Abstract
Objective:
Neither the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-III-R), nor the DSM-IV uses measures of substance consumption as part of the diagnostic criteria for substance use disorders. Therefore, this report examined the extent to which frequency and/or quantity of consumption across a broad spectrum of substances are associated with DSM-IV diagnoses of specific substance use disorders and whether there are informative hierarchical levels of consumption among users, abusers, and those who are substance dependent in the U.S. general population.
Method:
The analyses focused on consumption data from respondents of the 2001–2002 National Epidemiologic Survey of Alcohol and Related Disorders. Multinomial logistic regression was used to predict DSM-IV diagnoses of dependence or abuse based on the continuous consumption measures.
Results:
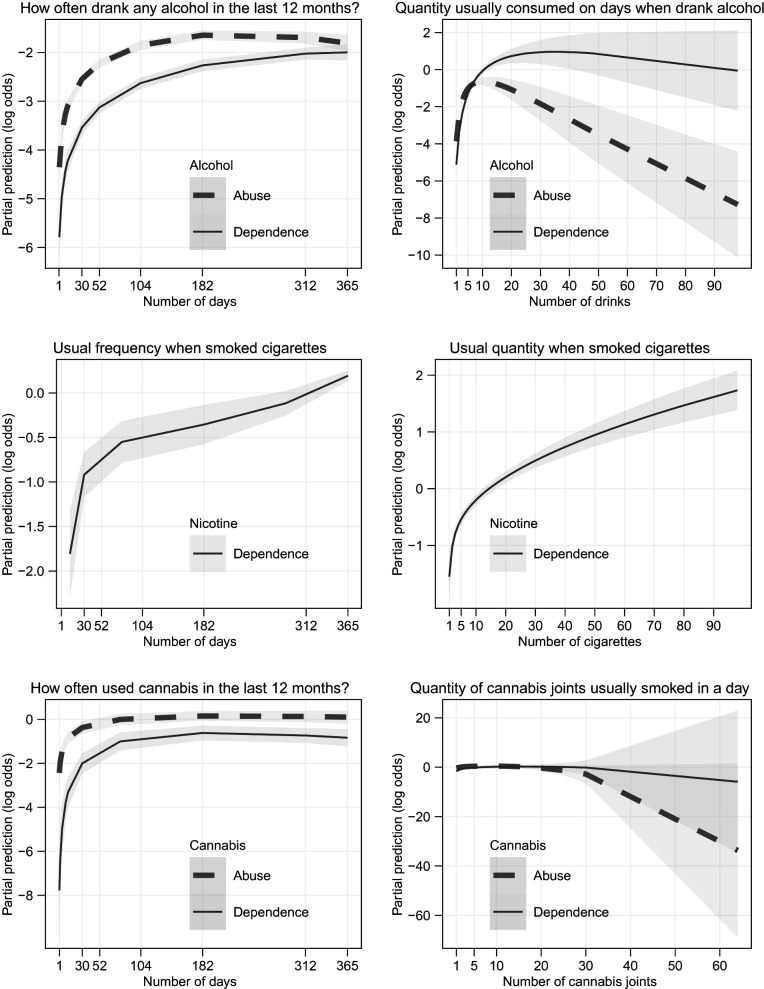
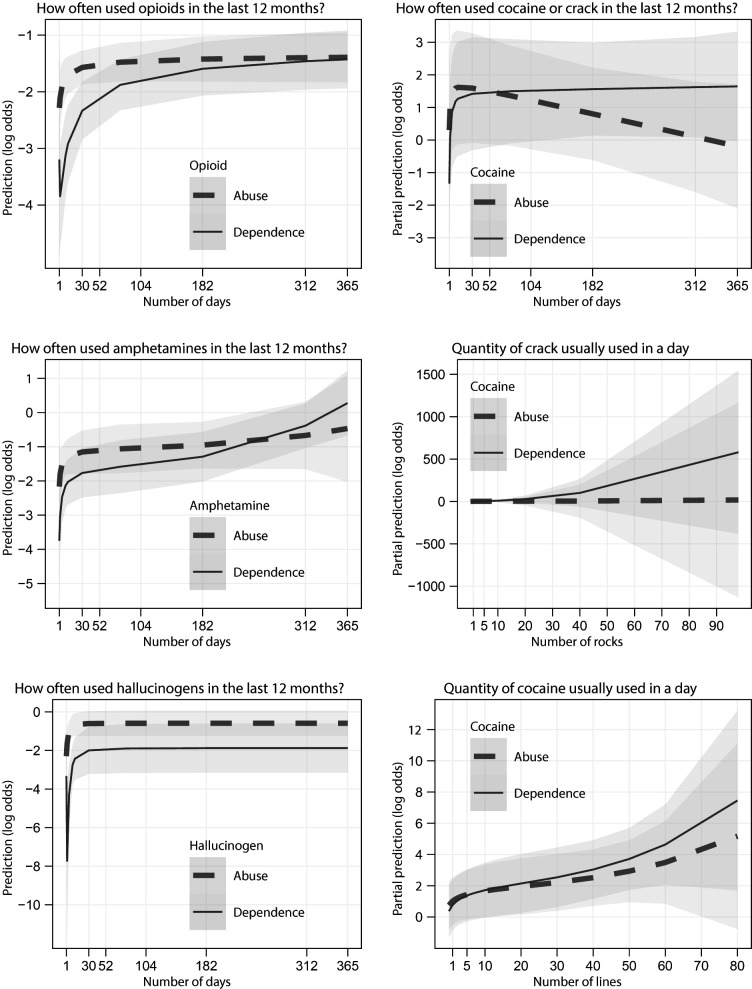
Among individuals who used substances, the substances with the greatest liability for dependence were nicotine first and cocaine second. For nearly all substances investigated, users without specific substance use disorders demonstrated lower levels of quantity and frequency of consumption relative to those with DSM-IV abuse and dependence disorders. Dose-response curves for the log odds of abuse and dependence suggested unidimensionality of abuse and dependence for frequency of alcohol drinking; frequency of cannabis use; frequency of opioid use; frequency of hallucinogen use; and, to a lesser extent, frequency of amphetamine use. However, the dose-response curves for the quantity of alcohol consumed demonstrated differential patterns for abuse and dependence such that alcohol dependence has a distinctly greater “quantity of use” relationship than that found among alcohol abusing individuals.
Conclusions:
These results confirm the findings of others concerning the unidimensionality of abuse and dependence diagnoses when consumption variables alone are examined and suggest that consumption measures may be useful metrics gauging severity.
Neither the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994), nor the draft version of DSM-5 (American Psychiatric Association, 2011) includes a consumption-level diagnostic criterion for a substance use disorder (SUD), although it seems obvious that the sine qua non for these conditions is a heightened consumption of the specific drug of abuse. In fact, few data are available relating the level of use of most substances of abuse (except alcohol) to the risk for a DSM-IV diagnosis for an SUD. A substantial literature supports the observation that the level of alcohol consumed by an individual is proximally associated with the risk for the development of alcohol use disorders, as well as the risk for a host of associated adverse biomedical consequences (Corrao et al., 2004; Dawson et al., 2005; Gmel and Rehm, 2003; Li et al., 2007). Public health thresholds for low, moderate, and hazardous levels of alcohol consumption have been established by the World Health Organization (2000), and they include a definition of “high risk” drinking based on the determination that a man who exceeds a daily consumption limit of 60 g of alcohol or a woman who exceeds a daily consumption limit of 40 g of alcohol has significantly elevated risks for all-cause mortality (Holman and English, 1995). Epidemiologic studies of alcohol intake have demonstrated that exceeding these daily consumption limits also increases the risk of mortality, morbidity (including injuries), and other problems including drunk driving and social harms (Rehm et al., 1999). The U.S. Department of Agriculture's (2010) Dietary Guidelines for Americans defined moderate alcohol consumption as the consumption of up to one drink per day for women and up to two drinks per day for men. Heavy or high-risk drinking is the consumption of more than 3 drinks on any day or more than 7 drinks per week for women and more than 4 drinks on any day or more than 14 drinks per week for men. One U.S. “standard” drink is defined as containing 0.6 fl. oz. of pure alcohol, which is equivalent to 12 fl. oz. of regular beer (5% alcohol), 5 fl. oz. of wine (12% alcohol), or 1.5 fl. oz. of 80 proof (40% alcohol) distilled spirits.
However, similar consumption-level data for illicit drugs are rarely examined within the context of risk for an SUD diagnosis, based in part on the assumption that for illicit drugs any use is misuse. Furthermore, unlike for alcohol, it is difficult in practice to define “standard” drug use measures because illicit drugs are frequently adulterated, and users tend to titrate their dose based on their desired subjective effects. In this report, we examine the extent to which frequency and/or quantity of consumption across a broad spectrum of substances are associated with DSM-IV diagnoses of specific SUDs and whether there are informative hierarchical levels of consumption among users, abusers, and those who are substance dependent in the U.S. general population.
Method
Sample
These analyses used data from the 2001-2002 National Epidemiological Survey on Alcohol and Related Conditions (NESARC), conducted by the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. As described elsewhere (Grant et al., 2004), the NESARC sample represents the civilian, noninstitutionalized adult population of the United States, from all 50 states and the District of Columbia. It includes persons living in households; military personnel living off base; and residents of boarding or rooming houses, nontransient hotels and motels, shelters, college quarters, and group homes. The Census Supplementary Survey, in combination with the Census 2000 Group Quarters Inventory, comprised the sampling frame for the NESARC. The NESARC oversampled African Americans, Hispanics, and young adults 18-24 years of age to ensure adequate sample size for minority subgroups and high-risk populations. A single sample adult age 18 years or older was randomly selected for interview from each sample household. Personal interviews were conducted in respondents' homes. The overall response rate was 81% (n = 43,093). The analyses herein are based on subsamples of respondents who reported use of seven substances in the past year (i.e., 12 months preceding the interview). The sample size varies by substance: 26,946 reported alcohol use; 9,913, cigarette use; 686, opioid use; 1,603, cannabis use; 186, amphetamine use; 217, cocaine or crack use; and 194, hallucinogen use. The numbers of respondents used in estimating frequency and quantity of substance use were slightly reduced because of missing data on these measures. Respondents who did not report use of any of these substances were not included in the analysis.
Measures
DSM-IV substance abuse and dependence diagnosis.
The presence of substance abuse and dependence was defined in accordance with the criteria established by the DSM-IV using the items from the Alcohol Use Disorders and Associated Disabilities Interview Schedule-DSM-IV version (AUDADIS-IV; Grant et al., 2003). The AUDADIS-IV is a fully structured diagnostic interview instrument that comprises modules to assess major mood and anxiety disorders, personality disorders, alcohol and drug use disorders, and family history of alcohol and drug use disorders. It also measures the frequency and quantity of substance use. DSM-IV diagnostic criteria for substance abuse and dependence are derived from multiple AUDADIS-IV question items. We used the four substance-specific past-year criteria for substance abuse from the DSM-IV. These were (a) recurrent use resulting in a pattern of failure to fulfill role obligations, (b) recurrent use in situations that are physically hazardous, (c) recurrent substance-related legal problems, and (d) continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance. We also used the seven substance-dependence criteria with a cutoff of three of the seven for a dependence diagnosis in accordance with the DSM-IV. Briefly, these criteria are (a) persistent desires or unsuccessful attempts to reduce or stop substance use (quit/ control), (b) using larger amounts or longer than intended (larger/longer), (c) tolerance, (d) withdrawal, (e) continued use despite physical or psychological problems caused by the substance (physical/psychological problems), (f) much time spent using or recovering from using (time spent), and (g) reduction or cessation of important activities in order to use the substance (activities given up).
Quantity and frequency measures of level of consumption.
For alcohol and many other drugs, the AUDADIS-IV also contains a comprehensive set of questions that monitor the respondent's specific substance consumption during usual and heaviest using periods. In our analyses, the consumption level was based on data reported for the usual using period during the past year. The consumption questions ask respondents about their frequency of use and the quantity consumed on the day the substance was used. The quantity data are generally in a continuous format (e.g., number of drinks or number of cigarettes), whereas the frequency data were collected in ordinal categories (e.g., every day, nearly every day, 3-4 times a week, two times a week, once a week, 2-3 times a month, once a month, 7-11 times in the last year, 3-6 times in the last year, and 1-2 times in the last year). For our analyses, the frequency data were converted to continuous variables, taking the midpoint value of each category. Although frequency data were available for all substances, quantity data were not collected in the AUDADIS-IV for opioids, amphetamines, and hallucinogens.
Analyses
Analyses were conducted on the samples of respondents who reported past-year use of specific substances using the statistical software Stata (StataCorp LP, College Station, TX). The mean and percentage estimates and their 95% confidence intervals were produced by the survey procedures that incorporate the sampling weight and adjust variance estimates for the complex multistage sample design of NESARC based on the Taylor series linearization method. All comparisons within each substance were made among three categories of the DSM-IV SUD status: substance use without a diagnosis (referred to as “users” or “no diagnosis”), abuse, and dependence. The percentage distribution of the three categories was presented along with their demographic characteristics (mean age and percentage male) for each substance. Mean estimates pertaining to frequency and quantity of past-year use of specific substances were compared across the three categories. Furthermore, multinomial logistic regression was used to predict DSM-IV diagnoses of dependence or abuse by the consumption measures. When both quantity and frequency of use were available for a specific substance group, both measures were included in the model as predictors. To characterize continuous dose-response relationships more flexibly, each use measure was transformed into fractional polynomials of degree 2, which are an extension of polynomials of degree 2 that allows for two integer/fractional powers, viz., F (x; p) = β0 + β1xp1 + β2xp2 with powers p = (p1, p2) and parameters β0, β1, β2. The multivariate fractional polynomial procedure developed by Royston and Sauerbrei (2008) was used to select the powers p1 and p2 from a predefined set of powers = {-2, -1, -0.5, 0, 0.5, 1, 2, 3}. It has been shown that combinations of power transformations of continuous predictors are capable of producing a wide range of curve shapes for modeling continuous functions encountered in health and other fields of science (Royston and Sauerbrei, 2008).
Given the clinical implications for prevention and intervention, we believe that correctly specifying the functional forms of the continuous consumption measures outweighs the convenience of assuming a linear dose-response relationship, as is traditionally done in linear regression. For better visualization, the predicted log odds and the associated 95% confidence intervals generated from the multinomial logit models are presented in graphs. Partial predictions are shown when quantity and frequency measures were mutually adjusted in the model. Although larger substance consumption was expected to be associated with greater risk for developing abuse and dependence, the risk may not always increase monotonically. If a dose-response curve is nonlinear, it is more likely that the speed of increase varies according to the magnitude of substance consumption. It is also possible that a threshold effect, as opposed to a dose-response effect, is more appropriate in certain ranges of substance consumption. The initial and subsequent slopes, as well as the location of the inflection point (i.e., the point at which the slope changes its sign), convey information on the cutoffs where substance consumption might appear to be comparatively safe or hazardous with respect to risks for abuse or dependence. In addition, the extent to which dose-response curves for abuse and dependence interact with or differ from each other could signal whether their relationships reflect dual dimensionality in terms of susceptibility and severity. Multinomial logistic regression does not make the assumption that no diagnoses, abuse, and dependence are ordinal. However, if the dose-response curves for abuse and dependence are largely parallel, the pattern means that the odds are proportional across a wide range of the consumption continuum, and it can be viewed as an indication that abuse and dependence lie in the same dimension.
Results
Table 1 displays demographic characteristics (percentage male and mean age) of individuals who reported past-year use of specific substance by their respective DSM-IV SUD status. It is noteworthy that 87% of the individuals who reported past-year alcohol use had no alcohol-related diagnosis, whereas 5.8% met diagnostic criteria for dependence. As for those who reported past-year opioid use, 6.3% met criteria for dependence. The liability for dependence associated with the use of cocaine is even higher, with nearly 24% of those who reported cocaine use meeting diagnostic criteria for cocaine dependence. Even more significant from a risk perspective is that 49% of those who reported cigarette use met diagnostic criteria for nicotine dependence. (DSM-IV contains only a dependence diagnosis for nicotine; there is no nicotine abuse diagnosis). Thus, the substances used with the greatest liability for dependence were nicotine first and cocaine second. Those who used hallucinogens were among the lowest risk group for a dependence syndrome, with only 2.7% achieving a dependence diagnosis.
Table 1.
Percentage distribution, percentage male, and mean age among individuals with past-year use of specific substance by their respective Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), substance use disorder status
| Past-year specific substance use | Respective DSM-IV Substance Use Disorder Status |
Total | ||
| No diagnosis | Abuse | Dependence | ||
| Alcohol use (n = 26,946) | ||||
| Row % | 87.1 [86.6, 87.6] | 7.1 [6.7, 7.5] | 5.8 [5.5, 6.2] | 100 |
| % Male | 50.0 [49.3, 50.8] | 71.4 [68.9, 73.8] | 68.2 [65.2, 71.0] | 52.6 [51.9,53.3] |
| Mean age (years) | 43.8 [43.6,44.1] | 37.4 [36.7, 38.1] | 31.5 [30.8, 32.2] | 42.7 [42.4, 42.9] |
| Cigarette use (n = 9,913) | ||||
| Row % | 50.8 [49.6, 52.0] | N.A. | 49.2 [48.0, 50.4] | 100 |
| % Male | 56.9 [55.2, 58.6] | N.A. | 50.3 [48.6,52.1] | 53.7 [52.5, 54.9] |
| Mean age (years) | 41.7 [41.2,42.2] | N.A. | 39.6 [39.1,40.1] | 40.7 [40.3,41.0] |
| Opioid use (n = 686) | ||||
| Row % | 80.4 [76.3,83.9] | 13.3 [10.4,16.9] | 6.3 [4.3,9.2] | 100 |
| % Male | 54.2 [48.8, 59.4] | 65.7 [52.5, 76.9] | 62.9 [44.7,78.1] | 56.2 [51.4,60.9] |
| Mean age (years) | 34.1 [32.7, 35.4] | 34.4 [30.9, 37.9] | 35.6 [30.6, 40.6] | 34.2 [33.0, 35.4] |
| Cannabis use (n = 1,603) | ||||
| Row % | 64.4 [61.4, 67.2] | 27.7 [25.0, 30.5] | 8.0 [6.5, 9.7] | 100 |
| % Male | 63.0 [59.2, 66.6] | 72.5 [67.3, 77.1] | 72.0 [62.6, 79.9] | 66.3 [63.4, 69.2] |
| Mean age (years) | 31.2 [30.4, 32.0] | 28.2 [27.0, 29.4] | 26.0 [24.2, 27.8] | 30.0 [29.3, 30.6] |
| Amphetamine use (n = 186) | ||||
| Row % | 66.4 [57.9, 73.9] | 19.3 [13.3,27.1] | 14.3 [9.4,21.2] | 100 |
| % Male | 58.8 [48.6, 68.3] | 59.7 [39.8, 76.9] | 39.4 [20.7, 61.9] | 56.2 [47.6, 64.5] |
| Mean age (years) | 28.9 [26.9, 30.9] | 31.8 [26.6, 37.1] | 29.9 [25.5, 34.2] | 29.6 [27.8,31.4] |
| Cocaine or crack use (n = 217) | ||||
| Row % | 52.4 [44.1,60.5] | 23.7 [17.4,31.4] | 23.9 [17.5,31.8] | 100 |
| % Male | 65.2 [54.3, 74.7] | 71.5 [56.1,83.2] | 75.2 [60.4, 85.8] | 69.1 [61.6, 75.7] |
| Mean age (years) | 28.9 [26.7,31.0] | 30.0 [25.9, 34.2] | 32.0 [28.5, 35.4] | 29.9 [28.2,31.6] |
| Hallucinogen use (n = 194) | ||||
| Row % | 75.6 [67.7, 82.0] | 21.7 [15.6, 29.5] | 2.7 [1.1,6.1] | 100 |
| % Male | 69.7 [60.2, 77.7] | 72.4 [55.5, 84.7] | 66.7 [26.7, 91.7] | 70.2 [62.3, 77.1] |
| Mean age (years) | 22.4 [21.6, 23.3] | 21.7 [19.6, 23.9] | 20.3 [19.2,21.4] | 22.2 [21.4, 23.0] |
Note: Ninety-five percent confidence intervals are in brackets. N.A. = not applicable.
Table 2 presents the mean frequencies and quantities (if available) of substances used during the past year among those who reported use of the specific substances. For nearly all substances investigated, users without specific SUDs demonstrated lower levels of quantity and frequency of consumption relative to those with DSM-IV abuse and dependence disorders. For alcohol, both quantity and frequency of use hierarchically differentiate users from abusers and those with dependence. For cigarettes, both quantity and frequency of use differentiate the nicotine dependent from cigarette users. For opioids, the frequency of opioid consumption differentiates those who are dependent from those who are subdiagnostic opioid users. For cannabis, both the quantity and frequency of use hierarchically differentiate users from abusers and those who are dependent. For amphetamines, frequency of use differentiates those dependent from abusers and users. For cocaine or crack, frequency of use differentiates those who are dependent from abusers and users. Quantity of crack rocks used differentiates users from abusers and from those dependent. Quantity of lines of cocaine powder only differentiates those dependent from subthreshold users. Last, frequency of hallucinogen use does not significantly differentiate users from abusers and those who met criteria for dependence.
Table 2.
Mean frequency and quantity of substance use among individuals with past-year use of specific substance users by their respective Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), substance use disorder status
| Frequency and quantity of past-year specific substance use | Respective DSM-IV Substance Use Disorder Status |
||
| No diagnosis | Abuse | Dependence | |
| Alcohol use (n = 26,642) | |||
| No. of days drank any alcohol | 72.5 [70.8, 74.2] | 138.7a [132.5, 144.8] | 176.4a,b [168.9, 183.9] |
| No. of drinks of any alcohol usually consumed on days when drank alcohol | 2.19 [2.16,2.22] | 4.17 [4.01,4.32] | 6.38a,b [6.06, 6.70] |
| Cigarette use (n = 9,804) | |||
| Usual frequency when smoked cigarettes | 296.3 [292.1,300.5] | N.A. | 352.1a [350.0, 354.2] |
| Usual quantity when smoked cigarettes | 12.5 [12.1, 12.8] | N.A. | 18.2a [17.9, 18.6] |
| Opioid use (n = 674) | |||
| No. of days used opioids | 57.6 [45.3, 69.9] | 92.1 [59.5, 124.6] | 151.7a [98.5, 204.9] |
| Cannabis use (n = 1,563) | |||
| No. of days used cannabis | 67.3 [58.6,76.1] | 153.2a [137.2, 169.2] | 232.3a,b [206.1,258.5] |
| No. of cannabis joints usually smoked in a day | 1.59 [1.44, 1.74] | 2.40a [2.11,2.68] | 4.03a,b [3.15,4.92] |
| Amphetamine use (n = 185) | |||
| No. of days used amphetamines | 59.0 [36.4,81.7] | 104.3 [32.9, 175.7] | 206.0a,b [135.1,276.9] |
| Cocaine or crack use (n = 210) | |||
| No. of days used cocaine or crack | 27.2 [12.7,41.6] | 34.9 [16.9, 52.8] | 115.9a,b [70.8, 161.0] |
| No. of rocks of crack usually used in a day | 0.16 [0.05, 0.27] | 0.64a [0.33, 0.95] | 3.84a,b [0.78, 6.90] |
| No. of lines of cocaine usually used in a day | 4.21 [2.97, 5.45] | 7.24 [3.42, 11.06] | 11.56a [4.83, 18.30] |
| Hallucinogen use (n = 194) | |||
| No. of days used hallucinogens | 9.42 [4.87, 14.0] | 11.7 [4.5, 18.9] | 43.3 [0, 103.7] |
Notes: Ninety-five percent confidence intervals are in brackets. Midpoint values of frequency categories were used to calculate the group means of frequency. The sample sizes were slightly reduced because of missing or incomplete consumption data. n.a. = not applicable.
Significantly different from the no-diagnosis group at .05 level.
significantly different from the abuse group at .05 level.
Figure 1 graphically displays the predicted log odds for DSM-IV substance-specific abuse or dependence diagnoses by frequency or quantity of specific drugs. As previously noted, if the dose-response curves for abuse and dependence are largely parallel, the pattern means that the odds are proportional across a wide range of the consumption continuum, and it can be viewed as an indication that abuse and dependence lie in the same dimension. Such parallelism indicates the unidimensionality of abuse and dependence is suggested by the dose-response curves for frequency of alcohol drinking; frequency of cannabis use; frequency of opioid use; frequency of hallucinogen use; and, to a lesser extent, frequency of amphetamine use. However, the doseresponse curves for the quantity of alcohol consumed demonstrate differential patterns for abuse and dependence such that alcohol dependence has a distinctly greater “quantity of use” relationship than that found among alcohol-abusing individuals. The situation for cocaine use is more complex. A parallel dose-response pattern is noted for the quantity of cocaine powder used, again suggesting that cocaine abuse and dependence together represent a single dimension or consumption construct. However, the quantity of crack used and the frequency of crack use differentiate between abuse and dependence as shown by the diverging dose-response curves, with greatest quantity of use associated with dependence relative to abuse. Nonetheless, the differences may not be significant because the 95% confidence intervals overlap.
Figure 1.
Predicted log odds for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, substance-specific abuse or dependence by frequency and/or quantity of consumption of respective substances. Note: Predicted log odds for frequency and quantity were mutually adjusted when both measures were available.
Discussion
There have been substantial changes in the role of substance consumption in SUD diagnoses since DSM-III (American Psychiatric Association, 1980). Consumption behavior was acknowledged in DSM-III within the context of a broadly defined “pathological pattern of use” lasting for a minimum of 1 month (Rounsaville et al., 1986). In the subsequent DSM-III-R diagnostic system (American Psychiatric Association, 1987), substance consumption patterns were largely eliminated from the criteria and replaced by the conceptualization of an observational dependence syndrome originally formulated by Edwards and Gross for alcohol dependence (Edwards and Gross, 1976) and extended in DSM-III-R to other substances of abuse. This exclusion of substance consumption indicators has been carried forward to DSM-IV and now to the newly proposed diagnostic criteria in DSM-5 (American Psychiatric Association, 2011). Nonetheless, it is logical that an SUD should involve the problematic consumption of a substance or substances and that the frequency and quantity of substance use is a clinically relevant characteristic of an SUD. In fact, the U.S. Food and Drug Administration now accepts reductions in heavy drinking days as the primary outcome measure for Phase 3 alcohol clinical trials (Falk et al., 2010).
The results of this study confirm that heavier levels of consumption pertaining to both quantities and frequencies are associated with most SUDs regardless of the etiology and the identity of the drug. Across almost all substances, the log odds for having SUDs increase rapidly with the increase in frequency of use within the lower range (i.e., between 1 and 52 days in a year). The utility of the frequency measure for predicting SUDs plateaus, however, when it reaches some thresholds, and from there the log odds become stagnant or increase very slowly. This pattern is also true of quantity of alcohol use; the increase from 1 to 10 drinks per drinking day is associated with rapid increases of the log odds for having alcohol abuse or dependence, and the utility of quantity for predicting alcohol dependence starts to plateau when quantity exceeds 10 drinks per drinking day.
The gap between the log odds for having alcohol dependence and abuse widens at higher quantity levels of alcohol use. The lower odds for having alcohol abuse at higher quantity levels is likely attributable to the hierarchical structure of the diagnosis category of abuse relative to dependence. In addition, higher quantity of crack or cocaine use also predicts higher risk for cocaine dependence and, to a lesser extent, for abuse. Taken together with item response theory studies that include alcohol consumption (e.g., Saha et al., 2007), these consumption measures appear to be informative criteria at the moderate and lower severity levels for SUDs. Consumption measures can be viewed as a valuable addition to the extant DSM-IV diagnostic criteria, which are heavily weighted toward more severe and rarer psychiatric phenomena as demonstrated by item response theory criterion response curves that exceed 50% probabilities at a severity level (θ) substantially greater than 1. Abuse could readily be differentiated from subdiagnostic use and from dependence for most drugs of abuse based on quantity measures of consumption. Specifically, quantity of alcohol consumed on days when alcohol was drunk, quantity of cannabis joints smoked on days when cannabis was consumed, and the quantity of crack used on crack-using days all differentiated drug abuse from drug dependence. Frequency of cocaine or crack use also differentiated abuse from dependence, even though quantity of cocaine powder used did not. These patterns again likely result from the hierarchical relationship between DSM-IV abuse and dependence such that the individuals who consumed substances heavily will not be classified as abusers once they have met the dependence diagnoses. By contrast, the unidimensionality of abuse and dependence (based on consumption measures) was found for frequency of alcohol drinking, frequency of cannabis used, frequency of opioid use, frequency of amphetamine use, frequency of hallucinogen use, and quantity of cocaine used. These results echo the published Item Response and taxometric analyses, which suggest that abuse and dependence are aspects of the same underlying behavioral dimension (Saha et al., 2006; Slade et al., 2009; Walters, 2008) when based on diagnostic criteria that are fundamentally behavioral rather than consumption oriented.
Although DSM-IV abuse is a category based largely on adverse consequences, it is also clearly associated with a heavier pattern of consumption compared with mere substance use, rendering it distinct from both use and dependence. A recent factor-analytic study using NESARC to examine the relationship of substance abuse to dependence found that two-factor models (factors roughly corresponding to abuse and dependence) fit significantly better than one-factor models across all substances (Saha et al., 2012). The substantially higher levels of consumption found among those with dependence may be epiphenomenal to the inherent compulsivity of “addiction,” or may be mediated, in part, through the neuroadaptive changes associated with repeated exposure of the brain to high doses of habituating drugs. In both cases, the results demonstrate that, although not explicitly part of our current diagnostic taxonomy, elevations in substance consumption are inherent in SUDs, and such elevations (particularly in frequency of use) may be useful indicators in the context of screening and brief interventions for a broad variety of substances. Although lacking precision for diagnostic purposes because of their substantial variability, measures of consumption may be clinically relevant as metrics of severity because there are well-established harmful biobehavioral consequences associated with the quantity and frequency of substance use. Thus, measures of consumption could be used as a continuous measure of severity or incorporated into a clinically useful but nonhier-archical diagnostic construct reflecting “harmful use,” as is categorically recognized in the International Classification of Diseases, 10th Revision (World Health Organization, 2004).
There are several caveats worthy of mention in these observations. First, although for all SUDs examined, greater levels of use were generally associated with markedly higher odds of being affected by specific DSM-IV SUDs, there were limited findings for cigarette smoking because of the absence of an “abuse” category. However, it is evident that higher “quantity” of smoking reflected higher dependence odds, as did “frequency” of smoking. In addition, small sample sizes in NESARC for amphetamine users, crack cocaine users, and hallucinogen users may lend some imprecision to the estimates. In some cases, the estimation of consumption quantities was guided by measures suggested in the literature. For example, in these analyses, it was estimated that 10 lines of cocaine powder was equivalent to 1.0 g, and this could have introduced some minor errors in the analyses. Because the DSM-5 Substance Use Disorders Work Group has recommended combining abuse and dependence into a single disorder of graded clinical severity, with two criteria required to make a diagnosis, further studies are needed to examine how consumption of substances is related to the DSM-5 SUDs, to the graded clinical severity categories, and to the latent factor of severity manifested by the unidimen-sional set of symptom criteria.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed., rev. Washington, DC: Author; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Proposed revisions/substance use and addictive disorders. 2011. Retrieved from http://www.dsm5.org/propose-drevision/Pages/SubstanceUseandAddictiveDisorders.aspx. [Google Scholar]
- Corrao G, Bagnardi V, Zambon A, La Vecchia C. A meta-analysis of alcohol consumption and the risk of 15 diseases. Preventive Medicine. 2004;38:613–619. doi: 10.1016/j.ypmed.2003.11.027. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Li TK. Quantifying the risks associated with exceeding recommended drinking limits. Alcoholism: Clinical and Experimental Research. 2005;29:902–908. doi: 10.1097/01.alc.0000164544.45746.a7. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: Provisional description of a clinical syndrome. British MedicalJournal. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk D, Wang XQ, Liu L, Fertig J, Mattson M, Ryan M, Lit-ten RL. Percentage of subjects with no heavy drinking days: evaluation as an efficacy endpoint for alcohol clinical trials. Alcoholism: Clinical and Experimental Research. 2010;34:2022–2034. doi: 10.1111/j.1530-0277.2010.01290.x. [DOI] [PubMed] [Google Scholar]
- Gmel G, Rehm J. Harmful alcohol use. Alcohol Research & Health. 2003;27:52–62. [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Holman CD, English DR. An improved aetiologic fraction for alcohol-caused mortality. Australian Journal of Public Health. 1995;19:138–141. doi: 10.1111/j.1753-6405.1995.tb00363.x. [DOI] [PubMed] [Google Scholar]
- Li T-K, Hewitt BG, Grant BF. Is there a future for quantifying drinking in the diagnosis, treatment, and prevention of alcohol use disorders? Alcohol and Alcoholism. 2007;42:57–63. doi: 10.1093/alcalc/agl125. [DOI] [PubMed] [Google Scholar]
- Rehm J, Frick U, Bondy S. A reliability and validity analysis of an alcohol-related harm scale for surveys. Journal of Studies on Alcohol. 1999;60:203–208. doi: 10.15288/jsa.1999.60.203. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Spitzer RL, Williams JB. Proposed changes in DSM-III substance use disorders: Description and rationale. American Journal of Psychiatry. 1986;143:463–468. doi: 10.1176/ajp.143.4.463. [DOI] [PubMed] [Google Scholar]
- Royston P, Sauerbrei W. Multivariable Model-Building: A pragmatic approach to regression analysis based on fractional polynomials for modelling continuous variables. Chichester, England: John Wiley and Sons; 2008. [Google Scholar]
- Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saha TD, Harford T, Goldstein RB, Kerridge BT, Hasin D. Relationship of substance abuse to dependence in the U.S. general population. Journal of Studies on Alcohol and Drugs. 2012;73:368–378. doi: 10.15288/jsad.2012.73.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug and Alcohol Dependence. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T, Grove R, Teesson M. A taxometric study of alcohol abuse and dependence in a general population sample: Evidence of dimensional latent structure and implications for DSM-V. Addiction. 2009;104:742–751. doi: 10.1111/j.1360-0443.2009.02498.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture. Dietary guidelines for Americans. 7th ed. Washington, DC: U.S. Government Printing Office; 2010. [Google Scholar]
- Walters GD. The latent structure of alcohol use disorders: A taxometric analysis of structured interview data obtained from male federal prison inmates. Alcohol and Alcoholism. 2008;43:326–333. doi: 10.1093/alcalc/agm165. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International guide for monitoring alcohol consumption and related harm. Geneva, Switzerland: Author; 2000. [Google Scholar]
- World Health Organization. International statistical classification of diseases and health related problems. Geneva, Switzerland: Author; 2004. [Google Scholar]