Abstract
Objective
To examine male students and their parents’ human papillomavirus (HPV) vaccine communication in relation to males’ willingness to discuss the vaccine with their healthcare provider and likelihood being vaccinated.
Participants
Dyads (n=111) of students and parents.
Methods
Participants completed a HPV vaccine survey based on the risk perception attitude framework in 2009.
Results
Male’s perceived susceptibility for HPV and self-efficacy to talk to their provider were directly related to their intention to discuss the HPV vaccine, and their intention was directly related to their likelihood of being vaccinated. Parents’ perceived self-efficacy to talk to their son and response-efficacy of the vaccine were directly related to their intention to talk to their son; however, parents’ intention was not related to the likelihood of their son being vaccinated.
Conclusions
College males may benefit from HPV vaccine educational programs that include communication skills training to discuss the HPV vaccine with their parents.
INTRODUCTION
Human papillomavirus (HPV) is a common sexually transmitted infection (STI) in the United States (U.S.).1,2 In 2009, the quadrivalent HPV vaccine was approved by the U.S. Food and Drug Administration (FDA) for use in males aged 9 through 26 years for prevention of genital warts, anal cancer and anal intraepithelial neoplasia. 3,4 In October 2011, the Advisory Committee on Immunization Practices (ACIP) recommended the routine use of the HPV vaccine in males aged 11 or 12 years, recommended vaccination of males aged 13–21 years who have not been vaccinated previously, and males aged 22-26 years may also be vaccinated.5 Furthermore, vaccinating males against HPV will indirectly assist with preventing HPV-related diseases among females. 6
HPV vaccine acceptance among males has been associated with being aware of HPV, being sexually active, having more lifetime sex partners, having a previous STI, perceiving themselves at risk for HPV, having a direct personal benefit, having peer acceptance of the vaccine, and believing that their parents, partners, or healthcare providers would encourage them to be vaccinated.7–11 HPV vaccination barriers include limited knowledge, a lack of perceived susceptibility, cost, and concern about vaccine safety. 7–11 Among parents of males, reported barriers include cost and the perception that their son would not directly benefit; however, parents were more willing to have their son receive the HPV vaccine if they perceived the HPV vaccine to be effective, and if the vaccine would benefit their son’s health and/or the health of their future spouse.11–15 To date, studies have not examined the potential for parents’ perceptions about the vaccine to influence their son’s HPV vaccination intention.
Given the limited information regarding HPV vaccine acceptance among males and parental influence on their medical decisions, we set out to understand these factors by incorporating a dyadic perspective. How perceptions of a health threat and efficacy can result from communication (e.g. message effects) or prompt communication (e.g. intention to engage in social influence) is addressed by the risk perception attitude (RPA) framework.16 The RPA is a communication theory that addresses perceived risk (susceptibility and severity) and perceived efficacy (self and response). The interdependent nature of these constructs between parents and their sons in relation to the son’s intended behavior to receive the HPV vaccine is an example of exploring the social context associated with a health behavior decision. The RPA would predict that as males perceive they are at risk for HPV and feel more efficacious, they will be more motivated to receive the HPV vaccine.
The purpose of this study was to understand how parents’ intention to talk about the HPV vaccine with their son and sons’ intention to talk to a healthcare provider are related to the likelihood that males would obtain the HPV vaccine. We developed four hypotheses: (1) Males’ perceived threat and efficacy are positively associated with intention to talk to a healthcare provider, which in turn, is positively associated with whether males are likely to receive the HPV vaccine; (2) Parents’ perceived threat and efficacy are positively associated with parents’ intention to talk to their son about the HPV vaccine, which in turn, is positively associated with whether sons are likely to receive the HPV vaccine; (3) Sons’ threat and efficacy are positively associated with parents’ intention to talk to their son about the HPV vaccine, which in turn, is positively associated with whether sons are likely to receive the HPV vaccine; and (4) Parents’ intention is positively associated with sons’ intention to talk to a healthcare provider, which in turn, is positively associated with whether sons are likely to receive the HPV vaccine.
METHODS
This study was conducted among male undergraduate students and their parents/legal guardians during spring 2009, just prior to the FDA approval of the HPV vaccine for males. The Institutional Review Board of The Ohio State University approved the protocol for this study.
Procedures
Students were recruited to complete a self-administered survey as part of a HPV vaccine research project. Announcements about the HPV vaccine survey study and about several other studies were made to students enrolled in a few introductory general education courses at a large public university located in the Midwest. The students had the option to complete a study for extra course credit. After completing the survey, participants were asked if they would be willing to send a shorter survey about the HPV vaccine to their parent/legal guardian. Students, who agreed, addressed an envelope containing a cover letter explaining the study, a survey with a subject identification number that linked to their sons’ survey, and a return stamped envelope. Research staff mailed the envelopes on the same day the student completed the survey. No compensation was offered to parents for completing the survey.
The Surveys
The surveys measured constructs of the RPA framework16 using items based on the risk behavior diagnosis scale17 and intention.18 The RPA includes constructs important to understanding HPV vaccine acceptance such as perceived susceptibility, severity, self-efficacy, response-efficacy, and intention. The survey took approximately 20 minutes for students and about 10 minutes for parents to complete. Since the surveys were completed just prior to FDA approval of the vaccine, each survey included the following message: “Currently, there is a vaccine available that prevents some types of human papillomavirus (HPV) in females. The HPV vaccine may be available for males in the near future. We are interested in what you think about HPV and the HPV vaccine should it be approved for males. Please complete the remainder of the survey as if the HPV vaccine will become available for males.”
Measures
Students and parents answered items on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree).17 Descriptive statistics and bivariate correlations are listed in Table 1.
Table 1.
Means, Standard Deviations, Frequencies, and Bivariate Correlations
| M (SD) or Frequencies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PSUS | 2.41 (.83) | -- | |||||||||||||
| 2. PSEV | 3.51 (.93) | .05 | -- | ||||||||||||
| 3. PEFF | 4.16 (.87) | .06 | .25** | -- | |||||||||||
| 4. PVREF | 3.73 (.85) | .15 | .37** | .48** | -- | ||||||||||
| 5. PINT | 4.16 (.97) | .20* | .19 | .77** | .60** | -- | |||||||||
| 6. SSUS | 2.12 (.86) | .23* | −.02 | .05 | .13 | .13 | -- | ||||||||
| 7. SSEV | 3.64 (.91) | −.01 | −.15 | −.03 | −.16 | −.08 | −.02 | -- | |||||||
| 8. SEFF | 3.00 (1.2) | −.18 | −.01 | .11 | .03 | .02 | .06 | .14 | -- | ||||||
| 9. SVREF | 3.64 (.57) | −.15 | .10 | .17 | −.01 | .15 | .07 | .05 | .07 | -- | |||||
| 10. SINT | 3.21 (1.0) | .12 | .04 | .13 | .11 | .17 | .48** | .04 | .44** | .04 | -- | ||||
| 11. SVAC | 3.08 (.73) | .07 | −.08 | .16 | .02 | .11 | .24* | .12 | .28** | .11 | .44** | -- | |||
| 12. GW | n = 96 (no); n = 14 (yes) | .02 | −.08 | −.02 | .09 | .02 | .13 | −.20* | .27** | −.16 | .27** | .12 | -- | ||
| 13. STI | n = 89 (no); n = 5 (yes) | .20 | −.03 | −.10 | −.04 | .03 | .34** | −.04 | .09 | −.09 | .21* | .20 | .34** | -- | |
| 14. RELIG | n = 50 (no); n = 61 (yes) | −.01 | .08 | −.06 | −.06 | −.20* | −.13 | .16 | .12 | −.08 | −.13 | .02 | .07 | .14 | -- |
p < .05,
p < .01
Note: Variables 1–10 are based on a 5-point scale (1 = strongly disagree to 5 = strongly agree). Variable 11 is based on a 4-point scale (1 = very unlikely to 4 = very likely). Variables 12, 13, and 14 were dichotomous (0 = no, 1 = yes). PSUS = parents’ susceptibility, PSEV = parents’ severity, PEFF = parents’ self-efficacy, PVREF = parents’ vaccine response efficacy, PINT = parents’ intention to talk to son, SSUS = sons’ susceptibility, SSEV = sons’ severity, SEFF = sons’ self-efficacy, SVREF = sons’ vaccine response efficacy, SINT = sons’ intention to talk to a healthcare practitioner, SVAC = sons’ likelihood of receiving the vaccine, GW = whether sons have heard of a shot or vaccine that prevents genital warts, STI = whether sons have heard about sexually transmitted infections from a healthcare provider, RELIG = sons’ religious membership.
Susceptibility
Parents reported the degree they perceived their son was susceptible to HPV by responding to three items (i.e. “My son is at high risk for getting HPV”) (Cronbach’s α = .84) and sons responded to similar items (Cronbach’s α = 83). Severity. Parents reported the degree they believed HPV would be a serious threat to their son’s life and health by responding to three items (i.e. “If my son were to get HPV it would be a very severe threat to his health”) (Cronbach’s α = .77) and sons responded to similar items (Cronbach’s α = .84).
Self-efficacy
Parents reported their ability to encourage their son to speak to a doctor about the HPV vaccine by responding to three items (i.e. “It would be easy for me to encourage my son to talk to his doctor about the HPV vaccine”) (Cronbach’s α =.94) and sons responded to similar items (Cronbach’s α = .94).
Vaccine response efficacy
How effective and safe parents perceived the HPV vaccine, parents responded to two items (i.e. “The HPV vaccine is an effective way to prevent my son from getting certain types of HPV”) (r =.77) and sons responded to similar items (r =.28).
Intention
Parents reported the degree they intended to encourage their son to talk to a doctor about the HPV vaccine, whereas sons reported the degree they intended to talk to a provider about the HPV vaccine. Parents responded to three items (i.e. “I intend to encourage my son to talk to his doctor about the HPV vaccine”) (Cronbach’s α = .96) and sons responded to three items (i.e. “I intend to ask my healthcare provider about the HPV vaccine if it becomes available for men”) (Cronbach’s α = .91).
Control variables
Whether sons had heard of a vaccine to prevent genital warts, whether sons were told they had a STI from a healthcare provider, and sons’ religious membership were included in the model as covariates. Sons responded to the following questions (yes/no): “Have you ever heard of a shot or vaccine to prevent genital warts?”, “Did a healthcare provider ever tell you that you had a sexually transmitted infection?”, “Do you belong to a church, synagogue, or any other religious organization?”
Student questions
Students answered questions regarding their personal history of sexual activity, HPV and HPV vaccine knowledge and beliefs, and their parental involvement in their medical decision making.
Analysis
To test the hypotheses, path analysis was used to examine an actor-partner model (APM) in Mplus 6.0.19 Path analysis refers to a statistical method that allows one to simultaneously examine the relationships between multiple independent and dependent observed variables in one model, which traditional regression analyses do not permit.20 Actor-partner path models allow one to determine the actor’s effect, also known as the effect of an individual’s independent variable on his/her own dependent variable (e.g., parents’ self-efficacy in relation to parents’ intention to talk to son about HPV).21 The actor-partner model also enables one to estimate the partner’s effect, which is the effect of an individual’s independent variable on the other person’s dependent variable (e.g., sons’ self-efficacy in relation to parents’ intention to talk to son about HPV).21
The hypothesized actor-partner model was evaluated based on Hu’s and Bentler’s guidelines of model fit.22 More specifically, model fit refers to the extent to which the hypothesized model is supported by the data set. A model was considered a reasonable approximation of the data based on the following criteria: a root mean square error of approximation (RMSEA) smaller than .06, a comparative fit index (CFI) greater than .95, and a standardized root mean square residual (SRMR) smaller than .08.
To test for mediation, Preacher and Hayes advise that paths be modeled from independent variables to dependent variables through potential intervening variables.23 Direct paths also must be modeled from the independent variables to the dependent variables. Thus, in the current study, direct and indirect paths were examined, and a bootstrapping procedure was performed to obtain 95% confidence intervals (CI) for the indirect associations.23 As a resampling method that has more power and is more robust against Type 1 error, bootstrapping draws from the same data set multiple times to estimate the confidence intervals and indirect associations. In the current study, the number of bootstrappingwas set to 5000, and indirect associations were significant when zero was not within the 95% CIs. Missing data across the main variables were minimal (5% or less), but to handle any missingness, the full information maximum likelihood was still used when examining the actor-partner path model.24
RESULTS
Males (N=181) completed the survey (total class enrollment of males was not known). Sixteen males were 27 years old or older and were excluded from the study. The remaining 165 students completed the survey and addressed an envelope to their parents. One hundred and twelve parents returned surveys, however, one parent did not complete the returned survey, for a 67.3% (111/165) parental response rate. This study is a report of the 111 dyads (Table 2). Sons’ mean age was 21.1 years, while the mean age of the parents was 51.2 years. Most (88.3%) parents were mothers and most (89.2%) parents and sons self-identified as non-Hispanic Whites, which reflects the student population at the university.
Table 2.
Demographic characteristics of male students and parents (n=111 dyads)
| STUDENT | Frequency N (%) | PARENT | Frequency N (%) |
|---|---|---|---|
| Age (years) | Age (years) | ||
| Mean | 21.1 | Mean | 51.2 |
| S.D. | 1.7 | S.D. | 4.8 |
| Range | 16–25 | Range | 40–61 |
| Ethnicity | Ethnicity | ||
| Hispanic | 7 (6.3) | Hispanic | 4 (3.6) |
| Non-Hispanic | 104 (93.7) | Non-Hispanic | 104 (93.7) |
| Race | Race | ||
| White | 99 (89.2) | White | 99 (89.2) |
| African American | 5 (4.5) | African American | 5 (4.5) |
| Asian | 1 (0.9) | Asian | 1 (0.9) |
| Other (including mixed) | 6 (5.4) | Other (including mixed) | 3 (2.7) |
| Marital Status | Gender | ||
| Single | 105 (94.6) | Female | 98 (88.3) |
| Married/Living with partner | 2 (1.8) | Male | 11 (9.9) |
| Other | 4 (3.6) | ||
| OSU student (years) | |||
| First | 9 (8.1) | ||
| Second | 15 (13.5) | ||
| Third | 29 (26.1) | ||
| Fourth | 39 (35.1) | ||
| Fifth | 19 (17.1) | ||
numbers for parents may not always equal 100% due to missing data
Among the 111 students: (1) 92 (82.9%) reported having had sexual intercourse; (2) 98 (88.3%) reported hearing about HPV prior to the survey; (3) 26 (23.4%) reported that HPV was the most common STI; (4) 5 (4.5%) expressed concern about HPV; (6) 29 (26.1%) reported that HPV was the STI causing genital warts; (7) 14 (12.6%) heard of a vaccine to prevent genital warts; and (8) 21 (18.9%) heard of a vaccine to prevent cancer. When making medical decisions, only 8 (7.2%) students reported never/rarely relying on parental input. Students reported sometimes/often/ always relying on both parents (n=78, 70.3%), only their female parent 17.1% (n=19), and only their male parent 4.5% (n=5) when making medical decisions.
In the preliminary analyses, paired-sample t-tests revealed that significant mean differences existed between parents and sons with respect to perceived susceptibility [p <.05] and self-efficacy [p < .001]. Parents reported significantly higher means compared to sons for perceived susceptibility (M=2.40, SD=.83 vs. M=2.14, SD=.87) and self-efficacy (M=4.16, SD=.87 vs. M=3.00, SD=1.16). Significant mean differences did not exist between parents (M=3.50, SD=.93) and sons (M=3.64, SD=.91) with regard to perceived severity [p = .31]. Similarly, parents (M=3.73, SD=.85) and sons (M=3.63, SD=.58) did not differ in mean vaccine response efficacy [p = .28].
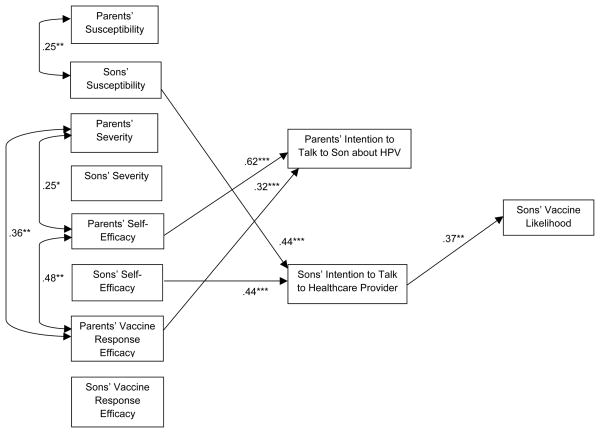
Figure 1 shows the model, which fit the data well: [χ2(6) = 7.94, p =.24; CFI = .99; RMSEA = 0.05, 90% CI = 0.00, 0.14; SRMR = 0.02]. Although all direct and indirect associations from perceived threat and efficacy to vaccine likelihood were examined during the analysis of this model, Figure 1 only shows the significant paths and correlations for visual simplicity. The model explained 71% of the variance in parents’ intention to talk to their son about the HPV vaccine, 43% of the variance in sons’ intention to talk to a healthcare provider about the HPV vaccine, and 24% of the variance in the extent to which sons would likely receive the HPV vaccine.
Figure 1.
Model with significant paths and correlations.
Note: *p < .05, **p < .01, ***p < .001. Completely standardized estimates are provided in this figure. All direct and indirect associations from perceived threat and efficacy to vaccine likelihood were examined in the analysis of this model; however, Figure 1 only shows the significant paths and correlations for visual simplicity.
The first hypothesis predicted that sons’ threat and efficacy would be positively associated with sons’ intention to talk to a healthcare provider, which in turn, would be positively associated with whether sons were likely to receive the HPV vaccine. The first hypothesis received partial support (Table 3). The results indicated that sons’ susceptibility and self-efficacy were positively related to their intention to talk to a healthcare provider. In turn, their intention was positively associated with their likelihood of obtaining the HPV vaccine. The 95% CIs provided support for these associations (Table 4). Sons’ intention to talk to a healthcare provider mediated the associations of sons’ susceptibility and self-efficacy with their likelihood of getting the HPV vaccine. Sons’ severity and vaccine response efficacy were not significantly related to sons’ intention to talk to a healthcare provider about HPV. Consistent with these findings, the 95% CIs did not provide support for the indirect associations of severity and vaccine response efficacy with their likelihood of getting the HPV vaccine.
Table 3.
Direct Associations from the model
| Direct Associations | Unstd (SE) | Std. | Direct Associations | Unstd (SE) | Std. | Direct Associations | Unstd (SE) | Std. |
|---|---|---|---|---|---|---|---|---|
| Associations with | Associations with | Associations with | ||||||
| PINT | SINT | SVAC | ||||||
| PSUS | .134 (.072) | .115 | PSUS | .080 (.116) | .065 | PSUS | .053 (.105) | .061 |
| PSEV | −.088 (.071) | −.086 | PSEV | .049 (.108) | .045 | PSEV | −.088 (.083) | −.113 |
| PEFF | .688*** (.086) | .623*** | PEFF | −.026 (.160) | −.022 | PEFF | .124 (.155) | .149 |
| PVREF | .361*** (.079) | .317*** | PVREF | −.070 (.134) | −.058 | PVREF | −.037 (.104) | −.043 |
| SSUS | −.034 (.061) | −.031 | PINT | .142 (.159) | .134 | PINT | −.037 (.140) | −.049 |
| SSEV | −.004 (.060) | −.004 | SSUS | .510*** (.079) | .440** | SSUS | .012 (.096) | .015 |
| SEFF | −.016 (.050) | −.019 | SSEV | −.013 (.087) | −.012 | SSEV | .033 (.087) | .042 |
| SVREF | .120 (.095) | .072 | SEFF | .377*** (.065) | .436*** | SEFF | .064 (.066) | .071 |
| SVREF | −.044 (.144) | −.025 | SVREF | .089 (.128) | .105 | |||
| SINT | .264**(.090 ) | .372** |
p < .05,
p < .01,
p < .001
Note: Unstd = unstandardized estimates, SE = standard error, Std = completely standardized estimates, PSUS = parents’ susceptibility, PSEV = parents’ severity, PEFF = parents’ self-efficacy, PVREF = parents’ vaccine response efficacy, PINT = parents’ intention to talk to their son, SSUS = sons’ susceptibility, SSEV = sons’ severity, SEFF = sons’ self-efficacy, SVREF = sons’ vaccine response efficacy, SINT = sons’ intention to talk to a healthcare practitioner, and SVAC = sons’ likelihood of receiving the HPV vaccine.
Table 4.
Indirect Associations Based on the Bias-Corrected Bootstrap CIs
| Parameters | Unstd. Indirect Assoc. | Unstd. 95% CI | Std. Indirect Assoc. | Std. 95% CI | Parameters | Unstd. Indirect Assoc. | Unstd. 95% CI | Std. Indirect Assoc. | Std. 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| SSUS →SINT → | .135* | .041, | .163* | .048, | PSEV →PINT → | .003 | −.019, | .004 | −.037, |
| SVAC | .250 | .278 | SVAC | .055 | .106 | ||||
| SSEV →SINT → | −.004 | −.054, | −.004 | −.063, | PEFF →PINT → | −.025 | −.228, | .083 | −.109, |
| SVAC | .046 | .054 | SVAC | .168 | .276 | ||||
| SEFF →SINT → | .100* | .033, | .162* | .052, | PVREF →PINT → | −.013 | −.121, | −.015 | −.130, |
| SVAC | .183 | .272 | SVAC | .082 | .099 | ||||
| SVREF →SINT → | −.012 | −.114, | −.001 | −.071, | PINT →SINT → | .037 | −.035, | .050 | −.071, |
| SVAC | .060 | .053 | SVAC | .156 | .171 | ||||
| PSUS →SINT → | .021 | −.036, | .024 | −.051, | PSUS →PINT → | .019 | −.013, | .015 | −.023, |
| SVAC | .105 | .099 | SINT | .090 | .054 | ||||
| PSEV →SINT → | .013 | −.039, | .017 | −.058, | PSEV →PINT → SINT | −.013 | −.082, | −.011 | −.051, |
| SVAC | .087 | .091 | .012 | .028 | |||||
| PEFF →SINT → | −.007 | −.115, | −.008 | −.113, | PEFF →PINT → | .098 | −.118, | −.030 | −.264, |
| SVAC | .075 | .097 | SINT | .340 | .204 | ||||
| PVREF →SINT → | −.018 | −.117, | −.022 | −.111, | PVREF →PINT → SINT | .051 | −.056, | .042 | −.054, |
| SVAC | .045 | .068 | .180 | .139 | |||||
| SSUS →PINT → | .001 | −.012, | .002 | −.022, | SSUS →PINT → | −.005 | −.065, | −.004 | −.029, |
| SVAC | .036 | .025 | SINT | .010 | .021 | ||||
| SSEV →PINT → | .000 | −.016, | .000 | −.021, | SSEV →PINT → SINT | −.001 | −.037, | −.000 | −.023, |
| SVAC | .024 | .021 | .021 | .022 | |||||
| SEFF →PINT → | .001 | −.010, | .001 | −.023, | SEFF →PINT → SINT | −.002 | −.044, | −.003 | −.030, |
| SVAC | .026 | .025 | .011 | .025 | |||||
| SVREF →PINT → | −.004 | −.071, | −.003 | −.037, | SVREF →PINT → SINT | .017 | −.015, | .010 | −.018, |
| SVAC | .026 | .003 | .097 | .038 | |||||
| PSUS →PINT → | −.005 | −.036, | −.006 | −.054, | |||||
| SVAC | .105 | .043 |
Note: Significant indirect associations (zero is not within the CI) are marked with an asterisk. PSUS = parents’ susceptibility, PSEV = parents’ severity, PEFF = parents’ self-efficacy, PVREF = parents’ vaccine response efficacy, PINT = parents’ intention to talk to their son, SSUS = sons’ susceptibility, SSEV = sons’ severity, SEFF = sons’ self-efficacy, SVREF = sons’ vaccine response efficacy, SINT = sons’ intention to talk to a healthcare practitioner, and SVAC = sons’ likelihood of receiving the HPV vaccine.
The second hypothesis posited that parents’ threat and efficacy would be positively associated with parents’ intention to talk to their son about the HPV vaccine, which in turn, would be positively associated with whether sons were likely to receive the HPV vaccine. The results did not support this second hypothesis. Parents’ self-efficacy and vaccine response efficacy were positively related to parents’ intention to talk to their son about HPV; however, parents’ intention was not significantly related to sons’ likelihood of receiving the HPV vaccine. Based on the 95% CIs, parents’ intention to talk to their son was not a significant mediator.
With respect to the third hypothesis, none of the sons’ threat and efficacy variables was significantly related to parents’ intention to talk to sons about the HPV vaccine. Consistent with this finding, the 95% CIs indicated that parents’ intention to talk to their son about the HPV vaccine did not significantly mediate the associations of sons’ threat and efficacy with sons’ likelihood of receiving the vaccine.
The results did not support the last hypothesis. Parents’ intention to talk to their son about the HPV vaccine was not significantly related to sons’ intention to talk to a healthcare provider about the vaccine. Similarly, the 95% CI did not provide support for the indirect association between parents’ intention and sons’ likelihood of receiving the vaccine.
COMMENT
HPV is a common STI, however, limited information is known about HPV vaccine acceptability among males and their parents. Despite the majority of male students reporting being sexually active and being aware of HPV, students had limited HPV knowledge and concern. These findings are similar to other studies of males’ awareness, knowledge, and beliefs about HPV and the HPV vaccine.7-12 Since only a small percent (7.2%) of students reported making medical decisions without/rarely relying on input from their parents, it may be important for parents to talk to their sons about HPV to increase their awareness of being at risk for HPV infection.
Overall, the results partially met our first hypothesis, which stated that males’ perceived susceptibility and self-efficacy were directly related to their intention to talk to their provider about the HPV vaccine, and their intention was directly related to the likelihood that they will receive the HPV vaccine. This finding partially supports the RPA framework because it suggests that certain types of threat and efficacy are related to intention, which in turn, is directly related to a health behavior. Students may have perceived themselves as being susceptible to HPV since most reported being sexually active and may have felt confident that they had the skill and resources needed to take care of a health problem if it occurred.
The lack of significant findings of the other hypotheses, however, may be attributed to the fact that the HPV vaccine was not approved for males at the time of this study. Males’ perceived severity and vaccine response efficacy were not significantly associated with intention, which may reflect the students’ lack of awareness about HPV-associated cancers that can occur among males and the vaccine’s effectiveness. One previous study also reported that perceived severity of HPV infection did not influence male students’ acceptability of the HPV vaccine.25 In another study, males were more willing to receive the HPV vaccine if the message framed the vaccine to prevent cancer instead of preventing genital warts.26
Parents’ self-efficacy and vaccine response efficacy were positively related to parents’ intention to talk to their son, however, parents’ intention was not significantly related to their sons’ intention to talk to a healthcare provider about the vaccine, nor was it related to their sons’ likelihood of receiving the vaccine. Again, this finding may be a reflection of the study’s timing prior to approval of the HPV vaccine for males. Although parents reported being confident in their ability to talk to their son about the HPV vaccine and believed in the vaccine’s effectiveness, parents had limited intention to discuss the vaccine with their sons because they may not have been aware of their son’s sexual activity and/or may not be aware of the HPV-related diseases that may occur among males. This finding is supported by a recent national sample of parents that found most (90%) supported the HPV vaccine for males but only 51% of parents intended to have their sons receive the HPV vaccine.15 In addition, this result is in contrast to the finding among college-age females and their mothers, where mother-daughter discussion about the HPV vaccine was an important factor in the daughter having received the HPV vaccine.27 The study among mothers and daughters, however, was conducted several years after the approval of the HPV vaccine for females and specifically measured mother-daughter talk about the HPV vaccine.
Many health decisions, such as whether to receive the HPV vaccine, are made with input from trusted individuals. The finding that the majority of males rely on their parents when making medical decisions is important for developing effective HPV vaccine messages and educational programs in the future.
Limitations
This study is not without limitations. This was a cross-sectional study and the directions of the hypothesized paths were based on the RPA framework. Future research with longitudinal data could provide further support for directionality and actual receipt of the HPV vaccine. Further, the survey was completed just prior to FDA approval of the HPV vaccine for males about two years ago. The timing of the survey may have affected the response rate from parents, and the findings about males’ awareness, knowledge, and intended communication about the HPV vaccine. The ACIP only recently recommended routine use of the HPV vaccine for males5 and previous research has reported that only a small percent of males have received the vaccine.11 It is interesting to note, that although the majority of males reported having had sexual intercourse, very few reported being concerned about HPV and being aware of a vaccine to prevent genital warts and/or cancer. In addition, this study includes a convenience sample and the dyads that agreed to participate may not reflect other male college students and parents or other populations, and thus only provides a preliminary perspective.
Conclusion
In spite of limitations, this study is unique because it addresses both male students and parents’ perceptions about the HPV vaccine. Future studies about HPV vaccine acceptability should explore the perceptions and communication of male adolescents and parents from a dyadic perspective. Although individuals over the age of 18 years may make HPV vaccination decisions, the results of this study suggest that parents continue to play a significant role in male students’ health decisions.
Acknowledgments
Funding: The authors acknowledge the following support for this study: The Ohio State University Coordinating Committee for the Population and Health: Targeted Investments in Excellence Initiative (Co-PIs: JK, AR, MLK); The National Cancer Institute K07 CA107079 (MLK) and P30 CA016058 (The Behavioral Measurement Shared Resource at The Ohio State University Comprehensive Cancer Center).
References
- 1.Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007 Feb 28;297(8):813–819. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 2.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004 Jan-Feb;36(1):6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 3.FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2010 May 28;59(20):630–632. [PubMed] [Google Scholar]
- 4.FDA. Gardasil approved to prevent anal cancer. U.S. Food and Drug Administration. [Accessed August 2011: ];News & Events. 2010 Dec 22; http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2010/ucm237941.htm.
- 5.Centers for Disease Control and Prevention. Recommendations on the use of quadrivalent human papillomavirus vaccine in males-Advisory Committee on Immunization Practices (ACIP) Morbidity and Mortality Weekly Report (MMWR) 2011;60:1705–1708. [PubMed] [Google Scholar]
- 6.Palefsky JM. Human papillomavirus-related disease in men: not just a women's issue. J Adolesc Health. 2010 Apr;46(4 Suppl):S12–19. doi: 10.1016/j.jadohealth.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liddon N, Hood J, Wynn BA, Markowitz LE. Acceptability of human papillomavirus vaccine for males: a review of the literature. J Adolesc Health. 2010;46(2):113–123. doi: 10.1016/j.jadohealth.2009.11.199. [DOI] [PubMed] [Google Scholar]
- 8.Reiter PL, Brewer NT, Smith JS. Human papillomavirus knowledge and vaccine acceptability among a national sample of heterosexual men. Sex Transm Infect. 2010;86(3):241–246. doi: 10.1136/sti.2009.039065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hernandez BY, Wilkens LR, Thompson PJ, Shvetsov YB, Goodman MT, Ning L, et al. Acceptability of prophylactic human papillomavirus vaccination among adult men. Hum Vaccin. 2010;6(6):467–475. doi: 10.4161/hv.6.6.11279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerend MA, Barley J. Human papillomavirus vaccine acceptability among young adult men. Sex Transm Dis. 2009 Jan;36(1):58–62. doi: 10.1097/OLQ.0b013e31818606fc. [DOI] [PubMed] [Google Scholar]
- 11.Reiter PL, McRee AL, Kadis JA, Brewer NT. HPV vaccine and adolescent males. Vaccine. 2011;29:5595–5602. doi: 10.1016/j.vaccine.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zimet GD, Rosenthal SL. HPV vaccine and males: issues and challenges. Gynecol Oncol. 2010;117:S26–S31. doi: 10.1016/j.ygyno.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 13.Reiter PL, McRee AL, Gottlieb SL, et al. HPV vaccine for adolescent males: acceptability to parents post-vaccine licensure. Vaccine. 2010;28(38):6292–6297. doi: 10.1016/j.vaccine.2010.06.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogilvie GS, Remple VP, Marra F, McNeil SA, Naus M, Pielak K, et al. Intention of parents to have male children vaccinated with the human papillomavirus vaccine. Sex Transm Infect. 2008;84(4):318–323. doi: 10.1136/sti.2007.029389. [DOI] [PubMed] [Google Scholar]
- 15.Dempsey AF, Butchart A, Singer D, Clark S, Davis M. Factors associated with parental intentions for male human papillomavirus vaccination: results of a national survey. Sexually Transmitted Diseases. 2011;38:769–776. doi: 10.1097/OLQ.0b013e318211c248. [DOI] [PubMed] [Google Scholar]
- 16.Rimal RN, Real K. Perceived risk and efficacy beliefs as motivators of change. Use of the risk perception attitude (RPA) framework to understand health behaviors. Human Communication Research. 2003;29:370–399. [Google Scholar]
- 17.Witte K, Cameron KA, McKeon JK, Berkowitz JM. Predicting risk behaviors: development and validation of a diagnostic scale. J Health Commun. 1996;1(4):317–341. doi: 10.1080/108107396127988. [DOI] [PubMed] [Google Scholar]
- 18.Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. Journal of Applied Social Psychology. 2002;32:665–683. [Google Scholar]
- 19.Muthen LK, Muthen BO. Mplus user's guide. 5. Los Angeles, CA: Muthen & Muthen; 2007. [Google Scholar]
- 20.Jackson JL, Dezee K, Douglas K, Shimeall W. Introduction to structural equation modeling (path analysis) 2005 Retrieved December 30, 2011 from http://sgim.org/userfiles/file/AMHandouts/AM05/handouts/PA08.pdf.
- 21.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: The Guilford Press; 2006. [Google Scholar]
- 22.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 23.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008 Aug;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 24.Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 25.Daley EM, Marhefka SL, Buhi ER, Vamos CA, Hernandez ND, Giuliano AR. Human papillomavirus vaccine intentions among men participating in a human papillomavirus natural history study versus a comparison sample. Sex Transm Dis. 2010;37:644–652. [PMC free article] [PubMed] [Google Scholar]
- 26.McRee AL, Reiter PL, Chantala K, Brewer NT. Does framing human papillomavirus vaccine as preventing cancer in men increase vaccine acceptability? Cancer Epidemiol Biomarkers Prev. 2010 Aug;19(8):1937–1944. doi: 10.1158/1055-9965.EPI-09-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krieger JL, Kam JA, Katz ML, Roberto AJ. Does mother know best? An actor-partner model of college-age females' human papillomavirus vaccination behavior. Human Communication Research. 2011;37:107–124. [Google Scholar]