Abstract
Introduction
Despite intense public awareness campaigns, many patients with ST-elevation myocardial infarction (STEMI) do not utilize Emergency Medical Services (EMS) transportation to the Emergency Department (ED). Predictors for mode of transport by EMS versus private vehicle in patients with an acute STEMI were investigated.
Hypothesis
It was hypothesized that patient characteristics, specifically older age, male sex, and a history of a prior cardiac intervention, would be associated with a higher likelihood of EMS utilization.
Methods
A retrospective, observational cohort study was performed for all STEMI patients treated from April 1, 2007 through June 30, 2010 at an urban, academic ED with 24-hour cardiac catheterization available. Multivariable analyses with predetermined predictors (age, sex, prior cardiac intervention, weekend/evening arrival) were performed to investigate associations with mode of transport. Door-to-balloon (D2B) times were calculated.
Results
Of the 209 STEMI patients, 11 were excluded, leaving 198 for analysis. Median age was 60 years (IQR: 53-70), 138 (70%) arrived by private vehicle, and 60 (30%) by EMS. The primary analysis did not identify significant predictors for EMS, but a post-hoc model found that private insurance (OR 0.18; 95% CI, 0.07-0.45) was associated with fewer EMS transports. Although not statistically significant due to the great variability in time of arrival for STEMI patients transported by private vehicle, EMS transports had shorter D2B times. During business hours and weekend/evenings, EMS had D2B times of 50 (IQR: 42-61) and 58 minutes (IQR: 47-63), respectively, while private vehicle transports had median D2B times of 62 (IQR: 50-74) and 78 minutes (IQR: 66-106).
Conclusion
No associations between mode of transport and patient age, sex, weekend/ evening presentation and history of a prior cardiac intervention were identified. Privately insured patients were less likely to use EMS when experiencing a STEMI. More effective ways are needed to educate the public on the importance of EMS activation when one is concerned for acute coronary syndrome.
Keywords: ambulance, Emergency Medical Services, forecasting, myocardial infarction, public health
Introduction
Early reperfusion therapy is essential for patients experiencing ST-elevation myocardial infarction (STEMI), and treatment delays in patients with STEMI are associated with increased morbidity and mortality.1-4 Emergency Medical Services (EMS) pre-arrival STEMI alerts, pre-arrival EMS catheterization lab activations, and the transmission of prehospital electrocardiograms to Emergency Department (ED) physicians have each been shown to expedite reperfusion therapy in STEMI patients, and to increase the percentage of patients who undergo percutaneous reperfusion in under 90 minutes.5,6 Despite intense public awareness education, however, many patients with chest pain do not utilize EMS transportation.7,8 Emergency Medical Services transports often bypass crowded waiting rooms, and EMS-transported patients are more rapidly evaluated by ED physicians, who may also have the benefit of the prehospital history, physical examination, and electrocardiograms. Non-EMS transported patients may encounter multiple impediments to rapid identification and treatment of their STEMI, including waiting at entrance security, registration, and triage.
The objective of this study was to investigate whether demographic data or a patient’s prior cardiac history predicted mode of transport to the ED. It was hypothesized that patient characteristics, specifically older age, male sex, and a history of a prior cardiac intervention, would be associated with a higher likelihood of EMS utilization.
Methods
Study Design and Setting
This study was a retrospective, observational cohort study of all patients diagnosed with a STEMI presenting to a single institution. The study was conducted at a tertiary care, university hospital with an annual ED census of approximately 60,000. Attending and resident emergency medicine physicians staff the ED 24 hours a day. An additional ED attending physician works in triage from 11AM-11PM on weekdays. The metropolitan EMS agency, which accounts for >90% of patients with STEMI transported by ambulance to this ED, began transmitting prehospital electrocardiograms in 2005. Multiple attending interventional cardiology faculty staff the cardiac catheterization laboratory during business hours, and an on-call interventional cardiologist is available at night and on weekends. The institutional STEMI protocol includes the emergent activation cardiac catheterization laboratory, using a dedicated ED phone line and paging system. The study period spanned from April 1, 2007 through June 30, 2010. The study protocol received institutional review board approval.
Detailed Methodology
The subjects were identified from the institution’s local database for the national ACTION registry, the methodology and contents of which have previously been described.9 This investigation focused on patients diagnosed with a STEMI, defined as greater than or equal to one millimeter of ST elevation in two contiguous leads, or a new left bundle branch block in patients with a history consistent with an acute myocardial infarction. Patients were excluded if they were transferred from another facility, including physician offices, nursing homes, and other hospitals, as such facilities often mandate EMS transportation regardless of the individual’s transport preference. In the ACTION registry, mode of transportation is recorded as “self/family,” “ambulance,” “mobile ICU,” or “air.”9 For this study, “ambulance,” “mobile ICU,” and “air” were categorized as EMS transport. One investigator reviewed each EMS transfer’s electronic medical record, including prehospital patient care reports, to determine if the patient was transferred from another facility and met exclusion criteria. The door-to-balloon (D2B) time for patients who underwent an emergent cardiac catheterization procedure was calculated, using the accepted D2B definition of the time period (in minutes) from the patient’s arrival in the ED until a coronary lesion is identified during percutaneous coronary intervention and the catheter balloon is inflated.1 The D2B times were stratified based on whether the patient arrived at the ED on a weekday evening or weekend, because at those times, the catheterization team often is required to be called in from home, leading to longer D2B times.
Data Analysis
Descriptive statistics on demographic and clinical data are presented as median (interquartile range [IQR]) or number (%), as appropriate. The primary question of interest, whether the mode of transportation to the ED (i.e., EMS or private vehicle) was associated with a priori selected covariates, was addressed using multivariable logistic regression. Based on clinical experience and sensibility, a priori was determined to include patient age, sex, history of prior myocardial infarction (MI), history of prior cardiac intervention (defined as a composite of history of prior percutaneous intervention [PCI] and history of prior cardiac bypass surgery [CABG]), and presentation to the ED at night or on the weekend. A post-hoc analysis that investigated a potential association between insurance status, race and EMS transportation was performed. All analyses were completed using the statistical programming language R, version 2.11.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
During the study period, 209 patients presented to the study facility with a STEMI. Eleven patients were excluded because they were transported from other medical or skilled nursing facilities. Therefore, 198 STEMI subjects (138 transported by private vehicle, 60 transported by EMS) were included in the analysis. Table 1 presents the patients’ baseline characteristics. The prevalence of cardiac risk factors was similar in the two groups. Of the 198 patients, 155 (78.3%) underwent emergent cardiac catheterization, with 141 (71.2%) receiving stents. The most common reported contraindications for emergent PCI were coronary artery anatomy not suitable to primary PCI, patient quality of life decision, and resolution of ST segment elevation.
Table 1.
Baseline characteristics of patients across transport status
| Characteristics | Private Vehicle N (%) N = 138 |
EMS N (%) N = 60 |
Total N (%) N = 198 |
|---|---|---|---|
| Age: years, median (IQR) | 61 (53-69) | 60 (54-70) | 60 (53-70) |
| Sex: Female | 43 (31) | 11 (18) | 54 (27) |
| Race | |||
| White | 116 (84) | 45 (75) | 161 (81) |
| Black | 21 (15) | 14 (23) | 35 (18) |
| Other | 1 (1) | 1 (2) | 2(2) |
| Insurance | |||
| Private | 96 (87) | 29 (60) | 125 (79) |
| Public (Medicaid, Medicare, military, state) | 76 (55) | 46 (77) | 122 (62) |
| Medicare | 62 (61) | 30 (62) | 91 (46) |
| Medicaid | 14 (20) | 14 (32) | 28 (24) |
| Military | 1 (2) | 1 (2) | 2(2) |
| State | 0(0) | 1 (2) | 1 (1) |
| Uninsured | 10 (14) | 6(13) | 16 (13) |
| Medical History | |||
| Smoking | 56 (41) | 27 (45) | 83 (42) |
| Hypertension | 93 (67) | 49 (82) | 142 (72) |
| Diabetes mellitus | 44 (32) | 14 (23) | 58 (29) |
| Dyslipidemia | 82 (59) | 38 (63) | 120 (61) |
| Prior myocardial infarction | 33 (24) | 21 (35) | 58 (29) |
| Prior cardiac intervention | 51 (37) | 24 (40) | 75 (38) |
| Prior percutaneous cardiac intervention (PCI) | 38 (28) | 19 (32) | 57 (29) |
| Prior cardiac bypass surgery | 23 (17) | 10(17) | 33 (17) |
| Prior atrial fibrillation | 7(10) | 3(7) | 10(9) |
| Prior stroke | 10 (14) | 4(7) | 14(7) |
| Home aspirin use | 56 (41) | 24 (40) | 80 (40) |
| Home Clopidogrel use | 20 (14) | 9(15) | 29 (15) |
| Home Warfarin use | 11 (8) | 2(3) | 13(7) |
| Clinical Variables | |||
| Weekday/Business hour ED Arrival | 53 (38) | 17 (28) | 70 (35) |
| Emergent PCI, yes | 105 (76) | 50 (83) | 155 (78) |
| Stents implanted, yes | 93 (67) | 48 (80) | 141 (71) |
| Reperfusion candidate, yes | 103 (75%) | 50 (83%) | 153 (77%) |
| Door-to-balloon time, business hours, min, median (IQR) | 62 (50-74) | 50 (42-61) | |
| Door-to-balloon time, weekend/evening hours, min, median (IQR) | 78 (66-106) | 58 (47-63) | |
| Emergent cardiac bypass surgery | 15 (11%) | 3 (5%) | 18 (9%) |
| Initial troponin I, median (IQR) | 0.089 (0.030-0.898) | 0.080 (0.020-0.530) | 0.081 (0.030-0.805) |
| Peak troponin, median (IQR) | 4.30 (2.1-11.4) | 18.14 (0.81-65.19) | 4.75 (0.52-40.03) |
| In-hospital deaths | 5(4) | 3(5) | 8(4) |
Scherer © 2012 Prehospital and Disaster Medicine
Table 2 lists the results from the primary and secondary analyses. Reported odds ratios (ORs) compare the odds of a subject taking an ambulance to the ED as compared to the odds of taking a private vehicle. Multivariable analysis failed to show a significant association of the predictors with mode of transport. Results were similar for the sensitivity analysis, in which prior myocardial infarction was removed given the potential for overlapping information with prior cardiac intervention covariate. The post-hoc model found that private insurance was associated with fewer EMS transports, but Caucasian race was not.
Table 2.
Results from logistic regression models investigating the association transport to the ED by EMS with primary model predictors (age, sex, prior MI, prior cardiac intervention, and time of week), secondary model (removing prior myocardial infarction) and an unplanned model (including White race and patients with private insurance in place of prior MI and prior cardiac intervention).
| Covariate | Primary Model | Secondary Model | Post-Hoc Model | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age (per year) | 1.01 | (0.99-1.04) | 1.01 | (0.99-1.04) | 1.01 | (0.98-1.04) |
| Female | 0.53 | (0.24-1.17) | 0.48 | (0.22-1.06) | 0.4 | (0.16-0.99) |
| Prior myocardial infarction |
1.95 | (0.82-4.64) | ||||
| Prior cardiac intervention |
0.82 | (0.36-1.86) | 1.18 | (0.62-2.25) | ||
| Weekend/evening | 1.68 | (0.83-3.37) | 1.61 | (0.81-3.2) | 1.81 | (0.81-4.01) |
| White race | 1.16 | (0.42-3.24) | ||||
| Private insurance | 0.18 | (0.07-0.45) | ||||
Scherer © 2012 Prehospital and Disaster Medicine
Abbreviation: MI, myocardial infarction
During weekday business hours, private vehicle and EMS transported 53 and 17 patients, respectively. Of these, 44 private vehicle and 14 EMS transports underwent emergent catheterization, with median D2B times of 62 (IQR: 50-74) and 50 minutes (IQR: 42-61), respectively. During weekday business hours, 36 of the 44 private vehicle patients (82%) and 13 of the 14 (93%) EMS transports met the 90-minute D2B benchmark.
During weekends and evenings, 85 patients arrived by private vehicle and 43 by EMS. Of these, 61 private vehicle and 36 EMS transports underwent emergent catheterization with median D2B times of 78 (IQR: 66-106) and 58 minutes (IQR: 47-63), respectively. On weekends and evenings, 39 of the 61 (64%) private automobile arrivals and 33 of the 36 (92%) EMS transports met the 90-minute benchmark. Figure 1 shows the boxplot graphs for these median D2B times by time of arrival. While the descriptive statistics suggest a difference in D2B by time of arrival and mode of transport, the 95% confidence intervals on the boxplots overlap, due in part to the wide Confidence Interval (CI) for the private vehicle group.
Figure 1.
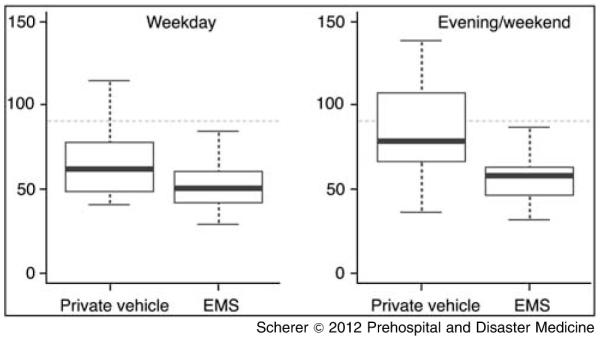
Box plots representing Median D2B times on Weekday and Weekend/Evening ED arrivalsa
aBoxplots illustrate the distribution of D2B time across mode of transport on weekdays (left) and weekend/evenings (right). Boxplots illustrate the typical five number summaries of the data (minimum, lower hinge, median, upper hinge, maximum). Dashed line represents the AHA-recommended 90-minute benchmark for STEMI revascularization.
Discussion
No significant association was identified between patient’s mode of transport and age, sex, weekend/evening arrival, or prior cardiac intervention among patients diagnosed with STEMI and treated in the ED. It had been hypothesized that patients who had a prior cardiac intervention might be more likely to use 911-EMS transport. That was not supported by this analysis, nor was there any association with age and choice of transport. Female sex appeared to be associated with reduced odds of EMS transport, whereas weekend and evening ED arrivals had higher odds of EMS transport. Neither variable reached statistical significance, although this might be the result of the relatively small sample size. Post hoc analysis found that privately insured patients were less likely to use EMS. Potentially these individuals are more likely to drive themselves or have family available to transport them to the ED.
Studies have shown the benefit of prehospital electrocardiograms and early catheterization laboratory activations for improving time to coronary reperfusion.5,6 Not only can EMS providers diagnose a STEMI prior to ED arrival, they also can provide important treatments (e.g., oxygen, nitroglycerine, aspirin) in stable patients and life-saving therapies (e.g., defibrillation, advanced cardiac life support) in decompensating patients. Given these potential benefits, EMS is the preferred transport in the setting of acute coronary syndrome. However, as this and other studies show, patients with serious cardiac disease continue to arrive at the ED by private vehicle, requiring ED triage systems to identify rapidly these high risk individuals among the many individuals who present to the ED with symptoms of potential acute coronary syndrome.7,8
Despite more than two-thirds of patients arriving by private vehicle and outside of typical business hours, the median D2B times were all within the 90-minute benchmark. This should not, however, be viewed as obviating the many potential benefits of EMS transport of STEMI patients. These results are due in large part to the team triage system. Patients who present to registration with any symptoms potentially representative of an acute coronary syndrome are rapidly brought back to a triage bay, and undergo an immediate electrocardiogram. An ED attending, who is working in triage 12 hours a day, immediately reviews that electrocardiogram for STEMI criteria. This triage system likely results in shorter times to STEMI diagnoses in patients transported by private vehicle than might be seen in many EDs without a physician staffing the registration area adjacent to the waiting room. Although not statistically significant due to the great variability in the arrival times of those who came via private vehicle, STEMI patients who presented via EMS did have shorter D2B times.
Limitations
This study is based on data from ED visits at a single, tertiary referral center with 24-hour cardiac catheterization available. The results may not be generalizable to other hospitals or geographic regions. There is the potential for referral bias, as a disproportionate number of patients with acute coronary syndrome might seek care at the hospital studied. However, six other hospitals within the county also provide 24-hour cardiac catheterization treatment.
This study was based on data entered into a national registry, so there is the potential for selection bias. This is minimized in that the hospital reviews all STEMI activations, and this data is reconciled with the information entered in the database. The authors are confident that this database included all patients diagnosed with STEMI in this ED during this study period. The relatively small sample size resulted in wide 95% confidence intervals, and increased the potential for Type II error. A formal sample size calculation was not performed, as all STEMI cases included in the local registry database were analyzed.
There is the potential that other measured and unmeasured covariates altered the multivariable analysis for predictors of mode of transportation. This study was limited to five clinically sensible covariates, based on the accepted 10-12 cases per predictor standard.10 The authors were unable to account for other individual patient factors that might have impacted patient or family decisions regarding mode of transportation.
Multiple factors might impact D2B times, including whether the catheterization team personnel are present when the STEMI activation occurs. Not all EMS services transmit prehospital electrocardiograms, and variability might occur with potential prehospital STEMI activations. This is minimized, as the metropolitan EMS agency, which transports more than 90% of the STEMI patients, began transmitting prehospital electrocardiograms in 2005. The presence of an ED attending in triage for twelve hours on weekdays may potentially result in quicker identification of patients with STEMI.
Conclusion
Emergency Medical Services is the preferred transport in the setting of acute coronary syndrome. However, this study reports that patients with serious cardiac disease continue to arrive at the ED by private vehicle, putting themselves at risk for delays in life-saving treatments. The majority of STEMI patients in this study did not use EMS for transportation to the ED. No significant associations were identified between patient’s use of EMS transport and age, sex, weekend/evening presentation and history of prior cardiac intervention. Secondary analysis found that privately-insured patients were less likely to use EMS. Continued emphasis must be focused on educating the public to activate the EMS system when there is a concern for acute coronary syndrome. Current educational efforts are not proving effective, and new and innovative ways must be found to educate the public on the significant benefits of EMS transport for patients with symptoms concerning for acute myocardial infarction.
Acknowledgments
This study was supported in part by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL102069, and in part by the Vanderbilt University Medical Center Department of Emergency Medicine Research Division.
Abbreviations
- D2B
door-to-balloon
- AHA
American Heart Association
- STEMI
ST-elevated myocardial infarction
Footnotes
Conflicts of interest and funding: The authors have no conflicts of interest to report.
References
- 1.Antman E, Anbe D, Armstrong P, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines on the Management of Patients with Acute Myocardial Infarction) Circulation. 2004;110(9):588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 2.Lambert L, Brown K, Segal E, et al. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. JAMA. 2010;303(21):2148–2155. doi: 10.1001/jama.2010.712. [DOI] [PubMed] [Google Scholar]
- 3.Nallamothu B, Fox KA, Kennelly BM, et al. Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of Acute Coronary Events. Heart. 2007;93(12):1552–1555. doi: 10.1136/hrt.2006.112847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rathore SS, Curtis JP, Nallamothu BK, et al. Association of door-to-balloon time and mortality in patients. or 565 oryears with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2009;104(9):1198–1203. doi: 10.1016/j.amjcard.2009.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown JP, Mahmud E, Dunford JV, et al. Effect of prehospital 12-lead electrocardiogram on activation of the cardiac catheterization laboratory and door-to-balloon time in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2008;101(2):158–161. doi: 10.1016/j.amjcard.2007.07.082. [DOI] [PubMed] [Google Scholar]
- 6.Ting HH, Krumholz HM, Bradley EH, et al. American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research, Emergency Cardiovascular Care Committee; American Heart Association Council on Cardiovascular Nursing; American Heart Association Council on Clinical Cardiology. Implementation and integration of prehospital ECGs into systems of care for acute coronary syndrome: a scientific statement from the American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research, Emergency Cardiovascular Care Committee, Council on Cardiovascular Nursing, and Council on Clinical Cardiology. Circulation. 2008;118(10):1066–1079. doi: 10.1161/CIRCULATIONAHA.108.190402. [DOI] [PubMed] [Google Scholar]
- 7.McCabe JM, Patel QB, Armstrong E, Garg S, Stein JC, Ganz P. Ambulance use or its lack – impact on triage of patients with ST-elevation myocardial infarctions by emergency physicians. J Am Coll Cardiol. 2011;57:1221. [Google Scholar]
- 8.Thuresson M, Jarlöv MB, Lindahl B, et al. Factors that influence the use of ambulance in acute coronary syndrome. Am Heart J. 2008;156(1):170–176. doi: 10.1016/j.ahj.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (Acute Coronary Treatment and Intervention Outcomes Network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2(5):491–499. doi: 10.1161/CIRCOUTCOMES.108.847145. [DOI] [PubMed] [Google Scholar]
- 10.Steyerberg EW. Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating. Springer; New York, NY: 2009. p. 50. [Google Scholar]


