Abstract
This study, the largest randomized controlled trial of treatment for major depressive disorder (MDD) in an incarcerated population to date, wave-randomized 38 incarcerated women (6 waves) in prison substance use treatment with MDD to group interpersonal psychotherapy (IPT) or to an attention-matched control. Intent-to-treat analyses found that IPT participants had significantly lower depressive symptoms at the end of 8 weeks of in-prison treatment than did control participants. Control participants improved later, after prison release. IPT's rapid effect on MDD within prison may reduce serious in-prison consequences of MDD.
Keywords: major depressive disorder, prison, women, substance use disorder
1. Introduction
At the end of 2008, state and federal prisons in the United States held more than 1.6 million prisoners (Sabol et al., 2009). Major depressive disorder (MDD) is the most common severe mental illness in prison settings (Brinded et al., 2001; Fazel & Danesh, 2002; James & Glaze, 2006). A recent survey found that 23.5% of state prisoners met criteria for MDD within the past 12 months, three times the national 12-month prevalence (James & Glaze, 2006). An especially high rate of MDD among substance-using women prisoners (lifetime prevalence of 32%-38%; Pelissier & O'Neil, 2000; Zlotnick et al., 2008) is of public health concern because of the negative personal and societal costs of depression in this population.
1.2. Negative consequences of MDD among substance-using incarcerated women
MDD reduces the likelihood of incarcerated women's recovery from substance use disorder. Depression in community populations is associated with premature drop-out from addiction treatment (Brown, 1997). With few exceptions (Carroll et al., 1995; Gerra et al., 2006), depression is also associated with poorer prognosis in community addiction treatment (Bottlender & Soyka, 2005; Brown et al., 1997; Brown et al., 1998; Kosten et al., 1986; McKay et al., 2002; O'Sullivan et al., 1988; Richardson et al., 2008; Rounsaville et al., 1987; Rounsaville et al., 1986a; Rounsaville et al., 1986b; Thase et al., 2001), despite higher treatment motivation (Joe et al., 1995; McKay et al., 2002; see also Rounsaville, 2004). In correctional populations, MDD and depressive symptoms strongly predict dropout from correctional substance use programs (Brady et al., 2004; Gray & Saum, 2005; Hickert et al., 2009; Hiller et al., 1999) and poorer addiction treatment outcomes (Johnson et al., 2011).
MDD also increases risk of prison recidivism. A large (n = 79,211) study of state prison inmates found those with MDD to be at significantly increased risk of multiple incarcerations, controlling for length of current sentence and criminal offense classification (violent vs. nonviolent; Baillargeon et al., 2009a). Psychiatric distress predicts future parole violations (Skeem et al., 2009). After accounting for length of current prison sentence and past parole revocation, MDD and other severe mental illnesses increase risk for future parole revocation (Baillargeon et al., 2009b). Depression is a stronger predictor of recidivism for women than for men (Benda, 2005).
The impairment in social (Hammen, 1991; Weissman & Bothwell, 1976; Weissman et al., 1974), family (Keitner & Miller, 1990), and occupational (Broadhead et al., 1990; DeLisio et al., 1986) functioning seen with MDD can interfere with women prisoners’ ability to cope with a wide array of stressors during and after incarceration. For example, MDD increases likelihood of rejection and victimization by other inmates (Blitz et al., 2008; Marcus et al., 2001; Varese et al., 1998). MDD also increases suicide risk for incarcerated individuals (Aharonovich et al., 2002; Charles et al., 2003), an already high risk population. Many (13-20%) incarcerated individuals have attempted suicide in the past, and 1-2 out of 1,000 complete suicide while incarcerated (Charles et al., 2003; DuRand et al., 1995; Fazel & Benning, 2009; Hayes & Rowan, 1988; Sarchiapone et al., 2009). MDD may also impair women's ability to successfully address life challenges. Women prisoners experience high rates of family conflict, medical problems, homelessness, unemployment, poverty, lack of education, stigma, physical and sexual victimization, and multiple Axis I psychiatric disorders (Hills, 2000). Failure to address these challenges effectively increases women's risk for continued depression, substance use relapse, prison recidivism, and further victimization (Freudenberg et al., 2005). Finally, approximately 7 in 10 incarcerated women in the U.S. are mothers. A quarter million U.S. children have incarcerated mothers (Greenfeld & Snell, 1999). These children often face multiple risks, including maternal MDD, maternal substance use disorder, and maternal incarceration.
1.3. Need for MDD treatment research in incarcerated populations
Despite the prevalence and serious consequences of MDD among incarcerated populations, there is only one published (n = 10) randomized treatment trial for incarcerated individuals with MDD (Wilson, 1990). This study randomly assigned 10 male inmates at a large maximum-security prison to 14 90-minute sessions of group cognitive therapy or 4 30-minute sessions of individual supportive treatment plus brief counseling contacts. Men in both treatments reported improvement from moderate to mild levels of depressive symptoms, with no difference between conditions.
The contrast between the thousands of randomized treatment studies for individuals diagnosed with MDD in the community (150 published in 2007 alone; Weinberger et al., 2010) and the almost complete lack of treatment studies for MDD among incarcerated populations illustrates the desperate need for more mental health treatment research in correctional settings. The current study, which evaluated interpersonal psychotherapy (IPT) for MDD among incarcerated women, is the largest randomized controlled (RCT) trial of treatment for MDD in an incarcerated population to date. It is also the first MDD treatment study in an incarcerated population to involve women, IPT, or an attention-matched control condition.
This study targeted MDD among incarcerated women in prison substance use treatment because MDD is extremely common in this population (Pelissier & O'Neil, 2000; Zlotnick et al., 2008). MDD and substance use disorder are strongly comorbid (Grant et al., 2004; Hasin & Grant, 2002), especially among women (Grant, 1995; Merikangas et al., 1998; Wang & Patten, 2001; Wang & Patten, 2002). Furthermore, substance use disorder is the rule rather than the exception among incarcerated women (with a 6-month prevalence of 45-60% and a lifetime prevalence of 70%; Jordan et al., 1996; Teplin et al., 1996). The study targeted women who met criteria for MDD after at least 4 weeks of substance use treatment because some studies (e.g., Brooner et al., 1997; Brown et al., 1995; Nunes et al., 1998) have documented a decrease in depressive symptoms following the first few weeks of substance use treatment. The study recruited women who would be released from prison in the near future in order to evaluate the effects of MDD treatment on both in-prison and post-release outcomes.
1.4. Appropriateness of IPT for MDD among women in prison
IPT is an evidence-based treatment with proven effectiveness for MDD in non-criminal justice settings in both individual and group formats (Bolton et al., 2003; Elkin et al., 1989; Frank & Spanier, 1995; Frank et al., 1991; Levkovitz et al., 2000; Rossello et al., 2008; Shea et al., 1992). Studies to date have not found IPT to be superior to other treatments as a standalone substance use disorder treatment (Carroll et al., 1991; Carroll et al., 2004; Markowitz et al., 2008; Rounsaville et al., 1983; Rounsaville et al., 1986b). However, these studies included few female subjects, few subjects with MDD, and little or no concurrent substance use treatment. In contrast, the current study tested whether IPT can improve MDD and outcomes of concurrent substance use treatment during a demanding and high-stakes life transition (i.e., community re-entry).
IPT's focus on addressing interpersonal stressors and life changes may be a good fit for the treatment needs of women prisoners with MDD. IPT identifies a current interpersonal crisis in one of four areas (role dispute, role transition, interpersonal deficits, grief) as the proximal trigger for the current depressive episode and addresses it by helping individuals improve communication, mourn losses, or adapt to changes by building or better utilizing a social support network (Weissman et al., 2000). The first focus area, role disputes (or conflicts), works with individuals to address conflict by negotiating differing expectations in relationships. Women prisoners face many conflicts. These include disagreements within the prison, abusive or exploitative romantic relationships, friends’ and family members’ continued involvement with drugs and crime, and negotiation with caretakers to ensure their children's well-being (Enos, 2001). Women prisoners are also attempting to make several major role transitions. They go to prison, are separated from loved ones, and then return to the community. In the process, they often lose jobs, lose and regain primary care of their children, and seek to leave a criminally involved or drug-abusing lifestyle (Freudenberg et al., 2005; Garcia Coll et al., 1998; Hurley & Dunne, 1991). In fact, one study found that 90% of newly sentenced female prisoners experienced clinically significant levels of life change and loss stressors in the past year. Their average “life change unit” score was more than twice the clinical cutoff (Keaveny & Zauszniewski, 1999). Women prisoners have commonly experienced physical and/or sexual abuse (Browne et al., 1999; Greenfeld & Snell, 1999; McDaniels-Wilson & Belknap, 2008; Tusher & Cook, 2010), parental neglect and rejection, and marital and family conflict (Klein & Santiago, 2003). These experiences can isolate women and contribute to problematic interpersonal patterns (interpersonal deficits). Finally, prisoners are more likely than many other populations to lose a friend or family member through traumatic death (grief; Hurley & Dunne, 1991). One study found that 26% of newly sentenced prisoners had lost a family member to death in the past year, and 27% had experienced the death of a close friend during that time (Keaveny & Zauszniewski, 1999). Bereavement may be exacerbated by other losses such as family dissolution and loss of parental rights to children (Genty, 2001).
IPT's emphasis on developing social support may also benefit women in prison. Social support and peer support are strongly related to treatment engagement during and after prison, understanding of prison program rules, and prison program participation (Sacks & Kressel, 2005; Simpson, 2005; Skeem et al., 2009). A lack of social support predicts likelihood of substance use relapse, parole violations, and re-incarceration (Benda, 2005; Liau et al., 2004; Parsons & Warner-Robbins, 2002; Skeem et al., 2009), especially for women (Simpson et al., 2004). Furthermore, loneliness and stress are strong predictors of suicidality among incarcerated populations (Bonner & Rich, 1990; Brown & Day, 2008). IPT's focus on social support may augment prison substance use treatment because poor social support has been associated with drinking to cope (Holahan et al., 2004), dropping out of addiction treatment (Dobkin et al., 2002), and failure to maintain abstinence (Hser et al., 1999) in non-incarcerated women. Thus, social support is not only related to depression (Johnson et al., 2011), but may also be related to prisoners’ ability to function successfully in many domains both in prison and after release.
1.5 Hypotheses
An open trial of IPT for MDD among 26 women prisoners with substance use disorder found that depressive symptoms, rates of MDD diagnosis, and social support improved significantly during 8 weeks of in-prison treatment (Johnson & Zlotnick, 2008). Results suggested that addressing depressive symptoms through work on interpersonal concerns is feasible for women in prison substance use treatment programs despite multiple Axis I and II comorbidities. Based on these encouraging findings, we conducted this pilot randomized trial, which included post-release follow-up data.
We hypothesized that interpersonal psychotherapy (IPT), relative to mental health psychoeducation, would result in: 1) lower depressive symptoms in prison; and 2) lower depressive symptoms and reduced likelihood of substance use relapse after release from prison among substance-abusing incarcerated women with MDD.
2. Method
2.1. Participants
Participants included 38 sentenced female volunteers from the Rhode Island state prison who met criteria for current primary (non substance-induced) MDD as determined by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First et al., 1996a) after at least 4 weeks of abstinence and prison substance use treatment. Participants were required to have a minimum 17-item Hamilton Depression Scale (HRSD; Hamilton, 1980) score of 18, indicating moderate to severe depression (Hamilton, 1980; Keller, 2003). This cutoff was used to ensure that participants had a significant clinical disorder that was more than a mild difficulty adjusting to incarceration and to avoid a floor effect on this primary outcome variable.
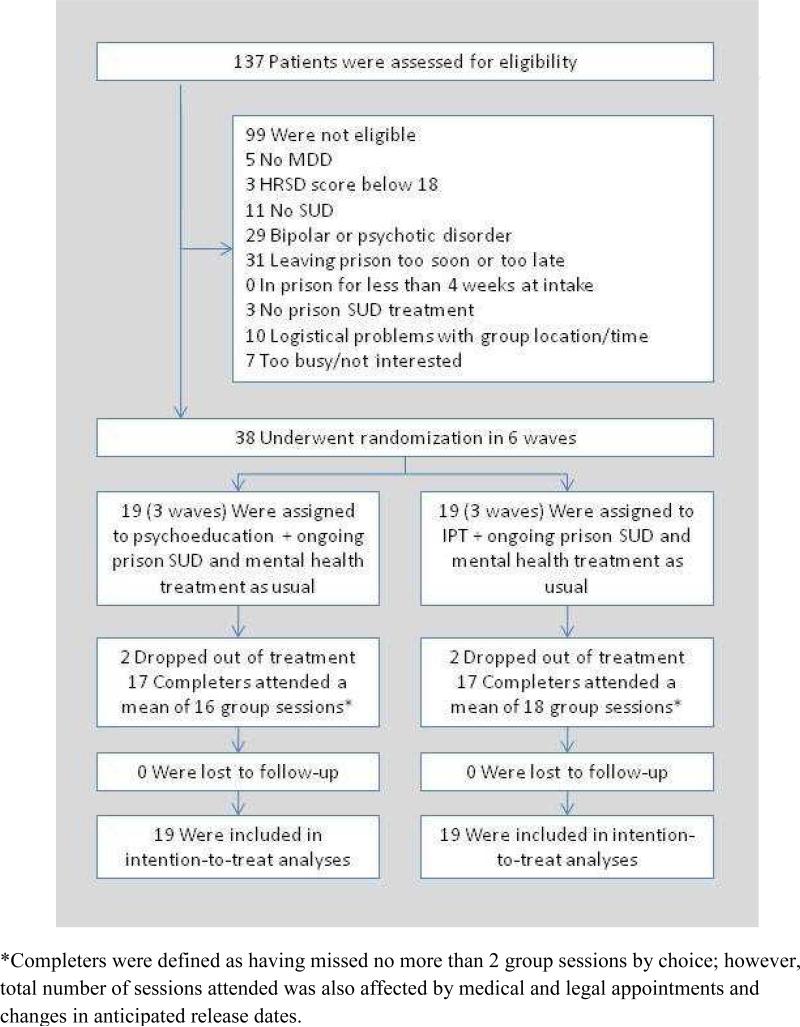
In order to determine whether MDD treatment improved post-release substance use outcomes, participants were also required to meet criteria for substance use disorder (SUD; abuse or dependence on alcohol or drugs) one month prior to incarceration as determined by the SCID and to be 10-24 weeks away from prison release. Women who met SCID-I lifetime criteria for bipolar disorder or psychotic disorder were excluded (see CONSORT diagram in Figure 1). To increase external validity, we did not exclude women who received non-study prison mental health treatment because receiving some mental health care was common practice within this prison setting.
Figure 1.
CONSORT Diagram
Potential participants were recruited through announcements made in prison substance abuse programs. Based on those announcements, women privately volunteered for the initial assessment. Study staff conducted informed consent procedures in private rooms. The consent form, which was read aloud, described randomization procedures and the voluntary nature of study participation. There were no legal and minimal financial (US$30 for completed follow-up assessments) incentives for participation. The study followed ethical guidelines for research with prisoners under institutional ethics review board approval. The trial was registered at clinicaltrials.gov under number NCT00606996.
2.2. Procedures
The study used wave randomization (Borkovec, 1993) with at least an 8 week hiatus between the end of one group and the beginning of the next group to avoid contamination due to the shared living environment. An independent individual generated the randomization sequence and concealed the assignment of each wave before the study started. Research assistants (RAs) assessed women for eligibility every four months. After intake assessments were completed, the principal investigator (PI) unsealed the wave's treatment assignment. RAs, who conducted follow-up assessments (after the in-prison portion of the treatment and at 3 months after prison release), were kept blind to condition assignment. At study completion, blinded study RAs matched participants to conditions with chance (50%) accuracy.
RAs had bachelor's or master's degrees in psychology-related fields and had experience working with substance-using women or women prisoners. RAs were trained in interviewer-administered instruments in Brown University Department of Psychiatry and Human Behavior's Clinical Assessment and Training Unit. Training consisted of an initial day-long workshop, periodic half-day booster meetings, and assessment supervision by the principal investigator.
2.3. Treatments and treatment integrity
IPT and control condition participants received manualized 60-75 minute group sessions three times per week for 8 weeks plus pre-group, midgroup, and post-group individual sessions in prison. Participants in both conditions also received 6 weekly post-release individual sessions to help maintain gains and address crises as women transitioned to the community. Session lengths varied between 60 and 75 minutes because of time taken to assemble women within the facilities, occasional early prison counts, and other facility logistics. In-prison treatment was condensed into two months because many incarcerated women serve short sentences (30 days, 60 days, 90 days, 180 days). Group sessions were kept short (60-75 minutes) because prison providers advised us that incarcerated women would have difficulty tolerating treatment sessions longer than 60-75 minutes.
Treatment structure differed slightly from the primary published group IPT manual (Wilfley et al., 2000). The Wilfley et al. manual described 20 90-minute group sessions for typical outpatients and suggested that more sessions are better for complex populations. We provided 24 slightly shorter group sessions over 8 weeks. The Wilfley model used 2-4 pre-group individual sessions, one of which was a diagnostic assessment session. We relied on a single post-baseline individual therapy session before groups began because extensive diagnostic work had already been done in the baseline research assessment and because individual clinician time is in short supply in correctional facilities. Unlike Wilfley, we provided 6 individual post-release treatment sessions for both conditions. Post-release sessions took place at safe, private locations in the community that were convenient for participants (e.g., their homes, the library, treatment facilities).
IPT condition participants received group IPT for MDD as outlined in the study treatment manual. IPT foci and techniques were taken from Weissman et al. (2000) and applied to the specific needs of women prisoners. These needs included disrupted family and friendship relationships resulting from women's entry into or attempted exit from drug- or crime involved lifestyles, substance use–specific social support and communication problems, and reactions to loss or potential loss of children to the child welfare system. In addition, interpersonal effects of child and adulthood abuse (such as isolation, distrust, problems establishing boundaries, strong attachment to serial abusive relationships) played a central role in many women prisoners’ interpersonal narratives in the open trial. As a result, in that trial, we adapted the interpersonal deficits focus in IPT for MDD among women prisoners to address current problematic relationship patterns (including isolation) that result from interpersonal trauma. That adaptation was continued into the current study. Others (e.g., Campanini et al., 2010; Krupnick et al., 2008; Talbot et al., 2011) have adapted IPT for populations of women with interpersonal trauma in a similar way. Efforts to improve social support were aimed at supports outside and inside the prison. Treatment heavily utilized IPT techniques of empathy and encouragement/acceptance of affect because of high rates of interpersonal trauma, significant negative life events (e.g., loss of children, partner suicide), and Axis II disorders in the sample.
All participants set one or two individual treatment goals in the first pre-group session, which were written, given to participants at the first group session, and referenced periodically during group treatment. These written case conceptualizations were useful to participants in our previous study of women prisoners (Johnson & Zlotnick, 2008) and in other studies of group IPT (e.g., Wilfley et al., 2000). Some refinement of group members’ treatment goals took place during the first five group sessions.
Control condition participants received attention-matched manualized in-prison and post-release psychoeducation, which described co-occurring mental health and substance use disorders (PSYCHOED). The psychoeducation condition was adapted from a class on co-occurring disorders for prisoners which had been used at the women's facilities in the past, but was not being used at the time of the study. It was designed to be credible and engaging without focusing on the theorized active ingredients of IPT (e.g., focus on social support, relationships, life changes, analysis of communication, and exploration of emotions). The stated purpose of PSYCHOED was to help women become informed and empowered consumers of mental health treatment services. The 24 in-prison sessions focused on the meaning of dual diagnosis, women's experience with dual diagnosis, major depression, bipolar disorder, each of the anxiety disorders, posttraumatic stress disorder, personality disorders, psychotic disorders, eating disorders, and self-care. Sessions for each disorder described symptoms (including relevant self-report tests), interactions between the disorder and substance use, effects of the disorder on women in prison (including film clips and written stories), and disorder-specific medication and psychosocial treatment options. When a woman in group had symptoms of a disorder, the group discussed her treatment options and preferences. The six post-release sessions focused on women's symptoms and connection with various mental health and substance use treatment options in the community.
Study treatments took place in addition to prison treatment as usual. Treatment as usual consisted of prison residential or day treatment for SUD (typically 16-30 hours per week) for all participants and prison mental health treatment as usual for most participants. Prison SUD treatment was abstinence-oriented and focused on drug education and coping skills. It took place in a psychoeducational large-group format with weekly individual case management and drug counseling. Psychoeducational groups addressed women's health, relapse prevention, problem-solving, introduction to self-help, community recovery training, anger management, and parenting. Prison treatment as usual was similar to other state prison SUD programs in the United States, which suggests that findings from this study may be generalizable to other U.S. state prisons. More than 75% of states offer programs in therapeutic community settings or day treatment settings, teach relapse prevention, and offer SUD education (Taxman et al., 2005). In-prison study treatment sessions took place during women's substance use treatment day. The intensity of study treatments (3 group sessions per week) was low relative to other treatments women were receiving (typically 16-30 hours per week). Prison treatment as usual counselors were not certified in any empirically supported treatments.
Post-release treatment as usual consisted of discharge and re-entry planning prior to release and referral for further residential or outpatient SUD treatment after release. Most participants were also released with mental health treatment referrals. However, follow-up on treatment referrals after release from prison is mixed.
The three study therapists consisted of two university-employed PhD-level psychologists (including the PI) and a bachelor's level prison substance use counselor. The PI, who led or co-led all three IPT groups, had two years of post-PhD experience when the study started and had received training and experience in IPT and in treating prisoners during the previous open trial. The other psychologist, who led two PSYCHOED groups and co-led one IPT group, was a postdoctoral fellow with one year of post-PhD experience. This therapist had prior experience in treating depression but no prior experience with either study treatment or with treating prisoners. The substance use counselor, who led one PSYCHOED group, had five years of experience in the residential prison substance use programs from which the sample was drawn. She had no previous training in depression treatment or in either study treatment except for co-leading IPT groups in the open trial (Johnson & Zlotnick, 2008). All therapists received training in both study treatments at the beginning of the trial and received weekly supervision by the PI. At least one of the psychologists led or co-led all groups except the last PSYCHOED group, which the substance use counselor led alone. Therapist allegiance effects were not assessed. However, the relative novelty of both study treatments to the two therapists who led PSYCHOED groups and the highly structured, scripted nature of PSYCHOED should have minimized the likelihood that allegiance effects played a large role in study outcomes.
An independent IPT-trained doctoral level psychologist rated adherence and competence for 18% of group sessions using adherence and competence scales adapted from those used in the National Institute of Mental Health Treatment of Depression Collaborative Research Program (Elkin et al., 1989). Interrater reliabilities (averaged measures intraclass correlations between the rater and the PI) for these scales were .99 for adherence and .84 for competence overall scores. Across treatments, therapists spent 95% of session time on topic and scored an average of 6.21 on a scale from “1 = poor” to “7 = ideal” on therapist competence items.
2.4. Measures
The SCID-I, SCID-II (First et al., 1996b), and Trauma History Questionnaire (Green, 1996) were used to characterize diagnoses and histories of physical and sexual abuse in the sample. RAs used the 17-item Hamilton Rating Scale for Depression (HRSD) to assess depressive symptoms and the Timeline Followback (TLFB; Sobell et al., 1980) to assess drug use and heavy drinking (4+ standard drinks) days and days reincarcerated after release. Both measures are standard and well-validated. The HRSD has been used extensively in MDD treatment studies (Keller, 2003), with inter-rater reliabilities of .78 - .91 and convergent validities of .73 - .86 in depressed female samples (Rehm & Ohara, 1985; Whisman et al., 1989). The TLFB has excellent reliability (Sobell & Sobell, 1978) and validity for alcohol (Sobell et al., 1980; Sobell et al., 1979) and drug use (Fals-Stewart et al., 2000; Sobell et al., 1996), and is sensitive to change as used in this study (Babor et al., 1987; Sobell et al., 1986). RAs conducted follow-up interviews with released women and women who were re-incarcerated. Of the participants not institutionalized at 3-month follow-up, all but three provided breath alcohol tests and urine drug screens (using Varian's OnSite Cupkit Pro 5). In addition, 31 women (82%) also provided a urine drug screen sample at 2 weeks after release. “Relapse” was defined as heavy drinking or using drugs on at least 10% of non-incarcerated days or any positive breath test/urine drug screen.
2.5. Sample size and analyses
Six waves (38 women total) were recruited and randomized between October 2006 and November 2008. Follow-up ended in December 2009 with 100% follow-up rates at pre-release and 3-month post-release follow-up assessments, leaving no missing data. All analyses were intent-to-treat and included all 38 participants. Intraclass correlations for primary outcomes within waves were 0.20 (95% CI -0.13 - 0.53) and 0.00 (-0.48 – 0.48) for post-treatment and follow-up HRSD scores and 0.00 (-0.29 - 0.29) for relapse. Wave-level effects were not modeled in analyses because there were too few waves for these models to be robust. Depression scores for post-treatment and 3-month follow-up points were analyzed using linear regression, predicted from treatment condition and intake HRSD score. Relapse was predicted from treatment condition using logistic regression, with drinking/using days in the 180 days prior to prison as a covariate. Re-incarceration in the first 90 days after release was predicted from treatment condition, using self-reported number of prior convictions as a covariate. Our sample size of 38 provided 80% power to detect a large effect size (d = 0.93) at α = 0.05 for continuous variables. For dichotomous outcomes, the sample size provided 80% power to detect an odds ratio of 0.10.
Because tests of moderation have lower power than tests of main effects, moderator analyses in this small study were exploratory. Intake depression severity (HRSD score), antisocial personality disorder, borderline personality disorder, history of physical abuse, history of sexual abuse, and minority status were independently tested as treatment moderators for significant treatment effects. Predictors were centered and each variable and its interaction with treatment condition were added to analyses predicting outcome. Moderator tests used p < .01 to control for multiple comparisons.
3. Results
3.1. Sample characteristics
Sample characteristics are shown in Table 1. Treatment as usual doses are shown in Table 2. All participants met criteria for current primary (non substance-induced) MDD, diagnosed after a median of 3 months (range 1-14) of abstinence from substances and several weeks of prison residential substance use treatment. Participants’ mean intake HRSD score was 28 (SD = 7), indicating a very severe level of depression, despite the fact that 63% were taking antidepressant medications. In fact, most were taking multiple antidepressant medications. All participants reported past depressive episodes during periods when they were not incarcerated, which suggested that depressive symptoms were not merely a passing reaction to incarceration. The median number of past depressive episodes was “10 or more.” Substance use disorder severity was also severe. More than half met current criteria for dependence on multiple substances in the month prior to prison and most dependence diagnoses were categorized as “severe” according to the SCID. Participants averaged 122 days of heavy drinking or drug use in the 180 days prior to incarceration. The sample was also young (median age 35, range 20-54), unmarried (87%), and low-income (74% had annual legal income less than $10,000 prior to incarceration), characteristics often associated with poor treatment outcome (Pelc et al., 2002; Siqueland et al., 2002). Other typically negative treatment indicators, including physical (84%) and sexual abuse (63%) histories and borderline (37%) and antisocial (42%) personality disorders, were also common in the sample. Women's most common offenses were possessing/selling drugs, probation violations, and theft/shoplifting. Many of these crimes were committed to pay for drugs.
Table 1.
Sample characteristics
| Psychoeducation (n = 19) | IPT (n = 19) | Overall (n = 38) | |
|---|---|---|---|
| Demographic characteristics | |||
| Age [M (SD)] | 37.1 (10.5) | 32.9 (7.3) | 35.0 (9.2) |
| Hispanic Ethnicity | 11% | 26% | 18% |
| African-American | 11% | 26% | 18% |
| Unmarried | 84% | 90% | 87% |
| Legal income < $10,000 USD per year | 74% | 74% | 74% |
| Depression severity | |||
| Intake HRSD score [M (SD)] | 27.2 (7.5) | 28.0 (6.0) | 27.6 (6.7) |
| Median duration of index episode in months | 10.0 | 18.0 | 16.5 |
| Median number of past depressive episodes | 10 or more | 10 or more | 10 or more |
| Had attempted suicide before | 53% | 26% | 40% |
| SUD diagnoses for month prior to prison | |||
| Cocaine dependence | 53% | 63% | 58% |
| Alcohol dependence | 53% | 63% | 58% |
| Opiate dependence | 26% | 21% | 24% |
| Marijuana dependence | 26% | 16% | 21% |
| Sedative/hypnotic dependence | 21% | 21% | 21% |
| Days using/drinking of 180 prior to prison [M (SD)] | 125 (54) | 119 (54) | 122 (53) |
| Criminal justice characteristics | |||
| Median (range) number of past arrests | 4 (0-20) | 6 (0-25) | 5 (0-25) |
| Median (range) months incarcerated for current sentence | 3 (1-14) | 3 (1-12) | 3 (1-14) |
| Minimum security | 100% | 89% | 95% |
| Comorbidities | |||
| Borderline personality disorder | 26% | 47% | 37% |
| Antisocial personality disorder | 53% | 32% | 42% |
| Had been sexually abused/assaulted | 68% | 58% | 63% |
| Had been physically abused/assaulted | 74% | 95% | 84% |
*p < .05 difference between conditions. Comparisons for data reported as percentages used chi-square tests, for medians used the Mann-Whitney U tests, and for means used t-tests. All percentages are relative to the total sample size of 38.
Table 2.
Treatment as usual
| Psychoeducation (n = 19) | IPT (n = 19) | Overall (n = 38) | |
|---|---|---|---|
| Prison treatment as usual at intake | |||
| Median weeks in prison SUD treatment | 5 | 6 | 5.6 |
| On antidepressant medicationsa | 79%* | 47% | 63% |
| For < 8 weeks | 58%* | 21% | 39% |
| For > 8 weeks | 21% | 26% | 24% |
| Past-month prison mental health counseling | 63%* | 21% | 42% |
| Community treatment as usual after prison releaseb | |||
| Any residential SUD treatment | 53% | 58% | 55% |
| Residential SUD treatment for entire post-prison follow-up period | 21% | 32% | 26% |
| Any antidepressant medication usec | 68% | 58% | 63% |
| Antidepressant medication use on at least 66% of days | 42% | 42% | 42% |
| Any mental health counseling | 37% | 53% | 45% |
| 1-6 sessions | 26% | 26% | 26% |
| 12+ sessions | 11% | 26% | 18% |
| Any substance use counseling | 58% | 63% | 60% |
| 1-8 sessions | 16% | 16% | 16% |
| 11+ sessions | 42% | 47% | 45% |
p < .05 difference between conditions. Comparisons for data reported as percentages used chi-square tests, for medians used the Mann-Whitney U tests, and for means used t-tests. All percentages are relative to the total sample size of 38.
The 24 women taking antidepressant medications at baseline were taking an average of 2.3 psychiatric medications each (2.1 antidepressant medications) each. 21 of the 24 women were taking multiple antidepressants or MDD treatment add-ons (such as lithium, aripiprazole, or quetiapine).
Use of medications to treat substance use was not common in this sample. Four participants took SUD treatment medications at some point during follow-up, but only one took these medications for more than 12 days of the follow-up period.
Women who were on psychiatric medications in prison were typically discharged with a 2-week supply. However, many women did not have medical insurance after release and some (4 of the 24 women prescribed antidepressants within the prison) did not obtain additional medications after release.
3.2. Feasibility and acceptability of study treatments
Study treatments were feasible and acceptable; 89% of participants in each condition completed in-prison treatment (missed less than 3 of the 24 group sessions by choice, rather than because of early release, court dates, etc.). Of the 6 post-release sessions in the community, 84% of the intent-to-treat sample attended at least 1 and 37% attended at least 5 sessions. Post-release attendance rates were identical across conditions. On a scale from 1 “Very dissatisfied” to 5 “Very satisfied”, both IPT and PSYCHOED participants reported a mean satisfaction score of 4.9 with the treatments they received. When asked if they would participate in the same treatment again, 84% of IPT participants and 76% of PSYCHOED participants said “definitely yes,” suggesting that PYCHOED was a credible control condition.
3.3. IPT problem areas
Treatment goals for the 19 women in the IPT condition were evenly divided among the four IPT problem areas. Primary treatment goals addressed grief for 4 women, transitions for 5 women, role disputes (i.e., conflicts) for 4 women, and interpersonal deficits for 6 women. Interpersonal deficits goals in this sample typically focused either on isolation or on interpersonal patterns that contributed to women remaining in serial abusive relationships. Isolation was often a direct (ex-boyfriend isolated the woman from friends and family) or indirect (woman does not trust anyone) result of abuse. Ten women also had secondary goals: 2 were in the area of grief, 1 in transitions, 5 in role disputes, and 2 in interpersonal deficits. The challenge in setting IPT treatment goals in this sample was not finding a triggering life stressor, it was determining which of many recent life stressors seemed most related to the onset of the current depressive episode and/or most related to the woman's current distress. Incarceration itself (a role transition) was rarely a salient triggering event.
3.3. In prison outcomes
Accounting for intake HRSD scores, participants in the IPT condition had significantly lower HRSD scores (M = 14.1, SD = 8.3) at the end of in-prison group treatment than did PSYCHOED participants (M = 20.6, SD = 10.5; β = -7.09, SE[B] = 2.81, β = -.36, t = -2.52, p = 0.016). This corresponds to a covariate-adjusted Cohen's d = 0.82 (95% CI = 0.15 – 1.48). In-prison MDD response rates (HRSD decrease of at least 50%) were 13/19 for IPT and 5/19 for PSYCHOED (OR = 6.07, 95% CI = 1.44 – 25.5). MDD point recovery rates (HRSD < 8 at the end of group treatment) were 5/19 for IPT and 2/19 for PSYCHOED (OR = 3.92, 95% CI = 0.57 - 27.4).
3.4. Post-release outcomes
Six of 19 women (32%) in the IPT condition and 9 of 19 (47%) women in the PSYCHOED condition experienced a substance use relapse after release, but this difference was not statistically significant (B = -0.81, SE[B] = 0.71, Wald = 1.29, p = 0.26; OR = 0.45, 95% CI = 0.11 – 1.86). By follow-up, participants in both conditions had lower HRSD scores than they did at intake (M = 15.8, SD = 11.7 for IPT; M = 12.0, SD = 12.3 for PSYCHOED) with no difference between them (B = 3.17, SE[B] = 3.54, β = .13, t = 0.90, p = 0.38).
3.5. Moderation of significant treatment effects
The interaction of treatment with minority status significantly predicted HRSD score at the end of group treatment (in prison; see Table 3), with a large effect size (Cohen's d = 1.22; 95% CI = .45 – 1.98). The difference between end-of-group depressive symptoms in the IPT and PSYCHOED conditions was larger for minority women than for non-minority women. We found no evidence that intake depression severity (HRSD score), antisocial personality disorder, borderline personality disorder, history of physical abuse, or history of sexual abuse moderated effects of treatment on in-prison depressive symptoms.
Table 3.
Minority status as a moderator of the effects of treatment on in-prison depressive symptoms (n = 38)
| Variable | B | SE(B) | β | t | p |
|---|---|---|---|---|---|
| Intake HRSD score | .71 | .19 | .48 | 3.80 | .001 |
| Treatment condition (+1/2 = IPT, -1/2 = PSYCHOED) | -12.04 | 2.79 | -.62 | -4.31 | .000 |
| Minority status (+1/2 = minority, -1/2 = non-minority) | 5.13 | 2.77 | .24 | 1.86 | .073 |
| Treatment condition*minority status | -19.25 | 5.62 | -.49 | -3.42 | .002 |
4. Discussion
This pilot study (n = 38) is the largest randomized treatment study of MDD in jails/prisons to date. Results suggested that group IPT is feasible and acceptable in a women's prison and that it resulted in lower in-prison depressive symptoms than did a credible, attention-matched control. Findings are notable because participants had severe and recurrent MDD, severe SUD, high rates of attempted suicide (40%), many comorbidities (including high rates of borderline and antisocial personality disorders), and complex social problems (including poverty and physical and sexual victimization). Findings are also notable because study treatment doses were small relative to the other services women in our study were receiving at the prison, including residential substance use treatment (for all women), individual mental health counseling (for some women), and antidepressant medications (for many women). In fact, IPT produced better in-prison depression outcomes despite patterns of medication use and other mental health treatment that should have biased the study in favor of the control condition (see Table 2).
Although control condition participants made improvements in the months after release from prison, IPT's quick (8-week) effect on MDD within prison is important because it may help reduce negative in-prison consequences of MDD (such as victimization, inability to complete correctional programs, and suicide attempts). IPT directly addresses the unusually high number of disruptive life events and conflicts experienced by incarcerated women. Addressing these stressors and reducing associated distress in prison may have important consequences. For example, prisoners who made serious suicide attempts reported interpersonal stressors (e.g., conflicts with spouse or other family members) shortly before the attempt (Daniel & Fleming, 2005).
The statistically and clinically significant moderation effects found in this study should be interpreted cautiously because of the small sample. However, the finding that IPT had a particularly strong effect on in-prison depressive symptoms among minority women is consistent with suggestions that members of many ethnic and racial minority groups in the United States may find relational (rather than an individual) approaches to problems to be more culturally congruent (Barrio, 2000; Campos et al., 2008). In fact, studies have found IPT to be feasible, culturally appropriate, and effective for depression in settings as diverse as rural Africa (Bolton et al., 2003).
Strong environmental influences may have overshadowed treatment effects as women left prison. In terms of group averages, the mean level of depressive symptoms in the control condition caught up with the experimental condition in the 3 months after release from prison. However, individual women's HRSD scores tended to fluctuate as they approached prison release and in the first 3 months after they left. HRSD scores for 68% of the sample changed by at least 7 points from the pre-release to the 3-month post-release assessment (with a correlation of .31 between the two scores in the overall sample). Change in HRSD scores ranged from a decrease of 31 points to an increase of 19 points during this time. Some women became less distressed as release to the community approached, but others became more distressed if they were worried about post-release housing or treatment arrangements. A variety of factors also seemed to affect mood after release. Some women returned to supportive family and friends while other women returned to conflictual or abusive ones. Some women were physically safe and others were homeless or lived with violence. Women received differing amounts of post-release substance use and mental health treatment as usual, ranging from residential treatment to nothing. Some women were able to maintain their sobriety and others were selling sex to support a heroin relapse. Women who are homeless, who live in violent neighborhoods, or who have violent partners may feel less safe in the community than they do in prison (Bradley & Davino, 2002). The varied environments to which women returned introduced within-subject and between-subject heterogeneity in post-release symptoms and functioning.
Both study treatments offered six weekly post-release sessions in an effort to help women weather the dramatic life changes they often experience as they return to the community and to bridge the gap between prison and other post-release services. The combination of these six sessions with the other services women received (see Table 2) resulted in good outcomes (HRSD < 8) at the 3-month post-release assessment for 45% of the sample. However, the other half of the sample could have benefited from additional post-release depression treatment. There are challenges to providing such treatment at sufficient intensity. Women leaving prison often have unreliable transportation and may return to communities hundreds of miles away. Therefore, continued in-person contact with prison providers is difficult. However, women often experience delays between prison release and linkage to community providers. Alternate methods of service delivery in the immediate post-release phase, such as phone treatment, might be helpful in delivering more intensive post-release treatment or providing additional counselor availability in times of crisis.
The limited exclusion criteria and addition of study treatments to prison treatment as usual increased the study's external validity. The 100% follow-up rate across assessments increased internal validity. However, results should be interpreted with caution because the small sample precluded modeling wave-level effects. In addition, the sample was too small and the follow-up period too short to test other potentially important outcomes (e.g., prison suicide attempts, recidivism) meaningfully. Furthermore, although substance use relapse rates looked as if they might be trending in the right direction (in favor of less relapse for women in the IPT condition), it is impossible to know if this is the case without a larger study with better power to test dichotomous effects, especially since 26% of the current sample spent the entire follow-up period in a controlled environment (residential treatment). Finally, it is possible that non-specific factors accounted for the decrease in depressive symptoms during incarceration for IPT condition compared to the matched attention placebo condition. However, both conditions received high doses of other group treatment (e.g., 16-30 hours per week), which suggests that it was unlikely that non-specific factors primarily or entirely accounted for results.
The fact that this small pilot is the largest randomized treatment study of MDD in jails/prisons to date highlights a desperate need for more treatment research for this vulnerable and understudied population. Most research on treatments for correctional populations has focused on reducing substance use and criminal behavior (e.g., Leukefeld et al., 2011; Pallone, 2004); little has addressed identification and implementation of effective mental health treatments. Research on the effectiveness of correctional mental health treatments is vital because mental health disorders are prevalent in these settings (Fazel & Denesh, 2002; James & Glaze, 2006). Little is known about how correctional contexts and population characteristics affect the outcomes of standard mental health treatments. For example, substance use and medical comorbidities (Fazel & Baillargeon, 2011; Hills, 2000; Jordan et al., 1996; Teplin et al., 1996); complex social circumstances (e.g., unemployment, poverty); training level and turn-over rate of prison treatment staff (e.g., many front-line counselors have only bachelor's degrees); and context-specific issues such as mental health stigma and potential consequences of disclosure of mental health problems (e.g., being put in isolation by the facility or being targeted or ostracized by other inmates) may impact the effectiveness and reach of mental health treatments within correctional settings. More research on correctional mental health treatment is needed, especially for women, who enter the correctional system with different psychosocial stressors (e.g., intimate partner violence, child care concerns) and more mental health morbidity (e.g., MDD, posttraumatic stress disorder) than do men (Browne et al., 1999; Zlotnick et al., 2008).
Acknowledgments
Role of Funding Source. This study was funded by the United States National Institute of Drug Abuse (NIDA; K23DA021159, PI: Johnson). NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors. Dr. Johnson, in continuing close consultation with Dr. Zlotnick, designed the study, wrote the protocol, conducted the study, conducted the analysis, and wrote the manuscript.
Contributor Information
Jennifer E. Johnson, Brown University, Providence, RI USA
Caron Zlotnick, Brown University and Butler Hospital, Providence, RI USA.
References
- Aharonovich E, Liu X, Nunes E, Hasin DS. Suicide attempts in substance abusers: Effects of major depression in relation to substance use disorders. American Journal of Psychiatry. 2002;159:1600–1602. doi: 10.1176/appi.ajp.159.9.1600. [DOI] [PubMed] [Google Scholar]
- Babor TF, Stephens RS, Marlatt GA. Verbal report methods in clinical research on alcoholism: Response bias and its minimization. Journal of Studies on Alcohol. 1987;48:410–424. doi: 10.15288/jsa.1987.48.410. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Binswanger IA, Penn JV, Murray OW, Williams BA. Psychiatric disorders and repeat incarcerations: The revolving prison door. American Journal of Psychiatry. 2009a;166:103–109. doi: 10.1176/appi.ajp.2008.08030416. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Williams BA, Mellow J, Harzke AJ, Hoge SK, Baillargeon G, Greifinger RB. Parole revocation among prison inmates with psychiatric and substance use disorders. Psychiatric Services. 2009b;60:1516–1521. doi: 10.1176/appi.ps.60.11.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrio C. The cultural relevance of community support programs. Psychiatric Services. 2001;51:879–884. doi: 10.1176/appi.ps.51.7.879. [DOI] [PubMed] [Google Scholar]
- Bech P. Rating scales for affective disorders: Their validity and consistency. Acta Psychiatrica Scandinavica. 1981;64(Suppl 295):S11–101. [PubMed] [Google Scholar]
- Benda BB. Gender differences in life-course theory of recidivism: A survival analysis. International Journal of Offender Therapy and Comparative Criminology. 2005;49:325–342. doi: 10.1177/0306624X04271194. [DOI] [PubMed] [Google Scholar]
- Blitz C, Wolff N, Shi J. Physical victimization in prison: The role of mental illness. International Journal of Law and Psychiatry. 2008;31:385–393. doi: 10.1016/j.ijlp.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, Speelman L, Ndogoni L, Weissman M. Group interpersonal psychotherapy for depression in rural Uganda: A randomized controlled trial. Journal of the American Medical Association. 2003;289(23):3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Bonner R, Rich AR. Psychosocial vulnerability, life stress, and suicide ideation in a jail population: A cross-validation study. Suicide and Life-Threatening Behavior. 1990;20:213–224. [PubMed] [Google Scholar]
- Borkovec TD. Between-group therapy outcome research: Design and methodology. NIDA Research Monograph. 1993;137:249–289. [PubMed] [Google Scholar]
- Bottlender M, Soyka M. Efficacy of an Intensive Outpatient Rehabilitation Program in Alcoholism: Predictors of Outcome 6 Months after Treatment. European Addiction Research. 2005;11:132–137. doi: 10.1159/000085548. [DOI] [PubMed] [Google Scholar]
- Bradley RG, Davino KM. Women's perceptions of the prison environment: When prison is “the safest place I've ever been.”. Psychology of Women Quarterly. 2002;26:351–359. [Google Scholar]
- Brady TM, Krebs CP, Laird G. Psychiatric comorbidity and not completing jail-based substance abuse treatment. American Journal on Addiction. 2004;13:83–101. doi: 10.1080/10550490490265398. [DOI] [PubMed] [Google Scholar]
- Brinded P, Simpson AIF, Laidlaw TM, Fairley N, Malcom F. Prevalence of psychiatric disorders in New Zealand prisons: A national study. Australian and New England Journal of Psychiatry. 2001;35:166–173. doi: 10.1046/j.1440-1614.2001.00885.x. [DOI] [PubMed] [Google Scholar]
- Broadhead W, Blazer D, George L, Tse C. Depression, disability days and days lost from work in a prospective epidemiological survey. Journal of the American Medical Association. 1990;264:2524–2528. [PubMed] [Google Scholar]
- Brooner RK, King VL, Kidorf M, Schmidt CW, Jr, Bigelow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Archives of General Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- Brown RA, Evans DM, Miller IW, Burgess ES, Mueller TI. Cognitive-behavioral treatment for depression in alcoholism. Journal of Consulting and Clinical Psychology. 1997;65:715–726. doi: 10.1037//0022-006x.65.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Monti PM, Myers MG, Martin RA, Rivinus T, Dubreuil ME, Rohsenow DJ. Depression among cocaine abusers in treatment: Relation to cocaine and alcohol use and treatment outcome. American Psychiatric Association. 1998;155:220–225. doi: 10.1176/ajp.155.2.220. [DOI] [PubMed] [Google Scholar]
- Brown S, Day A. The role of loneliness in prison suicide prevention and management. Journal of Offender Rehabilitation. 2008;47:433–449. [Google Scholar]
- Brown SA, Inaba RK, Gilin JC, Schuckit MA, Stewart MA, Irwin MR. Alcoholism and affective disorder: Clinical course of depressive symptoms. American Journal of Psychiatry. 1995;152:45–52. doi: 10.1176/ajp.152.1.45. [DOI] [PubMed] [Google Scholar]
- Browne A, Miller B, Maguin E. Prevalence and severity of lifetime physical and sexual victimization among incarcerated women. International Journal of Law and Psychiatry. 1999;22:301–322. doi: 10.1016/s0160-2527(99)00011-4. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Fenton LR, Ball SA, et al. Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatients. Archives of General Psychiatry. 2004;61:264–272. doi: 10.1001/archpsyc.61.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Rounsaville BJ. Differential symptom reduction in depressed cocaine abusers treatment with psychotherapy and pharmacotherapy. Journal of Nervous and Mental Disease. 1995;183:251–259. doi: 10.1097/00005053-199504000-00012. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Gawin FH. A comparative trial of psychotherapies for ambulatory cocaine abusers: Relapse prevention and interpersonal psychotherapy. American Journal of Drug and Alcohol Abuse. 1991;17:229–257. doi: 10.3109/00952999109027549. [DOI] [PubMed] [Google Scholar]
- Campanini RFB, Schoedl AF, Pupo MC, Costa ACH, Krupnick JL, Mello MF. Efficacy of interpersonal therapy-group format adapted to post-traumatic stress disorder: An open-label add-on trial. Depression and Anxiety. 2010;27:72–77. doi: 10.1002/da.20610. [DOI] [PubMed] [Google Scholar]
- Campos B, Schetter CD, Abdou CM, Hobel CJ, Glynn LM, Sandman CA. Familialism, social support, and stress: Positive implications for pregnant Latinas. Cultural Diversity and Ethnic Minority Psychology. 2008;14:155–162. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles DR, Abram KM, McClelland GM, Teplin LA. Suicidal ideation and behavior among women in jail. Journal of Contemporary Criminal Justice. 2003;19:65–81. [Google Scholar]
- Daniel A, Fleming J. Serious suicide attempts in a state correctional system and strategies to prevent suicide. The Journal of Psychiatry and Law. 2005;33:227–247. [Google Scholar]
- DeLisio G, Maremmani I, Perugi G. Impairment of work and leisure in depressed outpatients. Journal of Affective Disorders. 1986;10:346–349. doi: 10.1016/0165-0327(86)90029-7. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Civita MD, Paraherakis A, Gill K. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction. 2002;97:347–356. doi: 10.1046/j.1360-0443.2002.00083.x. [DOI] [PubMed] [Google Scholar]
- DuRand CJ, Burtka GJ, Federman EJ, Haycox JA, Smith JW. A quarter century of suicide in a major urban jail: Implications for community psychiatry. American Journal of Psychiatry. 1995;152:1077–1080. doi: 10.1176/ajp.152.7.1077. [DOI] [PubMed] [Google Scholar]
- Elkin I, Shea MT, Watkins JT, Imber SD, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program: General effectiveness of treatments. Archives of General Psychiatry. 1989;46:971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- Enos S. Mothering from the inside: Parenting in a women's prison. SUNY Press; New York: 2001. [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Frietas TT, McFarlin SK, Rutigliano P. The Timeline Followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Fazel S, Baillargeon J. The health of prisoners. Lancet. 2011;377(9769):956–965. doi: 10.1016/S0140-6736(10)61053-7. [DOI] [PubMed] [Google Scholar]
- Fazel S, Danesh J. Serious mental disorder in 23,000 prisoners: A systematic review of 62 surveys. Lancet. 2002;359:545–550. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- Fazel S, Benning R. Suicides in female prisoners in England and Wales, 1978-2004. The British Journal of Psychiatry. 2009;194:183–184. doi: 10.1192/bjp.bp.107.046490. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition. Biometrics Research Department. 1996a [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM Axis II Personality Disorders. Biometrics Research Department; New York: 1996b. [Google Scholar]
- Frank E, Spanier C. Interpersonal psychotherapy for depression: Overview, clinical efficacy, and future directions. Clinical Psychology: Science and Practice. 1995;2:349–369. [Google Scholar]
- Frank E, Kupfer DJ, Wagner EF, McEachran AB, Cornes C. Efficacy of interpersonal psychotherapy as a maintenance treatment of recurrent depression: Contributing factors. Archives of General Psychiatry. 1991;48:1053–1059. doi: 10.1001/archpsyc.1991.01810360017002. [DOI] [PubMed] [Google Scholar]
- Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. American Journal of Public Health. 2005;95:1725–1736. doi: 10.2105/AJPH.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia Coll C, Surrey JL, Buccio-Notaro P, Molla B. Incarcerated mothers: Crimes and punishments. In: Coll CG, Surrey JL, Weingarten E, editors. Mothering against the odds: Diverse voices of contemporary mothers. Guilford; New York: 1998. pp. 255–274. [Google Scholar]
- Genty PM. Permanency planning in the context of parental incarceration: Legal issues and recommendations. In: Seymour C, Hairston CF, editors. Children with parents in prison: Child welfare policy, program, and practice issues. Transaction Publishers; New Brunswick: 2001. pp. 75–92. [Google Scholar]
- Gerra G, Leonardi C, D'Amore A, Strepparola G, Fagetti R, Assi C, Zaimovic A, Lucchini A. Buprenorphine treatment outcome in dually diagnosed heroin dependent patients: A retrospective study. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2006;30:265–272. doi: 10.1016/j.pnpbp.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: Results of a national survey of adults. Journal of Substance Abuse. 1995;7:481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorder and independent mood and anxiety disorders. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Gray A, Saum CA. Mental health, gender, and drug court completion. American Journal of Criminal Justice. 2005;30:55–69. [Google Scholar]
- Greenfeld LA, Snell TL. Women Offenders: U.S. Department of Justice, Bureau of Justice Statistics (NCJ 175688) BJS Clearinghouse; Washington, DC: 1999. [Google Scholar]
- Green B. Trauma History Questionnaire. In: Stamm B, editor. Measurement of stress, trauma, and adaptation. Sidran Press; Lutherville, MD: 1996. pp. 366–369. [Google Scholar]
- Hamilton M. Rating depressive patients. Journal of Clinical Psychiatry. 1980;41:21–24. [PubMed] [Google Scholar]
- Hammen C. Depression runs in families: The social context of risk and resilience in children of depressed mothers. Springer-Verlag; New York: 1999. [Google Scholar]
- Hasin DS, Grant BF. Major depression in 6,050 former drinkers. Archives of General Psychiatry. 2002;59:794–800. doi: 10.1001/archpsyc.59.9.794. [DOI] [PubMed] [Google Scholar]
- Hayes LM, Rowan JR. National study of jail suicides: Seven years later. National Center for Institutions and Alternatives; Mansfield, MA: 1988. [Google Scholar]
- Hickert A, Boyle SW, Tollefson DR. Factors that predict drug court completion and drop out: Findings from an evaluation of Salt Lake County's adult felony drug court. Journal of Social Service Research. 2009;35:149–162. [Google Scholar]
- Hiller M, Knight K, Simpson D. Risk factors that predict dropout from corrections-based treatment for drug abuse. The Prison Journal. 1999;79:411–430. [Google Scholar]
- Hills HA. Creating effective treatment programs for persons with co-occurring disorders in the justice system (GAINS Center monograph) The GAINS Center; Delmar, NY: 2000. [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Unipolar depression, life context vulnerabilities, and drinking to cope. Journal of Consulting and Clinical Psychology. 2004;72:269–275. doi: 10.1037/0022-006X.72.2.269. [DOI] [PubMed] [Google Scholar]
- Holtfreter K, Morash M. The needs of women offenders: Implications for correctional programming. Women and Criminal Justice. 2003;14:137–160. [Google Scholar]
- Hser YI, Grella CE, Hsieh SC, Anglin MD, Brown BS. Prior treatment experience related to process and outcomes in DATOS. Drug and Alcohol Dependence. 1999;57:137–150. doi: 10.1016/s0376-8716(99)00081-2. [DOI] [PubMed] [Google Scholar]
- Hurley W, Dunne MP. Psychological distress and psychiatric morbidity in women prisoners. Australian and New Zealand Journal of Psychiatry. 1991;25:461–470. doi: 10.3109/00048679109064439. [DOI] [PubMed] [Google Scholar]
- James D, Glaze LE. Mental Health Problems of Prison and Jail Inmates. Bureau of Justice Statistics Special Report. 2006 [Google Scholar]
- Joe GW, Brown BS, Simpson DD. Psychological problems and client engagement in methadone treatment. Journal of Nervous and Mental Disease. 1995;183:704–710. doi: 10.1097/00005053-199511000-00006. [DOI] [PubMed] [Google Scholar]
- Johnson JE, Esposito-Smythers C, Miranda R, Justus AN, Rizzo C, Clum G. Gender, social support, and distress in criminal justice involved adolescents. International Journal of Offender Therapy and Comparative Criminology. 2011;55:1096–1109. doi: 10.1177/0306624X10382637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, O'Leary CC, Striley CW, Ben Abdallah A, Bradford S, Cottler LB. Effects of major depression on crack use and arrests among women in drug court. Addiction. 2011;106:1279–1286. doi: 10.1111/j.1360-0443.2011.03389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Zlotnick C. A pilot study of group interpersonal psychotherapy for depression in substance-abusing female prisoners. Journal of Substance Abuse Treatment. 2008;34:371–377. doi: 10.1016/j.jsat.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women: II. Convicted felons entering prison. Archives of General Psychiatry. 1996;53:513–519. doi: 10.1001/archpsyc.1996.01830060057008. [DOI] [PubMed] [Google Scholar]
- Keaveny M, Zauszniewski JA. Life events and psychological well-being in women sentenced to prison. Issues in Mental Health Nursing. 1999;20:73–89. doi: 10.1080/016128499248790. [DOI] [PubMed] [Google Scholar]
- Keitner G, Miller I. Family functioning in major depression: An overview. American Journal of Psychiatry. 1990;147:1128–1137. doi: 10.1176/ajp.147.9.1128. [DOI] [PubMed] [Google Scholar]
- Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression: Remission and beyond. Journal of the American Medical Association. 2003;289:3152–3160. doi: 10.1001/jama.289.23.3152. [DOI] [PubMed] [Google Scholar]
- Klein DN, Santiago NJ. Dysthymia and chronic depression: Introduction, classification, risk factors, and course. Journal of Clinical Psychology/In Session. 2003;59:807–816. doi: 10.1002/jclp.10174. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Rounsaville BJ, Kleber HD. A 2.5 year follow-up of depression, life crises, and treatment effects on abstinence among opioid addicts. Archives of General Psychiatry. 1986;43:733–738. doi: 10.1001/archpsyc.1986.01800080019003. [DOI] [PubMed] [Google Scholar]
- Krupnick JL, Green BL, Stockton P, Miranda J, Krause E, Mete M. Group interpersonal psychotherapy for low-income women with posttraumatic stress disorder. Psychotherapy Research. 2008;18:497–507. doi: 10.1080/10503300802183678. [DOI] [PubMed] [Google Scholar]
- Leukefeld C, Gullotta TP, Gregrich J. Handbook of evidence-based substance abuse treatment in criminal justice settings. Springer Press; 2011. [Google Scholar]
- Levkovitz Y, Shahar G, Native G, Hirsfeld IT, Krieger I, Fennig S. Group interpersonal psychotherapy for patients with major depression disorder – pilot study. Journal of Affective Disorders. 2000;60:191–195. doi: 10.1016/s0165-0327(99)00181-0. [DOI] [PubMed] [Google Scholar]
- Liau AK, Shively R, Horn M, Laudau J, Barriga A, Gibbs JC. Effects of psychoeducation for offenders in a community correctional facility. Journal Community Psychology. 2004;32:543–558. [Google Scholar]
- Marcus D, Hamlin RJ, Lyons PM. Negative affect and interpersonal rejection among prison inmates in a therapeutic community: A social relations analysis. Journal of Abnormal Psychology. 2001;110:544–552. doi: 10.1037//0021-843x.110.4.544. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Kocsis JH, Christos P, Bleiberg K, Carlin A. Pilot study of interpersonal psychotherapy versus supportive psychotherapy for dysthymic patients with secondary alcohol abuse or dependence. Journal of Nervous and Mental Disease. 2008;196:468–474. doi: 10.1097/NMD.0b013e31817738f1. [DOI] [PubMed] [Google Scholar]
- McDaniels-Wilson C, Belknap J. The extensive sexual violation and sexual abuse histories of incarcerated women. Violence Against Women. 14:1090–1127. doi: 10.1177/1077801208323160. [DOI] [PubMed] [Google Scholar]
- McKay JR, Pettinati HM, Morrison R, Feeley M, Mulvaney FD, Gallop R. Relation of depression diagnoses to 2-year outcomes in cocaine-dependent patients in a randomized continuing care study. Psychology of Addictive Behaviors. 2002;16:225–235. [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addictive Behaviors. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Nunes EV, Quitken FM, Donovan SJ, Deliyannides D, Ocepek-Welikson K, Koenig T, Brady R, McGrath PJ, Woody G. Imipramine treatment of opiate-dependent patients with depressive disorders: A placebo-controlled trial. Archives of General Psychiatry. 1998;55:153–160. doi: 10.1001/archpsyc.55.2.153. [DOI] [PubMed] [Google Scholar]
- O'Sullivan K, Rynne C, Miller J, O'Sullivan S, Fitzpatrick V, Hux M, Cooney J, Clare A. A follow-up study on alcoholics with and without co-existing affective disorder. British Journal of Psychiatry. 1988;152:813–819. doi: 10.1192/bjp.152.6.813. [DOI] [PubMed] [Google Scholar]
- Pallone LC. Treating substance abusers in correctional contexts: New Understandings, new modalities. Routledge. 2004 [Google Scholar]
- Parsons ML, Warner-Robbins C. Factors that support women's successful transition to the community following jail/prison. Health Care for Women International. 2002;23:6–18. doi: 10.1080/073993302753428393. [DOI] [PubMed] [Google Scholar]
- Pelc I, Asons C, Lehert P. The European NEAT Program: An integration approach using acamprosate and psychosocial support for the prevention of relapse among alcohol-dependent patients with a statistical modeling of therapy success prediction. Alcoholism: Clinical and Experimental Research. 2002;26:1529–1538. doi: 10.1097/01.ALC.0000029584.62149.22. [DOI] [PubMed] [Google Scholar]
- Pelissier B, O'Neil JA. Antisocial personality and depression among incarcerated drug treatment participants. Journal of Substance Abuse. 2000;11:379–393. doi: 10.1016/s0899-3289(00)00034-1. [DOI] [PubMed] [Google Scholar]
- Rehm LP, O'Hara MW. Item characteristics of the Hamilton Rating Scale for Depression. Journal of Psychiatric Research. 1985;19:31–41. doi: 10.1016/0022-3956(85)90066-4. [DOI] [PubMed] [Google Scholar]
- Richardson K, Baillie A, Reid S, Morley K, Teesson M, Sannibale C, Weltman M, Haber P. Do acamprosate or naltrexone have an effect on daily drinking by reducing craving for alcohol? Addiction. 2008;103:953–959. doi: 10.1111/j.1360-0443.2008.02215.x. [DOI] [PubMed] [Google Scholar]
- Rossello J, Bernal G, Rivera-Medina C. Individual and group CBT and IPT for Puerto Rican adolescents with depressive symptoms. Cultural Diversity and Ethnic Minority Psychology. 2008;14(3):234–245. doi: 10.1037/1099-9809.14.3.234. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ. Treatment of cocaine dependence and depression. Biological Psychiatry. 2004;56:803–809. doi: 10.1016/j.biopsych.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Archives of General Psychiatry. 1987;44:505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Glazer W, Wilber CH, Weissman MM, Kleber HD. Short-term interpersonal psychotherapy in methadone-maintained opiate addicts. Archives of General Psychiatry. 1983;40:629–636. doi: 10.1001/archpsyc.1983.04390010039005. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Kosten TR, Weissman MM, Kleber HD. Prognostic significance of psychopathology in treated opiate addicts. Archives of General Psychiatry. 1986a;43:739–745. doi: 10.1001/archpsyc.1986.01800080025004. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Kosten TR, Weissman MM, Kleber HD. A 2.5-year follow-up of short-term interpersonal psychotherapy in methadone-maintained opiate addicts. Comprehensive Psychiatry. 1986b;27:201–210. doi: 10.1016/0010-440x(86)90041-6. [DOI] [PubMed] [Google Scholar]
- Sabol W, West HC, Cooper M. Prisoners in 2008: Bureau of Justice Statistics, U.S. Department of Justice. 2009.
- Sacks JY, Kressel D. Measuring client progress in treatment: The Client Assessment Inventory (CAI). Paper presented at the CJ-DATS Steering Committee Meeting on April 4-5; Washington, DC. April, 2005. [Google Scholar]
- Sarchiapone M, Jovanovic N, Roy A, Podlesek A, Carli V, Amore M, Mancini M, Marusic A. Relations of psychological characteristics to suicide behavior: Results from a large sample of male prisoners. Personality and Individual Differences. 2009;47:250–255. [Google Scholar]
- Shea MT, Elkin I, Imber SD, Sotsky SM, et al. Course of depressive symptoms over follow-up. Findings from the National Institute of Mental Health Treatment of Depression Collaborative Research Program. Archives of General Psychiatry. 1992;49:782–787. doi: 10.1001/archpsyc.1992.01820100026006. [DOI] [PubMed] [Google Scholar]
- Simpson DD. Research updates: Performance indicators and targeted interventions studies. CJ-DATS Steering Committee Meeting; Washington, DC. 2005. [Google Scholar]
- Simpson DD, Knight K, Dansereau DF. Addiction treatment strategies for offenders. Journal of Community Corrections. 2004;8:7–10. 27–32. [Google Scholar]
- Siqueland L, Crits-Christoph P, Gallop R. Retention in psychosocial treatment of cocaine dependence: Predictors and impact on outcome. The American Journal on Addictions. 2002;11:240–40. doi: 10.1080/10550490252801611. [DOI] [PubMed] [Google Scholar]
- Skeem J, Louden JE, Manchak S, Haddad E, Vidal S. Social networks and social control of probationers with co-occurring mental and substance abuse problems. Law and Human Behavior. 2009;33:122–135. doi: 10.1007/s10979-008-9140-1. [DOI] [PubMed] [Google Scholar]
- Snell T. Women in prison. U.S. Department of Justice, Bureau of Justice Statistics. BJS Clearinghouse; Washington, DC: 1994. [Google Scholar]
- Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug and Alcohol Dependence. 1996;42:49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy. 1980;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Validity of self-reports in three populations of alcoholics. Journal of Consulting and Clinical Psychology. 1978;46:901–907. doi: 10.1037//0022-006x.46.5.901. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students’ recent drinking history: Utility for alcohol research. Addictive Behaviors. 1986;11:149–161. doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Vanderspek R. Relationship between clinical judgment, self-report, and . (1979 )breath-analysis measures of intoxication in alcoholics. Journal of Consulting and Clinical Psychology. 1979;47:204–206. doi: 10.1037//0022-006x.47.1.204. [DOI] [PubMed] [Google Scholar]
- Talbot NL, Chaudron LH, Ward EA, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed women with sexual abuse histories. Psychiatric Services. 2011;62:374–380. doi: 10.1176/appi.ps.62.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taxman F, Young D, Tesluk P, Mitchell S, Wainright J, Ormond J, Decelles K, Carson J, Rhodes A. The National Survey of Criminal Justice Treatment Practices: preliminary findings of the prevalence of state-based offender services, importance of offender programming, and systems development issues.. Paper presented at the CJ-DATS Steering Committee Meeting; Washington, DC. April 2005. [Google Scholar]
- Teplin LA, Abram KM, McClelland GM. Prevalence of psychiatric disorders among incarcerated women: I. Pretrial jail detainees. Archives of General Psychiatry. 1996;53:505–512. doi: 10.1001/archpsyc.1996.01830060047007. [DOI] [PubMed] [Google Scholar]
- Thase ME, Salloum IM, Cornelius JD. Comorbid alcoholism and depression: Treatment issues. Journal of Clinical Psychiatry. 2001;62:32–41. [PubMed] [Google Scholar]
- Tusher CP, Cook CL. Comparing revictimization in two groups of marginalized women. Journal of Interpersonal Violence. 2010;25:1893–1911. doi: 10.1177/0886260509354513. [DOI] [PubMed] [Google Scholar]
- Varese T, Pelowski S, Riedel H, Heiby EM. Assessment of cognitive-behavioral skills and depression among female prison inmates. European Journal of Psychological Assessment. 1998;14(2):141–145. [Google Scholar]
- Wang J, Patten SB. A prospective study of sex-specific effects of major depression on alcohol consumption. Canadian Journal of Psychiatry. 2001;46:422–425. doi: 10.1177/070674370104600507. [DOI] [PubMed] [Google Scholar]
- Wang J, Patten SB. Prospective study of frequent heavy alcohol use and the risk of major depression in the Canadian general population. Depression and Anxiety. 2002;15:42–45. doi: 10.1002/da.1084. [DOI] [PubMed] [Google Scholar]
- Weinberger A, McKee SA, Mazure CM. Inclusion of Women and Gender-Specific Analyses in Randomized Clinical Trials of Treatments for Depression. Journal of Women's Health. 2010;19:1727–1732. doi: 10.1089/jwh.2009.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Paykel ES, Prusoff B, Hanson B. Treatment effects on the social adjustment of depressed patients. Archives of General Psychiatry. 1974;30:771–778. doi: 10.1001/archpsyc.1974.01760120033006. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JC, Klerman GL. Comprehensive guide to interpersonal psychotherapy. Basic Books; New York: 2000. [Google Scholar]
- Whisman MA, Strosahl K, Fruzzetti AE, Schmaling KB, Jacobson NS, Miller DM. A structured interview version of the Hamilton Rating Scale for Depression: reliability and validity. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:238–241. [Google Scholar]
- Wilfley DE, MacKenzie KR, Welch RR, Ayres VE, Weissman MM. Interpersonal psychotherapy for group. Basic Books; New York: 2000. [Google Scholar]
- Wilson G. Psychotherapy with depressed incarcerated felons: A comparative evaluation of treatments. Psychological Reports. 1990;67:1027–1041. doi: 10.2466/pr0.1990.67.3.1027. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Clarke JG, Friedmann PD, Roberts MB, Sacks S, Melnick G. Gender differences in comorbid disorders among offenders in prison substance abuse treatment programs. Behavioral Sciences and the Law. 2008;26:402–412. doi: 10.1002/bsl.831. [DOI] [PMC free article] [PubMed] [Google Scholar]