Abstract
CONTEXT
The extent to which racial and ethnic differences in method choice are associated with financial barriers is unclear. Understanding these associations may provide insight into how to address racial and ethnic disparities in unintended pregnancy.
METHODS
Claims data from the California Family PACT program, which provides free family planning services to low-income residents, were used to determine the proportions of women receiving each type of contraceptive method in 2001–2007. Bivariate and multivariate analyses were performed to identify associations between women’s race and ethnicity and the primary contraceptive method they received in 2007.
RESULTS
Compared with white women, blacks and Latinas were less likely to receive oral contraceptives (odds ratios, 0.4 and 0.6, respectively) and the contraceptive ring (0.7 and 0.5), and more likely to receive the injectable (1.6 and 1.4) and the patch (1.6 and 2.3). Black women were less likely than whites to receive the IUD (0.5), but more likely to receive barrier methods and emergency contraceptive pills (2.6); associations were similar, though weaker, for Latinas. Racial and ethnic disparities in receipt of effective methods declined between 2001 and 2005, largely because receipt of the patch (which was introduced in 2002) was higher among minority than white women.
CONCLUSION
Although Family PACT eliminates financial barriers to method choice, the methods women received differed substantially by race and ethnicity in this low-income population. The reduction in racial and ethnic disparities following introduction of the patch suggests that methods with novel characteristics may increase acceptability of contraceptives among minority women.
Unintended pregnancy is a significant health problem in the United States, where more than three million such pregnancies occur each year.1 The burden of unintended pregnancy falls disproportionately on ethnic minority women—69% of pregnancies among blacks and 54% of those among Latinas are unintended, compared with 42% of those among white women.1 These disparities contribute to substantial differentials in abortion rates—49 abortions per 1,000 black women of reproductive age and 30 abortions per 1,000 Latina women of reproductive age, compared with 13 per 1,000 among whites.1 In addition, low-income women have higher rates of unintended pregnancy and abortion than do women with higher incomes; the largest differences are between women with incomes below 200% of the federal poverty level and those with incomes above this threshold.1
Disparities in unintended pregnancy and abortion rates are driven in part by differences in contraceptive use. Many women at risk for unintended pregnancy do not use a contraceptive method, and the proportion varies by race and ethnicity. The 2006–2008 National Survey of Family Growth (NSFG) found that among women who were sexually active and did not desire pregnancy, 9% of whites, 16% of blacks and 9% of Latinas were not using contraceptives.2 Disparities in use between blacks and whites at risk for unintended pregnancy persist in analyses that control for socioeconomic factors.3,4
Because contraceptive methods vary in their effectiveness, and because half of unintended pregnancies occur among women who are using contraceptives,1 differences by race and ethnicity in method choice may have an effect on racial and ethnic disparities in unintended pregnancy rates. Black and Latina women are more likely than whites to use the injectable and condoms, while whites are more likely than Blacks or Latinas to use oral contraceptives.2,5,6 In addition, Latinas are more likely than either white or black women to use an IUD.2
A few studies have investigated the relationship between contraceptive use and race and ethnicity while controlling for socioeconomic status. In one such study, black women were more likely than white women to have undergone tubal sterilization.7 In another, which controlled for education, income and insurance coverage, black women were less likely than whites to be using oral contraceptives, and more likely than whites to be using condoms and long-acting methods (the patch, ring, injectable, implant and IUD).6 In addition, U.S.-born Hispanics were more likely than white women to be using condoms, while foreign-born Hispanics were more likely than whites to be using long-acting methods. These findings indicate that racial and ethnic differences in use of oral contraceptives and condoms are not entirely due to socioeconomic factors, although conclusions cannot be drawn about the use of other individual methods.
In 1997, recognizing that financial access may influence contraceptive use, California implemented the Family PACT (Planning, Access, Care and Treatment) program, which provides free, family planning and reproductive health services to residents with incomes up to 200% of the federal poverty level who have no other source of family planning services. Program benefits include access to all contraceptive methods that have been approved by the Food and Drug Administration (FDA), as well as to screening and treatment for STDs. Family PACT serves more than 1.5 million clients per year, including approximately two-thirds of all women in California who are eligible for services, and reaches a diverse range of economically marginalized populations with poor access to health care services.8 A higher proportion of eligible Latinas (76%) than of whites (53%), Asians (49%) and blacks (43%) participate in the program.9 In 2007, Family PACT services prevented an estimated 296,200 unintended pregnancies in California.10
The availability of the program’s claims data offers a unique opportunity for researchers to analyze contraceptive method provision by clients’ race and ethnicity in a setting where women have access, without financial barriers, to all FDA-approved methods. These data have several valuable features. Because California is the most populous state and is racially and ethnically diverse,11 analyses of its population have relevance for the nation as a whole. In addition, because Family PACT covers only low-income women, the program’s data provide information about women with the greatest need for subsidized contraceptive services. Finally, claims data provide a different perspective on contraceptive provision than self-reported data, which have been the basis for most studies on the distribution of contraceptive methods.
In this article, we present characteristics of women receiving contraceptive methods in the Family PACT program in 2007 and review trends in the dispensing of contraceptives between 2001 and 2007. Examining this time period is particularly important given the arrival in 2002 of two new FDA-approved contraceptive methods: the ring and the patch. To date, information about the adoption of these methods has been limited. We will explore how contraceptive method distribution changed when these methods were introduced, as well as investigate trends by race and ethnicity in the receipt of these and other methods.
METHODS
All Family PACT providers, including clinics and pharmacies, submit claims for reimbursement to the California Department of Public Health‘s Office of Family Planning. Each client has an identification number, which enabled us to track the methods dispensed to each individual. Clients report their race and ethnicity, age and parity on the enrollment form they complete each year.
We examined paid claims data from female Family PACT clients for the years 2001–2007. Using the database of claims paid for women who had received at least one contraceptive method from the program during the year, we determined the proportion of women who received each contraceptive method in each calendar year. If a woman received multiple methods in a calendar year, only the primary (i.e., most effective) method she received was included in our analyses.* Methods were ranked from most effective to least: tubal sterilization, implant, IUD, injectable, combined hormonal methods, barrier methods and emergency contraceptive pills. Progestin-only pills were included with the combined hormonal methods, and barrier methods and emergency contraceptive pills are grouped together in our analyses. If a woman received more than one combined hormonal method in a year, she was categorized according to the method with the longest dosing interval (in declining order, the ring, the patch and the pill). All methods other than barrier methods and emergency contraceptive pills were considered highly effective.
Our data set contained information on approximately one million women in each calendar year, or more than seven million women in total. We excluded data on 310 women because of missing demographic information.
We performed bivariate analyses to determine the relationship between women’s demographic characteristics (race and ethnicity, age and parity) and their receipt of specific methods. We categorized a woman’s race and ethnicity as white, Latina, black, Asian* or other; age was classified according to the woman’s age at the midpoint of the calendar year. For our multivariate analyses, we constructed a separate logistic regression model for each method; the outcome variable in each model was receipt of the specified method. The reference group for all analyses was childless white women aged 20–29. We used STATA 9.2 for all analyses.
RESULTS
Method Provision in 2007
More than one million female Family PACT clients received a contraceptive method in 2007 (Table 1). Forty-five percent of contraceptive clients received oral contraceptives; 25% received barrier methods or emergency contraceptive pills, 14% received the injectable and 3–6% received the ring, patch or IUD. All other methods were provided to fewer than 1% of women (not shown). White women were more likely than members of other racial and ethnic groups to receive oral contraceptives (58% vs. 36–55%) and the ring (11% vs. 5–9%), but they were less likely than black women and Latinas to receive the injectable (9% vs. 16% each) and barrier methods or emergency contraceptive pills (18% vs. 28–35%). In addition, white women were the least likely to receive the patch (3% vs. 5–8%); the proportion of women receiving this method was highest among Latinas and Asian women (pairwise comparisons not shown). Women aged 30 or older were generally less likely than women in their 20s to receive the injectable, the pill or other hormonal methods, and were more likely to receive barrier methods or emergency contraceptive pills. Nulliparous women were more likely than women with one or more children to receive oral contraceptives (52% vs. 37–38%) and the ring (8% vs. 4–6%), and less likely to receive the injectable (9% vs. 17–19%) and the IUD (1% vs. 5–6%).
TABLE 1.
Number of California Family PACT clients who received a contraceptive method, and percentage distribution of these clients by primary method received, according to selected characteristics, 2007
| Characteristic | No. | Method
|
||||||
|---|---|---|---|---|---|---|---|---|
| Pill | Injectable | Ring | Patch | IUD | Barrier/ECP | Total | ||
| All | 1,046,447 | 45.1 | 13.5 | 6.4 | 6.3 | 3.0 | 25.4 | 100.0 |
| Race/ethnicity | ||||||||
| White | 243,826 | 57.6 | 9.1 | 10.6 | 3.1 | 1.7 | 17.8 | 100.0 |
| Latina | 644,263 | 39.8*** | 15.9*** | 4.5*** | 7.5*** | 3.9*** | 27.9*** | 100.0 |
| Black | 53,212 | 35.8*** | 15.5*** | 7.3*** | 4.9*** | 1.1*** | 35.2*** | 100.0 |
| Asian | 72,449 | 54.8*** | 7.0*** | 6.8*** | 7.9*** | 1.4*** | 22.1*** | 100.0 |
| Other | 32,697 | 50.3*** | 9.5* | 9.0*** | 4.6*** | 2.3*** | 24.3*** | 100.0 |
| Age | ||||||||
| 19 | 213,047 | 47.6*** | 13.3*** | 6.5*** | 5.4*** | 1.1*** | 26.1*** | 100.0 |
| 20–29 (ref) | 542,106 | 46.9 | 14.1 | 7.8 | 6.8 | 3.4 | 20.9 | 100.0 |
| 30–39 | 219,772 | 41.2*** | 13.5*** | 4.1*** | 6.8 | 4.1*** | 29.3*** | 100.0 |
| 40 | 71,522 | 35.9*** | 9.7*** | 2.1*** | 3.6*** | 2.5*** | 45.6*** | 100.0 |
| Parity | ||||||||
| 0 (ref) | 533,579 | 52.2 | 9.2 | 8.3 | 5.1 | 0.9 | 24.1 | 100.0 |
| 1 | 190,799 | 38.2*** | 18.9*** | 5.6*** | 7.7*** | 4.5*** | 24.9*** | 100.0 |
| 2 | 322,069 | 37.0*** | 17.4*** | 3.6*** | 7.4*** | 5.7*** | 27.9*** | 100.0 |
p<.05.
p<.001. Notes: Percentages may not sum to 100 because of rounding and because data on rarely used methods are not shown. ECP=emergency contraceptive pills. ref=reference group.
In multivariate analyses, race and ethnicity, age and parity were associated with the primary contraceptive method Family PACT clients received in 2007 (Table 2). The results of these analyses generally mirrored those of the bivariate analyses. Compared with white women, blacks and Latinas were less likely to receive the pill (odds ratios, 0.4 and 0.6, respectively) and the ring (0.7 and 0.5), and more likely to receive the injectable (1.6 and 1.4) and the patch (1.6 and 2.3). Black women were less likely than whites to receive an IUD (odds ratio, 0.5) but more likely to receive barrier methods or emergency contraception (2.6); similar, though weaker, associations were apparent for Latinas (0.96 and 1.9, respectively).
TABLE 2.
Odds ratios (and 95% confidence intervals) from logistic regression analyses examining associations between selected characteristics of Family PACT clients and the primary contraceptive method they received, 2007
| Characteristic | Pill | Injectable | Ring | Patch | IUD | Barrier/ECP |
|---|---|---|---|---|---|---|
| Race/ethnicity | ||||||
| White (ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Latina | 0.6 (0.6–0.6)*** | 1.4 (1.3–1.4)*** | 0.5 (0.5–0.5)*** | 2.3 (2.2–2.4)*** | 0.96 (0.92–0.99)* | 1.9 (1.9–1.9)*** |
| Black | 0.4 (0.4–0.4)*** | 1.6 (1.6–1.7)*** | 0.7 (0.7–0.7)*** | 1.6 (1.5–1.7)*** | 0.5 (0.4–0.5)*** | 2.6 (2.5–2.6)*** |
| Asian | 0.9 (0.9–0.9)*** | 0.8 (0.7–0.8)*** | 0.6 (0.6–0.6)*** | 2.7 (2.6–2.8)*** | 0.7 (0.7–0.8)*** | 1.3 (1.3–1.3)*** |
| Other | 0.8 (0.7–0.8)*** | 1.0 (0.9–1.0) | 0.8 (0.8–0.9)*** | 1.5 (1.5–1.6)*** | 1.2 (1.1–1.3)*** | 1.5 (1.4–1.5)*** |
| Age | ||||||
| 19 | 0.9 (0.8–0.9)*** | 1.4 (1.3–1.4)*** | 0.7 (0.7–0.7)*** | 0.9 (0.9–0.9)*** | 0.7 (0.7–0.8)*** | 1.2 (1.2–1.2)*** |
| 20–29 (ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 30–39 | 1.03 (1.02–1.05)*** | 0.6 (0.6–0.7)*** | 0.7 (0.7–0.7)*** | 0.8 (0.8–0.8)*** | 0.7 (0.7–0.7)*** | 1.7 (1.7–1.7)*** |
| 40 | 0.8 (0.8–0.9)*** | 0.4 (0.4–0.4)*** | 0.3 (0.3–0.4)*** | 0.4 (0.4–0.4)*** | 0.4 (0.4–0.4)*** | 3.6 (3.6–3.7)*** |
| Parity | ||||||
| 0 (ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 | 0.6 (0.6–0.6)*** | 2.4 (2.4–2.4)*** | 0.8 (0.8–0.8)*** | 1.3 (1.3–1.4)*** | 5.4 (5.2–5.6)*** | 0.9 (0.9–0.9)*** |
| 2 | 0.6 (0.6–0.6)*** | 2.7 (2.6–2.7)*** | 0.6 (0.6–0.7)*** | 1.4 (1.3–1.4)*** | 7.9 (7.6–8.2)*** | 0.8 (0.8–0.8)*** |
p<.05.
p<.001. Notes: ECP=emergency contraceptive pills. ref=reference group.
Method Provision over Time
The patch and the ring became available in 2002, and the proportion of contraceptive users receiving these methods changed markedly over time (Figure 1). Provision of the patch increased dramatically between 2002 and 2003 and peaked in 2005, at 18% of women who received a method. By 2007, however, the proportion of contraceptive users receiving the patch had declined to 6%. In contrast, the proportion using the ring increased slowly but steadily, reaching a high of 6% in 2007.
FIGURE 1. Percentage of contraceptive users receiving each method as their primary method, Family PACT, 2002–2007.
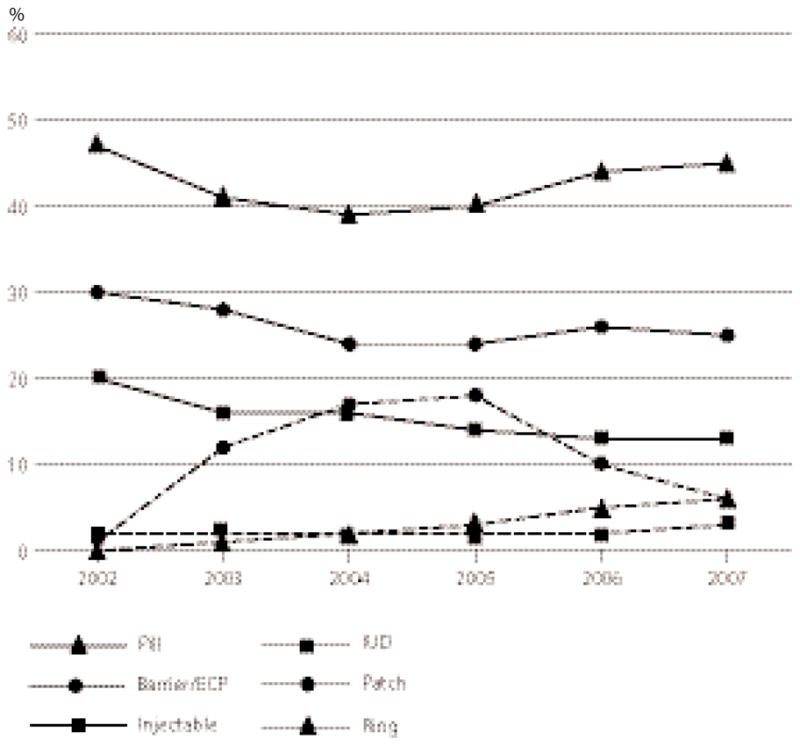
Note: ECP=emergency contraceptive pills.
During this same period, the proportion of women receiving barrier methods or emergency contraception declined from 30% to 25%, and the proportion receiving the injectable declined from 20% to 13%. While receipt of the pill declined between 2002 and 2004, it subsequently rebounded; its 2007 level (45%) nearly matched its 2002 level (47%). Receipt of an IUD increased by 50%, from 2% in 2002–2006 to 3% in 2007.
The changes in provision of the contraceptive patch over time were due largely to changes in receipt of this method by nonwhites (not shown). Receipt of the patch among Latina, black and Asian women increased between 2003 (the first year in which a substantial proportion of women used this method) and 2005, and then decreased. For example, 13% of Latinas received this method in 2003 and 22% in 2005, but only 7% did in 2007; similarly, the proportion of blacks who received this method was 12% in 2003, 15% in 2005, but only 5% in 2007. In contrast, the proportion of whites who received this method was 7–9% between 2003 and 2005), and dropped to 3% in 2007.
IUD provision also varied by race and ethnicity during the study period. In 2002, receipt of the IUD was greater among both Latinas (2.7%) and Asians (1.1%) than among whites (0.6%), and these differences held in a multivariate analysis (odds ratio, 1.5 each—not shown). By 2007, however, Latinas and Asians were less likely than whites to receive an IUD, after adjustment for age and parity (odds ratios, 0.7 and 0.96, respectively—Table 2). No substantial changes were apparent in racial and ethnic patterns of provision of the ring and the injectable.
The proportion of contraceptive users who received highly effective methods remained constant among whites (at about 81%) between 2001 and 2007 (Figure 2), but increased among blacks (from 59% to 65%) and Latinas (from 68% to 72%). Racial and ethnic disparities in the receipt of highly effective methods narrowed between 2001 and 2005, at which point 68% of blacks and 75% of Latinas were using highly effective methods, but widened slightly when provision of the contraceptive patch to Blacks and Latinas declined between 2005 and 2007.
FIGURE 2. Percentage of contraceptive users whose primary method was highly effective, by race and ethnicity, Family PACT, 2001–2007.
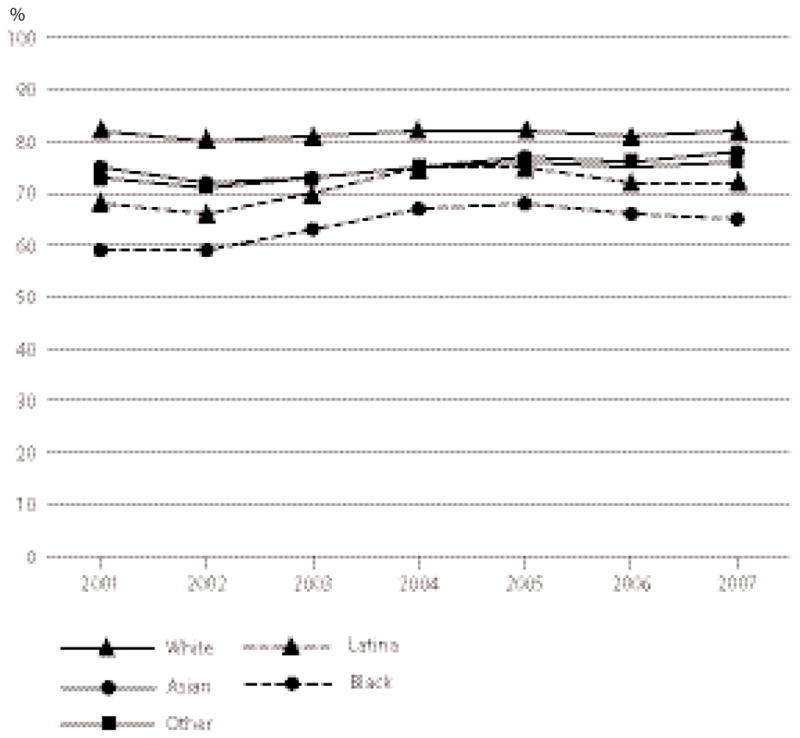
Note: Tubal sterilization, implant, IUD, injectable and combined hormonal methods were considered highly effective methods.
DISCUSSION
This analysis provides valuable information about the provision of contraceptive methods in a system where all methods are available at no charge. Our study population is limited by Family PACT policy to women with an income no higher than 200% of the federal poverty line; however, within this income range, we expand on earlier work by providing information about the association of method choice with race and ethnicity independent of financial access. In addition, our study yields information about the provision of contraceptives during a period in which new methods were introduced.
Our data show that the contraceptive methods women received differed substantially by race and ethnicity. After adjustment for age and parity, white women were more likely than Latina, black or Asian women to receive the pill, ring or IUD, while Latina and black women were more likely than whites to receive the injectable, patch or barrier methods. Although such differences most likely do not entirely explain racial and ethnic disparities in unintended pregnancy rates, our findings suggest that variations in use of highly effective methods may be one factor.
The persistence of racial and ethnic differences in methods received in a program in which all contraceptive methods are covered suggests that socioeconomic status and health care access are not the only factors that contribute to such differences. Patient preferences and knowledge may also play a role. Results of previous studies have suggested that black and Latina patients tend to have misconceptions and fears about hormonal contraceptives.12–14 These concerns may in part be a result of minority women’s having lower levels of knowledge than white women about birth control,15–17 and may be related to and reinforced by information obtained through social networks.12,18–20 In addition, these perceptions may be shaped by knowledge of the history of coercive family planning programs motivated by racist beliefs;21,22 one study found that more than one-third of black women felt that “medical and public health institutions use poor and minority people as guinea pigs to try out new birth control methods,” and 20% believed that “governmental family planning policies are designed to control the number of black people.”23
An additional potential source of racial and ethnic variation in contraceptive use is provider influence. Providers in clinics or communities serving minority women may be more likely than providers caring for white women to recommend or provide certain methods, such as the patch, although this has not been studied. Alternatively, providers may make different recommendations depending on clients’ race and ethnicity. While this possibility has not been well studied in the reproductive health field, race and ethnicity is a factor in recommendations in other areas of clinical medicine24 (the issue has been examined most fully in cardiology25,26). Moreover, in one study, providers were more likely to recommend the IUD to low-income minority women than to low-income white women.27 Although this finding differs from ours (the odds of receiving an IUD were highest among white Family PACT clients), the study suggests that patient race and ethnicity can influence provider behavior in a reproductive health context.
We found that receipt of hormonal contraceptives increased after the introduction of the patch and the ring; provision of these new methods more than offset a decline in provision of the injectable. Importantly, the increase in provision of hormonal methods, and the corresponding decrease in receipt of barrier methods, was most prominent among black and Latina clients, and was largely attributable to the increasing receipt of the patch. Together, these trends resulted in a narrowing of the gaps between provision of hormonal methods to whites and to black and Latina clients, at least between 2001 and 2005. However, these differences widened slightly after 2005, because of a decline in dispensing of the patch. This change is likely related to the FDA’s 2005 black box warning that use of this method results in higher serum levels of estrogen than does use of the pill, possibly resulting in an increased risk of venous blood clots.28 Nonetheless, our results suggest that minority women’s disinclination to use hormonal contraceptives12–14 may be overcome at least in part by the development of novel modes of drug delivery. This underscores the importance of the development of methods appropriate for women with a range of needs and preferences, and illustrates the potential for new methods to affect disparities in use.
Parity and age were also independently associated with receipt of contraceptive methods. Notably, nulliparous women were more likely than parous women to receive oral contraceptives and the ring, and women 29 or younger were more likely than older women to receive the injectable (trends by age for other methods were less clear). Reasons for these variations are unknown; future research could investigate the extent to which the disparities relate to provider or patient preference. In addition, women 40 or older were more likely than those aged 20–29 to receive barrier methods, but less likely to receive hormonal methods. This is of interest because the contraceptive use of women in their 40s has not been well studied. An analysis of NSFG data found that women in this age-group are more likely than younger women to not use any contraceptive methods.3 While our study is limited by the fact that women who had been sterilized in previous years would not be included in the Family PACT data, our findings are consistent with the NSFG analysis in suggesting that women 40 and older may have an elevated risk for unintended pregnancy because of low use of effective contraceptives.
The proportions of women receiving various contraceptive methods in 2007 are themselves of interest. Only about one-quarter of Family PACT clients who obtained a method received the injectable, ring, patch or IUD, which do not require daily administration and may be easier for women to use effectively than pills (the method received by almost half of clients). Possible reasons for the low rates of use of these methods include women’s lack of familiarity with them and concerns about side effects.29–32 In addition, many providers have misconceptions about the safety of the IUD and therefore inappropriately limit its use.33,34 Interventions designed to improve knowledge and dispel misconceptions about these methods may increase their use and ultimately help reduce the high rate of unintended pregnancy.
Data on the prevalence of IUD use since the 2000 introduction of the levonorgestrel-containing intrauterine system are limited. In our multivariate analyses, we found that in 2007, this method was more commonly provided to white women than to black or Asian women, to women aged 20–29 than to younger or older women, and to parous women than to women with children. While NSFG data regarding IUD use have not been evaluated using multivariate methods, the 2006–2008 NSFG results for age and parity appear to be consistent with our results.2
Limitations
Our data have some limitations. First, our measure of the primary method women received does not fully capture the complexity of method use within a given year. We categorized women according to the most effective method they received during the year, and did not take into account the variety of methods they may have received or the length of time that they may have used each. Furthermore, because we used claims data related to the provision of the method, our analysis provides limited insight into the use of long-term methods (such as the IUD and sterilization) that do not require one or multiple visits each year. Given that the proportion of women using these methods within the Family PACT program is small, this limitation should not have a marked impact on our findings.
Moreover, our data set included only women who accessed services through Family PACT, and not those who were eligible but did not receive methods through the program. This limitation may be especially relevant to our ability to identify women who used barrier methods or emergency contraceptive pills, as opposed to no method, because women could have bought these methods over the counter without accessing their Family PACT benefits. Some women whom we classified as nonusers, and hence excluded, may in fact have been using barrier methods, while others may have been trying to become pregnant or may not have been sexually active. However, when we included in our analyses women who had not received a method, the findings did not vary.
An additional limitation of our data set is that it does not include claims that were denied and thus never paid, even if the client received the method. Also, any fraudulent or erroneous claims that were not associated with actual provision of a method but were paid would have been included in our data set. Moreover, the data provide direct information about the methods dispensed to Family PACT clients, but not about the methods used by these clients. However, we have no reason to believe that actual use differed by method, except for the injectable, the IUD and tubal sterilization, which are provided in the health care setting.
These limitations are generally inherent to the use of claims data. As we would not expect these data quality issues to be differentially associated with use of particular methods, with specific patient demographic characteristics or with specific calendar years, they are unlikely to have altered our findings. Further, our results regarding oral contraceptives and condoms are similar to those found in a study using self-reported data.6 While the limitations of self-reported data, such as recall bias,35 differ from those of claims data, the concordance of these findings supports the validity of our results.
A final limitation to consider is the potential for residual confounding. Most notably, although the incomes of Family PACT clients do not exceed 200% of the federal poverty level, variations in socioeconomic status may exist among these individuals. We did not have access to information on other client characteristics, such as education and wealth, to control for variations in socioeconomic status within the Family PACT population.36 Therefore, some of the racial and ethnic differences we identified could be due to differences related to socioeconomic status.
Conclusion
Racial and ethnic differences in receipt of contraceptive methods may persist even when low-income women are provided with access to all methods. Further research into contraceptive methods, including alternative modes of delivery, may increase uptake of effective methods. Additional research into provider and patient factors that may influence contraceptive use, as well as choice of method, is necessary to guide efforts to reduce disparities in use of effective methods and to lower the prevalence of and disparities in unintended pregnancy.
Acknowledgments
This project was supported by NIH/NCRR/OD UCSF-CTSI grant number KL2 RR024130. The authors thank the Office of Family Planning, California Department of Health Services, for providing the claims data. All analyses, interpretation and conclusions in this article are solely the responsibility of the authors.
Footnotes
In any given year, fewer than 1 in 10 women (8%) received more than one highly effective contraceptive method (excluding condoms and emergency contraception).
This group also includes Pacific Islander women and Filipinas.
References
- 1.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38(2):90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 2.Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. Vital and Health Statistics. 2010;(29) Series 23. [PubMed] [Google Scholar]
- 3.Wu J, et al. Contraceptive nonuse among US women at risk for unplanned pregnancy. Contraception. 2008;78(4):284–289. doi: 10.1016/j.contraception.2008.04.124. [DOI] [PubMed] [Google Scholar]
- 4.Frost JJ, Singh S, Finer LB. Factors associated with contraceptive use and nonuse, United States, 2004. Perspectives on Sexual and Reproductive Health. 2007;39(2):90–99. doi: 10.1363/3909007. [DOI] [PubMed] [Google Scholar]
- 5.Mosher WD, et al. Use of contraception and use of family planning services in the United States: 1982–2002. Advance Data from Vital and Health Statistics. 2004;(350) [PubMed] [Google Scholar]
- 6.Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspectives on Sexual and Reproductive Health. 2008;40(2):94–104. doi: 10.1363/4009408. [DOI] [PubMed] [Google Scholar]
- 7.Borrero S, et al. Race, insurance status, and tubal sterilization. Obstetrics & Gynecology. 2007;109(1):94–100. doi: 10.1097/01.AOG.0000249604.78234.d3. [DOI] [PubMed] [Google Scholar]
- 8.Office of Family Planning, California Department of Public Health. [accessed Apr. 18, 2011];Fact sheet on Family PACT: an overview. 2008 < http://www.familypact.org/Files/Provider/Fact%20Sheets/FS_FamPACToverview11-08.pdf>.
- 9.Chabot MJ, Lewis C, Thiel de Bocanegra H. Access to Publicly Funded Family Planning Services in California, Fiscal Year 2006–07. Sacramento: University of California, San Francisco; 2010. [Google Scholar]
- 10.Foster DG, et al. Estimating the fertility effect of expansions of publicly-funded family planning services in California. Women’s Health Issues. 2011 doi: 10.1016/j.whi.2011.05.008. forthcoming. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Census Bureau. [accessed Apr. 18, 2011];State and county QuickFacts: California. 2010 < http://quickfacts.census.gov/qfd/states/06000.html>.
- 12.Gilliam ML, et al. Concerns about contraceptive side effects among young Latinas: a focus-group approach. Contraception. 2004;70(4):299–305. doi: 10.1016/j.contraception.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 13.Clark LR, et al. Menstrual irregularity from hormonal contraception: a cause of reproductive health concerns in minority adolescent young women. Contraception. 2006;74(3):214–219. doi: 10.1016/j.contraception.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 14.Gilliam ML, et al. Contraceptive attitudes among inner-city African American female adolescents: barriers to effective hormonal contraceptive use. Journal of Pediatric and Adolescent Gynecology. 2009;22(2):97–104. doi: 10.1016/j.jpag.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Baldwin SB, et al. Who is using emergency contraception? Awareness and use of emergency contraception among California women and teens. Women’s Health Issues. 2008;18(5):360–368. doi: 10.1016/j.whi.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Sangi-Haghpeykar H, et al. Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception. 2006;74(2):125–132. doi: 10.1016/j.contraception.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Borrero S, et al. Racial variation in tubal sterilization rates: role of patient-level factors. Fertility and Sterility. 2011;95(1):17–22. doi: 10.1016/j.fertnstert.2010.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuiper H, et al. Urban adolescent females’ views on the implant and contraceptive decision-making: a double paradox. Family Planning Perspectives. 1997;29(4):167–172. [PubMed] [Google Scholar]
- 19.Guendelman S, et al. Perceptions of hormonal contraceptive safety and side effects among low-income Latina and non-Latina women. Maternal and Child Health Journal. 2000;4(4):233–239. doi: 10.1023/a:1026643621387. [DOI] [PubMed] [Google Scholar]
- 20.Yee L, Simon M. The role of the social network in contraceptive decision-making among young, African American and Latina women. Journal of Adolescent Health. 2010;47(4):374–380. doi: 10.1016/j.jadohealth.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts D. Black women and the pill. Family Planning Perspectives. 2000;32(2):92–93. [PubMed] [Google Scholar]
- 22.Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. American Journal of Public Health. 2005;95(7):1128–1138. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thorburn S, Bogart LM. Conspiracy beliefs about birth control: barriers to pregnancy prevention among African Americans of reproductive age. Health Education & Behavior. 2005;32(4):474–487. 478. doi: 10.1177/1090198105276220. [DOI] [PubMed] [Google Scholar]
- 24.van Ryn M, Fu SS. Paved with good intentions: Do public health and human service providers contribute to racial/ethnic disparities in health? American Journal of Public Health. 2003;93(2):248–255. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hannan EL, et al. Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Medical Care. 1999;37(1):68–77. doi: 10.1097/00005650-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Schulman KA, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. New England Journal of Medicine. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 27.Dehlendorf C, et al. Recommendations for intrauterine contraception: a randomized trial of the effects of patients’ race/ethnicity and socioeconomic status. American Journal of Obstetrics & Gynecology. 2010;203(4):319.e1–e8. doi: 10.1016/j.ajog.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.U.S. Food and Drug Administration (FDA) FDA updates labeling for Ortho Evra contraceptive patch, news release. Silver Spring, MD: FDA; Nov 10, 2005. [Google Scholar]
- 29.Whitaker AK, et al. Adolescent and young adult women’s knowledge of and attitudes toward the intrauterine device. Contraception. 2008;78(3):211–217. doi: 10.1016/j.contraception.2008.04.119. [DOI] [PubMed] [Google Scholar]
- 30.Fleming KL, Sokoloff A, Raine TR. Attitudes and beliefs about the intrauterine device among teenagers and young women. Contraception. 2010;82(2):178–182. doi: 10.1016/j.contraception.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raine TR, et al. Attitudes toward the vaginal ring and transdermal patch among adolescents and young women. Journal of Adolescent Health. 2009;45(3):262–267. doi: 10.1016/j.jadohealth.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Terrell LR, et al. Acceptability of the vaginal contraceptive ring among adolescent women. Journal of Pediatric and Adolescent Gynecology. 2011;24(4):204–210. doi: 10.1016/j.jpag.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Dehlendorf C, et al. Health care providers’ knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81(4):292–298. doi: 10.1016/j.contraception.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harper CC, et al. Challenges in translating evidence to practice: the provision of intrauterine contraception. Obstetrics & Gynecology. 2008;111(6):1359–1369. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 35.Evans C, Crawford B. Patient self-reports in pharmacoeconomic studies: their use and impact on study validity. Pharmacoeconomics. 1999;15(3):241–256. doi: 10.2165/00019053-199915030-00004. [DOI] [PubMed] [Google Scholar]
- 36.Braveman PA, et al. Socioeconomic status in health research: One size does not fit all. Journal of the American Medical Association. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]


