Abstract
Hippocampus plays an important role in learning and memory and in spatial navigation. Production of new neurons that are functionally integrated into the hippocampal neuronal network is important for the maintenance of functional plasticity. In adults, production of new neurons in the hippocampus takes place in the subgranular zone (SGZ) of dentate gyrus. Neural progenitor/stem cells go through processes of proliferation, differentiation, migration, and maturation. This process is exquisitely sensitive to oxidative stress, and perturbation in the redox balance in the neurogenic microenvironment can lead to reduced neurogenesis. Cranial irradiation is an effective treatment for primary and secondary brain tumors. However, even low doses of irradiation can lead to persistent elevation of oxidative stress and sustained suppression of hippocampal neurogenesis. Superoxide dismutases (SODs) are major antioxidant enzymes for the removal of superoxide radicals in different subcellular compartments. To identify the subcellular location where reactive oxygen species (ROS) are continuously generated after cranial irradiation, different SOD deficient mice have been used to determine the effects of irradiation on hippocampal neurogenesis. The study results suggest that, regardless of the subcellular location, SOD deficiency leads to a significant reduction in the production of new neurons in the SGZ of hippocampal dentate gyrus. In exchange, the generation of new glial cells was significantly increased. The SOD deficient condition, however, altered the tissue response to irradiation, and SOD deficient mice were able to maintain a similar level of neurogenesis after irradiation while wild type mice showed a significant reduction in the production of new neurons.
Keywords: Oxidative stress, cranial irradiation, adult neurogenesis, superoxide dismutase, redox balance, hippocampus
1. Introduction
Under normal physiological conditions, the production of reactive oxygen species (ROS) in oxygen utilizing organisms is balanced with the production of reducing equivalents and the removal of ROS by antioxidant defense systems in cells and their surrounding microenvironment. Although ROS is highly reactive and can cause damages to macromolecules, production of ROS as by-products during normal metabolic processes is a necessary trade-off in a not-so-perfect biological system for efficient energy production. Low levels of ROS are also essential for controlling redox-sensitive proteins involved in various biochemical reactions, such as growth factor-induced cell proliferation, differentiation, and survival [1]. Under conditions leading to over-production of ROS or under-performance of antioxidant defense system, oxidative stress occurs and causes perturbations in cellular homeostasis. Acute exposure to oxidative stress, such as acute infections or inflammation and exposure to radiation or redox generating chemicals, leads to apoptotic cell death, or in extreme cases, necrotic cell death. After removal of the oxidative stress-inducing agents, cellular homeostasis may be restored. However, in some cases, chronically elevated levels of oxidative stress can be sustained for a long time. Depending on the state of redox balance, the altered redox homeostasis can have different effects on different cellular functions and cell fate decisions. Adult neurogenesis is an important process to maintain neuronal plasticity and sustain neurocognitive functions, and yet the neurogenic microenvironment (neurogenic niche) is exquisitely sensitive to oxidative stress and other types of stresses. This article addresses the role of redox balance in mediating adult neurogenesis in the context of cranial irradiation and superoxide dismutase (SOD) deficiency.
2. Adult neurogenesis
Studies from mice and rats show that new neurons are continuously generated through adult lives, albeit at a substantially reduced rate as the animals age, in the subgranular zone (SGZ) of hippocampal dentate gyrus and the subventricular zone (SVZ) of lateral ventricles [2]. Although the sample size was small, Eriksson and colleagues proved that adult humans were also capable of adult hippocampal neurogenesis by analyzing post-mortem samples from cancer patients previously injected with bromodeoxyuridine (BrdU) for diagnostic purposes [3]. In the SGZ of the hippocampus, neural stem cells give rise to neuroblasts, which can then differentiate and mature. Over the span of several weeks these cells develop axons and dendritic structures which help them migrate into the granule cell layer and develop granule cell morphology and markers of mature neurons. It is in the granule cell layer where they become functionally integrated into the hippocampal network [2]. Similar processes happen in the SVZ, from which new born cells migrate via the rostral migratory stream to the olfactory bulb [2]. The combination of cell proliferation, migration, and differentiation are generally considered to constitute the process of neurogenesis [2]. Within these microenvironments, proliferating neural progenitor cells are shown to be closely associated with astrocytes and vascular structures in the SGZ, and it is this close proximity to microvasculature that is hypothesized to be important for adult neurogenesis [4, 5]. Adult neurogenesis has been shown to provide the plasticity necessary for the functionally imperative role that the hippocampus plays in learning, memory and spatial navigation [6–8]. Consequently, reduction in hippocampal neurogenesis due to pathological changes, or as a consequence of the normal aging process, reduces the hippocampal function of learning and memory [9, 10].
3. Redox control of neural stem cell proliferation and differentiation
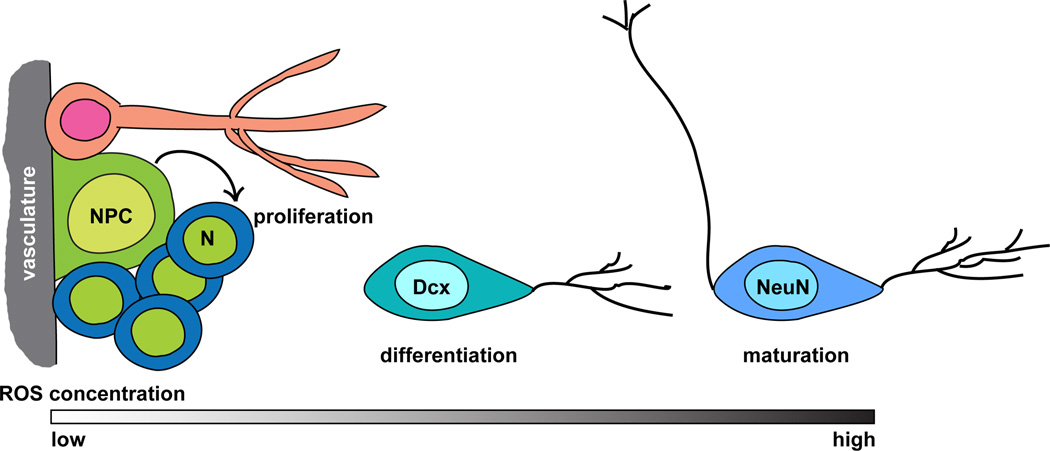
ROS-mediated activation or suppression of redox-sensitive signaling molecules critical for cell proliferation and survival have been well established, and the mechanism usually involves the formation of inter- or intra-molecular disulfide bounds in the cysteine residues [1]. Through these mechanisms, intracellular redox status has been tied to cell cycle progression and the decision between proliferation and quiescence in primary fetal fibroblasts [11–13]. Recent studies with precise measurements of the cellular redox status indicate that a more reduced environment favors cell proliferation, whereas a more oxidized environment favors cell differentiation [14]. Although the cell fate decision, in terms of quiescence vs. proliferation and proliferation vs. differentiation, in stem cells is deemed more complicated, the redox status associated with the fate decision appears to be consistent. Stem cells are known to maintain a low metabolic status, and the production of ROS is minimal. As the stem cells are stimulated, either by tissue injury, inflammation, or growth factors, low levels of ROS are produced, which activates redox-sensitive signaling pathways that favor cell proliferation [15–19]. Recent in vivo and in vitro studies with neural progenitor cells suggest that NADPH oxidase activation may be essential for ROS production, and activation of PI3K/Akt signaling pathway, through oxidative inactivation of PTEN [18, 19] is responsible for the increased cell proliferation. As the ROS levels increase, the rate of proliferation slows down and in turn the intracellular environment favors differentiation (Figure 1). This appears to be true for both neural progenitor cells and glial precursor cells [17, 19]. In order to achieve neurogenesis, a delicate redox balance needs to be achieved. Because neural progenitor cells have a choice to differentiate into either neuronal or astroglia lineage, a recent study suggests that, perhaps within the redox environment that favors differentiation, a more oxidized environment favors differentiation towards the astroglia lineage, whereas a more reduced environment favors neuronal lineage [20]. The lineage decision was shown to be mediated through NAD+ dependent Sirt1 activation [20]. Consequently, perturbation of redox balance within the neurogenic microenvironment can lead to changes in the production, functional integration, and long-term survival of new neurons.
Figure 1.
Neurogenesis and redox balance. The relationship between the redox status and the process of neural progenitor cell (NPC) proliferation, differentiation, and maturation is depicted. N, neuroblasts; Dcx, doublecortin positive cell (immature neuron); NeuN, NeuN+ cell (mature neuron). The neurogenic niche is depicted at the left as a cluster of NPC, neuroblast, astrocyte, and microvasculature. At the junction for lineage decision (differentiation), higher ROS concentration would favor the astroglial lineage and lead to the differentiation and maturation of glial cells.
4. Brain oxidative stress and the antioxidant system
The CNS is inherently vulnerable to oxidative stress and the related damages. Brain contains high levels of polyunsaturated fatty acids (PUFA), particularly arachidonic acid (AA) and docosahexaenoic acid (DHA). These two PUFAs are the major components of neural cell membrane phospholipids and are released from cell membranes upon brain injuries. Enzymatic metabolism of AA by cyclooxygenases (COXs) and lipooxygenase (LOX) leads to the production of pro-inflammatory mediators, prostaglandins, leukotrienes, and thromboxanes [21], while non-enzymatic process of AA generates isoprostanes and 4-hydroxynonenal (4-HNE). These mediators eventually lead to more production of reactive oxygen species (ROS), and consequently, higher levels of lipid peroxidation and oxidative damage [21]. Glutamate is the major excitatory neurotransmitter in the brain. Its release and uptake is tightly regulated because excessive amount of glutamate is toxic to cells. Under pathological conditions, abnormally high levels of glutamate can be present in the nervous system, leading to over activation of glutamate receptors, influx of Ca+2 into neurons, over production of ROS in the mitochondria, and eventually neuronal cell death [22]. The heightened vulnerability to oxidative stress in the nervous system is further amplified by the high energy demand for neuronal functions such as axonal transport and synaptic transmission. However, neurons have limited glycolytic capacity and mainly rely on oxidative phosphorylation for energy generation [23, 24]. Consequently, perturbation in energy metabolism, such as mitochondrial damage or oxygen and glucose deprivation, can easily lead to neuronal death or dysfunction.
The antioxidant system in the brain is probably sufficient and adequate under normal conditions. However, contrary to the higher degree of vulnerability in the mitochondria, the expression levels of brain antioxidant enzymes appear to be higher in the cytosolic compartment, and are usually ~10 times lower in the mitochondria [25, 26]. Consequently, deficiency in certain antioxidant enzymes in the nervous system leads to mitochondrial defects and neuronal degeneration in experimental animals. Examples include the mitochondrial degeneration and vacuolar degeneration in the brain caused by ubiquitous deletion of Mn superoxide dismutase (MnSOD) [27, 28]; and, increased lipid peroxidation and neural degeneration caused by neuronal-specific deletion [29] or inducible deletion [30] of glutathione peroxidase 4 (Gpx4) in mouse models.
5. Radiation therapy
Radiation therapy is used as an adjunct to surgery and chemotherapy in cancer treatments. The high energy protons generated by ionizing radiation mainly leads to ejection of electrons from water molecules via hydrolysis in biological systems where water is abundant (eq 1) [31]. In the presence of oxygen, the free electrons interact with oxygen and form superoxide radicals (O2•−) (eq 2). Superoxide radicals then cascade down to generating H2O2 via enzymatic or spontaneous dismutation. H2O2 in turn generates hydroxyl radicals (OH•−) via Fenton reaction or Haber-Weiss reaction [32, 33]. Collectively, the effect of irradiation can be viewed as imposing oxidative stress on the biological system. Most reactive radicals generated by ionizing radiation are disruptive, but short-lived, and the immediate effects from radiation exposure are double-strand DNA breaks and apoptotic cell death. This acute phase usually lasts 48 to 72 hours. The production of H2O2 and the downstream changes in redox-sensitive signaling pathways, on the other hand, can last for months and sometimes years after the initial irradiation. Persistently elevated oxidative stress of up to 80 generations of cell doubling has been demonstrated in vitro with cells treated with 10 Gy of x-ray irradiation [34]. Similarly, markers for oxidative damage can be detected in tissues months after the initial irradiation [35]. The sustained elevation of ROS in tissues and cells leads to a shift in the redox homeostasis which could alter the course of cell proliferation, differentiation, and long-term survival.
| (eq 1) |
| (eq 2) |
6. Central nervous system (CNS) and cranial irradiation
Exposure of CNS to high levels of ionizing radiation usually happens in the clinics where patients with primary or secondary brain tumors receive cranial irradiation following surgical resection. Cranial irradiation has also been used as a prophylactic treatment for patients with small cell lung carcinoma and breast cancer to prevent metastasis to the brain. Therapeutic radiation of the brain can cause severe damage to normal tissues if high dose, large fraction size, and large field size are used [36]. With the improvement of technology and limited fraction size, overt tissue damage can be avoided. However, deficits in the neurocognitive functions, including verbal and short-term memory recall, learning, memory, and spatial processing, and severe dementia, persists [36–38]. Although some deficits can be observed within the first few months following irradiation therapy, most deficits occur several months to years later. The toll on the quality of life on the patients and their care takers can be enormous.
Symptoms of the neurocognitive deficits point to hippocampus as the main target of radiation-induced tissue damage. The precise mechanism leading to radiation-induced cognitive dysfunction is not clear; however, clinical evidence from the past point to vascular damage and the subsequent hypoxic and ischemic damage to the hippocampal formation [39]. More recently, experimental evidence suggests that damage to neural stem cells and suppression of neurogenesis after radiation therapy are the most immediate and persistent events, followed by a late onset of demyelination [40, 41]. Damage to the vasculatures appears to be a very late event [40]. Studies from mice and rats suggest that neural progenitor cells from the SGZ of hippocampal dentate gyrus are exquisitely sensitive to irradiation, which causes a prolonged and dose-related reduction of overall cell proliferation and the production of new neurons in the SGZ [42, 43]. Persistent inflammation and activation of reactive microglia may be responsible for the sustained suppression of neurogenesis, and long-term treatment with indomethacin, a non-steroidal anti-inflammatory drug, before and after cranial irradiation can partially reduce the suppression of neurogenesis in experimental mice [44]. Therefore, oxidative stress and sustained alteration of the redox balance in the neurogenic microenvironment need to be considered as the underlining cause of irradiation-mediated changes in hippocampal neurogenesis.
7. Superoxide dismutase (SOD, EC 1.15.1.1)
Superoxide radicals are generated as a by-product of mitochondrial oxidative phosphorylation and from normal cellular biochemical reactions. Active production of O2•− is also achieved by activation of NADPH oxidases [45]. In addition, ionizing radiation and a number of redox-cycling chemicals can produce overwhelming amounts of O2•− in cells within a short time [46–48]. Over production of O2•− can lead to wide spread damage, and superoxide dismutases are the first line defense against O2•− in cells and tissues. In mammals, there are three types of superoxide dismutases (SODs) with different subcellular distributions, and each encoded by a different gene. The three mammalian SODs are the cytosolic Cu and Zn containing superoxide dismutase (CuZnSOD), the mitochondrial Mn containing superoxide dismutase (MnSOD), and the extracellular Cu and Zn containing superoxide dismutase (EC-SOD). The genetic and biochemical characteristics of each enzyme are listed in Table 1. Regardless of their subcellular distribution and the metal co-factors, SODs catalyze the dismutation of superoxide radicals into hydrogen peroxide (eq 3), which is then converted into water by catalase, glutathione peroxidase, or peroxiredoxin (eq 4). The reaction rate constant for each enzyme is in the 109M−1S−1 range at physiological pH [49]. CuZnSOD and EC-SOD are sensitive to inactivation by cyanide (CN), and the difference in CN sensitivity allows the measurement of CuZnSOD and MnSOD activities directly from whole cell or tissue extracts without the need for mitochondrial isolation. Although the in vivo half life of each SOD has not been determined, SODs are very stable enzymes, and available data puts the half life in tissues and cells in the range of 70–80 hours [50–52].
| (eq 3) |
 |
(eq 4) |
Table 1.
Genetic and Biochemical properties of mammalian superoxide dismutases
| CuZnSOD | MnSOD | EC-SOD | |
|---|---|---|---|
| Gene designation (human/mouse) | SOD1/Sod1 | SOD2/Sod2 | SOD3/Sod3 |
| Chromosome location (human/mouse) | HAS 21/MMU16 | HAS 6/MMU 17 | HAS 4/MMU 5 |
| Polymorphisms/mutations | 165 mutations to date1 | Val(−9)Ala and Ile(58)Thr [87–89] | Arg(213)Gly [90] |
| Disease caused by enzyme defects | Amyotrophic lateral sclerosis (ALS) | None | None |
| Metal co-factor(s) | Cu and Zn | Mn | Cu and Zn |
| Active form | dimer | tetramer | tetramer |
| Subcellular locations | Cytosol, intermembrane space of mitochondria, nucleus | Mitochondrial matrix | Extracellular matrix and circulation |
| Tissue distribution (from high to low) | Liver, kidney, brain, heart | Heart, brain, skeletal muscle | Blood vessels, lung, kidney, uterus |
| Post-translational modification | Nitration, phosphorylation, glutathiolation, glycation [91] | Acetylation, nitration, phosphorylation [91] | Glycosylation [92] |
See ALS online database (ALSoD) http://alsod.iop.kcl.ac.uk/Overview/gene.aspx?gene_id=SOD1
Mouse models deficient in each one of the SOD isoforms have been generated and used in various experimental systems [50, 53–55]. CuZnSOD and EC-SOD null mice (Sod1−/− and Sod3−/−) are viable and develop normally into adulthood without overt abnormalities. A subset of CuZnSOD null mice develop hepatocellular carcinoma by 18 months of age, while EC-SOD null mice appear to have a normal lifespan [56, 57]. MnSOD null mice (Sod2−/−), on the other hand, suffer from severe mitochondrial damage and metabolic abnormalities [54]. Consequently, MnSOD null mice, depending on their genetic backgrounds, either die in mid gestation or survive for up to 3 weeks after birth [27, 28]. Heterozygous CuZnSOD, MnSOD, and EC-SOD knockout mice (Sod1−/+, Sod2−/+, and Sod3−/+) with 50% reduction of each SOD, on the other hand, all appear to be healthy with no overt abnormalities for the majority of their lives under normal laboratory conditions [56, 58]. Transgenic mice with ubiquitous or tissue-specific overproduction of each SOD isoforms have also been created by several research groups [59–65]. High levels of SOD in cells have been shown to generate higher levels of H2O2, which can change the redox balance and can have detrimental effects on cells. However, high levels of CuZnSOD and EC-SOD seem to be well tolerated by transgenic mice [60, 65]. On the other hand, one transgenic mouse line with a 10-fold increase in MnSOD was reported to be smaller in size with mitochondrial defects [61]. In general, overexpression of SOD provides protection against acute oxidative stress, whereas deficient in SODs render mutant mice more vulnerable to oxidative damage.
8. SOD deficiency and hippocampal neurogenesis
Change in SOD levels is expected to alter the redox status of neural progenitor cells and their microenvironment. To examine hippocampal neurogenesis, proliferating cells in the SGZ can be identified with BrdU incorporation, while lineage-specific markers, NeuN and GFAP, can be used to identify mature neurons and glia, respectively. Consequently, BrdU+/NeuN+ cells in the SGZ and granule cell layer can be identified as new-born neurons and BrdU+/GFAP+ cells as new-born glia. Studies of adult neurogenesis in the SGZ of heterozygous CuZnSOD and MnSOD knockout mice and EC-SOD null mice showed a significant, across the board, reduction in the production of new neurons (BrdU+/NeuN+ cells), with the reduction ranging from 35–50% [35, 66]. The data also suggested that heterozygous CuZnSOD knockout mice had the most severe reduction in neuronal production, followed in order by EC-SOD null mice and heterozygous MnSOD knockout mice [35, 66]. Contrary to that finding, the generation of new glial cells (BrdU+/GFAP+) increased significantly [66], and the largest increase was observed in heterozygous CuZnSOD knockout mice, followed by heterozygous MnSOD knockout mice. In comparison, EC-SOD null mice only showed a modest increase in BrdU+/GFAP+ cells [35]. Although more stringent side-by-side comparison will need to be carried out to draw a firm conclusion, the data suggest that the EC-SOD deficient environment has the least impact on lineage decision, whereas the CuZnSOD deficient environment has the most impact in directing progenitor cell differentiation toward the astroglia lineage.
Reduced production of neurons can be due to a reduction in progenitor cell proliferation, reduction in differentiation into the neuronal lineage, or reduction in the long-term survival of new-born neurons. Preliminary analysis examining the rate of cell proliferation and the production of immature neurons (Dcx+, doublecortin positive cells) in the SGZ of EC-SOD null mice showed that the number of Ki67 and Dcx+ cells were comparable between EC-SOD null mice and age-matched wild type controls [35]. The data suggest that the rate of progenitor cell proliferation and the early stage differentiation into immature neurons was not altered in EC-SOD null mice and that reduced long-term survival of new-born neurons may be the cause. Whether the same mechanism applies to CuZnSOD and MnSOD deficient mice will need to be determined.
9. Interaction of SOD deficiency and cranial irradiation on hippocampal neurogenesis
Increased oxidative stress during the acute and chronic phase following irradiation is expected to play a major role in the suppression of hippocampal neurogenesis and the associated cognitive deficits, and the notion is consistently supported by animal studies [42, 43, 67]. Consequently, animals deficient in SOD are expected to be more sensitive to irradiation. However, study results from CuZnSOD, MnSOD, and EC-SOD deficient mice suggested otherwise [35, 66]. Whereas the level of BrdU+ and BrdU+/NeuN+ cells in the SGZ of irradiated wild type mice were significantly lower than that of non-irradiated controls at two months after a single dose of 5 Gy cranial irradiation, levels of BrdU+ and BrdU+/NeuN+ cells in irradiated CuZnSOD, MnSOD, and EC-SOD deficient mice were not further reduced [35, 66]. Consequently, the levels of neurogenesis in irradiated CuZnSOD, MnSOD, and EC-SOD deficient mice were higher than irradiated wild type controls. Better neurogenesis also translated into better cognitive functions in irradiated EC-SOD null mice as assessed by Morris Water Maze and contextual fear conditioning tests [68].
The preserved hippocampal neurogenesis in irradiated SOD deficient mice was unexpected, and the outcome was not due to up-regulation of other antioxidant enzymes [35, 66]. Study results from EC-SOD deficient mice, which have the most complete data in hippocampal neurogenesis and the associated cognitive functions, suggest that the EC-SOD deficient neurogenic niche perhaps adjusts and returns effectively to a state of redox balance that is similar to, or a little more reduced than the non-irradiated counterpart during the chronic phase following irradiation [68]. It is possible that the redox balance in the neurogenic niche in irradiated wild type controls will eventually return to the same level as its non-irradiated counterpart; however, the speed at which EC-SOD null mice recover from the disturbance would be faster, and the mechanism by which a more reduced redox environment is created may be different between wild type and SOD deficient mice.
10. Conclusion and future studies
In summary, oxidative stress and perturbation of redox balance can have significant consequences in hippocampal neurogenesis and quite possibly, in hippocampal-dependent function of learning and memory. In patients with primary and secondary brain tumors, radiation therapy is associated with a high probability of neurocognitive dysfunction long after the radiation therapy is completed. Antioxidant compounds and other drugs have been used in experimental animal models with some success to mitigate radiation-mediated damage to normal tissues [69–77]. However, those approaches may also provide protection to tumor cells. The SOD deficient system, on the other hand, does not appear to induce a compensatory up-regulation of other antioxidant enzymes, but at the same time, is able to restore quickly to a state of redox balance that is favorable for hippocampal neurogenesis following cranial irradiation. This may be a form of adaptive response or pre-conditioning due to SOD deficiency.
The mechanism underlies the “adaptive response” is not clear at this stage, but may involve multiple cell types and modification of the extracellular environment in the neurogenic niche. It is interesting to point out that CuZnSOD and MnSOD deficient mice all have significantly elevated levels of BrdU+/GFAP+ cells in the SGZ. Glial cells are known to produce neurotrophic factors that promote survival of neurons [78–81]. In addition, glial cells are capable of producing large amounts of GSH, which can facilitate the cystine/cysteine cycle and provide cysteine to the extracellular space. Neurons can then take up cysteine for GSH synthesis [82, 83]. Therefore, a larger glial population can ultimately support better neuronal survival and provide a better redox buffering capacity under conditions of oxidative stress.
To understand the underlying mechanism, it is important to (1) know which cell type(s) in the neurogenic niche is involved, (2) what factors are important for supporting long-term survival of the new-born neurons, (3) what signaling pathways are activated and what type of communication is going on among different cells in the neurogenic niche, and (4) what may be an effective way to recapitulate the adaptive response in normal tissues to enhance tissue recovery from radiation therapy. SOD transgenic and knockout mice are available to allow tissue/cell-specific expression or elimination of SODs. These mouse models will be helpful in identifying the specific cell types important for providing a favorable environment for neurogenesis after irradiation and for identifying the signaling pathways and cell communication involved. Different pharmacological approaches can be taken to temporarily simulate the SOD-deficient environment. One example would be using heparin, which can displace EC-SOD from its heparin sulfate or collagen binding site in the extracellular matrix [84, 85] and creates an EC-SOD deficient environment. The catalytic pocket of SODs is very small and has hampered the design of specific inhibitors for a long time. However, an inhibitor of CuZnSOD has been identified recently in a small molecule screen for the inhibition of lung adenocarcinoma growth [86]. The finding thus opens the possibility for inhibiting CuZnSOD to temporarily simulate the CuZnSOD deficient environment. Knowledge on the underlying mechanism of SOD deficiency-induced adaptive response against radiation-mediated suppression of hippocampal neurogenesis will make it possible to apply the same principle to the clinical setting to prevent or reduce radiation-mediated neurocognitive defects in the future. Likewise, detailed knowledge on how redox balance affect neurogenesis and the associated neurocognitive function will provide the opportunity to preserve functional neurogenesis during normal aging and under pathological conditions.
Highlights.
Redox balance affects neural stem cells proliferation and differentiation
Redox balance affects the lineage decision of neural stem cells
Ionizing radiation induces sustained elevation of oxidative stress in tissues
SOD deficiency leads to reduced neurogenesis and increased production of glia
SOD deficiency alters irradiation-mediated suppression of hippocampal neurogenesis
Acknowledgements
This work is supported by funding from the National Institutes of Health (NS046051) and the VA Merit Review, and the facility and resource of VA Palo Alto Health Care System.
Abbreviations
- 4-HNE
4-hydroxynonenal
- AA
Arachidonic acid
- BrdU
Bromodeoxyuridine
- COX
Cyclooxygenase
- DHA
Docosahexaenoic acid
- CNS
Central nervous system
- CuZnSOD
CuZn containing superoxide dismutase
- Dcx
Doublecortin
- EC-SOD
Extracellular superoxide dismutase
- GFAP
Glial fibrillary acidic protein
- Gpx4
Glutathione peroxidase 4
- LOX
Lipooxygenase
- MnSOD
Mn containing superoxide dismutase
- NeuN
Neuronal nuclear antigen
- PUFA
Polyunsaturated fatty acid
- ROS
Reactive oxygen species
- SGZ
Subgranular zone
- SOD
Superoxide dismutase
- SVZ
Subventricular zone
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ray PD, Huang BW, Tsuji Y. Reactive oxygen species (ROS) homeostasis and redox regulation in cellular signaling. Cell Signal. 2012 doi: 10.1016/j.cellsig.2012.01.008. [Epublication ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ming GL, Song H. Adult neurogenesis in the mammalian central nervous system. Annu Rev Neurosci. 2005;28:223–250. doi: 10.1146/annurev.neuro.28.051804.101459. [DOI] [PubMed] [Google Scholar]
- 3.Eriksson PS, Perfilieva E, Bjork-Eriksson T, Alborn AM, Nordborg C, Peterson DA, Gage FH. Neurogenesis in the adult human hippocampus. Nat Med. 1998;4:1313–1317. doi: 10.1038/3305. [DOI] [PubMed] [Google Scholar]
- 4.Palmer TD. Adult neurogenesis and the vascular Nietzsche. Neuron. 2002;34:856–858. doi: 10.1016/s0896-6273(02)00738-9. [DOI] [PubMed] [Google Scholar]
- 5.Palmer TD, Willhoite AR, Gage FH. Vascular niche for adult hippocampal neurogenesis. J Comp Neurol. 2000;425:479–494. doi: 10.1002/1096-9861(20001002)425:4<479::aid-cne2>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 6.Deng W, Aimone JB, Gage FH. New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosci. 2010;11:339–350. doi: 10.1038/nrn2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bruel-Jungerman E, Rampon C, Laroche S. Adult hippocampal neurogenesis, synaptic plasticity and memory: facts and hypotheses. Rev Neurosci. 2007;18:93–114. doi: 10.1515/revneuro.2007.18.2.93. [DOI] [PubMed] [Google Scholar]
- 8.Lledo PM, Alonso M, Grubb MS. Adult neurogenesis and functional plasticity in neuronal circuits. Nat Rev Neurosci. 2006;7:179–193. doi: 10.1038/nrn1867. [DOI] [PubMed] [Google Scholar]
- 9.Jinno S. Topographic differences in adult neurogenesis in the mouse hippocampus: a stereology-based study using endogenous markers. Hippocampus. 2011;21:467–480. doi: 10.1002/hipo.20762. [DOI] [PubMed] [Google Scholar]
- 10.Burger C. Region-specific genetic alterations in the aging hippocampus: implications for cognitive aging. Front Aging Neurosci. 2010;2:140. doi: 10.3389/fnagi.2010.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarsour EH, Kumar MG, Chaudhuri L, Kalen AL, Goswami PC. Redox control of the cell cycle in health and disease. Antioxid Redox Signal. 2009;11:2985–3011. doi: 10.1089/ars.2009.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menon SG, Goswami PC. A redox cycle within the cell cycle: ring in the old with the new. Oncogene. 2007;26:1101–1109. doi: 10.1038/sj.onc.1209895. [DOI] [PubMed] [Google Scholar]
- 13.Menon SG, Sarsour EH, Spitz DR, Higashikubo R, Sturm M, Zhang H, Goswami PC. Redox regulation of the G1 to S phase transition in the mouse embryo fibroblast cell cycle. Cancer Res. 2003;63:2109–2117. [PubMed] [Google Scholar]
- 14.Schafer FQ, Buettner GR. Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple. Free Radic Biol Med. 2001;30:1191–1212. doi: 10.1016/s0891-5849(01)00480-4. [DOI] [PubMed] [Google Scholar]
- 15.Noble M, Mayer-Proschel M, Proschel C. Redox regulation of precursor cell function: insights and paradoxes. Antioxid Redox Signal. 2005;7:1456–1467. doi: 10.1089/ars.2005.7.1456. [DOI] [PubMed] [Google Scholar]
- 16.Noble M, Smith J, Power J, Mayer-Proschel M. Redox state as a central modulator of precursor cell function. Ann N Y Acad Sci. 2003;991:251–271. doi: 10.1111/j.1749-6632.2003.tb07481.x. [DOI] [PubMed] [Google Scholar]
- 17.Smith J, Ladi E, Mayer-Proschel M, Noble M. Redox state is a central modulator of the balance between self-renewal and differentiation in a dividing glial precursor cell. Proc Natl Acad Sci U S A. 2000;97:10032–10037. doi: 10.1073/pnas.170209797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoneyama M, Kawada K, Gotoh Y, Shiba T, Ogita K. Endogenous reactive oxygen species are essential for proliferation of neural stem/progenitor cells. Neurochem Int. 56:740–746. doi: 10.1016/j.neuint.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 19.Le Belle JE, Orozco NM, Paucar AA, Saxe JP, Mottahedeh J, Pyle AD, Wu H, Kornblum HI. Proliferative neural stem cells have high endogenous ROS levels that regulate self-renewal and neurogenesis in a PI3K/Akt-dependant manner. Cell Stem Cell. 8:59–71. doi: 10.1016/j.stem.2010.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prozorovski T, Schulze-Topphoff U, Glumm R, Baumgart J, Schroter F, Ninnemann O, Siegert E, Bendix I, Brustle O, Nitsch R, Zipp F, Aktas O. Sirt1 contributes critically to the redox-dependent fate of neural progenitors. Nat Cell Biol. 2008;10:385–394. doi: 10.1038/ncb1700. [DOI] [PubMed] [Google Scholar]
- 21.Phillis JW, Horrocks LA, Farooqui AA. Cyclooxygenases, lipoxygenases, and epoxygenases in CNS: their role and involvement in neurological disorders. Brain Res Rev. 2006;52:201–243. doi: 10.1016/j.brainresrev.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Atlante A, Calissano P, Bobba A, Giannattasio S, Marra E, Passarella S. Glutamate neurotoxicity, oxidative stress and mitochondria. FEBS Lett. 2001;497:1–5. doi: 10.1016/s0014-5793(01)02437-1. [DOI] [PubMed] [Google Scholar]
- 23.Kasischke KA, Vishwasrao HD, Fisher PJ, Zipfel WR, Webb WW. Neural activity triggers neuronal oxidative metabolism followed by astrocytic glycolysis. Science. 2004;305:99–103. doi: 10.1126/science.1096485. [DOI] [PubMed] [Google Scholar]
- 24.Almeida A, Almeida J, Bolanos JP, Moncada S. Different responses of astrocytes and neurons to nitric oxide: the role of glycolytically generated ATP in astrocyte protection. Proc Natl Acad Sci U S A. 2001;98:15294–15299. doi: 10.1073/pnas.261560998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shmueli O, Horn-Saban S, Chalifa-Caspi V, Shmoish M, Ophir R, Benjamin-Rodrig H, Safran M, Domany E, Lancet D. GeneNote: whole genome expression profiles in normal human tissues. C R Biol. 2003;326:1067–1072. doi: 10.1016/j.crvi.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 26.Yanai I, Benjamin H, Shmoish M, Chalifa-Caspi V, Shklar M, Ophir R, Bar-Even A, Horn-Saban S, Safran M, Domany E, Lancet D, Shmueli O. Genome-wide midrange transcription profiles reveal expression level relationships in human tissue specification. Bioinformatics. 2005;21:650–659. doi: 10.1093/bioinformatics/bti042. [DOI] [PubMed] [Google Scholar]
- 27.Huang TT, Carlson EJ, Kozy HM, Mantha S, Goodman SI, Ursell PC, Epstein CJ. Genetic modification of prenatal lethality and dilated cardiomyopathy in Mn superoxide dismutase mutant mice. Free Radic Biol Med. 2001;31:1101–1110. doi: 10.1016/s0891-5849(01)00694-3. [DOI] [PubMed] [Google Scholar]
- 28.Huang TT, Naeemuddin M, Elchuri S, Yamaguchi M, Kozy HM, Carlson EJ, Epstein CJ. Genetic modifiers of the phenotype of mice deficient in mitochondrial superoxide dismutase. Hum Mol Genet. 2006;15:1187–1194. doi: 10.1093/hmg/ddl034. [DOI] [PubMed] [Google Scholar]
- 29.Seiler A, Schneider M, Forster H, Roth S, Wirth EK, Culmsee C, Plesnila N, Kremmer E, Radmark O, Wurst W, Bornkamm GW, Schweizer U, Conrad M. Glutathione peroxidase 4 senses and translates oxidative stress into 12/15-lipoxygenase dependent- and AIF-mediated cell death. Cell Metab. 2008;8:237–248. doi: 10.1016/j.cmet.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 30.Yoo SE, Chen L, Na R, Liu Y, Rios C, Van Remmen H, Richardson A, Ran Q. Gpx4 ablation in adult mice results in a lethal phenotype accompanied by neuronal loss in brain. Free Radic Biol Med. 2012 doi: 10.1016/j.freeradbiomed.2012.02.043. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riley PA. Free radicals in biology: oxidative stress and the effects of ionizing radiation. Int J Radiat Biol. 1994;65:27–33. doi: 10.1080/09553009414550041. [DOI] [PubMed] [Google Scholar]
- 32.Liochev SI, Fridovich I. The Haber-Weiss cycle -- 70 years later: an alternative view. Redox Rep. 2002;7:55–57. doi: 10.1179/135100002125000190. author reply 59–60. [DOI] [PubMed] [Google Scholar]
- 33.von Sonntag C. Advanced oxidation processes: mechanistic aspects. Water Sci Technol. 2008;58:1015–1021. doi: 10.2166/wst.2008.467. [DOI] [PubMed] [Google Scholar]
- 34.Limoli CL, Hartmann A, Shephard L, Yang CR, Boothman DA, Bartholomew J, Morgan WF. Apoptosis, reproductive failure, and oxidative stress in Chinese hamster ovary cells with compromised genomic integrity. Cancer Res. 1998;58:3712–3718. [PubMed] [Google Scholar]
- 35.Rola R, Zou Y, Huang TT, Fishman K, Baure J, Rosi S, Milliken H, Limoli CL, Fike JR. Lack of extracellular superoxide dismutase (EC-SOD) in the microenvironment impacts radiation-induced changes in neurogenesis. Free Radic Biol Med. 2007;42:1133–1145. doi: 10.1016/j.freeradbiomed.2007.01.020. discussion 1131–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarkissian V. The sequelae of cranial irradiation on human cognition. Neurosci Lett. 2005;382:118–123. doi: 10.1016/j.neulet.2005.02.068. [DOI] [PubMed] [Google Scholar]
- 37.Laack NN, Brown PD. Cognitive sequelae of brain radiation in adults. Semin Oncol. 2004;31:702–713. doi: 10.1053/j.seminoncol.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 38.Gondi V, Tome WA, Mehta MP. Why avoid the hippocampus? A comprehensive review. Radiother Oncol. 2010;97:370–376. doi: 10.1016/j.radonc.2010.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abayomi O, Chun MS, Kelly K. Cerebral calcification and learning disabilities following cranial irradiation for medulloblastoma. J Natl Med Assoc. 1990;82:833–836. [PMC free article] [PubMed] [Google Scholar]
- 40.Panagiotakos G, Alshamy G, Chan B, Abrams R, Greenberg E, Saxena A, Bradbury M, Edgar M, Gutin P, Tabar V. Long-term impact of radiation on the stem cell and oligodendrocyte precursors in the brain. PLoS One. 2007;2:e588. doi: 10.1371/journal.pone.0000588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abayomi OK. Pathogenesis of irradiation-induced cognitive dysfunction. Acta Oncol. 1996;35:659–663. doi: 10.3109/02841869609083995. [DOI] [PubMed] [Google Scholar]
- 42.Mizumatsu S, Monje ML, Morhardt DR, Rola R, Palmer TD, Fike JR. Extreme sensitivity of adult neurogenesis to low doses of X-irradiation. Cancer Res. 2003;63:4021–4027. [PubMed] [Google Scholar]
- 43.Monje ML, Mizumatsu S, Fike JR, Palmer TD. Irradiation induces neural precursor-cell dysfunction. Nat Med. 2002;8:955–962. doi: 10.1038/nm749. [DOI] [PubMed] [Google Scholar]
- 44.Monje ML, Toda H, Palmer TD. Inflammatory blockade restores adult hippocampal neurogenesis. Science. 2003;302:1760–1765. doi: 10.1126/science.1088417. [DOI] [PubMed] [Google Scholar]
- 45.Leto TL, Morand S, Hurt D, Ueyama T. Targeting and regulation of reactive oxygen species generation by Nox family NADPH oxidases. Antioxid Redox Signal. 2009;11:2607–2619. doi: 10.1089/ars.2009.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parke DV, Sapota A. Chemical toxicity and reactive oxygen species. Int J Occup Med Environ Health. 1996;9:331–340. [PubMed] [Google Scholar]
- 47.Aust SD, Chignell CF, Bray TM, Kalyanaraman B, Mason RP. Free radicals in toxicology. Toxicol Appl Pharmacol. 1993;120:168–178. doi: 10.1006/taap.1993.1100. [DOI] [PubMed] [Google Scholar]
- 48.Cohen GM, d'Arcy Doherty M. Free radical mediated cell toxicity by redox cycling chemicals. Br J Cancer Suppl. 1987;8:46–52. [PMC free article] [PubMed] [Google Scholar]
- 49.Gray B, Carmichael AJ. Kinetics of superoxide scavenging by dismutase enzymes and manganese mimics determined by electron spin resonance. Biochem J. 1992;281(Pt 3):795–802. doi: 10.1042/bj2810795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carlsson LM, Jonsson J, Edlund T, Marklund SL. Mice lacking extracellular superoxide dismutase are more sensitive to hyperoxia. Proc Natl Acad Sci U S A. 1995;92:6264–6268. doi: 10.1073/pnas.92.14.6264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nakano R, Inuzuka T, Kikugawa K, Takahashi H, Sakimura K, Fujii J, Taniguchi N, Tsuji S. Instability of mutant Cu/Zn superoxide dismutase (Ala4Thr) associated with familial amyotrophic lateral sclerosis. Neurosci Lett. 1996;211:129–131. doi: 10.1016/0304-3940(96)12701-4. [DOI] [PubMed] [Google Scholar]
- 52.Berkovich A, Massaro D, Clerch LB. Pertussis toxin alters the concentration and turnover of manganese superoxide dismutase in rat lung. Am J Physiol. 1996;271:L875–L879. doi: 10.1152/ajplung.1996.271.6.L875. [DOI] [PubMed] [Google Scholar]
- 53.Huang TT, Yasunami M, Carlson EJ, Gillespie AM, Reaume AG, Hoffman EK, Chan PH, Scott RW, Epstein CJ. Superoxide-mediated cytotoxicity in superoxide dismutase-deficient fetal fibroblasts. Arch Biochem Biophys. 1997;344:424–432. doi: 10.1006/abbi.1997.0237. [DOI] [PubMed] [Google Scholar]
- 54.Li Y, Huang TT, Carlson EJ, Melov S, Ursell PC, Olson JL, Noble LJ, Yoshimura MP, Berger C, Chan PH, Wallace DC, Epstein CJ. Dilated cardiomyopathy and neonatal lethality in mutant mice lacking manganese superoxide dismutase. Nat Genet. 1995;11:376–381. doi: 10.1038/ng1295-376. [DOI] [PubMed] [Google Scholar]
- 55.Lebovitz RM, Zhang H, Vogel H, Cartwright J, Jr, Dionne L, Lu N, Huang S, Matzuk MM. Neurodegeneration, myocardial injury, and perinatal death in mitochondrial superoxide dismutase-deficient mice. Proc Natl Acad Sci U S A. 1996;93:9782–9787. doi: 10.1073/pnas.93.18.9782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Elchuri S, Oberley TD, Qi W, Eisenstein RS, Jackson Roberts L, Van Remmen H, Epstein CJ, Huang TT. CuZnSOD deficiency leads to persistent and widespread oxidative damage and hepatocarcinogenesis later in life. Oncogene. 2005;24:367–380. doi: 10.1038/sj.onc.1208207. [DOI] [PubMed] [Google Scholar]
- 57.Sentman ML, Granstrom M, Jakobson H, Reaume A, Basu S, Marklund SL. Phenotypes of mice lacking extracellular superoxide dismutase and copper- and zinc-containing superoxide dismutase. J Biol Chem. 2006;281:6904–6909. doi: 10.1074/jbc.M510764200. [DOI] [PubMed] [Google Scholar]
- 58.Van Remmen H, Ikeno Y, Hamilton M, Pahlavani M, Wolf N, Thorpe SR, Alderson NL, Baynes JW, Epstein CJ, Huang TT, Nelson J, Strong R, Richardson A. Life-long reduction in MnSOD activity results in increased DNA damage and higher incidence of cancer but does not accelerate aging. Physiol Genomics. 2003;16:29–37. doi: 10.1152/physiolgenomics.00122.2003. [DOI] [PubMed] [Google Scholar]
- 59.Epstein CJ, Avraham KB, Lovett M, Smith S, Elroy-Stein O, Rotman G, Bry C, Groner Y. Transgenic mice with increased Cu/Zn-superoxide dismutase activity: animal model of dosage effects in Down syndrome. Proc Natl Acad Sci U S A. 1987;84:8044–8048. doi: 10.1073/pnas.84.22.8044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tu PH, Raju P, Robinson KA, Gurney ME, Trojanowski JQ, Lee VM. Transgenic mice carrying a human mutant superoxide dismutase transgene develop neuronal cytoskeletal pathology resembling human amyotrophic lateral sclerosis lesions. Proc Natl Acad Sci U S A. 1996;93:3155–3160. doi: 10.1073/pnas.93.7.3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Raineri I, Carlson EJ, Gacayan R, Carra S, Oberley TD, Huang TT, Epstein CJ. Strain-dependent high-level expression of a transgene for manganese superoxide dismutase is associated with growth retardation and decreased fertility. Free Radic Biol Med. 2001;31:1018–1030. doi: 10.1016/s0891-5849(01)00686-4. [DOI] [PubMed] [Google Scholar]
- 62.Yen HC, Oberley TD, Vichitbandha S, Ho YS, St Clair DK. The protective role of manganese superoxide dismutase against adriamycin-induced acute cardiac toxicity in transgenic mice. J Clin Invest. 1996;98:1253–1260. doi: 10.1172/JCI118909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ho YS, Vincent R, Dey MS, Slot JW, Crapo JD. Transgenic models for the study of lung antioxidant defense: enhanced manganese-containing superoxide dismutase activity gives partial protection to B6C3 hybrid mice exposed to hyperoxia. Am J Respir Cell Mol Biol. 1998;18:538–547. doi: 10.1165/ajrcmb.18.4.2959. [DOI] [PubMed] [Google Scholar]
- 64.Oury TD, Ho YS, Piantadosi CA, Crapo JD. Extracellular superoxide dismutase, nitric oxide, and central nervous system O2 toxicity. Proc Natl Acad Sci U S A. 1992;89:9715–9719. doi: 10.1073/pnas.89.20.9715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zou Y, Chen CH, Fike JR, Huang TT. A new mouse model for temporal- and tissue-specific control of extracellular superoxide dismutase. Genesis. 2009;47:142–154. doi: 10.1002/dvg.20470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fishman K, Baure J, Zou Y, Huang TT, Andres-Mach M, Rola R, Suarez T, Acharya M, Limoli CL, Lamborn KR, Fike JR. Radiation-induced reductions in neurogenesis are ameliorated in mice deficient in CuZnSOD or MnSOD. Free Radic Biol Med. 2009;47:1459–1467. doi: 10.1016/j.freeradbiomed.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fike JR, Rola R, Limoli CL. Radiation response of neural precursor cells. Neurosurg Clin N Am. 2007;18:115–127. doi: 10.1016/j.nec.2006.10.010. x. [DOI] [PubMed] [Google Scholar]
- 68.Raber J, Villasana L, Rosenberg J, Zou Y, Huang TT, Fike JR. Irradiation enhances hippocampus-dependent cognition in mice deficient in extracellular superoxide dismutase. Hippocampus. 2011;21:72–80. doi: 10.1002/hipo.20724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carpenter M, Epperly MW, Agarwal A, Nie S, Hricisak L, Niu Y, Greenberger JS. Inhalation delivery of manganese superoxide dismutase-plasmid/liposomes protects the murine lung from irradiation damage. Gene Ther. 2005;12:685–693. doi: 10.1038/sj.gt.3302468. [DOI] [PubMed] [Google Scholar]
- 70.Epperly M, Bray J, Kraeger S, Zwacka R, Engelhardt J, Travis E, Greenberger J. Prevention of late effects of irradiation lung damage by manganese superoxide dismutase gene therapy. Gene Ther. 1998;5:196–208. doi: 10.1038/sj.gt.3300580. [DOI] [PubMed] [Google Scholar]
- 71.Epperly MW, Defilippi S, Sikora C, Gretton J, Kalend A, Greenberger JS. Intratracheal injection of manganese superoxide dismutase (MnSOD) plasmid/liposomes protects normal lung but not orthotopic tumors from irradiation. Gene Ther. 2000;7:1011–1018. doi: 10.1038/sj.gt.3301207. [DOI] [PubMed] [Google Scholar]
- 72.Greenberger JS, Epperly M, Luketich J, Gooding W, Belani CP. Manganese superoxide dismutase-plasmid/liposome (MnSOD-PL) gene therapy protection of the esophagus from chemoradiotherapy damage during treatment of locally unresectable non-small-cell lung cancer (NSCLC) Clin Lung Cancer. 2000;1:302–304. doi: 10.3816/clc.2000.n.013. [DOI] [PubMed] [Google Scholar]
- 73.Greenberger JS, Epperly MW, Gretton J, Jefferson M, Nie S, Bernarding M, Kagan V, Guo HL. Radioprotective gene therapy. Curr Gene Ther. 2003;3:183–195. doi: 10.2174/1566523034578384. [DOI] [PubMed] [Google Scholar]
- 74.Guo H, Epperly MW, Bernarding M, Nie S, Gretton J, Jefferson M, Greenberger JS. Manganese superoxide dismutase-plasmid/liposome (MnSOD-PL) intratracheal gene therapy reduction of irradiation-induced inflammatory cytokines does not protect orthotopic Lewis lung carcinomas. In Vivo. 2003;17:13–21. [PubMed] [Google Scholar]
- 75.Gobbel GT, Marton LJ, Lamborn K, Seilhan TM, Fike JR. Modification of radiation-induced brain injury by alpha-difluoromethylornithine. Radiat Res. 1991;128:306–315. [PubMed] [Google Scholar]
- 76.Fike JR, Gobbel GT, Marton LJ, Seilhan TM. Radiation brain injury is reduced by the polyamine inhibitor alpha-difluoromethylornithine. Radiat Res. 1994;138:99–106. [PubMed] [Google Scholar]
- 77.Fike JR, Gobbel GT, Chou D, Wijnhoven BP, Bellinzona M, Nakagawa M, Seilhan TM. Cellular proliferation and infiltration following interstitial irradiation of normal dog brain is altered by an inhibitor of polyamine synthesis. Int J Radiat Oncol Biol Phys. 1995;32:1035–1045. doi: 10.1016/0360-3016(95)00030-3. [DOI] [PubMed] [Google Scholar]
- 78.Lindvall O, Wahlberg LU. Encapsulated cell biodelivery of GDNF: a novel clinical strategy for neuroprotection and neuroregeneration in Parkinson's disease? Exp Neurol. 2008;209:82–88. doi: 10.1016/j.expneurol.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 79.Kilic E, Kilic U, Hermann DM. TAT-GDNF in neurodegeneration and ischemic stroke. CNS Drug Rev. 2005;11:369–378. doi: 10.1111/j.1527-3458.2005.tb00054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang Y, Chang CF, Morales M, Chiang YH, Hoffer J. Protective effects of glial cell line-derived neurotrophic factor in ischemic brain injury. Ann N Y Acad Sci. 2002;962:423–437. doi: 10.1111/j.1749-6632.2002.tb04086.x. [DOI] [PubMed] [Google Scholar]
- 81.Alberch J, Perez-Navarro E, Canals JM. Neuroprotection by neurotrophins and GDNF family members in the excitotoxic model of Huntington's disease. Brain Res Bull. 2002;57:817–822. doi: 10.1016/s0361-9230(01)00775-4. [DOI] [PubMed] [Google Scholar]
- 82.Conrad M, Sato H. The oxidative stress-inducible cystine/glutamate antiporter, system x (c) (−) : cystine supplier and beyond. Amino Acids. 2011 doi: 10.1007/s00726-011-0867-5. [DOI] [PubMed] [Google Scholar]
- 83.Trotti D, Danbolt NC, Volterra A. Glutamate transporters are oxidant-vulnerable: a molecular link between oxidative and excitotoxic neurodegeneration? Trends Pharmacol Sci. 1998;19:328–334. doi: 10.1016/s0165-6147(98)01230-9. [DOI] [PubMed] [Google Scholar]
- 84.Karlsson K, Marklund SL. Heparin-, dextran sulfate- and protamine-induced release of extracellular-superoxide dismutase to plasma in pigs. Biochim Biophys Acta. 1988;967:110–114. doi: 10.1016/0304-4165(88)90195-x. [DOI] [PubMed] [Google Scholar]
- 85.Karlsson K, Marklund SL. Heparin-induced release of extracellular superoxide dismutase to human blood plasma. Biochem J. 1987;242:55–59. doi: 10.1042/bj2420055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Somwar R, Erdjument-Bromage H, Larsson E, Shum D, Lockwood WW, Yang G, Sander C, Ouerfelli O, Tempst PJ, Djaballah H, Varmus HE. Superoxide dismutase 1 (SOD1) is a target for a small molecule identified in a screen for inhibitors of the growth of lung adenocarcinoma cell lines. Proc Natl Acad Sci U S A. 2011;108:16375–16380. doi: 10.1073/pnas.1113554108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Millikan RC, Player J, de Cotret AR, Moorman P, Pittman G, Vannappagari V, Tse CK, Keku T. Manganese superoxide dismutase Ala-9Val polymorphism and risk of breast cancer in a population-based case-control study of African Americans and whites. Breast Cancer Res. 2004;6:R264–R274. doi: 10.1186/bcr786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Grasbon-Frodl EM, Kosel S, Riess O, Muller U, Mehraein P, Graeber MB. Analysis of mitochondrial targeting sequence and coding region polymorphisms of the manganese superoxide dismutase gene in German Parkinson disease patients. Biochem Biophys Res Commun. 1999;255:749–752. doi: 10.1006/bbrc.1998.9998. [DOI] [PubMed] [Google Scholar]
- 89.Zhang HJ, Yan T, Oberley TD, Oberley LW. Comparison of effects of two polymorphic variants of manganese superoxide dismutase on human breast MCF-7 cancer cell phenotype. Cancer Res. 1999;59:6276–6283. [PubMed] [Google Scholar]
- 90.Sandstrom J, Nilsson P, Karlsson K, Marklund SL. 10-fold increase in human plasma extracellular superoxide dismutase content caused by a mutation in heparin-binding domain. J Biol Chem. 1994;269:19163–19166. [PubMed] [Google Scholar]
- 91.Yamakura F, Kawasaki H. Post-translational modifications of superoxide dismutase. Biochim Biophys Acta. 1804:318–325. doi: 10.1016/j.bbapap.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 92.Stromqvist M, Holgersson J, Samuelsson B. Glycosylation of extracellular superoxide dismutase studied by high-performance liquid chromatography and mass spectrometry. J Chromatogr. 1991;548:293–301. doi: 10.1016/s0021-9673(01)88611-8. [DOI] [PubMed] [Google Scholar]