Abstract
Background
Research conducted using small samples of persons exposed to extreme stressors has documented an association between parental and offspring posttraumatic stress disorder (PTSD), but it is unknown whether this association exists in the general population and whether trauma exposure mediates this association. We sought to determine whether mothers’ posttraumatic stress symptoms were associated with PTSD in their young adult children and whether this association was mediated by higher trauma exposure in children of women with PTSD.
Methods
Using data from a cohort of mothers (n=6924) and a cohort of their children (n=8453), we calculated risk ratios (RR) for child’s PTSD and examined mediation by trauma exposure.
Results
Mother’s lifetime posttraumatic stress symptoms were associated with child’s PTSD in dose-response fashion (mother’s 1 to 3 symptoms, child’s RR=1.2; mother’s 4-5 symptoms, RR=1.3; mother’s 6-7 symptoms, RR=1.6, compared to children of mothers with no symptoms, p<0.001 for each). Mother’s lifetime symptoms were also associated with child’s trauma exposure in dose-response fashion. Elevated exposure to trauma substantially mediated elevated risk for PTSD in children of women with symptoms (mediation proportion, 74%, p<0.001).
Conclusions
Intergenerational association of PTSD is clearly present in a large population-based sample. Children of women who had PTSD were more likely than children of women without PTSD to experience traumatic events; this suggests, in part, why the disorder is associated across generations. Health care providers who treat mothers with PTSD should be aware of the higher risk for trauma exposure and PTSD in their children.
Keywords: Posttraumatic stress disorder, trauma, childhood abuse, epidemiology, family studies, violence
Introduction
Posttraumatic stress disorder (PTSD) has severe behavioral and health sequelae that may interfere with educational, career and interpersonal goals. Several studies have shown an association between parental and offspring PTSD in selected populations of children of refugees, war veterans, or victims of other major traumas[1-6]. The evidence however, is conflicting. Although some studies have found up to five times greater risk for PTSD in children of parents with PTSD compared with children of parents without PTSD[2, 4, 5, 7, 8], other studies have found no increased risk[6, 9-11]. These investigations may have produce inconsistent findings due to the small number of participants in most studies[1, 3, 4, 6, 9-12], recruitment of participants on the basis of trauma exposure[1-3, 6, 9, 11-14] or from clinics[2, 9], restriction to families in which parents and children were exposed to the same event (e.g., war)[4, 15] or to children of persons exposed to extremely severe traumas (e.g., the Holocaust, torture)[3, 8, 14, 16-18]. Thus it is unknown whether intergenerational transmission of PTSD occurs in relation to more usual events occurring in civilian populations or in families in which parents and children are not exposed to the same traumatic incident. Moreover, our understanding of possible mechanisms of intergenerational PTSD transmission is highly limited, both due to the scarcity of studies examining possible mechanisms and to the uncertain generalizability of these studies[2].
The present paper builds on this prior work in four ways. First, we assess here, to our knowledge for the first time, intergenerational PTSD association in a large population-based sample exposed to a range of traumatic events common in civilian populations. Second, in our study mothers and their young adult offspring reported their own trauma exposure and PTSD, reducing concerns about reporting bias and low sensitivity resulting from children reporting parents’ PTSD[1] or parents reporting children’s PTSD[19-21]. Third, we test whether the association between maternal and child PTSD is mediated by child’s exposure to traumatic events. Elevated exposure to trauma in the children may be one mechanism by which PTSD is transmitted across generations, as prior work has suggested that PTSD in parents may put their children at increased risk of exposure to trauma[5, 22-24], and exposure to a larger number of traumatic events has been associated with increased risk of developing PTSD[25-28]. Finally, our large sample of young adult children enables us to test for sex differences in intergenerational association of PTSD. Men and women experience different types of traumas, frequency of exposure to trauma[29], risk of PTSD following trauma[30], and prevalence of PTSD[29], thus intergenerational transmission of PTSD may also differ by sex.
Methods
Sample
We assess the relationship between maternal and child PTSD in two longitudinal cohorts, the Nurses’ Health Study II (NHSII), a cohort of women, and the Growing Up Today Study (GUTS), a cohort of their children. The NHSII is a cohort of 116,430 female nurses from 14 populous U.S. states whose nursing boards were able to provide information on nurses’ gender and birth date. Because the goal of the NHSII was to establish a long-term longitudinal cohort, only the most responsive potential participants were enrolled: women who agreed to enroll after a single mailing and who returned the initial questionnaire after only one request. The overall response rate to the baseline mailing was thus approximately 123,000 of 517,000 (24%). The cohort was established in 1989 and followed up biennially. In 2008, when respondents were age 44 to 62 years, we mailed the Trauma and PTSD Screening Questionnaire[31, 32] to 60,804 participants who had completed recent questionnaires (to retain participation in the longitudinal study, participants who have not responded to the most recent biennial questionnaire are not asked to participate in supplemental studies). The response rate was 89% (n=54,282).
GUTS is a cohort of 16,882 children of NHSII participants, established in 1996 and followed up annually or biennially. GUTS investigators initially contacted the 34,174 NHSII women who were mothers of children ages 9 to 14 year to request consent for their children to participate in GUTS; 18,526 mothers (54%) consented. In 1996, 13,261 girls and 13,504 boys whose mothers had granted consent were invited to participate. Approximately 68% of the girls (n=9,039) and 58% of the boys (N=7,843) returned completed questionnaires, thereby assenting to participate. Exposure to traumatic events and lifetime probable PTSD were assessed in the 2007 wave (n=9864), when respondents were age 19 to 27 years (mean age=22.7 years). We restrict our analyses to families in which both mother and child(ren) responded to the trauma and PTSD questionnaires (n=6924 mothers, n=8453 children).
Measures
NHSII mothers’ exposure to traumatic events was measured in 2008. Lifetime trauma was measured with a modified version of the Brief Trauma Questionnaire[31, 32]. The 16-item questionnaire queried exposure to 15 traumas as well as “a seriously traumatic event not already covered,” each coded present or absent[31]. These mothers’ experiences of childhood maltreatment and intimate partner abuse were measured in more detail in a 2001 questionnaire. Childhood sexual abuse victimization was assessed for two age periods, age 11 years or younger, and ages 12 to 17 years, with two questions about actions by an adult or older child touching or forcing to touch in a sexual way, and forcing or attempting to force sexual activity by threatening, holding down, or hurting the respondent[33] and was coded any or none. Physical abuse was measured with 4 questions from the Conflict Tactic Scales regarding perpetration by an adult in the family, also for two age periods, age 11 years or younger, and ages 12 to 17 years. Respondents who were ever kicked, punched, attacked, hit with something, or choked or burned were considered physically abused[34]. Additionally, respondents who reported having been hit so hard they were bruised or marked in response to a question from the Child Trauma Questionnaire were considered physically abused[35]. Emotional abuse at ages 11 years or younger was measured with 4 questions from the Child Trauma Questionnaire about frequency of adults in the family: screaming, saying insulting things, punishing in a way that seemed cruel, and making the child feel important (reverse coded)[35]. Each emotional abuse item was coded from 0 (never) to 4 (very often), and a score was formed from the sum. Respondents whose mean score was “sometimes” were considered emotionally abused. Intimate partner abuse was assessed with a modified version of the Assessing Abuse Scale[36].
NHSII mothers’ lifetime PTSD symptoms were assessed in 2008 with the 7-item Short Screening Scale with respect to their worst or most distressing trauma[37]. Mothers were additionally asked to report the year in which this worst event occurred. To investigate a possible dose-response relationship between risk of child’s PTSD with mother’s PTSD symptoms, we grouped mother’s number of symptoms as 0, 1-3, 4-5 and 6-7.
GUTS children’s exposure to traumatic events
In 2007, when offspring were ages 19 to 27 years (mean age=22), lifetime exposure to trauma was measured with a 12-item modified version of the Brief Trauma Questionnaire[31, 32] regarding exposure to 11 specific items, including accidents, illness, witnessing violence, sudden death of a loved one and an additional item querying exposure to “a seriously traumatic event not already covered.” Each item was coded present or absent. Exposure to childhood maltreatment was measured in more detail. Children’s sexual abuse victimization was assessed and coded identically to the NHSII mothers’ victimization[33]. Physical abuse was coded identically to mothers’ physical abuse, except that experiences of being kicked, punched, hit with something that hurt, or attacked in some other way were queried with one item rather than three separate items[34]. Child’s emotional abuse was measured and coded identically to mother’s, except that abuse at ages 11 to 17 was also assessed[35]. Witnessing abuse in childhood was assessed with 6 questions regarding physical and emotional abuse of mother, another adult, or another child in the household, and was coded present or absent. Intimate partner abuse was assessed identically to mothers’[36].
Child’s number of event types was a count of trauma types and child abuse types endorsed. Because few children endorsed more than 8 events, we coded 8 or more events as 8 to enable models to converge. We were unable to calculate the total number of events to which children were exposed because, to minimize respondent burden, our questionnaire did not query the number of instances for each event type (e.g., we did not ask, “How many serious car accidents have you experienced?”).
Child’s PTSD
Following the traumatic event questionnaires, children were asked to think about the event that was most distressing for them and were then asked about symptoms of PTSD. Lifetime PTSD was measured with the 7-item Short Screening Scale for DSM-IV PTSD, with 4 or more symptoms indicating probable PTSD[37]. The Short Scale identified PTSD cases with a sensitivity of 80%, specificity of 97%, positive predictive value of 71%, and negative predictive value of 98% in a representative sample of Detroit residents ages 18-45 years[37]. In the present study, we describe children as having “PTSD” if they reported 4 or more lifetime symptoms on this scale.
Covariates
Nurse’s socioeconomic status was measured in 2001 with the US MacArthur Scale of Subjective Social Status[38]. Participants were shown a picture of a ladder that represented the US and were asked to select the rung they felt represented their socioeconomic status, with 1 representing the highest and 10 the lowest status. Nurse’s self-reported family income in 2001 was measured in 9 levels, from less than $15,000 to more than $150,000. Nurse’s childhood socioeconomic status was measured by the maximum of her parents’ education at her birth, assessed by self-report in 2005.
Analyses
We examined prevalence of lifetime PTSD and exposure to traumatic events in mothers and children. To ascertain whether the mother’s PTSD symptoms were associated with the number of event types to which the child was exposed, we first calculated prevalence of event types in children by each level of mother’s PTSD symptoms (e.g., 0, 1-3, 4-5, or 6-7 symptoms). We then modeled child’s number of traumatic event types as the dependent variable with mother’s PTSD symptoms as the independent variable. To investigate possible sex differences, we tested a mother’s-PTSD-symptoms-by-child’s-sex interaction term and compared findings in models stratified by sex.
To investigate whether child’s PTSD was associated with mother’s PTSD symptoms, we modeled child’s PTSD as a function of mother’s PTSD symptoms. To examine possible sex differences in this relationship, we tested for a mother’s-PTSD-symptoms-by-child’s-sex interaction and ran models stratified by sex. To estimate the extent to which the relationship between mother’s PTSD symptoms and child’s risk of PTSD was mediated through child’s event exposure, we compared models with and without child’s number of traumatic event types. These models were restricted to children who reported at least one trauma, since there was no risk of PTSD for children reporting no traumatic events. We then calculated the mediation proportion, which is the proportion of the relationship between mother’s PTSD symptoms and child’s risk of PTSD explained by number of child’s trauma types, using the publically available Mediate macro[39, 40]. To investigate mediation of the association between mother’s PTSD symptoms and child’s risk of PTSD by type of child’s event exposure, we created a single model of child’s PTSD risk as a function of mother’s PTSD symptoms, with 15 dichotomous variables indicating presence or absence of each of the event types (e.g., natural disaster, accident) rather than child’s total number of event types and again calculated the mediation proportion.
We conducted three sensitivity analyses to explore our findings. First, as mother and child’s PTSD may be associated solely due to exposure to the same trauma incident or because a trauma to the child caused PTSD symptoms in the mother, we additionally modeled children’s risk of PTSD as a function of mother’s PTSD symptoms in mothers whose worst traumatic event preceded the child’s birth (42% of all mothers, N=2968). Second, because mother’s PTSD symptoms may have been associated with child’s PTSD due to mother’s other mental illnesses rather than PTSD symptoms, we modeled child’s PTSD as a function of mother’s number of PTSD symptoms adjusted for mother’s lifetime depression (coded any or none), phobic anxiety (measured by the Middlesex Hospital Questionnaire in 2005[41], coded in quartiles[42]), and past year binge drinking, measured in 2005. Third, to adjust more extensively for socioeconomic status, we added two additional measures to the models: nurse’s self-reported socioeconomic status in 2001 and family income in 2001. We did not include these measures in the main analyses as maternal PTSD status may have affected perceived socioeconomic status and family income. Additionally, 16% of nurses did not report family income.
All models were adjusted for maternal childhood socioeconomic status and child’s age and sex or were stratified by sex. As some women enrolled more than one child in GUTS, we used generalized estimating equations to account for clustering of data by family, with a log link and Poisson distribution to estimate risk ratios (RR) for dichotomous variables[43] and an identity link and Poisson distribution for models of number of child’s traumatic events, using SAS 9.2[44, 45].
Results
Mothers in our sample were a mean age of 55 years in 2008, as were women in the whole NHS II. Mothers in our sample were somewhat more likely to be White (98% versus 95%), less likely to be Hispanic (1.5% versus 1.9%) and were more likely to have been married at baseline (95% versus 77%) compared with the whole NHS II. Children in our study were the same mean age, 12 years, as the whole GUTS sample at baseline. Children in our sample were slightly less likely to be Hispanic (1.4% versus 1.6%) and more likely to be White (94% versus 93%) than the whole GUTS sample.
Both mothers and children were exposed to a wide variety of traumatic event types. For mothers, the most prevalent events were childhood physical abuse and emotional intimate partner abuse (46% and 34% of mothers exposed, respectively) (Table 1). For female children, emotional intimate partner abuse and stalking were most prevalent (31% and 21% exposed). For male children, witnessing someone hurt or killed and accidents were the most common events (20% and 17% exposed). Mothers reported a mean of 3.5 lifetime event types (standard deviation (SD)=2.4), while female children reported 2.3 (SD=1.9) and male children reported 1.9 (SD=1.7) mean event types. Lifetime PTSD was 21% in mothers, 29% in daughters, and 18% in sons.
Table 1. Lifetime prevalence of probable PTSD and potentially traumatic events in NHS II mothers and their GUTS adult children.
| Mothers (Nurses’ Health Study II, N=6924) |
Female children (GUTS, N=5209) |
Male children (GUTS, N=3244) |
|
|---|---|---|---|
|
| |||
| Lifetime prevalence % (N) | |||
|
| |||
| Probable PTSD | 20.7 (1237) | 28.8 (1500) | 17.7 (575) |
| Traumatic events | |||
| Natural disaster | 11.2 (685) | 5.9 (303) | 6.9 (217) |
| Accident | 15.6 (951) | 16.0 (822) | 17.3 (543) |
| Illness | 10.5 (641) | 2.0 (104) | 1.4 (43) |
| War zone | 1.2 (75) | 0.8 (42) | 2.7 (84) |
| Family or friend die violently |
21.7 (1326) | 15.6 (801) | 12.3 (385) |
| Attacked/mugged | 10.7 (655) | 12.1 (618) | 13.8 (425) |
| Witness someone hurt/killed |
17.7 (1085) | 12.1 (620) | 20.1 (633) |
| Stalked | 10.9 (756) | 21.2 (1083) | 10.4 (323) |
| Intimate partner abuse | |||
| Physical | 20.4 (1398) | 13.9 (677) | 12.5 (362) |
| Forced sex | 8.8 (602) | 12.6 (614) | 2.5 (71) |
| Emotional | 34.5 (2364) | 30.7 (1496) | 15.9 (458) |
| Child abuse | |||
| Sexual | 32.1 (2206) | 14.2 (723) | 4.8 (150) |
| Physical | 45.6 (3153) | 15.1 (754) | 16.6 (504) |
| Emotional, before age 11 years |
15.4 (1073) | 5.4 (268) | 3.3 (98) |
| Other traumatic event | 15.9 (970) | 22.6 (1373) | 15.5 (555) |
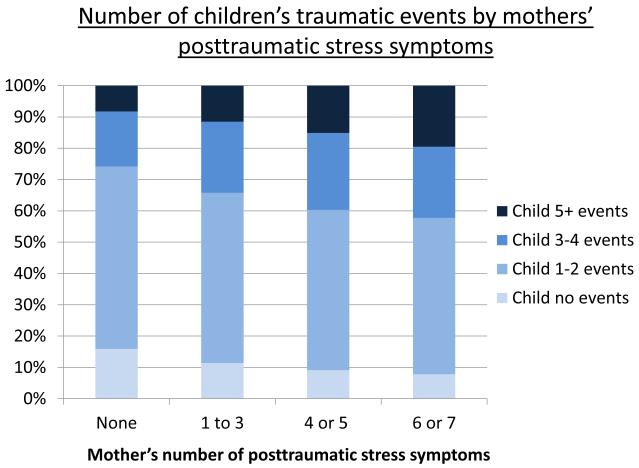
Mother’s PTSD symptoms were associated with the number of events to which her child was exposed in dose-response fashion (Figure 1). While 15.9% of children of mothers with no PTSD symptoms had no trauma exposure, only 7.8% of children of mothers with 6 or 7 PTSD symptoms had no trauma exposure. Similarly, 19.5% of children of mothers with 6 or 7 PTSD symptoms were exposed to 5 or more traumatic events, while only 8.2% of children of mothers with no PTSD symptoms were exposed to 5 or more events. In a model with child’s number of traumatic events as the dependent variable and mother’s PTSD symptoms as the independent variable, mother’s symptoms remained associated in dose-response fashion with child’s number of traumatic event types (1-3 PTSD symptoms were associated with 0.4 additional event types (95% CI=0.3, 0.5); 4-5 symptoms were associated with 0.6 additional types (95% CI=0.5, 0.8); 6-7 symptoms were associated with 0.9 additional types (95% CI=0.7, 1.1)). Mother’s-PTSD-symptoms-by-child’s-sex interaction term was not statistically significant in this model, and findings in models stratified by sex were similar for both sexes.
Figure 1.
Child’s number of traumatic event types by mother’s posttraumatic stress symptoms, NHS II and GUTS cohorts, n=6924 mothers, n=8453 children.
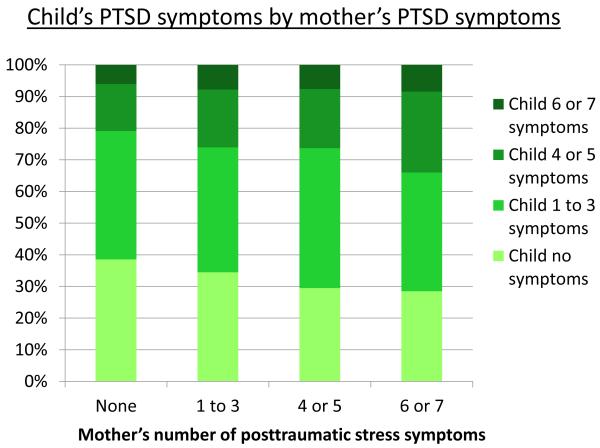
Mother’s PTSD symptoms were also associated with increased risk of child’s PTSD in dose-response fashion, such that the child of a woman with 6 or 7 PTSD symptoms was at 60% greater risk of PTSD than a child of a woman with no PTSD symptoms (RR=1.6, 95% confidence interval (CI)=1.4, 1.9, p<0.001, Table 2, Model 1, Figure 2). The maternal-PTSD-symptoms-by-child’s-sex interaction term was not statistically significant in this model, and findings were similar in models stratified by sex. In models including the number of events to which children were exposed and restricted to children exposed to at least one event, the association between mother’s PTSD symptoms and child’s risk of PTSD was greatly attenuated, though still statistically significant. Children’s exposure to traumatic events substantially mediated the relationship between mother’s PTSD symptoms and children’s PTSD (mediation proportion, 74%, Table 2, Models 2 and 3). In additional exploration of mediation, the mediation proportion by specific event types was also substantial (53%, p<0.001), although slightly attenuated compared with mediation by number of child’s event types.
Table 2. Risk ratios for lifetime probable PTSD in child associated with number of PTSD symptoms in the mother, with mediation by number of traumatic event types to which child is exposed (N=7341)†.
| Independent variables |
Model 1 | Model 2 | Model 3 | Proportion of effect mediated by child’s number of event types |
|
|---|---|---|---|---|---|
|
| |||||
| All children | Restricted to children exposed to at least one traumatic event |
||||
|
| |||||
| N | Risk ratio (95% confidence interval) | ||||
| Mother’s PTSD | |||||
| symptoms | |||||
| 0 symptoms | 3407 | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] | 74%*** |
| 1-3 symptoms | 2362 | 1.2 (1.1, 1.4)*** | 1.2 (1.1, 1.3)*** | 1.1 (1.0, 1.2)* | |
| 4-5 symptoms | 996 | 1.3 (1.1, 1.4)*** | 1.2 (1.0, 1.3)* | 1.0 (0.9, 1.2) | |
| 6-7 symptoms | 488 | 1.6 (1.4, 1.9)*** | 1.5 (1.3, 1.7)*** | 1.3 (1.1, 1.5)*** | |
|
Child’s number of event types |
|||||
| 1 | 1.0 [Reference] | ||||
| 2 | 1.1 (0.9, 1.2) | ||||
| 3 | 1.5 (1.3, 1.7)*** | ||||
| 4 | 1.8 (1.6, 2.1)*** | ||||
| 5 | 2.3 (2.0, 2.6)*** | ||||
| 6 | 2.4 (2.0, 2.7)*** | ||||
| 7 | 2.9 (2.5, 3.4)*** | ||||
| 8 | 3.1 (2.7, 3.6)*** | ||||
Models adjusted for maternal childhood socioeconomic status, child’s sex, and age of child. Difference from reference group, χ2 test significant at:
=p<0.05
= p<0.01
=p<0.001.
Figure 2.
Child’s number of PTSD symptoms by mother’s posttraumatic stress symptoms, NHS II and GUTS cohorts, n=6924 mothers, n=8453 children.
Results were similar in sensitivity analyses restricted to mothers whose worst traumatic event preceded the child’s birth (mother’s 1-3 symptoms, child PTSD RR=1.3, 95% CI=1.1, 1.5; 4-5 symptoms, RR=1.4, 95% CI=1.2, 1.7; 6-7 symptoms, RR=1.5, 95% CI=1.2, 1.8). Mediation by child’s number of events in this subsample was also similar to analyses using the entire sample. Additionally, the association of mother’s PTSD symptoms with child’s PTSD did not substantively differ in models including mother’s lifetime depression, phobic anxiety, and binge drinking or perceived socioeconomic status and income in 2001.
Discussion
Our results suggest that risk for PTSD may be transmitted intergenerationally in a large population-based sample. We found a dose-response relationship: women who had experienced high levels of PTSD symptoms during their life had children at higher risk of PTSD compared to women with lower levels of PTSD symptoms. Elevated exposure to traumatic events in children of mothers with PTSD was likely a major mechanism for this risk transmission. However, we found that mother’s PTSD symptoms predicted child’s PTSD even after extensive adjustment for child’s trauma exposure. Although prevalence of PTSD and exposure to specific event types differed by child’s sex, we did not find sex differences in the relationship between mother’s PTSD symptoms and child’s trauma exposure or PTSD. Maternal PTSD symptoms were associated with increased event exposure and greater risk of PTSD for both males and females.
Our study is the first to demonstrate intergenerational association of PTSD in a population-based sample exposed to a variety of traumatic events. A further strength of our study is that PTSD symptoms and exposure to multiple traumas were assessed independently in each generation by self-report rather than by family history, with many identical measures given to the two generations. Moreover, assessment of the timing of the onset of PTSD symptoms in mothers provided evidence that the association we found between maternal PTSD and child PTSD was not substantially due to shared trauma exposure causing PTSD in both mother and child or child’s trauma exposure causing PTSD symptoms in the mother. In analyses restricted to mothers whose index trauma occurred before the birth of her child, maternal PTSD remained associated with increased PTSD in the child. Prior studies of families exposed to extreme stressors, such as war, have had mixed findings regarding whether parental PTSD is associated with increased risk of PTSD in children. However, due to the selection of participants and small sample sizes, the relevance of these studies to the general population is unclear. By examining intergenerational transmission in a large population-based sample not selected on the basis of trauma exposure or PTSD, we provide the most compelling evidence to date that PTSD is transmitted intergenerationally. The size of the intergenerational association we found is slightly smaller than associations found for depression and other anxiety disorders. Studies examining depression and social phobia have found two to three times greater risk for those illnesses among children of affected mothers compared with children of unaffected mothers[46, 47].
We identify increased exposure to traumatic events in children of women with PTSD as a principal mechanism for intergenerational transmission of PTSD. Studies conducted primarily in the families of war veterans and disaster survivors have suggested several pathways by which parental PTSD may increase risk for child’s trauma exposure. PTSD negatively affects parenting, such that children of parents with PTSD are more likely to be abused[7, 14, 15, 18, 48]. Mother’s PTSD may also affect the child’s risk of trauma exposure through PTSD sequelae that disrupt family life, including substance abuse, job loss, and divorce[49-51]. Social, emotional, and cognitive deficits found in children of parents with PTSD may also put these children at greater risk for trauma[52-54]. We found that increased risk of trauma exposure only partly mediated intergenerational transmission of PTSD, thus there are likely other mechanisms we did not explore. Maternal PTSD during gestation may increase risk for child’s PTSD through epigenetic or other mechanisms[3, 55-57]. In addition, maternal PTSD may also be an indicator of shared risk for exposure to trauma and consequent PTSD rather than solely a cause of trauma and PTSD risk. For example, the association we found between mother’s PTSD symptoms and child’s PTSD may reflect common risk factors to which both mothers and children are exposed, for example, hazardous residential location or chronic adversity[52, 58], although results were unchanged in models adjusted for nurses’ childhood and adulthood socioeconomic status. Traits, including risk-taking, IQ, and neuroticism[59-61], and learned behaviors, such as approaches to conflict resolution, that put mothers at increased risk of trauma exposure and PTSD may be shared across generations due to genetic or other mechanisms, and may also lead to an association between maternal PTSD symptoms and child’s risk of PTSD[59, 62-67]. It is also possible, however, that had we measured trauma exposure more precisely, including the number and severity of specific traumas, we would have obtained a larger estimate of mediation by trauma exposure.
Our findings suggest that despite notable sex differences in type of trauma exposure, male and female children may be equally affected by parent’s PTSD. Few prior studies have examined sex difference in the effect of parental PTSD on children[7, 22, 24], although small studies in selected samples have had mixed findings[68, 69]. Although in general females are at higher risk of PTSD than males, clinicians should note that sons as well as daughters of women with PTSD may be at elevated risk of trauma exposure and PTSD compared with children of women without PTSD.
Our study has two main limitations. Because our study participants were primarily White US nurses ages 46 to 64 and their children, our results may not apply to other demographic groups. The nurse mothers may have experienced more work-related trauma and fewer traumas outside of work, due respectively to their occupation and high level of education, compared with the general population. Participants in the present study were a subsample of two larger cohorts, therefore study attrition and nonresponse may have biased our results. NHSII participants in our study were healthier than the whole NHSII at baseline on several measures, including lifetime smoking, alcohol consumption, and body mass index. Similarly, GUTS participants in our sample were slightly less likely to have ever smoked at baseline and were less likely to be overweight than the whole cohort. Dropout of less healthy mothers and children may have attenuated our findings. We also note that we used a validated measure of PTSD relying on participant reports; although this is consistent with a large body of epidemiological literature it does not constitute a clinical diagnosis.
We present the most comprehensive examination of intergenerational transmission of PTSD symptoms and trauma to date. Our findings have implications for research and practice. In terms of practice, health care providers who treat mothers for PTSD should be aware of the higher risk of trauma exposure and PTSD in their children. In terms of research, future studies must determine whether pathways connecting parental PTSD with child trauma in families of war veterans and disaster survivors apply to the general population or whether different pathways need to be considered. Such studies would facilitate the design and evaluation of interventions to reduce trauma exposure and PTSD in at-risk children.
Acknowledgements
This study was supported by the National Institutes of Health Grants MH070627 and MH078928 (ALR, KCK), R01 HL064108 (RW), K01DA030449 (MC), R01MH082729 (SG), and the Leadership Education in Adolescent Health project, Maternal and Child Health Bureau, HRSA grant 6T71-MC00009-17 (SBA). This study was also supported by National Institutes of Health Grant R01CA50385 to support the Nurses’ Health Study II cohort follow-up. We acknowledge the Channing Laboratory, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School for its management of the Growing Up Today Study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure
The authors report no biomedical financial interests or potential conflicts of interest.
References
- 1.Yehuda R, Halligan SL, Bierer LM. Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. J Psychiatr Res. 2001;35(5):261–270. doi: 10.1016/s0022-3956(01)00032-2. [DOI] [PubMed] [Google Scholar]
- 2.Daud A, Skoglund E, Rydelius PA. Children in families of torture victims: Transgenerational transmission of parents’ traumatic experiences to their children. International Journal of Social Welfare. 2005;14(1):23–32. [Google Scholar]
- 3.Yehuda R, Bell A, Bierer LM, Schmeidler J. Maternal, not paternal, PTSD is related to increased risk for PTSD in offspring of Holocaust survivors. J Psychiatr Res. 2008;42(13):1104–1111. doi: 10.1016/j.jpsychires.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sack WH, Clarke GN, Seeley J. Posttraumatic stress disorder across two generations of Cambodian refugees. J Am Acad Child Adolesc Psychiatry. 1995;34(9):1160–1166. doi: 10.1097/00004583-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Famularo R, Fenton T, Kinscherff R, Ayoub C, Barnum R. Maternal and child posttraumatic stress disorder in cases of child maltreatment. Child Abuse & Neglect. 1994;18(1):27–36. doi: 10.1016/0145-2134(94)90093-0. [DOI] [PubMed] [Google Scholar]
- 6.van IJzendoorn MH, Bakermans-Kranenburg MJ, Sagi-Schwartz A. Are children of Holocaust survivors less well-adapted? A meta-analytic investigation of secondary traumatization. J Trauma Stress. 2003;16(5):459–469. doi: 10.1023/A:1025706427300. [DOI] [PubMed] [Google Scholar]
- 7.Dekel R, Goldblatt H. Is there intergenerational transmission of trauma? The case of combat veterans’ children. Am J Orthopsychiatry. 2008;78(3):281–289. doi: 10.1037/a0013955. [DOI] [PubMed] [Google Scholar]
- 8.Baider L, Peretz T, Hadani PE, Perry S, Avramov R, De-Nour AK. Transmission of Response to Trauma? Second-Generation Holocaust Survivors’ Reaction to Cancer. Am J Psychiatry. 2000;157(6):904–910. doi: 10.1176/appi.ajp.157.6.904. [DOI] [PubMed] [Google Scholar]
- 9.Westerink J, Giarratano L. The impact of posttraumatic stress disorder on partners and children of Australian Vietnam veterans. Australian and New Zealand Journal of Psychiatry. 1999;33(6):841–847. doi: 10.1046/j.1440-1614.1999.00638.x. [DOI] [PubMed] [Google Scholar]
- 10.Sagi-Schwartz A, Van IMH, Grossmann KE, Joels T, Grossmann K, Scharf M, Koren-Karie N, Alkalay S. Attachment and traumatic stress in female holocaust child survivors and their daughters. Am J Psychiatry. 2003;160(6):1086–1092. doi: 10.1176/appi.ajp.160.6.1086. [DOI] [PubMed] [Google Scholar]
- 11.Mellor DJ, Davidson AC. The adjustment of children of Australian Vietnam veterans: is there evidence for the transgenerational transmission of the effects of war-related trauma? Australian & New Zealand Journal of Psychiatry. 2001;35(3):345–351. doi: 10.1046/j.1440-1614.2001.00897.x. [DOI] [PubMed] [Google Scholar]
- 12.Davidson AC, Mellor DJ. The adjustment of children of Australian Vietnam veterans: is there evidence for the transgenerational transmission of the effects of war-related trauma? Aust N Z J Psychiatry. 2001;35(3):345–351. doi: 10.1046/j.1440-1614.2001.00897.x. [DOI] [PubMed] [Google Scholar]
- 13.Daud A, af Klinteberg B, Rydelius PA. Resilience and vulnerability among refugee children of traumatized and non-traumatized parents. Child Adolesc Psychiatry Ment Health. 2008;2(1):7. doi: 10.1186/1753-2000-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Dev Psychopathol. 2001;13(3):733–753. doi: 10.1017/s0954579401003170. [DOI] [PubMed] [Google Scholar]
- 15.Li X, Huang X, Tan H, Liu A, Zhou J, Yang T. A study on the relationship between posttraumatic stress disorder in flood victim parents and children in Hunan, China. Aust N Z J Psychiatry. 2010;44(6):543–550. doi: 10.3109/00048671003601400. [DOI] [PubMed] [Google Scholar]
- 16.Yehuda R, Bierer LM. Transgenerational transmission of cortisol and PTSD risk. Prog Brain Res. 2008;167:121–135. doi: 10.1016/S0079-6123(07)67009-5. [DOI] [PubMed] [Google Scholar]
- 17.Yehuda R, Bierer LM, Schmeidler J, Aferiat DH, Breslau I, Dolan S. Low cortisol and risk for PTSD in adult offspring of holocaust survivors. American Journal of Psychiatry. 2000;157(8):1252. doi: 10.1176/appi.ajp.157.8.1252. [DOI] [PubMed] [Google Scholar]
- 18.Kroboth PD, Salek FS, Pittinger AL, Fabin TJ, Frye F. DHEA and DHEA-S: A review. Journal of Clinical Pharmacology. 1999;39:327–328. doi: 10.1177/00912709922007903. [DOI] [PubMed] [Google Scholar]
- 19.Suglia SF, Ryan L, Bellinger DC, Enlow MB, Wright RJ. Children’s exposure to violence and distress symptoms: influence of caretakers’ psychological functioning. Int J Behav Med. 2011;18(1):35–43. doi: 10.1007/s12529-010-9090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orvaschel H, Thompson WD, Belanger A, Prusoff BA, Kidd KK. Comparison of the family history method to direct interview: Factors affecting the diagnosis of depression. Journal of Affective Disorders. 1982;4(1):49–59. doi: 10.1016/0165-0327(82)90019-2. [DOI] [PubMed] [Google Scholar]
- 21.Rougemont-Buecking A, Rothen S, Jeanprêtre N, Lustenberger Y, Vandeleur CL, Ferrero F, Preisig M. Inter-informant agreement on diagnoses and prevalence estimates of anxiety disorders: Direct interview versus family history method. Psychiatry Research. 2008;157(1-3):211–223. doi: 10.1016/j.psychres.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 22.Ahmadzadeh G, Malekian A. Aggression, anxiety, and social development in adolescent children of war veterans with PTSD versus those of non-veterans. Journal of Research in Medical Sciences. 2004;9(5):231–234. [Google Scholar]
- 23.Byrne CA, Riggs DS. The cycle of trauma; relationship aggression in male Vietnam veterans with symptoms of posttraumatic stress disorder. Violence Vict. 1996;11(3):213–225. [PubMed] [Google Scholar]
- 24.Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, Weiss DS. Problems in families of male Vietnam veterans with posttraumatic stress disorder. J Consult Clin Psychol. 1992;60(6):916–926. doi: 10.1037//0022-006x.60.6.916. [DOI] [PubMed] [Google Scholar]
- 25.Roberts AL, Austin SB, Corliss HL, Vandermorris AK, Koenen KC. Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. American Journal of Public Health. 2010;100(12):2433–2441. doi: 10.2105/AJPH.2009.168971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Breslau N, Davis GC. Posttraumatic stress disorder: The etiologic specificity of wartime stressors. Am J Psychiatry. 1987;144(5):578–583. doi: 10.1176/ajp.144.5.578. [DOI] [PubMed] [Google Scholar]
- 27.Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, Seedat S. Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive Psychiatry. 2009;50(2):121–127. doi: 10.1016/j.comppsych.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 28.Kolassa IT, Ertl V, Eckart C, Glockner F, Kolassa S, Papassotiropoulos A, de Quervain DJ, Elbert T. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. The Journal of clinical psychiatry. 2010;71(5):543–547. doi: 10.4088/JCP.08m04787blu. [DOI] [PubMed] [Google Scholar]
- 29.Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- 30.Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10(3):198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- 31.Morgan CA, 3rd, Hazlett G, Wang S, Richardson EG, Jr., Schnurr P, Southwick SM. Symptoms of dissociation in humans experiencing acute, uncontrollable stress: a prospective investigation. Am J Psychiatry. 2001;158(8):1239–1247. doi: 10.1176/appi.ajp.158.8.1239. [DOI] [PubMed] [Google Scholar]
- 32.Schnurr P, Vielhauer M, Weathers F. Brief Trauma Interview. 1995 [Google Scholar]
- 33.Koss MP, Gidycz CA. Sexual experiences survey: reliability and validity. J Consult Clin Psychol. 1985;53(3):422–423. doi: 10.1037//0022-006x.53.3.422. [DOI] [PubMed] [Google Scholar]
- 34.Straus MA, Hamby SL, Boney-McCoy SUE, Sugarman DB. The Revised Conflict Tactics Scales (CTS2) Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- 35.Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 36.McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267(23):3176–3178. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- 37.Breslau N, Peterson EL, Kessler RC, Schultz LR. Short screening scale for DSM-IV posttraumatic stress disorder. Am J Psychiatry. 1999;156(6):908–911. doi: 10.1176/ajp.156.6.908. [DOI] [PubMed] [Google Scholar]
- 38.Goldman N, Cornman JC, Chang MC. Measuring subjective social status: a case study of older Taiwanese. J Cross Cult Gerontol. 2006;21(1-2):71–89. doi: 10.1007/s10823-006-9020-4. [DOI] [PubMed] [Google Scholar]
- 39.Hertzmark E, Fauntleroy J, Skinner S, Jacobson D, Spiegelman D. The SAS mediate macro. Brigham and Women’s Hospital, Channing Laboratory; Boston: 2009. [Google Scholar]
- 40.Lin DY, Fleming TR, De Gruttola V. Estimating the proportion of treatment effect explained by a surrogate marker. Stat Med. 1997;16(13):1515–1527. doi: 10.1002/(sici)1097-0258(19970715)16:13<1515::aid-sim572>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 41.Crown S, Crisp AH. A short clinical diagnostic self-rating scale for psychoneurotic patients. The Middlesex Hospital Questionnaire (M.H.Q.) Br J Psychiatry. 1966;112(490):917–923. doi: 10.1192/bjp.112.490.917. [DOI] [PubMed] [Google Scholar]
- 42.Kawachi I, Colditz GA, Ascherio A, Rimm EB, Giovannucci E, Stampfer MJ, Willett WC. Prospective study of phobic anxiety and risk of coronary heart disease in men. Circulation. 1994;89(5):1992–1997. doi: 10.1161/01.cir.89.5.1992. [DOI] [PubMed] [Google Scholar]
- 43.Zou G. A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 44.SAS Institute . SAS 9.2 for Windows. 9.2 edn SAS Institute; Cary NC: 2002. [Google Scholar]
- 45.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 46.Weissman M, Jensen P. What research suggests for depressed women with children. Journal of Clinical Psychiatry. 2002 doi: 10.4088/jcp.v63n0717. [DOI] [PubMed] [Google Scholar]
- 47.Tillfors M, Furmark T, Ekselius L, Fredrikson M. Social phobia and avoidant personality disorder as related to parental history of social anxiety: a general population study. Behaviour research and therapy. 2001;39(3):289–298. doi: 10.1016/s0005-7967(00)00003-6. [DOI] [PubMed] [Google Scholar]
- 48.Pears KC, Capaldi DM. Intergenerational transmission of abuse: a two-generational prospective study of an at-risk sample. Child Abuse & Neglect. 2001;25(11):1439–1461. doi: 10.1016/s0145-2134(01)00286-1. [DOI] [PubMed] [Google Scholar]
- 49.Riggs DS, Byrne CA, Weathers FW, Litz BT. The quality of the intimate relationships of male Vietnam veterans: problems associated with posttraumatic stress disorder. J Trauma Stress. 1998;11(1):87–101. doi: 10.1023/A:1024409200155. [DOI] [PubMed] [Google Scholar]
- 50.Roberts AL, Dohrenwend BP, Aiello A, Wright RJ, Maercker A, Galea S, Koenen KC. The stressor criterion for posttraumatic stress disorder: Does it matter? Journal of Clinical Psychiatry. 2012:73. doi: 10.4088/JCP.11m07054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- 52.Koenen KC, Moffitt TE, Poulton R, Martin J, Caspi A. Early childhood factors associated with the development of post-traumatic stress disorder: results from a longitudinal birth cohort. Psychological Medicine. 2007;37(2):181–192. doi: 10.1017/S0033291706009019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Galea S, Tracy M, Norris F, Coffey SF. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. J Trauma Stress. 2008;21(4):357–368. doi: 10.1002/jts.20355. [DOI] [PubMed] [Google Scholar]
- 54.Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- 55.Seckl JR, Meaney MJ. Glucocorticoid “programming” and PTSD risk. Ann N Y Acad Sci. 2006;1071:351–378. doi: 10.1196/annals.1364.027. [DOI] [PubMed] [Google Scholar]
- 56.Meaney MJ. Maternal care, gene expression, and the transmission of individual differences in stress reactivity across generations. Annu Rev Neurosci. 2001;24:1161–1192. doi: 10.1146/annurev.neuro.24.1.1161. [DOI] [PubMed] [Google Scholar]
- 57.Brand SR, Engel SM, Canfield RL, Yehuda R. The effect of maternal PTSD following in utero trauma exposure on behavior and temperament in the 9-month-old infant. Ann N Y Acad Sci. 2006;1071:454–458. doi: 10.1196/annals.1364.041. [DOI] [PubMed] [Google Scholar]
- 58.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- 59.Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: a follow-up study at age 17 years. Archives of General Psychiatry. 2006;63(11):1238–1245. doi: 10.1001/archpsyc.63.11.1238. [DOI] [PubMed] [Google Scholar]
- 60.Kendler KS, Gardner CO, Prescott CA. Personality and the experience of environmental adversity. Psychol Med. 2003;33(7):1193–1202. doi: 10.1017/s0033291703008298. [DOI] [PubMed] [Google Scholar]
- 61.Koenen KC, Fu QJ, Lyons MJ, Toomey R, Goldberg J, Eisen SA, True W, Tsuang M. Juvenile conduct disorder as a risk factor for trauma exposure and posttraumatic stress disorder. J Trauma Stress. 2005;18(1):23–32. doi: 10.1002/jts.20010. [DOI] [PubMed] [Google Scholar]
- 62.Sarapas C, Cai G, Bierer LM, Golier JA, Galea S, Ising M, Rein T, Schmeidler J, Muller-Myhsok B, Uhr M, et al. Genetic markers for PTSD risk and resilience among survivors of the World Trade Center attacks. Dis Markers. 2011;30(2-3):101–110. doi: 10.3233/DMA-2011-0764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Skelton K, Ressler KJ, Norrholm SD, Jovanovic T, Bradley-Davino B. PTSD and gene variants: New pathways and new thinking. Neuropharmacology. 2011 doi: 10.1016/j.neuropharm.2011.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Koenen KC, Harley R, Lyons MJ, Wolfe J, Simpson JC, Goldberg J, Eisen SA, Tsuang M. A twin registry study of familial and individual risk factors for trauma exposure and posttraumatic stress disorder. Journal of nervous and mental disease. 2002;190(4):209–218. doi: 10.1097/00005053-200204000-00001. [DOI] [PubMed] [Google Scholar]
- 65.Kremen WS, Koenen KC, Afari N, Lyons MJ. Twin studies of posttraumatic stress disorder: Differentiating vulnerability factors from sequelae. Neuropharmacology. doi: 10.1016/j.neuropharm.2011.03.012. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stein MB, Jang KL, Taylor S, Vernon PA, Livesley WJ. Genetic and Environmental Influences on Trauma Exposure and Posttraumatic Stress Disorder Symptoms: A Twin Study. Am J Psychiatry. 2002;159(10):1675–1681. doi: 10.1176/appi.ajp.159.10.1675. [DOI] [PubMed] [Google Scholar]
- 67.Afifi TO, Asmundson GJ, Taylor S, Jang KL. The role of genes and environment on trauma exposure and posttraumatic stress disorder symptoms: a review of twin studies. Clin Psychol Rev. 2010;30(1):101–112. doi: 10.1016/j.cpr.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 68.Dansby VS, Marinelli RP. Adolescent children of Vietnam combat veteran fathers: a population at risk. Journal of Adolescence. 1999;22(3):329–340. doi: 10.1006/jado.1999.0225. [DOI] [PubMed] [Google Scholar]
- 69.Parsons J, Kehle TJ, Owen SV. Incidence of behavior problems among children of vietnam war veterans. School Psychology International. 1990 [Google Scholar]