INTRODUCTION
As its name suggests, Clostridium difficile–associated diarrhea (CDAD) is a common infection caused by the toxin-producing bacterium C. difficile. The infection can result in inflammation and cellular damage in the colon, leading to potentially severe complications, including enterocolitis with toxic megacolon, and possible death.1–3 CDAD accounts for more than $1.1 billion in health care costs each year in the U.S.3–6 The disease is usually associated with antimicrobial exposure, gastrointestinal (GI) surgery, advanced age, a compromised immune system, and long stays in health care settings, among other risk factors (Table 1).5,7–9 Between 1999 and 2004, the mortality rate associated with CDAD increased from 5.7 to 23.7 deaths per 1 million people in the U.S.10 Individuals become infected if they touch items or surfaces contaminated with the bacteria or spores and then touch their mouths.5
Table 1.
Risk Factors for Clostridium difficile–Associated Diarrhea
|
For decades, therapies for CDAD have been studied in numerous comparative randomized trials, but current treatment guidelines favor metronidazole and oral vancomycin (Vancocin, ViroPharma).5,11,12 Current guidelines from Infectious Diseases Society of America (IDSA) state that vancomycin is the drug of choice for the treatment of severe CDAD, whereas metronidazole is the drug of choice for mild-to-moderate CDAD.13 Because of concerns about emerging vancomycin-resistant enterococci and cost, however, metronidazole may be preferred.2,14–16
In May 2011, the FDA approved fidaxomicin (Dificid, Optimer Pharmaceuticals) for the treatment of CDAD based on recent data from a large phase 3 trial that compared fidamoxacin with vancomycin in infected patients.17 Fidaxomicin is the first antibacterial agent approved for CDAD in nearly 30 years.
According to the drug’s labeling, fidaxomicin should be used only for infections that are known or are strongly suspected to be caused by C. difficile to avoid the development of drug-resistant bacteria, which would lessen the effectiveness of fidaxomicin.17 To date, fidaxomicin and vancomycin are the only medications approved for the treatment of CDAD.
No prophylactic therapies are used in patients with CDAD, but preventive measures include the judicious use of antibacterial agents, thorough hand-washing between patient contacts, cautious handling of an infected patient or of items in the patient’s immediate environment, proper disinfection of objects, education of staff members, and isolation of the infected patient.7
CHEMISTRY AND PHARMACOLOGY
Fidaxomicin is a locally acting bactericidal macrolide agent derived from fermentation of the actinomycete Dactylosporangium aurantiacum. Fidaxomicin is not effective for systemic infections because of its minimal absorption.17
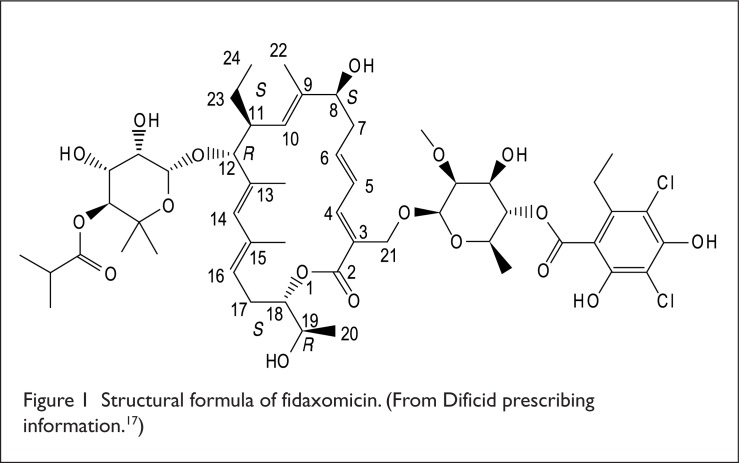
The drug’s chemical name is Oxacyclooctadeca-3,5,9,13,15-pentaen-2-one, 3-[[[6-deoxy-4-O-(3,5-dichloro-2-ethyl-4,6-dihydroxybenzoyl)-2-O-methyl-β-D-man-nopyranosyl]oxy]methyl]-12-[[6-deoxy-5-C-methyl-4-O-(2-methyl-1-oxopropyl)-β-D-lyxo-hexopyranosyl]oxy]-11-ethyl-8-hydroxy-18-[(1R)-1-hydroxyethyl]-9,13,1 5-trimethyl-,(3E,5E,8S,9E,11S,12R,13E,15E,18S). Figure 1 illustrates the drug’s structural formula.
Figure 1.
Structural formula of fidaxomicin. (From Dificid prescribing information.17)
Fidaxomicin is available in white to off-white film-coated, oblong tablets. The inactive ingredients are microcrystalline cellulose, pregelatinized starch, hydroxypropyl cellulose, butylated hydroxytoluene, sodium starch glycolate, magnesium stearate, polyvinyl alcohol, titanium dioxide, talc, polyethylene glycol, and lecithin (soy).17
In vitro, fidaxomicin is primarily active against Clostridium species, including C. difficile, via inhibition of RNA polymerases. The minimum inhibitory concentration (MIC) quality-control range for the C. difficile strain is 0.03 to 0.25 mcg/mL (via American Type Culture Collection 700057). During clinical trials, fidaxomicin’s low incidence of spontaneous resistance to C. difficile ranged from less than 1.4 × 10−9 to 12.8 × 10−9. Some resistance to fidaxomicin was observed with a specific mutation (Val-ll43-Gly) in the RNA polymerase beta subunit.17
In vitro, fidaxomicin and its main metabolite (OP-1118) were synergistic with rifampin and rifaximin against C. difficile, with fractional inhibitory concentration (FIC) values of 0.5 or less.17 Fidaxomicin demonstrates a post-antibiotic effect against C. difficile lasting from 6 to 10 hours.17,18
PHARMACODYNAMICS AND PHARMACOKINETICS
Fidaxomicin acts locally on C. difficile in the GI tract. In a 10-day dose-ranging study, the drug’s efficacy showed a dose–response relationship at dosages of 50, 100, and 200 mg twice daily.17
After fidaxomicin 200 mg twice daily was administered for 10 days in clinical trials, the maximum plasma concentration (Cmax) of both fidaxomicin and its OP-1118 metabolite within the time to maximum plasma concentration (Tmax) window (1–5 hours) was two-fold to sixfold higher than in healthy adults. In addition, plasma concentrations were 2 to 179 ng/mL for fidaxomicin and 10 to 829 ng/mL for the OP-1118 metabolite. The mean plasma concentrations of fidaxomicin and OP-1118 were about two-fold to four-fold higher in patients 65 years of age or older than in younger patients.17
After a single-dose of oral fidaxomicin 200 mg in 14 healthy adult men, the median Cmax of fidaxomicin was 5.2 ng/mL, compared with 12.0 ng/mL with OP-1118. Fidaxomicin and OP-1118 had a median Tmax of 2.00 and 1.02 hours, respectively. The median AUC was 62.9 ng • hours/mL with fidaxomicin and 118 ng • hours/mL with the metabolite.17
After 28 healthy adults took fidaxomicin with a high-fat meal, systemic absorption was minimal, and the Cmax of both fidaxomicin and its metabolite was decreased (by 21.5% and 33.4%, respectively) compared with the fasting state. Fidaxomicin may be taken with or without food. The drug is metabolized to its active metabolite via hydrolysis of the isobutyryl ester, which occurs primarily in the intestine and therefore does not depend on hepatic CYP450 enzymes. Fidaxomicin is eliminated primarily in feces (more than 92%), and only a small fraction of the administered dose (0.59%) is recovered unchanged in the urine.17
PIVOTAL CLINICAL TRIALS
In a prospective, double-blind, randomized, parallel-group study, fidaxomicin was compared with vancomycin in 629 adults with CDAD. For 10 days, patients received either vancomycin 125 mg four times daily (n = 327) or fidaxomicin 200 mg twice daily with intervening placebo for the other two doses (n = 302). The patients had either no history of CDAD or only one prior CDAD episode in the previous 3 months. Patients with life-threatening infections, hypotension, septic shock, peritoneal signs, significant dehydration, or toxic megacolon were excluded from the study.16,17,19
In the per-protocol group, nonresponding patients received at least 3 days of treatment, and cured patients received at least 8 days of treatment. In the modified intent-to-treat group (mITT), all randomized patients received at least one dose of study drug. Non-inferiority was established if the lower limit of the one-sided 97.5% confidence interval (CI) for the treatment difference was greater than −10%.16,17,19
The primary efficacy endpoint was the rate of clinical cure, defined as equal to or less than three unformed stools over 2 consecutive days or a marked reduction in unformed stools with continuing abdominal discomfort.16,17,19
In the per-protocol group, clinical cure rates were 92.1% with fidaxomicin (244/265) and 89.8% with vancomycin (254/283), respectively (lower limit of 97.5% CI for the difference, −2.6%). In the mITT group, clinical cure rates were 88.2% (253/287) and 85.8% (265/309), respectively (lower limit of 97.5% CI for the difference, −3.1%).16,17,19
During the 4 weeks following therapy, significantly lower recurrence rates were noted with fidaxomicin than with vancomycin in the per-protocol group (13.3% vs. 24.0%, respectively; P = 0.004). Significantly fewer recurrences were also observed with fidaxomicin, compared with vancomycin, in the mITT group (15.4% vs. 25.3%, respectively; P = 0.005).
There was no significant difference between fidaxomicin and vancomycin in the rate of recurrence in patients infected with the hypervirulent NAP1/B1/027 strain of C. difficile. Fidaxomicin, however, provided a 69% relative reduction in the risk of recurrence of non-NAP1/B1/027 strains compared with vancomycin. There were no significant differences between the two medications in terms of adverse events.16,17,19
Fidaxomicin and vancomycin were also compared in a prospective, double-blind, randomized, parallel-group trial involving 509 adults with CDAD. The patients were randomly assigned to receive 10 days of treatment with fidaxomicin 200 mg twice daily (n = 253) or vancomycin 125 mg four times daily (n = 256). The primary efficacy endpoint was the rate of clinical cure, defined as an improvement in diarrhea or other symptoms at the end of therapy. The non-inferiority value was the lower limit of the 95% CI for a treatment difference greater than −10%.16,17,19
Clinical cure rates were 88% and 87% for fidaxomicin and vancomycin, respectively (treatment difference, 1%). A sustained response, defined as no recurrence at 25 days after the end of treatment in patients who had achieved a clinical cure, was observed in 72% of the fidaxomicin group and in 57% of the vancomycin patients (treatment difference, 15%).16,17,19
Thus, the study findings show that twice-daily fidaxomicin was non-inferior to four-times-daily vancomycin in achieving a clinical cure in patients with CDAD; however, it was superior to vancomycin in reducing the recurrence of acute symptoms of the disease.16,17,19
SAFETY PROFILE
Contraindications
There are no contraindications to the use of fidaxomicin.17
Warning and Precautions
Fidaxomicin is not effective for the treatment of systemic infections because of its minimal systemic absorption. Therefore, to avoid promoting the development of drug-resistant bacteria, fidaxomicin should not be administered in the absence of a proven or strongly suspected C. difficile infection.17
Adverse Reactions
In controlled clinical trials, the most common adverse reactions (with an incidence of 2% or more) associated with fidaxomicin included nausea, vomiting, abdominal pain, GI hemorrhage, anemia, and neutropenia (Table 2).17
Table 2.
Selected Adverse Reactions With an Incidence of 2% or Higher In Controlled Trials Comparing Fidaxomicin and Vancomycin
| System Organ Class (Preferred Term) | Fidaxomicin (n = 564) % | Vancomycin (n = 583) % |
|---|---|---|
| Blood and lymphatic system disorders | ||
| Anemia | 2 | 2 |
| Neutropenia | 2 | 1 |
| Gastrointestinal disorders | ||
| Nausea | 11 | 11 |
| Vomiting | 7 | 6 |
| Abdominal pain | 6 | 4 |
| Gastrointestinal hemorrhage | 4 | 2 |
From fidaxomicin (Dificid) prescribing information.17
The safety of fidaxomicin was evaluated in 564 patients with CDAD in two active-comparator controlled trials in which 86.7% of patients received a full course of therapy. Thirty-three patients (5.9%) who were treated with fidaxomicin withdrew from the trials because of adverse reactions, primarily vomiting.17
The following adverse reactions were reported at an incidence of less than 2% in controlled trials of fidaxomicin: abdominal distention, abdominal tenderness, dyspepsia, dysphagia, flatulence, intestinal obstruction, megacolon, increased alkaline phosphatase levels, decreased bicarbonate levels, elevated hepatic enzymes, decreased platelet count, hyperglycemia, metabolic acidosis, drug eruption, pruritus, and rash.17
Drug Interactions
Fidaxomicin and its major metabolite, OP-1118, are substrates of the efflux transporter P-glycoprotein (P-gp), which is expressed in the GI tract. When cyclosporine, a P-gp inhibitor, was given with fidaxomicin, the plasma concentrations of fidaxomicin and OP-1118 were significantly increased. The labeling for fidaxomicin, however, does not recommend a dose reduction when the drug is administered with cyclosporine.17
Pregnancy and Nursing
Fidaxomicin is a Pregnancy Category B drug. No adequate or well-controlled studies have been conducted in pregnant women.
No evidence of fetal harm was observed when pregnant rabbits and rats were given intravenous fidaxomicin at doses up to 7.0 and 12.6 mg/kg, respectively. This represented approximately 66 and 200 times the human plasma exposure (AUC0–t).17
Caution is advised when administering fidaxomicin to nursing mothers because it is not known whether fidaxomicin is excreted in human milk.17
DOSAGE AND ADMINISTRATION
The recommended dosage of fidaxomicin for the treatment of adults with CDAD is 200 mg twice daily with or without food for 10 days. No dosage adjustment is required based on the patient’s renal function, age, or sex.17
P&T COMMITTEE CONSIDERATIONS
Fidaxomicin may be added to the formulary as a treatment option for patients with CDAD, especially in those with recurrent or treatment-resistant disease. The drug’s approval was based on the results of two randomized, double-blind, non-inferiority studies involving more than 1,100 patients with CDAD. In these trials, the clinical response in patients treated with fidaxomicin was similar to the response in patients who received vancomycin. However, more patients who received fidaxomicin achieved a sustained cure compared with the vancomycin patients.
Common adverse reactions associated with fidaxomicin included nausea, vomiting, abdominal pain, GI hemorrhage, anemia, and neutropenia.
The lack of serious adverse events and of adverse drug–drug interactions, along with convenient twice-daily oral dosing, makes fidaxomicin an appealing alternative to the other agents currently used to treat patients with CDAD (i.e., vancomycin and metronidazole).
COST
The average wholesale price for 10 days of therapy with fidaxomicin 200 mg twice daily is $3,360, compared with $1,273 for 10 days of therapy with vancomycin capsules and only $21.90 for 10 days of therapy with generic metronidazole (Table 3).19
Table 3.
Cost of Current Therapies for Clostridium difficile–Associated Diarrhea
| Drug | Dosage Regimen | Cost Per Dose (AWP) | Cost Per Treatment (AWP) |
|---|---|---|---|
| Fidaxomicin | 200 mg twice daily for 10 days | $168.00 | $3,360 (10 days) |
| Metronidazole | 500 mg three times daily for 10 to 14 days | $0.69 (generic) | $20.70 (10 days) $28.98 (14 days) |
| Vancomycin | 125 mg four times daily for 10 to 14 days | $34.82 (Vancocin HCl pulvules) | $1,392.80 (10 days) $1,949.92 (14 days) |
AWP = average wholesale price.19,20
CONCLUSION
Fidaxomicin (Dificid) is a macrolide antibacterial agent indicated for adults with CDAD. Fidaxomicin was approved on the basis of two randomized, double-blind, non-inferiority studies in which the clinical response to twice-daily fidaxomicin was similar to the response to four-times-daily vancomycin. However, higher clinical cure rates were achieved with fidaxomicin than with vancomycin.
C. difficile is a bacterium that can cause diarrhea, colitis, serious intestinal conditions, and death in severe cases. People at risk for CDAD include the elderly, patients in hospitals or nursing homes, and patients taking antibiotics for another infection.
Fidaxomicin provides a new therapeutic option for CDAD, and it is the first antibacterial medication approved for this indication in almost 30 years. Fidaxomicin is not effective for systemic infections and should not be used until C. difficile infection is confirmed in order to avoid the development of drug-resistant bacteria.
Footnotes
Disclosure: The author reports no commercial or financial relationships in regard to this article.
REFERENCES
- 1.Drekonja DM, Butler M, MacDonald R, et al. Comparative ef fectiveness of Clostridium difficile treatments: A systematic review. Ann Intern Med. 2011;155:839–847. doi: 10.7326/0003-4819-155-12-201112200-00007. [DOI] [PubMed] [Google Scholar]
- 2.Gerding DDN, Johnson S, Peterson LR, et al. Clostridium difficile–associated diarrhea and colitis. Infect Control Hosp Epidemiol. 1995;16:459–477. doi: 10.1086/648363. [DOI] [PubMed] [Google Scholar]
- 3.Reinke CM, Messick CR. Update on Clostridium difficile–induced colitis (parts 1 and 2) Am J Hosp Pharm. 1994;51:1771–1781. 1892–1901. [PubMed] [Google Scholar]
- 4.Fekety R. Guidelines for the diagnosis and management of Clostridium difficile–associated diarrhea and colitis. Am J Gastroenterol. 1997;92:739–750. [PubMed] [Google Scholar]
- 5.American Society of Health-System Pharmacists Pharmacy News. Fidaxomicin approved for C. difficile infections. May 31, 2011. Available at: www.ashp.org/menu/News/PharmacyNews/NewsArticle.aspx?id=3549. Accessed February 29, 2012. [DOI] [PubMed]
- 6.Kyne L, Hamel MB, Polavaram R, Kelly CP. Health care costs and mortality associated with nosocomial diarrhea due to Clostridium difficile. Clin Infect Dis. 2002;34:346–353. doi: 10.1086/338260. [DOI] [PubMed] [Google Scholar]
- 7.Schroeder MS. Clostridium difficile–associated diarrhea. Am Fam Physician. 2005;71:921–928. [PubMed] [Google Scholar]
- 8.Dallal RM, Harbrecht BG, Boujoukas AJ, et al. Fulminant Clostridium difficile: An underappreciated and increasing cause of death and complications. Ann Surg. 2002;235:363–372. doi: 10.1097/00000658-200203000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bartlett JG. Clinical practice: Antibiotic-associated diarrhea. N Engl J Med. 2002;346:334–339. doi: 10.1056/NEJMcp011603. [DOI] [PubMed] [Google Scholar]
- 10.Redelings MD, Sorvillo F, Mascola L. Increase in Clostridium difficile–related mortality rates: United States, 1999–2004. Emerg Infect Dis. 2007;13:1417–1419. doi: 10.3201/eid1309.061116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wenisch C, Parschalk B, Hasenhündl M, et al. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile–associated diarrhea. Clin Infect Dis. 1996;22:813–818. doi: 10.1093/clinids/22.5.813. [DOI] [PubMed] [Google Scholar]
- 12.Teasley DG, Gerding DN, Olson MM, et al. Prospective randomised trial of metronidazole versus vancomycin for Clostridium difficile–associated diarrhoea and colitis. Lancet. 1983;2:1043–1046. doi: 10.1016/s0140-6736(83)91036-x. [DOI] [PubMed] [Google Scholar]
- 13.Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America 421 (SHEA) and the Infectious Diseases Society of America (IDSA) Infect Control Hosp Epidemiol. 2010;31(5):431–455. doi: 10.1086/651706. [DOI] [PubMed] [Google Scholar]
- 14.Hospital Infection Control Practices Advisory Committee (HICPAC) Recommendations for preventing the spread of vancomycin resistance. Infect Control Hosp Epidemiol. 1995;16:105–113. doi: 10.1086/647066. [DOI] [PubMed] [Google Scholar]
- 15.Olson MM, Shanholtzer CJ, Lee JT, Jr, Gerding DN. Ten years of prospective Clostridium difficile–associated disease surveillance and treatment at the Minneapolis VA Medical Center, 1982–1991. Infect Control Hosp Epidemiol. 1994;15:371–381. doi: 10.1086/646934. [DOI] [PubMed] [Google Scholar]
- 16.Louie TJ, Miller MA, Mullane KM, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364:422–431. doi: 10.1056/NEJMoa0910812. [DOI] [PubMed] [Google Scholar]
- 17.Dificid (fidaxomicin) Tablets, prescribing information. San Diego, Calif: Optimer Pharmaceuticals; May, 2011. Available at: www.dificid.com/files/prescribing.pdf. Accessed March 15, 2012. [Google Scholar]
- 18.Ackermann G, Loffler B, Adler D, Rodloff AC. In vitro activity of OPT-80 against Clostridium difficile. Antimicrob Agents Chemother. 2004;48:2280–2282. doi: 10.1128/AAC.48.6.2280-2282.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomson Reuters Drugdex. Fidaxomicin. Available at: www.thomsonhc.com. Accessed February 29, 2012.