Abstract
Background: Laser therapy has been proposed as a physical therapy for musculoskeletal disorders and has attained popularity because no side effects have been reported after treatment. However, its true effectiveness is still controversial because several clinical trials have reported the ineffectiveness of lasers in treating pain. Methods: In this systematic review, we investigate the clinical effectiveness of low-level laser therapy (LLLT) on joint pain. Clinical trials on joint pain satisfying the following conditions are included: the laser is irradiated on the joint area, the PEDro scale score is at least 5, and the effectiveness of the trial is measured using a visual analogue scale (VAS). To estimate the overall effectiveness of all included clinical trials, a mean weighted difference in change of pain on VAS was used. Results: MEDLINE is the main source of the literature search. After the literature search, 22 trials related to joint pain were selected. The average methodological quality score of the 22 trials consisting of 1014 patients was 7.96 on the PEDro scale; 11 trials reported positive effects and 11 trials reported negative effects. The mean weighted difference in change of pain on VAS was 13.96 mm (95% CI, 7.24–20.69) in favor of the active LLLT groups. When we only considered the clinical trials in which the energy dose was within the dose range suggested in the review by Bjordal et al. in 2003 and in World Association for Laser Therapy (WALT) dose recommendation, the mean effect sizes were 19.88 and 21.05 mm in favor of the true LLLT groups, respectively. Conclusions: The review shows that laser therapy on the joint reduces pain in patients. Moreover, when we restrict the energy doses of the laser therapy into the dose window suggested in the previous study, we can expect more reliable pain relief treatments.
Introduction
Low-level laser therapy (LLLT) has been used for >30 years for pain relief, and has become increasingly popular because it is a noninvasive and nonthermal treatment.1 And although many studies using laser therapy have been conducted pertaining to the improvement of pain relief for various musculoskeletal conditions, the true effectiveness of this therapy is still controversial,2 as the number of clinical trials reporting ineffectiveness is also significant; there is also a possibility that several ineffective trials might not have been reported. Hence, laser therapies have yet to receive United States Food and Drug Administration (FDA) approval, except for the treatment of carpal tunnel syndrome.3 One reason for the different outcomes in effectiveness might be the result of factors affecting the effectiveness of laser therapy. These factors can include patient diagnoses, symptoms, pain duration, laser irradiation location, distance from laser probe to skin, laser type (HeNe, GaAs, GaAsAl, Nd:YAG), wavelength, laser mode (continuous, pulsed), average power (mW), power density (mW/cm2), energy (J), energy dose (J/cm2), number of sessions, laser irradiation point size (cm2), and co-interventions (exercises, analgesics, nonsteroidal anti-inflammatory drugs [NSAIDs], and conventional physical therapies).
Studies attempting to explain mechanisms for pain relief from laser therapies have typically been based on anti-inflammatory effects4 or the laser's activity on the immune system.5 In a systematic review of LLLT for use in joint diseases by Bjordal et al.,6 it was reported that one of the main causes of joint disease is inflammation, and that LLLT is effective for anti-inflammation. They then hypothesized that an important factor for the treatment of joint disease is the LLLT energy dose. The study reported the use of LLLT location-specific energy doses on chronic joint disorders based on both previous laboratory trials and anatomical factors. This systematic review showed that LLLT can be effective for joint disease if the energy dose is properly selected such that it inhibits inflammatory activity in the joint capsule.
Although joint pain can be controlled by medications such as acetaminophen,8 NSAIDs,9 and corticosteroid injections,10 some patients are reluctant to use them because of the potential side effects.11 In some cases, surgery is also conducted to repair damaged joints, although surgery does not always bring satisfying results.12 For treatment of these types of joint problems, alternative treatments or physical therapies including exercise,13 electrical stimulation,14 acupuncture,15 laser acupuncture, and LLLT16 can be used.
Therefore, the primary objective of this study is to investigate the effectiveness of laser therapy by analyzing previous clinical trials for common patient conditions; that is, patients suffer pain in joint regions and laser irradiation is used as the treatment on joint areas. As the basis of this study, we conducted a literature search for randomized controlled clinical trials on joint areas, and selected 22 articles. Among the various joint areas investigated, our study includes finger joints, temporomandibular joints (TMJ), glenohumeral joints, knee joints, and cervical and lumbar spinal regions. Joint pain in these areas can be caused by osteoarthritis, rheumatoid arthritis, or other conditions. Note that osteoarthritis is associated with the degeneration of cartilage in the joint and is the most common cause of joint pain in people older than 60 years.17 Rheumatoid arthritis is an autoimmune and systemic inflammatory disorder;7 it affects synovial joints such as those in fingers, wrists, and knees.
The second objective of our study is to investigate whether we can obtain improved pain relief when certain energy doses are applied. Our study contains 15 studies not included in Bjordal et al.6; using these data, we subsequently validate their proposed energy doses.
Materials and Methods
Literature search
MEDLINE and PubMed were the main sources of searching for previous clinical trials. The following keywords were used to find instances of joint pain: musculoskeletal, rheumatoid, arthritis, osteoarthritis, temporomandibular, cervical, neck, hand, finger, wrist, shoulder, back, low back, knee, spine, and pain. These keywords were then combined with the following keywords: laser, laser therapy, and laser irradiation, and references pertaining to existing publications of laser therapies were also examined. Among the literature collected, clinical trials were first selected by excluding publications involving animal experiments, in vitro experiments, and reviews, by examining titles and abstracts. Some clinical trials were also excluded if we failed to obtain their full text, as the abstract did not provide enough relevant information to assess the quality of the methodology used. The literature search is current to the end of May 2011.
Types of studies
Studies were restricted to randomized controlled trials (RCTs). Clinical trials for assessing the pain relief effect of laser therapy between true laser treatment groups and placebo laser treatment groups were included; trials not having placebo laser groups were excluded because it is necessary to compare the results of the true laser therapy group with the results of the placebo laser therapy group in order to determine the true effectiveness of the laser therapy. Crossover-type studies were excluded because the results of the experiments were deemed to be less reliable. Because of concerns about the systematic effects of laser therapy, trials that used a counterpart of the body as the control group were also excluded. Finally, trials that compare laser treatments with other types of interventions (cryotherapy, acupuncture, electro-acupuncture, electrical stimulation, ultrasound therapy) were subsequently excluded.
Patient characteristics
Patients suffering pain in joint areas were the target of our study. However, although patients suffered pain in their joints, trials for patients with myofascial pain, radiculopathy, or tendinitis were excluded because the source of the pain may not be related to joint pain.
Type of interventions
Clinical trials containing at least one irradiation point on the joint area were included. Clinical trials with co-interventions such as exercises, analgesics, and hot packs were also included. In addition, trials with noninvasive laser irradiation were included; intravascular types of laser irradiation were excluded.18
Clinical trial quality assessment
To assess the quality of the clinical trials, 10 methodological criteria of the PEDro scale were used.19 This scale was developed by the PEDro database of physiotherapy trials. Two assessors independently assessed the trials using the PEDro scale. If the quality score of a study was<5, the study was excluded.
Outcome measure of pain relief effect
Studies include clinical trials that reported at least one subjective pain measure that was the same as or similar to the 0–10 cm visual analogue scale (VAS). In cases in which the pain measure scale was different from the usual VAS scale in which 0 cm denotes no pain and 10 cm denotes severe pain, values were transformed into the usual scale. When the study reported several aspects of pain (i.e., pain on rest, pain on movement, pain on function, or pain on activity), pain on movement, function, or activity was chosen rather than pain on rest.
Inferences of missing parameters
When the clinical trial did not describe the parameters of laser therapy, parameter values were inferred from the relations among laser parameter factors. For example, power density (mW/cm2), energy density (J/cm2), size of irradiation area (cm2), and irradiation time (sec) were inferred from the following relations.
 |
Effect size and pooling of effect size
The mean value of each group was first calculated using the difference between the pretreatment VAS value for pain and the post-treatment VAS value for pain. Then, the effect size was calculated using the difference between the mean value of the true laser group and the mean value of the placebo laser group. The following equation is the formulation of the effect size for each clinical trial.
 |
To calculate the mean effect size of several clinical trials, the weighted mean difference (WMD) can be used. To calculate the WMD, variance of the effect size is required; in this study, using the method described by Bjordal et al.,6 the sample variances of the post-treatment values were used as the effect size variance. Then, the mean effect size was calculated using the random-effect model. We used the “metafor” package from R20 to calculate the pooled estimate, and to draw a forest tree and publication bias plot.
Results
Literature search
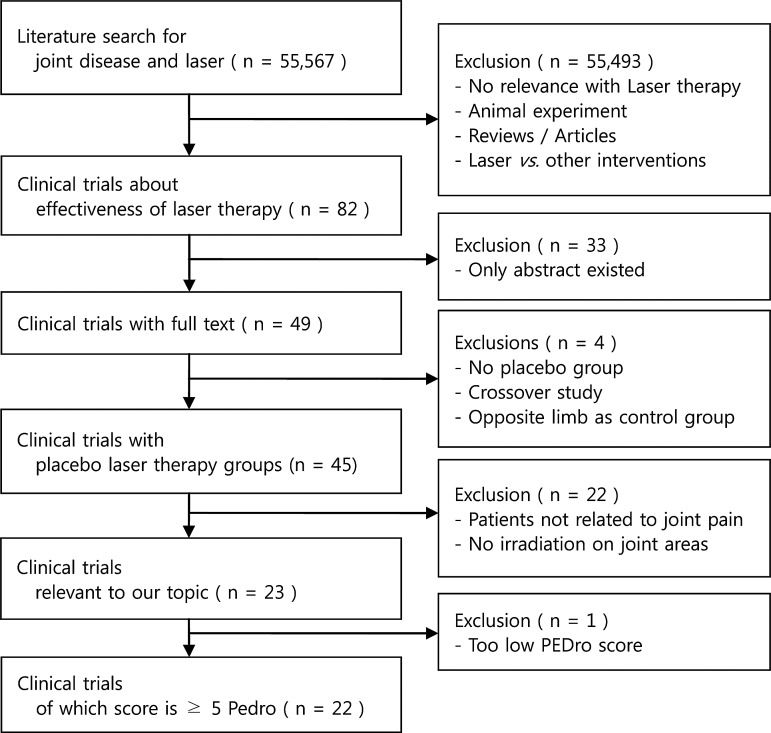
Figure 1 describes the literature search process. In total, 55,567 abstracts of potentially relevant publications were identified through an electronic search. Of these, 82 clinical trials of laser therapy remained after excluding publications that were not related to laser therapy or those that compared laser therapy with other physical interventions, animal experiment researches, or reviews. Among these 82 trials, 33 trials were excluded because we failed to obtain their full text, and 4 trials were excluded because these studies contained no placebo laser therapy group, was a crossover study, or the opposite limb was used as the control group. Out of the remaining 45 trials, 22 trials were excluded because there was no evidence of irradiation on the joint areas or the primary cause of patient pain was not related to joint problems. After assessing the quality of the clinical trials, one more trial was excluded because its quality assessment score was too low to for us be confident in its results. Finally, 22 trials were selected for inclusion in this study.
FIG. 1.
Selection process.
Excluded studies
Among the 49 clinical trials with full text available, 27 studies were excluded because important conditions for the meta-analysis were not satisfied. Table 1 summarizes some of excluded studies. Studies performed by Carvalho et al.,21 Gur et al. (lower back),22 and Heussler et al.23 were excluded because they had no placebo group. Studies by de Bie et al.,24 Ekim et al.,25 Rogvi-Hansen et al.,26 Aigner et al.,27 Yurtkuran et al.,28 and Shen et al.16 were excluded because there was no description of irradiation on the joint area or irradiation was performed only on the acupuncture points. Two studies from Konstantinovic et al.29,30 were excluded because the primary cause of pain in the subjects was radiculopathy. Finally, the study by Fikácková et al.31 was excluded because of its low quality assessment score (PEDro scale score<5).
Table 1.
Summary of Excluded Studies
| Author | Pain of patients | Author's decision | Reason for exclusion |
|---|---|---|---|
| Carvalho21 | Temporomandibular disorders (TMD) | O | No placebo group |
| Gur (low back)22 | Low back pain | X | No placebo group |
| Heussler23 | Rheumatoid arthritis (RA) | X | No placebo group |
| de Bie24 | Ankle sprains | X | No clear description of joint irradiation |
| Ekim25 | RA with carpal tunnel syndrome | O | No clear description of joint irradiation |
| Rogvi-Hansen26 | Chondromalacia patellae | X | No clear description of joint irradiation |
| Aigner27 | Whiplash injuries | X | Acupuncture Point |
| Yurtkuran28 | Knee osteoarthritis (OA) | X | Acupuncture point |
| Shen16 | Knee OA | O | Acupuncture point |
| Konstantinovic29 | Neck pain | O | Radiculopathy |
| Konstantinovic30 | Low back pain | O | Radiculopathy |
| Fikácková31 | TMD | O | Low quality assessment score |
In the author's decision, O indicates the effectiveness of the trial and X indicates the ineffectiveness of the trial.
Included studies
A total of 22 trials were included for further analysis; 668 people were in the laser therapy group and 565 people were in the placebo laser group. Patient properties, irradiation locations, session schedules, and co-interventions of the included trials are listed in Table 2. There is one trial for rheumatoid arthritis,32 eight trials for osteoarthritis,33–40 five trials for temporomandibular disorders,41–45 five trials for low back pain,2,46–49 two trials for shoulder pain,50,51 and two trials for neck pain.40,52 All patients in these trials suffered from pain in their joint regions and their joint regions were irradiated by lasers. In some trials, the laser was applied to other locations (e.g., muscles, nerves, and tendons) in addition to the joint capsule, but all included trials had at least one irradiation on the joint area.
Table 2.
Summary of Laser Therapy Parameters of Clinical Trials I
| Author | Patient's properties | Irradiation location | Total sessions/sessions per weeks | Co-interventions | AD |
|---|---|---|---|---|---|
| Meireles32 | RA | Wrist and finger joint | 16/2 | Analgesics | X |
| Basford33 | OA | Thumb joints | 9/3 | Drugs* | X |
| Brosseau34 | OA | Hand | 18/3 | Drugs | X |
| Stelian35 | OA knee |
Both sides of the knee | 20/10* | Drugs | O |
| Bulow36 | OA | Periarticular tender points | 9/3 | Drugs | X |
| Gur37 | OA | Knee joint | 10/5 | Drugs Exercise |
O |
| Tascioglu38 | OA | Knee joint | 10/5 | Analgesics | X |
| Hegedus39 | OA | Epicondyle of femur Knee joint gap Edge of the tendon |
8/2 | Not allowed | O |
| Kulekcioglu41 | TMD | TMJ Muscles related to TMD |
15/- | Exercise | X |
| Venancio42 | TMD (arthrogenous origin) | TMJ | 6/2 | - | X |
| Cetiner43 | TMD (myogenic origin) | TMJ | 10/5 | - | O |
| Emshoff44 | TMD | TMJ | 20/2∼3 | - | X |
| Santos45 | TMD | Joint capsule | 1/1 | - | O |
| Bingol50 | Shoulder pain | Muscles related with shoulder pain Anterior and posterior faces of the capsule |
10/5 | Analgesics Exercise |
X |
| Stergiouslas51 | Frozen shoulder | Shoulder area | 12/1∼2 | Exercise | O |
| Ozdemir40 | OA (neck pain) | Neck area | 10/- | - | O |
| Chow52 | Neck pain | Neck area | 14/2* | Drugs | O |
| Klein46 | LBP (chronic) | Spine Fascia Ligament |
12/3 | Exercise | X |
| Soriano47 | LBP | Low back area | 10/5 | Not allowed | O |
| Basford48 | LBP | L2 to S3 paraspinal tissues | 12/3 | Analgesics NSAIDs |
O |
| Djavid2 | LBP | Paravertebral region | 12/2 | Exercise | O |
| Ay49 | LBP disk herniation | Paraspinal tissues of the disk spaces | 15/5 | Hot pack | X |
OA, osteoarthritis; RA, rheumatoid arthritis; TMD, temporomandibular disorder; TMJ, temporomandibular joint; LBP, Low back pain. *, inferred values as not explicitly described; −, no descriptions or failed to infer; AD, author's decision on effectiveness (O, effective; X, ineffective). In the case of Stelian 199235, number of treatments per week was not described, but the author described that the treatment was applied twice a day for 10 days.
Except for the study by Santos et al.,45 all studies included at least 6 sessions, with an average 12 irradiation sessions applied. Then, except for 7 trials,39,40,42–45,47 the remaining 15 trials simultaneously combined other interventions with laser therapy. Some trials used drugs such as analgesics, NSAIDs, antidepressants, and tranquilizers,32–36,38,48,52 and other trials used exercises2,37,41,46,50,51 or hot packs49 as co-interventions during laser therapy.
Table 3 summarizes the parameter specifications for laser irradiation. For each irradiation point, wavelengths range from 632.8 to 1060 nm, with average powers from 0.4 to 2656 mW, power densities from 0.4 to 10,000 mW/cm2, energy doses from 0.0135 to 239.4 J, energy densities from 0.1 to 1200 J/cm2, irradiation point sizes from 0.005 to 4.9 cm2, and irradiation times from 1 to 900 sec. The numbers of irradiation points are also included in Table 3; the number of irradiation points for the specific joint was described in only five studies,32–34,37,51 whereas most of the studies only described the number of irradiation points for one session or did not describe the number of irradiations.
Table 3.
Summary of Laser Therapy Parameters of Clinical Trials II
| Author | Patient's properties | Irradiated joint | Laser | Average power mW | Power density mW/cm2 | Energy dose J/p | Energy density J/cm2 | Irradiation time (sec) | Irradiation point size cm2 | No. of irradiation points | AD |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Meireles32 | RA | Finger | GaAlAs 785(C*) |
70 | 1166* | 0.18* | 3 | 2.57* | 0.06 | 4/finger joint | X |
| Basford33 | OA | Thumb | HeNe 632.8(C) |
0.9 | 90* | 0.0135* | 1.35* | 15 | 0.01* | 4/finger joint | X |
| Brosseau34 | OA | Finger | GaAlAs 860 |
30 | 3000 | 0.03* | 3 | 1 | 0.01 | 4/finger joint | X |
| Stelian for 830 nm35 | OA | Knee | GaAlAs 830(C)(P) |
25(C) 270(P) |
11(C) 122(P) |
11.1 (J/joint) | 5.6 | 450(C) 450(P) |
2 | - | O |
| Stelian for 633 nm35 | OA | Knee | HeNe 633(C)(P) |
18(C) 75(P) |
8(C) 34(P) |
10.3 (J/joint) |
5.1 | 450(C) 450(P) |
2 | - | O |
| Bulow36 | OA | Knee | GaAlAs 830(C) |
25 | 90* | 3 (1.5– 4.5) | 10.7* | 60–180 | 0.28 | 5–15/session | X |
| Gur for 3 J37 | OA | Knee | GaAs 904(P*) |
10 | 10* | 3 (J/joint) | 3* | 300 | 1 | 2/knee joint | O |
| Gur for 2 J37 | OA | Knee | GaAs 904(P*) |
11.2 | 11.2* | 2 (J/joint) | 2* | 180 | 1 | 2/knee joint | O |
| Tascioglu for 3 J38 | OA | Knee | GaAlAs 830(C) |
50 | 6369* | 3 | 382* | 120(60*) | 0.00785* | 5/session | X |
| Tascioglu for 1.5 J38 | OA | Knee | GaAlAs 830(C) |
50 | 6369* | 1.5 | 191* | 60(30*) | 0.00785* | 5/session | X |
| Hegedus39 | OA | Knee | GaAlAs 830(C) |
50 | 10,000 | 6 | 1200* | 120* | 0.005* | 8/session** | O |
| Kulekcioglu41 | TMD | TMJ | GaAs 904 |
17 | 17* | 3* | 3 | 180 | 1* | 4/session | X |
| Venancio42 | TMD (arthrogenous origin) | TMJ | GaAlAs 780 |
30 | 630* | 0.3* | 6.3 | 10 | 0.0476* | 3/session | X |
| Cetiner43 | TMD (myogenic origin) | TMJ | GaAlAs 830 |
- | 43.21* | - | 7 | 162 | - | 4/session | O |
| Emshoff44 | TMD | TMJ | HeNe 632.8(C) |
30 | 12.5* | 3.6* | 1.5 | 120 | 2.4* | - | X |
| Santos45 | TMD | TMJ | GaAlAs 830 |
40 | 5000* | 0.64* | 80 | 16 | 0.04 (0.008*) | 4/session | O |
| Bingol50 | Shoulder pain | Shoulder | GaAs 904(P*) |
40* | 49* | 2.384* | 2.98 | 60 | 0.8 | - | X |
| Stergioulas51 | Frozen shoulder | Shoulder | GaAlAs 810(C) |
60 | 120* | 1.8 | 3.6 | 30 | 0.5 | 8/glenohumeral joint | O |
| Ozdemir40 | OA | Neck area | GaAlAs 830(C) |
50 | 50* | 0.9 | 0.9* | 15 | 1 | 12/session | O |
| Chow52 | Neck pain | Neck area | GaAlAs 830(C) |
300 | 670 | 9* | 20.1* | 30 | 0.45* | up to 50/session | O |
| Klein46 | LBP (chronic) | Low back | GaAs 904 |
0.4* [5.4*] |
0.4* [5.4*] |
0.1* [1.3*] |
0.1* [1.3] |
240 | 1 | - | X |
| Soriano47 | LBP | Low back | GaAs 904(P*) |
40 | - | - | 4 | - | - | 2–4/session | O |
| Basford48 | LBP | Low back | Nd:YAG 1060(C) |
2656* | 542 | 239.4* | 48.8* | 90 | 4.9* | 8/session | O |
| Djavid2 | LBP | Low back | GaAlAs 810(C) |
50 | 226* | 6* | 27 | 120* | 0.221 | 8/session | O |
| Ay for acute49 Ay for chronic49 |
LBP disk herniation | Low back | GaAlAs 850(C) |
11.7* | 166.7* | 2.8* | 40 | 240 | 0.07 | - | X |
OA, osteoarthritis; RA, rheumatoid arthritis; TMD, temporomandibular disorder; TMJ temporomandibular joint; LBP, low back pain; (C), continuous wave; (P), pulsed wave; *, inferred values as not explicitly described; **, not described but confirmed by the author; −, not described or cannot infer; AD, author's decision on effectiveness (O, effective; X, ineffective).
Most trials consisted of a single LLLT group and a single placebo LLLT group. But the study of Ay et al.49 consisted of two LLLT groups and two placebo LLLT groups; one LLLT–placebo pair was performed on acute low back pain and the other pair focused on chronic low back pain. The study by Gur et al.37 consisted of two true laser therapy groups (one used a 3 J energy dose per knee joint and the other used a 2 J energy dose per knee joint) and one placebo laser group. The study by Tascioglu et al.38 also had two true laser therapy groups (one used a 3 J energy dose per point and the other used 1.5 J per point). Stelian et al.35 used both continuous wave and pulsed wave irradiation on one knee: during each session, irradiation in each mode was split into 7.5 min segments.
Clinical trial quality assessment
The quality assessment scores of 22 studies are listed in Table 4. The scores range from 5 to 10, with an average of 7.9. Note that in terms of blinding the assessor items, all trials obtained a point because all used self-assessment measures. All trials except for Cetiner et al.43 and Santos et al.45 reported that they randomly allocated groups.
Table 4.
List of Quality Assessment of Clinical Trials by PEDro Scale
| Author | RA | CA | BS | BP | BT | BA | 85% | IT | BC | MV | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Meireles32 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Basford33 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| Brosseau34 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 9 |
| Stelian35 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| Bulow36 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 7 |
| Gur37 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| Tascioglu38 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
| Hegedus39 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 6 |
| Kulekcioglu41 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 6 |
| Venancio42 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 7 |
| Cetiner43 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 5 |
| Emshoff44 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Santos45 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 5 |
| Bingol50 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
| Stergioulas51 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 7 |
| Ozdemir40 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| Chow52 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Klein46 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 7 |
| Soriano47 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 7 |
| Basford48 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| Djavid2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Ay49 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
RA, random allocation; CA, concealed allocation; BS, baseline similarity; BP, blinding of patients; BT, blinding of therapists; BA, blinding of assessor; 85%, key outcome obtained from >85% of the initial subjects; IT, intentions to treat analysis; BC, between-group comparisons, MV, mean and variability data.
Effect sizes of studies
Table 5 presents the outcome measures of the included studies. All trials except for Basford et al.,33 Brosseau et al.,34 and Soriano et al.47 have self-assessed pain measures. In most cases, VAS was used as the pain measure, ranging from 0 (no pain) to 10 (severe pain). However, the studies of Basford et al.33 and Klein et al.46 used a pain scale ranging from 0 (no pain) to 4 (severe pain) and from 0 (no pain) to 7.5 (severe pain), respectively. Therefore, for consistency, the pain values of these trials were converted into a 0–10 scale.
Table 5.
Summary of Pain Measures and Differences in Mean Changes
| Author | AD | Mean diff | Mean diff. var | #(L) | (L) Pre SM | (L) Pre SD | (L) Post SM | (L) Post SD | #(P) | (P) Pre SM | (P) Pre SD | (P) Post SM | (P) Post SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Meireles32 | X | −7.6 | 34.64 | 41 | 60.8 | 18.7 | 42 | 25 | 41 | 58.5 | 17.6 | 32.1 | 28.2 |
| Basford33 | X | - | - | 47 | 53 | - | - | - | 34 | 48 | - | - | - |
| Brosseau34 | X | - | - | 42 | 56.9 | 18.4 | - | - | 46 | 49.4 | 22.4 | - | - |
| Stelian for 830nm35 | O | 40 | 67.77 | 18 | 71.6 | 22.2 | 32.2 | 26.2 | 17 | 62.3 | 24.1 | 62.9 | 22.2 |
| Stelian for 633nm35 | O | 32.6 | 66.16 | 15 | 65.3 | 24.7 | 33.3 | 23.8 | 17 | 62.3 | 24.1 | 62.9 | 22.2 |
| Burow36 | X | 19 | - | 14 | 82 | - | 61 | - | 15 | 71 | - | 69 | - |
| Gur at 3J37 | O | 13 | 10.53 | 30 | 73.2 | 23.7 | 35.8 | 11.2 | 30 | 67.4 | 17.3 | 43 | 13.8 |
| Gur at 2J37 | O | 12 | 8.81 | 30 | 74.4 | 13.8 | 38 | 8.6 | 30 | 67.4 | 17.3 | 43 | 13.8 |
| Tascioglu at 3J38 | X | −1.04 | 25.69 | 20 | 68 | 15.45 | 64.96 | 13.1 | 20 | 63.88 | 16.07 | 59.8 | 18.5 |
| Tascioglu at 1.5J38 | X | 1.36 | 28.97 | 20 | 65.72 | 18.68 | 60.28 | 15.4 | 20 | 63.88 | 16.07 | 59.8 | 18.5 |
| Hegedus39 | O | 25.5 | - | 18 | 57.5 | - | 17.1 | - | 9 | 56.2 | - | 41.3 | - |
| Kulekcioglu41 | X | 5 | 27.36 | 20 | 42.8 | 27 | 10.5 | 18.5 | 15 | 35.3 | 29 | 8 | 9.4 |
| Venancio42 | X | 11.4 | 146.98 | 15 | 82.7 | 17.9 | 40.7 | 33.5 | 15 | 77.3 | 19.1 | 46.7 | 32.9 |
| Cetiner43 | O | 43.4 | 41 | 24 | 75.6 | 14.6 | 22.5 | 20.5 | 15 | 65.7 | 19.1 | 56 | 17.6 |
| Emshoff44 | X | -2 | 20.83 | 26 | 38.2 | 7.6 | 12.3 | 16.1 | 26 | 39.7 | 12.2 | 11.8 | 16.8 |
| Santos45 | O | 14.8 | 42.25 | 25 | 51.4 | 21.1 | 29 | 17 | 25 | 54 | 23.7 | 46.4 | 27.7 |
| Bingol50 | X | 2.4 | - | 20 | 61 | 17.7 | 56.5 | - | 20 | 61.7 | 16.4 | 59.6 | - |
| Stergioulas51 | O | 24.13 | 3.02 | 31 | 80.55 | 8.82 | 22.54 | 6.02 | 32 | 73.66 | 8.74 | 39.78 | 7.65 |
| Ozdemir40 | O | 48 | 8.83 | 30 | 77 | 13 | 24 | 13 | 30 | 73 | 14.3 | 68 | 9.8 |
| Chow52 | O | 30 | 16.205 | 45 | - | - | - | - | 45 | - | - | - | - |
| Klein46 | X | 1.33 | 60.44 | 10 | 40 | 16 | 22.6 | 18.6 | 10 | 44 | 14.6 | 28 | 16 |
| Soriano47 | O | - | - | 38 | - | - | - | - | 33 | - | - | - | - |
| Basford48 | O | 13.5 | 35.67 | 30 | 35.2 | 29 | 17.1 | 15.8 | 29 | 37.4 | 36 | 32.8 | 28.5 |
| Djavid2 | O | 6 | 39.25 | 19 | 62 | 16 | 46 | 17 | 18 | 63 | 20 | 53 | 21 |
| Ay at acute49 | X | −4 | 20.49 | 20 | 67 | 21.5 | 27 | 14.9 | 20 | 61.5 | 23.9 | 20 | 13.7 |
| Ay at chronic49 | X | −6 | 20.74 | 20 | 60 | 22.9 | 26.5 | 14.2 | 20 | 66 | 22.5 | 26.5 | 14.6 |
AD, author's decision on effectiveness (O, effective, X, ineffective); SM, sample mean; SD, standard deviation; −, no description or failed to infer. This table lists pain measure differences between low-level laser therapy (LLLT) group (L) and placebo group (P). For each group, the number of patients in the group and outcomes of pretreatment in the group (A) and post-treatment in the group (B) are described. The mean changes between pretreatment and post-treatment within each group (C=B-A) are used for calculating the mean difference between LLLT group and placebo group(CLLLT – CPlacebo).
Most trials only reported pain with no specific location or activities. However, Emshoff et al.44 reported pain during function (mastication) and Meireles et al.32 reported total 47 pain measure outcomes that included “global pain at each hand,” “pain at wrist,” and “pain in each finger joint;” of these, we chose “global pain of the right hand.”
The study by Ay et al.49 consisted of four groups: LLLT group with low back pain (LBP)<3 months, placebo group with LBP<3 months, LLLT group with LBP>3 months, and placebo group with LBP>3 months. To calculate the effect size, we divided the four groups into two LLLT–placebo pairs; one pair for LBP<3 months and the other pair for LBP>3 months. The study by Djavid et al.2 consisted of an LLLT group, an LLLT plus exercise group, and a placebo LLLT plus exercise group. Of these, we selected the LLLT plus exercise group and the placebo LLLT plus exercise group in order to calculate the effect size. Studies by Stelian et al.,35 Gur et al.,37 and Tascioglu et al.38 included three groups: two laser groups using different laser doses and one placebo laser group. To calculate the effect size for each group, we used the outcome measure of the placebo laser group twice.
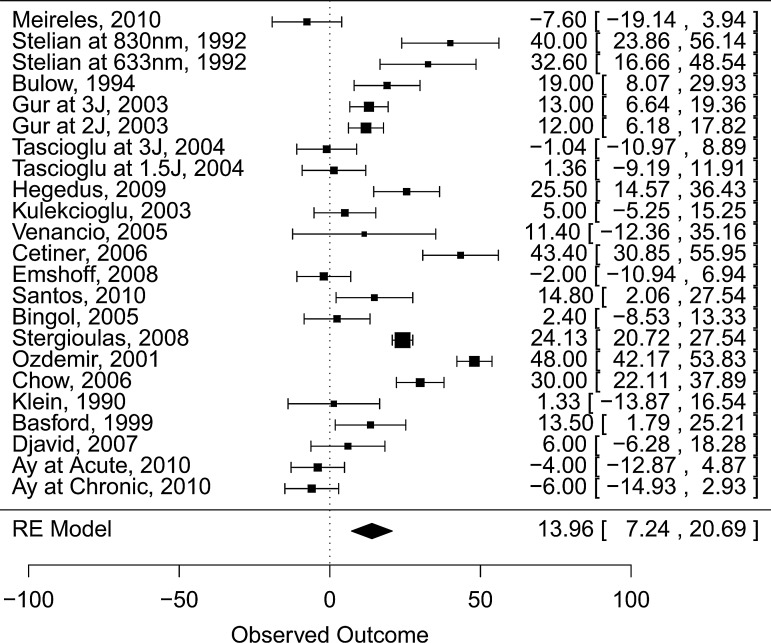
Mean effect size
Figure 2 shows the mean effect size for the included studies, except for studies with no self-assessment pain measure reported (Basford et al.,33 Brosseau et al.,34 and Soriano et al.47). The result was 13.96 mm (95% CI, 7.24–20.69) (number in active group: 541; number in placebo group: 452) in favor of true laser use.
FIG. 2.
Effect of pain relief from low-level laser therapy.
Classification of studies about energy dose and wavelength
Our study focused on trials that included at least one laser irradiation on the joint area. The review article by Bjordal et al.6 suggested energy doses for the joint diseases. They assumed that there were location-specific effective doses for joint pain, and subsequently categorized anatomical sites that could be irradiated with approximately the same ranges of wavelengths, power densities, and energy doses. In Table 6, we classify the studies using similar categories: locations with TMJ/finger joints, knee, shoulder, cervical area, and lumbar area, and wavelengths <700 nm, >700 and <900 nm,>900 and<1,000 nm, and>1,000 nm. For each category, the energy dose suggested by Bjordal et al.6 is listed, except for shoulder, as there is no suggested dose for the shoulder. A total of 25 true laser groups from the 22 clinical trials included are listed along with the energy dose used in the trial and the author's perception about the effectiveness of the laser therapy; note that three of the clinical trials include two true laser groups.
Table 6.
Energy Doses Reported for Joint Areas
| |
<700 nm |
>700 and<900 nm |
>900 and<1,000 nm |
>1,000 nm |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wavelength Location | SR (J) | Author | J/p | AD | SR (J) | Author | J/p | AD | SR (J) | Author | J/p | AD | SR (J) | Author | J/p | AD |
| TMJ | 6∼30 | Basford33 | 0.0135* | X | 0.5∼15 | Cetiner43 | - | O | 0.2∼1.4 | Kulekcioglu41 | 3* | X | ||||
| Finger | Emshoff44 | 3.6* | X | Brosseau34 | 0.03* | X | ||||||||||
| Meireles32 | 0.18* | X | ||||||||||||||
| Venancio42 | 0.3* | X | ||||||||||||||
| Santos45 | 0.64* | O | ||||||||||||||
| Knee | 9∼2700 | Stelian35 | 10.3 J/joint | O | 6∼180 | Tascioglu38 | 1.5 | X | 1.2∼84 | Gur37 | 2 J/joint | O | ||||
| Tascioglu38 | 3 | X | Gur37 | 3 J/joint | O | |||||||||||
| Bulow36 | 1.5∼4.5 | X | ||||||||||||||
| Hegedus39 | 6 | O | ||||||||||||||
| Stelian35 | 11.1 J/joint | O | ||||||||||||||
| Shoulder | Stergioulas51 | 1.8 | O | Bingol50 | 2.38* | X | ||||||||||
| Cervical | 11∼360 | Ozdemir40 | 0.9 | O | 0.8∼56 | |||||||||||
| Area | Chow52 | 9* | O | |||||||||||||
| Lumbar | 48∼480 | Ay49 | 2.8* | X | 15∼105 | Soriano47 | - | O | 48∼480 | Basford51 | 239* | O | ||||
| Area | Djavid2 | 6* | O | Klein46 | 0.1* | X | ||||||||||
SR, suggested Range of dose (J) by Bjordal; J/p, Joule per point; J/joint, Joule per joint; AD, author's decision on effectiveness; O, laser is effective; X, laser is ineffective; *, inferred value; −, no description or failed to infer.
Among the 25 clinical trials, 7 trials were within the range of suggested energy doses (Stelian et al.,35 Gur et al.,37 Hegedus et al.,39 Santos et al.,45 Basford et al.48). For the remaining trials, we could not determine whether their energy doses were within suggested energy doses per joint (Basford et al.,33 Emshoff et al.,44 Brosseau et al.,34 Meireles et al.,32 Cetiner et al.,43 Venancio et al.,42 Tascioglu et al.,38 Bulow et al.,36 Stergioulas et al.,51 Chow et al.,52 Ay et al.,49 Djavid et al.,2 Kulekcioglu et al.,41 Bingol et al.,50 Soriano et al.,47 Klein et al.46). In two trials, the information was either not reported or we could not infer the energy dose (J/point) (Cetiner et al.,43 Soriano et al.47), and the other two trials pertained to irradiation on the shoulder joint (Bingol et al.,50 Stergioulas et al.51).
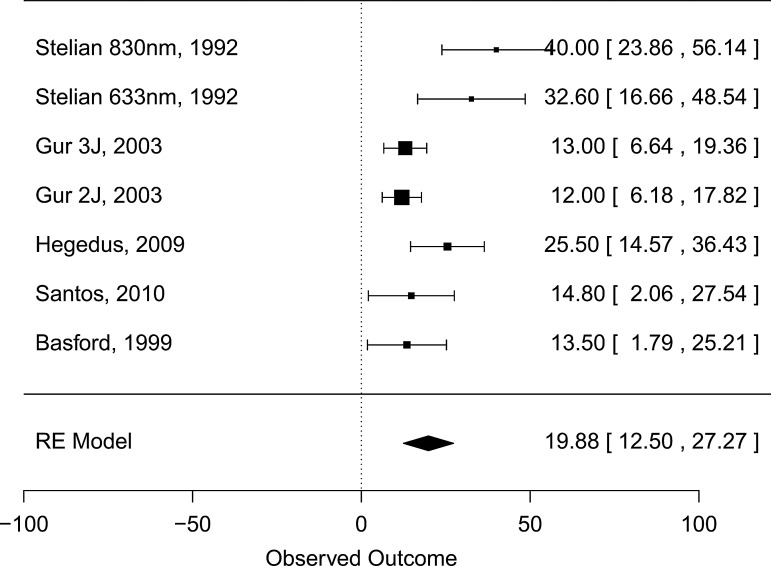
Figure 3 presents the effect size for studies in which doses are within the energy dose range suggested by Bjordal et al.6 We can observe the effect of 19.88 mm (95% CI, 12.50, 27.27) (number in active group:166; number in placebo group: 110), which is larger than the size measured in the 22 studies.
FIG. 3.
Effect of pain relief from low-level laser therapy from trials within energy dose window.
Although the energies of some studies of cervical or lumbar pain (Ozdemir et al.,40 Chow et al.,52 Djavid et al.2) are lower than the energy suggestion by Bjordal et al.,6 they report notable pain relief from laser therapy. For zygapophyseal joints, the suggested lower energy bound might be decreased.
In addition, we examined the included studies using World Association for Laser Therapy (WALT) dosage recommendations.53 Because WALT recommends energy doses for the laser therapy of 780–860 nm and 904 nm wavelengths and requires higher energy doses than Bjordal et al., only three studies2,39,52 satisfied the recommendation criteria, and their mean effect size was 21.05 mm (95% CI, 6.93, 35.17). It is similar to the mean effect size of the studies satisfying Bjordal's recommendation. Considering studies satisfying both Bjordal's and WALT recommendations, only one study39 was included, and its effect size was 25.5 mm.
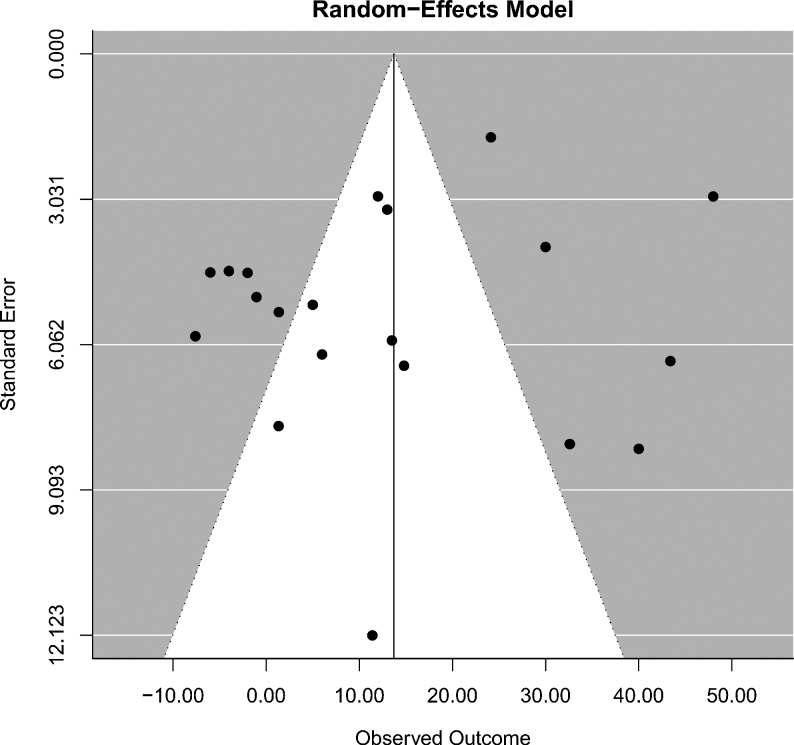
Publication bias issue
It is also important to investigate whether there is a publication bias in this systematic review. To calculate the publication bias, we excluded the studies36,39,50 in which we failed to infer any variance of the mean difference. The funnel plot in Fig. 4 shows that the studies on the left side of the mean effect size are more focused than the studies on the right side. However, we cannot find the typical asymmetry in other reviews with publication bias; the number of studies on the bottom left side is smaller than the number of studies on the bottom right side. This funnel plot shows that there is no publication bias in this systematic review.
FIG. 4.
Funnel plot publication bias analysis.
Discussion
The effectiveness of laser therapy is still controversial. As it is possible that numerous factors in laser therapy can contribute to different treatment outcomes, we focused here on trials that included at least one laser irradiation on joint areas and displayed a high methodological quality with respect to the PEDro scale. As a result, 22 trials were included in this study. Through a series of analyses, this review supports the finding that LLLT trials that satisfy the abovementioned conditions are effective if the energy dose is properly selected for each joint region. However, it should be noted that this study has several weaknesses because of the heterogeneity of studies in terms of patient conditions, laser irradiation locations, and area size, in addition to ambiguities in calculating the parameters.
Patient conditions
The duration of pain or symptoms might affect the effectiveness of pain reduction when LLLT is irradiated. However, most studies did not report the duration, even though studies reporting the pain duration varied, ranging from 2.45 (SD±1.43) months49 to 16.90 (SD±12.5) years.52 It would be useful for the duration of pain to be included in future analyses.
Laser irradiation locations
Another factor that potentially contributes to the outcome of LLLT is co-irradiation on other regions in addition to the joint regions. Among the studies for finger and hand areas, LLLT was also irradiated on the nerve32 and wrist.34 In all studies pertaining to spinal areas, LLLT might also have been irradiated on the fascia, muscle, nerve, and ligament regions. In one study of the knee area,39 the tendon was also irradiated. Among studies for TMJ areas, muscles around the TMJ were also irradiated. It is important to note that in all of these studies, irradiation on the joint area is common.
Laser irradiation area size
The irradiation size varied among studies. In the studies of finger and hand pain,32–34 the irradiation area sizes were≤0.06 cm2 and all studies reported the lack of significance of the laser therapy. In the studies pertaining to neck pain,40,52 all studies reported the significance of the laser therapy. Although one study52 had smaller irradiation size (0.45 cm2) than the other study40 (1 cm2), the energy dose of the former study was higher than that of the latter study. In the case of low back pain, the studies2,48 with irradiation sizes of 0.22 and 4.9 cm2 reported the effectiveness of laser therapy, although a study49 having an irradiation size of 0.07 cm2 reported that lasers were ineffective in treating pain. Yet another study,46 with an irradiation size of 1 cm2, reported ineffectiveness, although its energy dose per point was the lowest among the studies of low back pain. In investigations of knee pain, studies35,37 in which the irradiation size was≥1 cm2 showed the effectiveness of laser treatments. Among three studies36,38,39 in which the irradiation size was<1 cm2, however, two studies36,38 reported ineffectiveness and one study39 reported effectiveness. In this case, the energy per point of study39 with an improved outcome (6 J) was greater than the energies of the two ineffective studies36,38 (≤3 J). In the studies of TMJ pain, two studies42,45 used a similar irradiation area (0.04 cm2), but their results were different, possibly because of the difference in energy dose (0.3 and 0.64 J). Two shoulder pain studies50,51 used irradiation areas<1 cm2, but their wavelengths were different, and, therefore, results of the effectiveness of these two studies were also different. Based on the current body of knowledge in this field, it was difficult to confirm any definitive relationship between the irradiation area size and effectiveness of laser therapy; therefore, further analyses of more clinical trials are required.
Calculating parameters
Most studies did not clearly report the parameters of laser therapy. To infer missing parameters in terms of energy dose (J/point), energy density (J/cm2), average power (mW/point), power density (mW/cm2), irradiation area (cm2), and irradiation time (sec), we applied the formulae described in the Methods section. In the study by Basford et al.,33 the power density was not described in the article and could not be inferred here; rather, we used the description about power density of Basford et al.33 that was presented in the review article by Bjordal et al.6 to infer the energy density and irradiation size. In the study by Santos et al.,45 the laser irradiation size described in the full text was larger than the size we calculated; hence, both values are described in Table 3. In the study by Klein et al.,46 we inferred two different energy doses: 0.1 and 1.3 J, both of which are described in Table 3. In the studies by Basford et al.48 and Tascioglu et al.,38 a total of eight points were irradiated. In these studies, the laser beam size was described in terms of diameter, not as cm2; therefore, we calculated the size using the formula: 3.14 * 1.25 cm * 1.25 cm. Note that in the study by Tascioglu et al.,38 irradiation times were described as being 120 sec for the 3 J groups and 60 sec for 1.5 J groups, but we inferred these values to be 60 sec for the 3 J groups and 30 sec for 1.5 J groups.
We also inferred the effect sizes of some studies in Table 5. Instead of reporting the VAS variance, Santos et al.45 and Chow et al.52 reported each patient's pain measures before and after treatment and the confidence interval of pain measures. From these data, we calculated the effect size. Furthermore, some studies did not report the variance data (Burow et al.,36 Hegedus et al.,39 Bingol et al.50); in such cases, we used the average of the standard deviations of the other studies included in this review.
Calculating energy doses
Extraction of the energy dose used on the joint capsules is a difficult task although it is important for determining the effective energy dose for different joint pain regions. Whereas two studies reported the energy dose for each joint capsule,35,37 other clinical studies2,32–34,36,38–50 did not describe the exact energy dose for each joint capsule. Instead, these studies only reported the energy dose per irradiation point and the number of laser irradiations. Because some laser irradiations might be applied to other joint capsules or non-joint regions such as tendons, ligaments, muscles, and nerves—as well as the specific joint capsule—we cannot be sure how much energy dose was applied to the specific joint capsule. In these cases, we used the energy dose per irradiation point to calculate the energy dose per joint capsule and then determined whether these clinical trials were within the energy dose suggested by Bjordal et al.6 In this way, we determined that some clinical trials39,45,48 were within the suggested doses.
Effect of co-intervention
Laser therapy often has been applied by combining with co-interventions such as analgesics, NSAIDs, exercises, and other physical therapies. We examined the effectiveness of the included studies when the co-intervention was used. Among the 15 included studies using co-interventions, 6 studies2,35,37,48,51,52 reported effectiveness and the other 9 studies32–34,36,38,41,46,50,49 reported ineffectiveness of laser therapy. Among the seven included studies not using co-interventions, five studies39,40,43,45,47 reported effectiveness and the other two studies42,44 reported ineffectiveness. When we hypothesized that the proportion of ineffectiveness is higher among the studies using co-intervention than the studies not using co-intervention, the difference of proportion was not statistically significant by Fisher's exact test (p=0.3615). When we restricted co-interventions to drugs such as analgesics and NSAIDs, among the 10 studies using drugs, 4 studies35,37,48,52 reported effectiveness and the other 6 studies32–34,36,38,50 reported ineffectiveness. Similarly, the proportion of ineffectiveness was not statistically significant by Fisher's exact test (p=0.3348).
Conclusions
Obtaining pain relief from LLLT might be a good alternative to the use of NSAIDs, particularly for elderly people, because laser therapy has no reported side effects.47 In addition, clinical studies have reported that applying laser therapy in addition to exercise might show greater pain reduction effects than using laser therapy alone.2,22 In conclusion, investigations pertaining to laser therapies have indicated that laser irradiation on joint areas can be an effective pain relief treatment when appropriate energy doses are selected.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MEST) (No. 2011-0029447) and by a grant of the Traditional Korean Medicine Industry Development Product R&D Project, Ministry of Health & Welfare, Republic of Korea (F090001).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Marks R. de Palma F. Clinical efficacy of low power laser therapy in osteoarthritis. Physiother. Res. Int. 1999;4:141–157. doi: 10.1002/pri.159. [DOI] [PubMed] [Google Scholar]
- 2.Djavid G.E. Mehrdad R. Ghasemi M. Hasan-Zadeh H. Sotoodeh-Manesh A. Pouryaghoub G. In chronic low back pain, low level laser therapy combined with exercise is more beneficial than exercise alone in the long term: a randomised trial. Aust. J. Physiother. 2007;53:155–160. doi: 10.1016/s0004-9514(07)70022-3. [DOI] [PubMed] [Google Scholar]
- 3.Fulop A.M. Dhimmer S. Deluca J.R., et al. A meta-analysis of the efficacy of laser phototherapy on pain relief. Clin. J. Pain. 2010;26:729–736. doi: 10.1097/AJP.0b013e3181f09713. [DOI] [PubMed] [Google Scholar]
- 4.Honmura A. Yanase M. Obata J. Haruki E. Therapeutic effect of Ga-Al-As diode laser irradiation on experimentally induced inflammation in rats. Lasers Surg. Med. 1992;12:441–449. doi: 10.1002/lsm.1900120414. [DOI] [PubMed] [Google Scholar]
- 5.Tadakuma T. Possible application of the laser in immunobiology. Keio J. Med. 1993;42:180–182. doi: 10.2302/kjm.42.180. [DOI] [PubMed] [Google Scholar]
- 6.Bjordal J.M. Couppe C. Chow R.T. Tuner J. Ljunggren E.A. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust. J. Physiother. 2003;49:107–116. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- 7.Parekh R.B. Dwek R.A. Sutton B.J., et al. Association of rheumatoid arthritis and primary osteoarthritis with changes in the glycosylation pattern of total serum IgG. Nature. 1985;316:452–457. doi: 10.1038/316452a0. [DOI] [PubMed] [Google Scholar]
- 8.Bradley J.D. Brandt K.D. Katz B.P. Kalasinski L.A. Ryan S.I. Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee. N. Engl. J. Med. 1991;325:87–91. doi: 10.1056/NEJM199107113250203. [DOI] [PubMed] [Google Scholar]
- 9.Zayat A.S. Conaghan P.G. Sharif M., et al. Do non-steroidal anti-inflammatory drugs have a significant effect on detection and grading of ultrasound-detected synovitis in patients with rheumatoid arthritis? Results from a randomised study. Ann. Rheum. Dis. 2011;70:1746–1751. doi: 10.1136/annrheumdis-2011-200017. [DOI] [PubMed] [Google Scholar]
- 10.Leung A. Liew D. Lim J., et al. The effect of joint aspiration and corticosteroid injections in osteoarthritis of the knee. Int. J. Rheum. Dis. 2011;14:384–389. doi: 10.1111/j.1756-185X.2011.01631.x. [DOI] [PubMed] [Google Scholar]
- 11.Scanzello C.R. Moskowitz N.K. Gibofsky A. The post-NSAID era: what to use now for the pharmacologic treatment of pain and inflammation in osteoarthritis. Curr. Rheumatol. Rep. 2008;10:49–56. doi: 10.1007/s11926-008-0009-6. [DOI] [PubMed] [Google Scholar]
- 12.Kirkley A. Birmingham T.B. Litchfield R.B., et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N. Engl. J. Med. 2008;359:1097–1107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
- 13.Loza E. Benito-Ruiz P. Blanco F. de Miguel E. Roman J.A. Feasibility and efficacy of a multidisciplinary health care programme for patients with knee osteoarthritis. Clin. Exp. Rheumatol. 2011;29:913–920. [PubMed] [Google Scholar]
- 14.Fary R.E. Carroll G.J. Briffa T.G. Briffa N.K. The effectiveness of pulsed electrical stimulation in the management of osteoarthritis of the knee: results of a double-blind, randomized, placebo-controlled, repeated-measures trial. Arthritis Rheum. 2011;63:1333–1342. doi: 10.1002/art.30258. [DOI] [PubMed] [Google Scholar]
- 15.Whitehurst D.G. Bryan S. Hay E.M. Thomas E. Young J. Foster N.E. Cost-effectiveness of acupuncture care as an adjunct to exercise-based physical therapy for osteoarthritis of the knee. Phys. Ther. 2011;91:630–641. doi: 10.2522/ptj.20100239. [DOI] [PubMed] [Google Scholar]
- 16.Shen X. Zhao L. Ding G., et al. Effect of combined laser acupuncture on knee osteoarthritis: a pilot study. Lasers Med. Sci. 2009;24:129–136. doi: 10.1007/s10103-007-0536-9. [DOI] [PubMed] [Google Scholar]
- 17.Manek N.J. Lane N.E. Osteoarthritis: current concepts in diagnosis and management. Am. Fam. Physician. 2000;61:1795–1804. [PubMed] [Google Scholar]
- 18.Zvereva K.V. Gladkova N.D. Grunina E.A. Logunov P.L. The choice of the method for intravascular laser therapy in rheumatoid arthritis [in Russian] Ter. Arkh. 1994;66:29–32. [PubMed] [Google Scholar]
- 19.de Morton N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J. Physiother. 2009;55:129–133. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 20.The Metafor Package: A Meta-Analysis Package for R. http://www.metafor-project.org/ http://www.metafor-project.org/
- 21.Carvalho C.M. de Lacerda J.A. dos Santos Neto F.P. Cangussu M.C. Marques A.M. Pinheiro A.L. Wavelength effect in temporomandibular joint pain: a clinical experience. Lasers Med. Sci. 2010;25:229–232. doi: 10.1007/s10103-009-0695-y. [DOI] [PubMed] [Google Scholar]
- 22.Gur A. Karakoc M. Cevik R. Nas K. Sarac A.J. Efficacy of low power laser therapy and exercise on pain and functions in chronic low back pain. Lasers Surg. Med. 2003;32:233–238. doi: 10.1002/lsm.10134. [DOI] [PubMed] [Google Scholar]
- 23.Heussler J.K. Hinchey G. Margiotta E., et al. A double blind randomised trial of low power laser treatment in rheumatoid arthritis. Ann. Rheum. Dis. 1993;52:703–706. doi: 10.1136/ard.52.10.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Bie R.A. de Vet H.C. Lenssen T.F. van den Wildenberg F.A. Kootstra G. Knipschild P.G. Low-level laser therapy in ankle sprains: a randomized clinical trial. Arch. Phys. Med. Rehabil. 1998;79:1415–1420. doi: 10.1016/s0003-9993(98)90237-4. [DOI] [PubMed] [Google Scholar]
- 25.Ekim A. Armagan O. Tascioglu F. Oner C. Colak M. Effect of low level laser therapy in rheumatoid arthritis patients with carpal tunnel syndrome. Swiss Med. Wkly. 2007;137:347–352. doi: 10.4414/smw.2007.11581. [DOI] [PubMed] [Google Scholar]
- 26.Rogvi-Hansen B. Ellitsgaard N. Funch M. Dall-Jensen M. Prieske J. Low level laser treatment of chondromalacia patellae. Int. Orthop. 1991;15:359–361. doi: 10.1007/BF00186879. [DOI] [PubMed] [Google Scholar]
- 27.Aigner N. Fialka C. Radda C. Vecsei V. Adjuvant laser acupuncture in the treatment of whiplash injuries: a prospective, randomized placebo-controlled trial. Wien Klin. Wochenschr. 2006;118:95–99. doi: 10.1007/s00508-006-0530-4. [DOI] [PubMed] [Google Scholar]
- 28.Yurtkuran M. Alp A. Konur S. Ozcakir S. Bingol U. Laser acupuncture in knee osteoarthritis: a double-blind, randomized controlled study. Photomed. Laser Surg. 2007;25:14–20. doi: 10.1089/pho.2006.1093. [DOI] [PubMed] [Google Scholar]
- 29.Konstantinovic L.M. Cutovic M.R. Milovanovic A.N., et al. Low-level laser therapy for acute neck pain with radiculopathy: a double-blind placebo-controlled randomized study. Pain Med. 2010;11:1169–1178. doi: 10.1111/j.1526-4637.2010.00907.x. [DOI] [PubMed] [Google Scholar]
- 30.Konstantinovic L.M. Kanjuh Z.M. Milovanovic A.N., et al. Acute low back pain with radiculopathy: a double-blind, randomized, placebo-controlled study. Photomed. Laser Surg. 2010;28:553–560. doi: 10.1089/pho.2009.2576. [DOI] [PubMed] [Google Scholar]
- 31.Fikácková H. Dostalova T. Navratil L. Klaschka J. Effectiveness of low-level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed. Laser Surg. 2007;25:297–303. doi: 10.1089/pho.2007.2053. [DOI] [PubMed] [Google Scholar]
- 32.Meireles S.M. Jones A. Jennings F. Suda A.L. Parizotto N.A. Natour J. Assessment of the effectiveness of low-level laser therapy on the hands of patients with rheumatoid arthritis: a randomized double-blind controlled trial. Clin. Rheumatol. 2010;29:501–509. doi: 10.1007/s10067-009-1347-0. [DOI] [PubMed] [Google Scholar]
- 33.Basford J.R. Sheffield C.G. Mair S.D. Ilstrup D.M. Low-energy helium neon laser treatment of thumb osteoarthritis. Arch. Phys. Med. Rehabil. 1987;68(11):794–797. [PubMed] [Google Scholar]
- 34.Brosseau L. Wells G. Marchand S., et al. Randomized controlled trial on low level laser therapy (LLLT) in the treatment of osteoarthritis (OA) of the hand. Lasers Surg. Med. 2005;36:210–219. doi: 10.1002/lsm.20137. [DOI] [PubMed] [Google Scholar]
- 35.Stelian J. Gil I. Habot B., et al. Improvement of pain and disability in elderly patients with degenerative osteoarthritis of the knee treated with narrow-band light therapy. J. Am. Geriatr. Soc. 1992;40:23–26. doi: 10.1111/j.1532-5415.1992.tb01824.x. [DOI] [PubMed] [Google Scholar]
- 36.Bulow P.M. Jensen H. Danneskiold-Samsoe B. Low power Ga-Al-As laser treatment of painful osteoarthritis of the knee. A double-blind placebo-controlled study. Scand. J. Rehabil. Med. 1994;26:155–159. [PubMed] [Google Scholar]
- 37.Gur A. Cosut A. Sarac A.J. Cevik R. Nas K. Uyar A. Efficacy of different therapy regimes of low-power laser in painful osteoarthritis of the knee: a double-blind and randomized-controlled trial. Lasers Surg. Med. 2003;33:330–338. doi: 10.1002/lsm.10236. [DOI] [PubMed] [Google Scholar]
- 38.Tascioglu F. Armagan O. Tabak Y. Corapci I. Oner C. Low power laser treatment in patients with knee osteoarthritis. Swiss Med. Wkly. 2004;134:254–258. doi: 10.4414/smw.2004.10518. [DOI] [PubMed] [Google Scholar]
- 39.Hegedus B. Viharos L. Gervain M. Galfi M. The effect of low-level laser in knee osteoarthritis: a double-blind, randomized, placebo-controlled trial. Photomed. Laser Surg. 2009;27:577–584. doi: 10.1089/pho.2008.2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ozdemir F. Birtane M. Kokino S. The clinical efficacy of low-power laser therapy on pain and function in cervical osteoarthritis. Clin. Rheumatol. 2001;20:181–184. doi: 10.1007/s100670170061. [DOI] [PubMed] [Google Scholar]
- 41.Kulekcioglu S. Sivrioglu K. Ozcan O. Parlak M. Effectiveness of low-level laser therapy in temporomandibular disorder. Scand. J. Rheumatol. 2003;32:114–118. doi: 10.1080/03009740310000139. [DOI] [PubMed] [Google Scholar]
- 42.Venancio R. de A. Camparis C.M. Lizarelli R. de F. Low intensity laser therapy in the treatment of temporomandibular disorders: a double-blind study. J. Oral Rehabil. 2005;32:800–807. doi: 10.1111/j.1365-2842.2005.01516.x. [DOI] [PubMed] [Google Scholar]
- 43.Cetiner S. Kahraman S.A. Yucetas S. Evaluation of low-level laser therapy in the treatment of temporomandibular disorders. Photomed. Laser Surg. 2006;24:637–641. doi: 10.1089/pho.2006.24.637. [DOI] [PubMed] [Google Scholar]
- 44.Emshoff R. Bosch R. Pumpel E. Schoning H. Strobl H. Low-level laser therapy for treatment of temporomandibular joint pain: a double-blind and placebo-controlled trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008;105:452–456. doi: 10.1016/j.tripleo.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 45.Santos T. de S. Piva M.R. Ribeiro M.H. Antunes A.A. Melo A.R. Silva E.D. Lasertherapy efficacy in temporomandibular disorders: control study. Braz. J. Otorhinolaryngol. 2010;76:294–299. doi: 10.1590/S1808-86942010000300004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klein R.G. Eek B.C. Low-energy laser treatment and exercise for chronic low back pain: double-blind controlled trial. Arch. Phys. Med. Rehabil. 1990;71:34–37. [PubMed] [Google Scholar]
- 47.Soriano F. Rios R. Gallium arsenide laser treatment of chronic low back pain: a prospective, randomized and double blind study. Laser Therapy. 1998;10:175–180. [Google Scholar]
- 48.Basford J.R. Sheffield C.G. Harmsen W.S. Laser therapy: a randomized, controlled trial of the effects of low-intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch. Phys. Med. Rehabil. 1999;80:647–652. doi: 10.1016/s0003-9993(99)90167-3. [DOI] [PubMed] [Google Scholar]
- 49.Ay S. Dogan S.K. Evcik D. Is low-level laser therapy effective in acute or chronic low back pain? Clin. Rheumatol. 2010;29:905–910. doi: 10.1007/s10067-010-1460-0. [DOI] [PubMed] [Google Scholar]
- 50.Bingol U. Altan L. Yurtkuran M. Low-power laser treatment for shoulder pain. Photomed. Laser Surg. 2005;23:459–464. doi: 10.1089/pho.2005.23.459. [DOI] [PubMed] [Google Scholar]
- 51.Stergioulas A. Low-power laser treatment in patients with frozen shoulder: preliminary results. Photomed. Laser Surg. 2008;26:99–105. doi: 10.1089/pho.2007.2138. [DOI] [PubMed] [Google Scholar]
- 52.Chow R.T. Heller G.Z. Barnsley L. The effect of 300 mW, 830 nm laser on chronic neck pain: a double-blind, randomized, placebo-controlled study. Pain. 2006;124:201–210. doi: 10.1016/j.pain.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 53.World Association of Laser Therapy. Recommended treatment doses for low level laser therapy. 2010. http://www.walt.nu http://www.walt.nu