at baseline for exercise self-efficacy. At 18-month follow-up, approximately 30% of the sample did not participate, and missing data for each construct was as follows: self-efficacy (29.3%), physical outcome expectations (29.3%), self-evaluative outcome expectations (29.3%), social outcome expectations (29.3%), PASE (30.5%), disability limitations (29.6%), and goals (29.6%). We chose to analyze the full sample as Graham (2009) has provided evidence that there is very little “fall off” in model estimates with up to 50% missing data.
Model specification and fit.—
All variables included in the model were manifest variables. The hypothesized model specified (a) a direct path from self-efficacy to physical outcome expectations, social outcome expectations, self-evaluative outcome expectations, disability limitations, and goals at baseline and 18 months; (b) direct paths from physical outcome expectations, self-evaluative outcome expectations, and social outcome expectations to both goals and physical activity at baseline and 18 months; (c) direct path from disability limitations to goals; and (d) direct path from self-efficacy to physical activity and indirect paths from self-efficacy to physical activity via physical outcome expectations, self-evaluative outcome expectations, social outcome expectations, disability limitations, and goals at baseline and 18 months. It was also hypothesized that the residuals of each type of outcome expectation (physical, social, and self-evaluative) would be correlated at both time points because they have been shown to be highly related (Wójcicki et al., 2009). Stability coefficients were also estimated (Kessler & Greenberg, 1981). These coefficients represent correlations between the same variables (e.g., PASE at baseline and 18 months) measured across time while controlling for the influence of other variables in the model. Overall, the stability coefficients were acceptable for self-efficacy (β = .51), physical outcome expectations (β = .50), self-evaluative outcome expectations (β = .62), social outcome expectations (β = .63), goals (β = .38), disability limitations (β = .49), and PASE (β = .45). These paths are not shown in subsequent figures for the sake of clarity. Finally, demographic factors were included as covariates in this model.
In summary, in the context of the hypothesized model, the analyses conducted allowed for a simultaneous examination of the hypothesized relationships at baseline and the hypothesized relationships among changes in model constructs across time when controlling for baseline associations, stability coefficients, and covariates.
Standard model fit indices were calculated including the chi-square goodness of fit, the root mean square error of approximation (RMSEA; Browne & Cudeck, 1993; Hu & Bentler, 1999), and the comparative fit index (CFI; Hu & Bentler, 1999). A nonsignificant chi-square, values greater than .95 for the CFI, and values of .08 or less for the RMSEA are indicative of a good model data fit (Hu & Bentler, 1999).
RESULTS
Participants
As previously reported (Wójcicki et al., 2009), the sample was 80.1% female and 88.7% White. More than half of the sample (58.1%) had at least a college degree, and 65.1% had an annual household income greater than $40,000.
Model Results
Descriptive statistics for all variables in the hypothesized model are displayed in Table 1. There were modest, but significant, increases in physical, self-evaluative, and social outcome expectations over the 18-month study period. Additionally, there was a significant decline in exercise self-efficacy and a nonsignificant decline in goals and disability limitations over the 18-month study period. The correlations of all the variables included in the model are shown in Table 2.
Table 1.
Descriptive Statistics of Model Variables at Baseline and 18 Months
| Variable | Baseline | 18 months | t |
| Self-efficacy | 65.84 (33.95) | 62.06 (34.81) | −2.71* |
| Physical outcome expectations | 26.38 (2.90) | 27.28 (2.65) | 4.14** |
| Self-evaluative outcome expectations | 21.30 (2.60) | 21.93 (2.64) | 3.60** |
| Social outcome expectations | 12.70 (2.71) | 13.32 (2.90) | 4.04** |
| Disability limitations | 37.02 (4.18) | 37.40 (3.91) | 1.43 |
| Goals | 21.39 (6.57) | 21.11 (6.60) | −1.49 |
| Physical activity | 148.68 (80.20) | 160.22 (79.29) | 0.78 |
Note. *p ≤ .05; **p ≤ .001.
Table 2.
Correlations Among Model Constructs
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
| m0 | ||||||||||||||
| 1. SE | 1.00 | |||||||||||||
| 2. PO | 0.22** | 1.00 | ||||||||||||
| 3. SEO | 0.26** | 0.74** | 1.00 | |||||||||||
| 4. SO | 0.17** | 0.32** | 0.44** | 1.00 | ||||||||||
| 5. Goals | 0.33** | 0.29** | 0.22** | 0.07 | 1.00 | |||||||||
| 6. DLIM | 0.28** | 0.20** | 0.09 | −0.05 | 0.25** | 1.00 | ||||||||
| 7. PA | 0.28** | 0.21** | 0.09 | −0.06 | 0.18** | 0.15 | 1.00 | |||||||
| m18 | ||||||||||||||
| 8. SE | 0.50** | 0.17* | 0.16* | 0.10 | 0.25** | 0.28** | 0.19** | 1.00 | ||||||
| 9. PO | 0.28** | 0.56** | 0.51** | 0.21** | 0.31** | 0.25** | 0.22** | 0.30** | 1.00 | |||||
| 10. SEO | 0.20 ** | 0.52** | 0.68** | 0.34** | 0.24** | 0.18** | 0.17* | 0.22** | 0.69** | 1.00 | ||||
| 11. SO | 0.20** | 0.27** | 0.42** | 0.65** | 0.10 | −0.03 | −0.01 | 0.19** | 0.33** | 0.43** | 1.00 | |||
| 12. Goals | 0.23** | 0.22** | 0.21** | 0.17* | 0.45** | 0.14* | 0.08 | 0.34** | 0.29** | 0.25** | 0.24** | 1.00 | ||
| 13. DLIM | 0.15* | 0.15* | 0.05 | 0.04 | 0.11 | 0.51** | 0.03 | 0.25** | 0.13* | 0.08 | 0.10 | 0.10 | 1.00 | |
| 14. PA | 0.33** | 0.30** | 0.20** | 0.10 | 0.15* | 0.21** | 0.52** | 0.33** | 0.33** | 0.25** | 0.19** | 0.18** | 0.09 |
Notes. DLIM = disability limitations; PA = physical activity; PO = physical outcome expectations; SE = self-efficacy; SEO = self-evaluative outcome expectations; SO = social outcome expectations.
*p < .05; **p < .001.
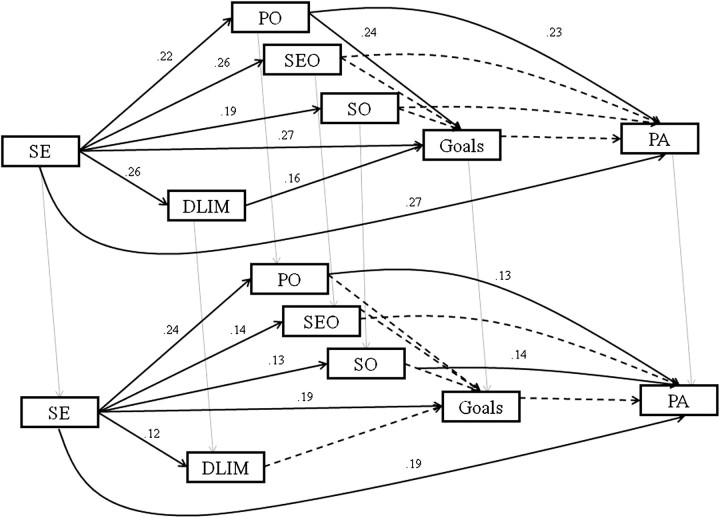
The panel model analyzing the relationships shown in Figure 1 provided an excellent overall fit to the data (χ2 = 86.24, df = 55, p = .00, RMSEA [90% confidence interval] = .04 [.02–.06], CFI = .98) At baseline, the direct paths from self-efficacy to physical, self-evaluative and social outcome expectations, disability limitations, goals, and physical activity were all significant (p ≤ .05) such that more efficacious individuals had higher physical outcome expectations (β = .22), self-evaluative outcome expectations (β = .26), social outcome expectations (β = .19), goals (β = .27), fewer disability limitations (β = .26), and participated in greater levels of physical activity (β = .27). Self-efficacy also indirectly influenced physical activity participation via physical outcome expectations and social outcome expectations. Physical outcome expectations were directly related to physical activity participation such that greater physical activity participation was associated with higher physical outcome expectations (β = .23). Physical outcome expectations and disability limitations were directly associated with goals with more positive physical outcome expectations (β = .24), and fewer disability limitations (β = .16) associated with stronger goals at baseline. The direct path from goals to physical activity was not significant.
Figure 1.
Social cognitive theory of physical activity in older adults. Note: SE = self-efficacy, PA = physical activity, PO = physical outcome expectations, SEO = self-evaluative outcome expectations, SO = social outcome expectations, DLIM = disability limitations.
At 18 months, changes in self-efficacy were associated with residual changes in physical outcome expectations (β = .24), self-evaluative outcome expectations (β = .14), social outcome expectations (β = .13), disability limitations (β = .12), goals (β = .19), and physical activity (β = .19). The only significant indirect relationship between changes in self-efficacy and changes in physical activity was through changes in physical outcome expectations. Changes in physical outcome expectations (β = .13) and changes in social outcome expectations (β = .14) were also directly related to changes in physical activity levels. Changes in outcome expectations and changes in disability limitations were not associated with changes in goals at follow-up. The overall model accounted for 17.0% and 40.0% of the variance in physical activity at baseline and follow-up, respectively.
In terms of the relationships among model constructs and the demographic factors, a few interesting relationships emerged. At baseline, older adults had significantly higher social outcome expectations (β = .27) and lower physical activity levels (β = −.18). Males reported higher social outcome expectations (β = .11) and more disability limitations (β = −.12) than females, and individuals with a greater income reported fewer disability limitations (β = .19). At 18 months, females reported a greater increase in physical outcome expectations (β = −.12), and older age was associated with fewer disability limitations (β =.14) and a decline in physical activity (β =−.24).
DISCUSSION
In this study, we report findings from an 18-month prospective examination of a social cognitive model for explaining physical activity behavior in a sample of community-dwelling middle-aged and older adults. This model was designed to test the relationships hypothesized by Bandura (2004) and proposed that self-efficacy both directly and indirectly, via disability limitations, goals, and outcome expectations, influences physical activity behavior. The test of this model controlled for baseline associations, stability of measures over time, and demographic variables and resulted in a good model data fit.
Our findings show that more efficacious middle-aged and older adults participated in greater levels of physical activity, have fewer disability limitations that could impede their ability to participate in physical activity, set higher goals, and had higher physical, social, and self-evaluative outcome expectations at baseline. Additionally, changes in self-efficacy over an 18-month period were associated with changes in physical activity, goals, disability limitations, and physical, social, and self-evaluative outcome expectations. At baseline, self-efficacy was also found to indirectly influence physical activity participation via physical outcome expectations, whereas changes in self-efficacy across the study period were shown to indirectly influence changes in physical activity via physical outcome expectations and social outcome expectations. Hence, our findings also provide some support for the fact that outcome expectations may differentially influence changes in physical activity participation across time, independent of self-efficacy. These results collectively provide initial support for a social cognitive model of physical activity behavior in community-dwelling middle-aged and older adults utilizing the pathways specified by Bandura (2004). Unfortunately, however, our model did not provide support for a direct relationship between goals and physical activity or for the role of goals as a mediator between physical activity and self-efficacy alone or via outcome expectations or impediments to physical activity. However, it did provide some support for the role of goals as a mediator between self-efficacy and disability limitations, a commonly experienced barrier to physical activity participation in older adults at baseline but not across time.
Self-efficacy was the strongest predictor of physical activity behavior in this model providing further support for the direct relationship between self-efficacy and physical activity levels across time in middle-aged and older adults. Additionally, the findings from this study provide support for the often neglected indirect relationship of self-efficacy with physical activity via outcome expectations and barriers to physical activity participation. Interestingly, physical outcome expectations were directly related to physical activity participation at baseline, but both changes in physical outcome expectations and changes in social outcome expectations were related to changes in physical activity at follow-up. Self-evaluative outcome expectations did not show any relationship with physical activity participation. We do not interpret these findings to mean self-evaluative outcome expectations are not important. Rather, it may just suggest that physical and social outcome expectations become more salient and important as individuals age. This is not surprising given that the need to maintain independence is more relevant as one enters later life and may be viewed as more of a key motivating factor influencing physical activity participation. Additionally, higher levels of social support have demonstrated a relationship with greater levels of physical activity participation. Thus, higher levels of social outcome expectations may be reflective of greater levels of social support for exercise.
Our null findings relative to the direct relationship between physical activity and goals may be surprising, given the literature that suggests that individuals who set higher physical activity goals tend to have greater increases in physical activity levels and adhere better to structured physical activity programs (Bravata et al., 2007; Dishman et al., 2009). Thus, we are cautious in interpretation of these findings as we do not want to imply that goals are not important in understanding physical activity behavior. Rather, we believe that the nonsignificant relationship in this study could be a function of a number of factors. First, we used a relatively crude measure of goals, which could attenuate the relationship between goals and physical activity. This measure simply asked individuals to indicate whether they had made plans as to when, where, what, and how they were going to exercise over the next 2 months. The level of specificity of these goals was not evaluated. Thus, this measure may not have fully captured how effectively these individuals were in setting goals, further limiting its utility. Second, this measure was specific to leisure-time walking. Although walking is one of the most common physical activities in which middle-aged and older adults engage, some study participants may have participated in other forms of exercise. As such, they may not have found the items on this measure to be particularly relevant to their exercise goals. In addition, it is quite conceivable that some participants’ goals for physical activity might have a social basis to them, and our measure did not capture such goals. Furthermore, this was a prospective study. We did not intervene or instruct individuals to set goals. As a result, these findings may highlight that in order to see significant relationships between goals and physical activity participation, it may be necessary to (a) design measures that assess effectiveness and frequency of goal setting and (b) intervene at some level in order to assist individuals in setting effective goals.
These findings have important implications for understanding physical activity behavior and designing effective physical activity behavior change interventions. All the constructs included in the present model (self-efficacy, outcome expectations, disability limitations, and goals) are modifiable, suggesting that they could, and should, be targeted in interventions. Self-efficacy was demonstrated to be the strongest predictor of physical activity behavior in this model, suggesting that designing interventions that target the four sources of efficacy (i.e., mastery and vicarious experiences, social persuasion, and interpretation of physiological and psychological states) may be extremely important in order to see increases in physical activity. Interestingly, although there was significant variation, mean level self-efficacy decreased over time. This is not entirely surprising as there is evidence from several randomized controlled physical activity trials to suggest that, even in the presence of an exercise program, efficacy declines. This is likely due to overestimates of efficacy at baseline and that participants “recalibrate” after a few weeks of exposure to the program (McAuley et al., 2011).
Although self-efficacy appears to have a strong influence on physical activity participation, our findings suggest that it is not the only construct that should be targeted. Physical outcome expectations also seem to be important predictors of physical activity across time. They may serve as important motivating factors, and thus, interventions should be designed to educate individuals about realistic outcome expectations. Although goals were not found to be significantly related to physical activity participation in this sample, physical activity interventions may benefit from effective goal setting lessons. Finally, the effect of perceived disability limitation as a barrier to physical activity could be reduced by enhancing individual’s efficacy or providing them with exercises specifically designed to target functional limitations and disability. In addition to targeting disability limitations, several other facilitators or impediments such as social support, disease symptoms, or fatigue could be included as targets in program design. To enhance participants’ ability to overcome their barriers to physical activity, individual plans of action could be developed and social support could be incorporated into intervention and program design to further increase physical activity participation. Although self-efficacy is one of the strongest predictors of physical activity, it is important to recognize that it does not exert its influence in isolation. Developing a better understanding of the other social cognitive constructs and incorporating them into the design of physical activity interventions may not only increase the adoption of physical activity but could also increase the long-term maintenance of physical activity if targeted properly. Moreover, if programs and interventions are able to effectively apply SCT to change and maintain physical activity behavior, considerable public health benefits could occur in terms of disease prevention and control.
These data provide partial support for the social cognitive model for physical activity proposed by Bandura (2004). Additionally, these finding suggest that, although self-efficacy is a strong predictor of physical activity behavior, other social cognitive constructs, particularly outcome expectations, appear to significantly contribute to physical activity behavior in middle-aged and older adults. As one of the first studies to test a more comprehensive social cognitive model of physical activity in community-dwelling middle-aged and older adults, a population at high risk for inactivity, we believe that our findings are promising. However, our study is not without limitations. First, we used a relatively crude measure of goals that may limit interpretation of our findings regarding the role of goals in the SCT model for physical activity. Second, we used manifest self-report measures of all variables. Utilizing multiple indicators of each model construct would allow for a more comprehensive latent variable social cognitive model to be tested. Additionally, although age was only significantly associated with social outcome expectations and physical activity, our study sample did consist of a wide age range of individuals. Future studies should examine whether these relationships hold in separate samples of middle-aged and older adults. Finally, it may be particularly valuable to use an objective measure of physical activity to determine how these relationships hold as the current study only used a self-report measure of physical activity that may be subject to overreporting of physical activity participation.
To the best of our knowledge, this is one of the few studies to test the pathways proposed by Bandura’s (2004) social cognitive model to explain physical activity behavior in middle-aged and older adults. Our findings support both direct and indirect relationships between self-efficacy and physical activity. Future studies should attempt to replicate this model in middle-aged and older adults and other populations in order to understand whether the SCT model holds when applied to physical activity in other populations as well as to better understand the relationship of outcome expectations, facilitators and impediments, and goals to physical activity participation across time and as a result of intervention. Findings from such research could be applied to program design and implementation at multiple levels (e.g., individual, community, organizational), which could ultimately increase physical activity participation and reduce the risk and burden of disease, especially in older adults and other high-risk populations.
Funding
This work was supported by a Shahid and Ann Carlson Khan endowed professorship awarded to Edward McAuley. S. M. White is supported by Award Number F31AG034025 from the National Institute on Aging.
References
- Anderson ES, Winett RA, Wojcik JR, Williams DM. Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: Social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. Journal of Health Psychology. 2010;15:21–32. doi: 10.1177/1359105309342297. doi:10.1177/1359105309342297. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and techniques. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. pp. 243–278. [Google Scholar]
- Bandura A. The explanatory and predictive scope of self-efficacy theory. Journal of Social and Clinical Psychology. 1986;4:359–373. doi:10.1521/jscp.1986.4.3.359. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W.H. Freeman and Company; 1997. [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. In: Norman P, Abraham C, Conner M, editors. Understanding and changing health behaviour. Reading, UK: Harwood; 2000. pp. 299–339. [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–164. doi: 10.1177/1090198104263660. doi:10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, Sirard JR. Using pedometers to increase physical activity and improve health: A systematic review. Journal of the American Medical Association. 2007;298:2296–2304. doi: 10.1001/jama.298.19.2296. doi:10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- Brown DW, Balluz LS, Heath GW, Moriarty DG, Ford ES, Giles WH, Mokdad AH. Associations between recommended levels of physical activity and health-related quality of life. Findings from the 2001 Behavioral Risk Factor Surveillance System (BRFSS) survey. Preventive Medicine. 2003;37:520–528. doi: 10.1016/s0091-7435(03)00179-8. doi:10.1016/S0091-7435(03)00179-8. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Dishman RK, Motl RW, Saunders R, Felton G, Ward DS, Dowda M, Pate RR. Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Preventive Medicine. 2004;38:628–636. doi: 10.1016/j.ypmed.2003.12.007. doi:10.1016/j.ypmed.2003.12.007. [DOI] [PubMed] [Google Scholar]
- Dishman RK, Vandenberg RJ, Motl RW, Wilson MG, DeJoy DM. Dose relations between goal setting, theory-based correlates of goal setting and increases in physical activity during a workplace trial. Health Education Research. 2009;25:620–631. doi: 10.1093/her/cyp042. doi:10.1093/her/cyp042. [DOI] [PubMed] [Google Scholar]
- Duncan TE, McAuley E. Social support and efficacy cognitions in exercise adherence: A latent growth curve analysis. Journal of Behavioral Medicine. 1993;16:199–218. doi: 10.1007/BF00844893. doi:10.1007/BF00844893. [DOI] [PubMed] [Google Scholar]
- Enders CK. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychological Methods. 2001;6:352–370. doi:10.1037/1082-989X.6.4.352. [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. doi:10.1207/S15328007SEM0803_5. [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. doi:10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi:10.1080/10705519909540118. [Google Scholar]
- Kessler RC, Greenberg DF. Linear panel analysis: Models of quantitative change. New York: Academic; 1981. [Google Scholar]
- McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. Journal of Behavioral Medicine. 1993;16:103–113. doi: 10.1007/BF00844757. doi:10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exercise and Sport Science Reviews. 2000;28:85–88. [PubMed] [Google Scholar]
- McAuley E, Jerome GJ, Elavsky S, Marquez DX, Ramsey SN. Predicting long-term maintenance of physical activity in older adults. Preventive Medicine. 2003;37:110–118. doi: 10.1016/s0091-7435(03)00089-6. doi:10.1016/S0091-7435(03)00089-6. [DOI] [PubMed] [Google Scholar]
- McAuley E, Konopack JF, Motl RW, Rosengren K, Morris KS. Measuring disability and function in older women: Psychometric properties of the late-life function and disability instrument. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 2005;60:901–909. doi: 10.1093/gerona/60.7.901. doi:10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- McAuley E, Mailey EL, Mullen SP, Szabo AN, Wójcicki TR, White SM, Kramer AF. Growth trajectories of exercise self-efficacy in older adults: Influence of measures and initial status. Health Psychology. 2011;30:75–83. doi: 10.1037/a0021567. doi:10.1037/a0021567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E, Motl RW, Morris KS, Hu L, Doerksen SE, Elavsky S, Konopack JF. Enhancing physical activity adherence and well-being in multiple sclerosis: A randomised controlled trial. Multiple Sclerosis. 2007;13:652–659. doi: 10.1177/1352458506072188. doi:10.1177/1352458506072188. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus (version 5.0) Los Angeles, CA: Author; 1998–2007. [Google Scholar]
- Netz Y, Wu MJ, Becker BJ, Tenenbaum G. Physical activity and psychological well-being in advanced age: A meta-analysis of intervention studies. Psychology and Aging. 2005;20:272–284. doi: 10.1037/0882-7974.20.2.272. doi:10.1037/0882-7974.20.2.272. [DOI] [PubMed] [Google Scholar]
- Nothwehr F, Yang J. Goal setting frequency and the use of behavioral strategies related to diet and physical activity. Health Education Research. 2007;22:532–538. doi: 10.1093/her/cyl117. doi:10.1093/her/cyl117. [DOI] [PubMed] [Google Scholar]
- Plotnikoff RC, Lippke S, Courneya KS, Birkett N, Sigal RJ. Physical activity and social cognitive theory: A test in a population sample of adults with type 1 or type 2 diabetes. Applied Psychology. 2008;57:628–643. doi:10.1111/j.1464-0597.2008.00344.x. [Google Scholar]
- Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 2001;56:23–35. doi: 10.1093/gerona/56.suppl_2.23. doi:10.1093/gerona/56.suppl_2.23. [DOI] [PubMed] [Google Scholar]
- Rise J, Thompson M, Verplanken B. Measuring implementation intentions in the context of the theory of planned behavior. Scandinavian Journal of Psychology. 2003;44:87–95. doi: 10.1111/1467-9450.00325. doi:10.1111/1467-9450.00325. [DOI] [PubMed] [Google Scholar]
- Rogers LQ, McAuley E, Courneya KS, Verhulst SJ. Correlates of physical activity self-efficacy among breast cancer survivors. American Journal of Health Behavior. 2008;32:594–603. doi: 10.5555/ajhb.2008.32.6.594. [DOI] [PubMed] [Google Scholar]
- Rovniak LS, Anderson ES, Winett RA, Stephens RS. Social cognitive determinants of physical activity in young adults: A prospective structural equation analysis. Annals of Behavioral Medicine. 2002;24:149–156. doi: 10.1207/S15324796ABM2402_12. doi:10.1207/S15324796ABM2402_12. [DOI] [PubMed] [Google Scholar]
- Son JS, Kerstetter DL, Mowen AJ, Payne LL. Global self-regulation and outcome expectations: Influences on constraint self-regulation and physical activity. Journal of Aging and Physical Activity. 2009;17:307–326. doi: 10.1123/japa.17.3.307. [DOI] [PubMed] [Google Scholar]
- Steele BG, Holt L, Belza B, Ferris S, Lakshminaryan S, Buchner DM. Quantitating physical activity in COPD using a triaxial accelerometer. Chest. 2000;117:1359–1367. doi: 10.1378/chest.117.5.1359. doi:10.1378/chest.117.5.1359. [DOI] [PubMed] [Google Scholar]
- Stewart A, King A. Evaluating the efficacy of physical activity for influencing quality of life outcomes in older adults. Annals of Behavioral Medicine. 1991;13:108–116. [Google Scholar]
- Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: Review and update. Medicine & Science in Sports & Exercise. 2002;34:1996–2002. doi: 10.1097/00005768-200212000-00020. doi:10.1249/01.MSS.0000038974.76900.92. [DOI] [PubMed] [Google Scholar]
- Umstattd MR, Hallam J. Older adults’ exercise behavior: Roles of selected constructs of social-cognitive theory. Journal of Aging and Physical Activity. 2007;15:206–218. doi: 10.1123/japa.15.2.206. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau, Population Division. Table 2. Projections of the population. 2008. Retrieved from http://www.census.gov/population/www/projections/summarytables.html. [Google Scholar]
- U.S. Department of Health and Human Service, Centers for Disease Control and Prevention. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. 2009. DHHS Publication No. (PHS) 2011-1577 Retrieved from http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [Google Scholar]
- Washburn RA, Ficker JL. Physical Activity Scale for the Elderly (PASE): The relationship with activity measured by a portable accelerometer. Journal of Sports Medicine and Physical Fitness. 1999;39:336–340. [PubMed] [Google Scholar]
- Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): Evidence for validity. Journal of Clinical Epidemiology. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. doi:10.1016/S0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): Development and evaluation. Journal of Clinical Epidemiology. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. doi:10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- Williams DM, Anderson ES, Winett RA. A review of the outcome expectancy construct in physical activity research. Annals of Behavioral Medicine. 2005;29:70–79. doi: 10.1207/s15324796abm2901_10. doi:10.1207/s15324796abm2901_10. [DOI] [PubMed] [Google Scholar]
- Wójcicki TR, White SM, McAuley E. Assessing outcome expectations in older adults: The Multidimensional Outcome Expectations for Exercise Scale (MOEES) The Journals of Gerontology, Series B: Psychological Science and Social Sciences. 2009;64:33–40. doi: 10.1093/geronb/gbn032. doi:10.1093/geronb/gbn032. [DOI] [PMC free article] [PubMed] [Google Scholar]