Abstract
Background
Oxandrolone, an anabolic agent, has been administered for 1 year post burn with beneficial effects in pediatric patients. However, the long-lasting effects of this treatment have not been studied. This single-center prospective trial determined the long-term effects of 1 year of oxandrolone administration in severely burned children; assessments were continued for up to 4 years post-therapy.
Study Design
Patients 0–18 years old with burns covering >30% of the total body surface area were randomized to receive placebo (n=152) or oxandrolone, 0.1 mg/kg twice daily for 12 months (n=70). At hospital discharge, patients were randomized to a 12 week exercise program or to standard of care. Resting energy expenditure (REE), standing height, weight, lean body mass, muscle strength, bone mineral content (BMC), cardiac work, rate pressure product (RPP), sexual maturation, and concentrations of serum inflammatory cytokines, hormones, and liver enzymes were monitored.
Results
Oxandrolone significantly decreased REE, RPP, and increased IGF-1 secretion during the first year after burn injury, and in combination with exercise significantly increased lean body mass and muscle strength. Oxandrolone-treated children exhibited improved height percentile and BMC content compared to controls. The maximal effect of oxandrolone was found in children aged 7–18 years. No deleterious side effects were attributed to long-term administration.
Conclusions
Administration of oxandrolone improves the long-term recovery of severely burned children in height, BMC, cardiac work and muscle strength; the increase in BMC is likely to occur by means of IGF 1. These benefits persist for up to 5 years post burn.
Keywords: Burn, oxandrolone, children, height, bone mineral content, hypermetabolic response, hypercatabolic response, resting energy expenditure
INTRODUCTION
Burn injury induces a hypermetabolic response that is characterized by elevations in cardiac work, metabolic rate, and muscle catabolism. Increased protein breakdown coupled with inadequate protein synthesis leads to muscle weakness and a loss of lean body mass (LBM). [1] Post-burn catabolic effects are not limited to muscle, as bone mineral content (BMC) and fat mass are decreased as well. This hypermetabolic response persists for up to 2 years after burn injury, greatly reducing the quality of life of severely burned patients. [2]
Oxandrolone, a synthetic oral non-aromatizable testosterone derivative, has only 5% of the virilizing activity and lower hepatotoxicity when compared to testosterone. Following administration, oxandrolone reaches peak serum concentrations within one hour and is excreted through the urine. Oxandrolone binds to androgen receptors in the skeletal muscle to initiate protein synthesis and anabolism. Because oxandrolone cannot be aromatized to estrogen, the likelihood of estrogen-dependent bone age advancement is reduced, making oxandrolone a safe therapeutic approach for growing children. [3–5]
In children with Turner’s syndrome and other growth-related conditions, oxandrolone has been successfully for many decades to safely treat growth delays. [6–10] More recently, oxandrolone has been used to induce anabolism in patients experiencing muscle wasting associated with AIDS, major surgery, infections, malnutrition, neuromuscular disorders, or thermal injury. [11–12] Oxandrolone is the only androgenic steroid approved by the Food and Drug Administration to maintain body weight in these catabolic states. [3] These studies have demonstrated that oxandrolone has an excellent safety profile and is well tolerated by patients.
We have previously shown in severely burned children that short-term administration of oxandrolone during the acute phase of burn injury increases net muscle protein balance, maintains LBM, and shortens intensive care unit (ICU) stay. [1,13–15] Additionally, short term oxandrolone use was associated with elevation of liver enzymes aspartate aminotransrferase (AST) and alanine aminotransferase (ALT) from 17 – 40 days post burn.[13] Amino acid utilization was improved for up to 6 months post-burn in patients randomized to oxandrolone treatment.[16] In a small group of severely burned children, the administration of oxandrolone for 1 year post-burn increased LBM, BMC, muscle strength, heights, and weights. These benefits lasted for at least a full year after discontinuation of oxandrolone. [17–18] The addition of a 12-week exercise program to 1 year of oxandrolone therapy provided an even greater increase in weight and LBM. [19]
We conducted a single-center prospective randomized controlled trial in massively burned pediatric patients to investigate the effects of oxandrolone administration for 1 year post burn on growth, body composition, muscle strength, REE, liver and cardiac function, serum markers, hormones, bone mass, and sexual maturation. We present the data from this trial, including data gathered up to 5 years post-burn to determine the safety and efficacy of the drug. A subset of these patients also underwent a 12-week exercise program to determine if exercise, in combination with oxandrolone, further affects LBM and BMC. These data are presented as well.
METHODS
Patients
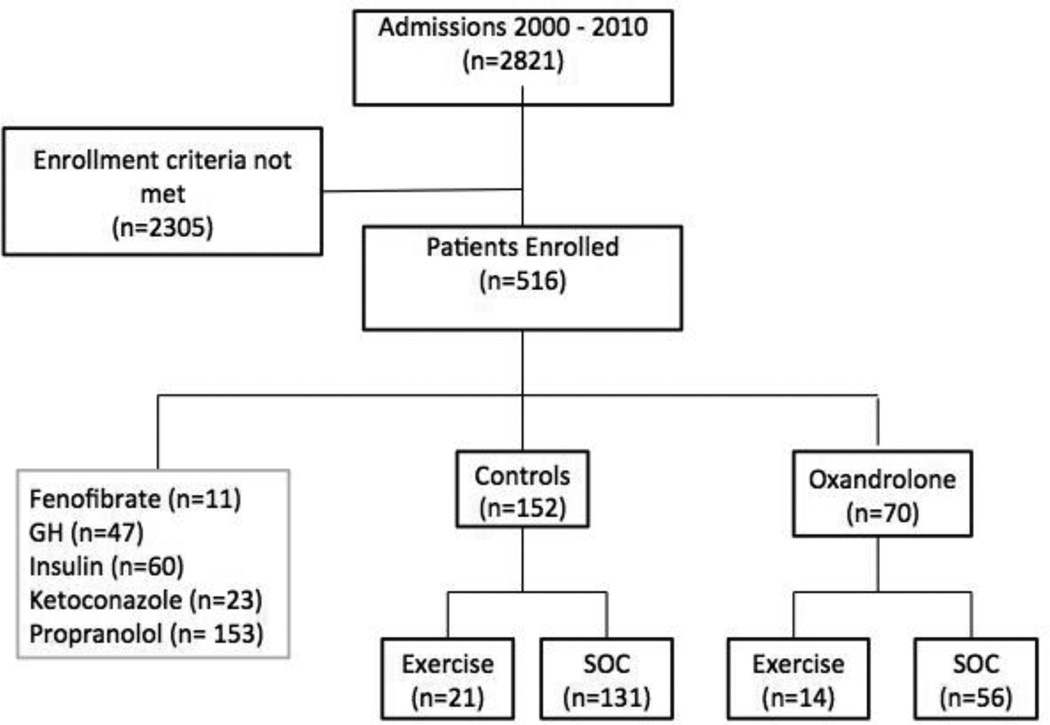
Two thousand eight-hundred twenty one severely burned children were admitted to our institution from 2000 to 2010. Of these, 516 patients with burns over 30% of the total body surface area (TBSA) were consented and randomized to studies of various anabolic agents administered acutely and long-term post injury. Seventy patients were randomized to receive oxandrolone, 152 to the control group, and 294 to other ongoing studies (Figure 1). Control patients outnumbered oxandrolone-treated patients due to the balanced design of the randomization schedule, in order to share control subjects with all studies in a time contiguous fashion.
FIGURE 1.
Consort diagram.
Patients 0–18 years of age at the time of the burn, with >30% of TBSA burned, and the need for at least one surgical intervention were included in the study. Exclusion criteria were the decision not to treat due to severity of the burn injury; anoxic brain injury; the presence of preexisting conditions such as HIV, AIDS, hepatitis, 5 year history of malignancy, or diabetes; and an inability to obtain informed consent. The administration of oxandrolone was started within 48 hours after the first operation and given orally at a dose of 0.1 mg/kg twice a day for one full year (BTG Pharmaceuticals, Iselin, NJ). Four Patients over 50 kg received 5 mg twice daily. Patients were assessed at admission; during acute hospitalization; at discharge; at 6, 9, 12, 18, and 24 months after burn; and annually thereafter. Patients who withdrew from the study were included in the data analysis up to the time of the withdrawal. This study was part of a large clinical trial (www.clinicaltrials.gov, NCT00675714) evaluating the outcomes of burn survivors after administration of therapeutic agents such as oxandrolone, propranolol, insulin, and the combination of oxandrolone and propranolol. Informed written consent approved by the Institutional Review Board of The University of Texas Medical Branch (Galveston, TX) was obtained from a legal guardian before enrollment in the study. Children older than 7 years assented to participate. This study adhered to ethical standards set forth by the Declaration of Helsinki (1975, revised 1983–2008).
Nutritional Support
Patients were resuscitated at admission according to the Galveston formula (a total of 5,000 ml/m2 TBSA burned + 2, 000 ml/m2 TBSA lactated Ringer’s solution given during the first 24 hours). Within 48 hours of admission, all patients underwent burn wound excision and autograft / allograft application. After excision and grafting procedures, patients remained on bed rest for 3 days and then ambulated daily thereafter until the next procedure. Sequential staged excision and grafting were performed until the wounds healed.
Each patient received Vivonex TEN® enteral nutrition composed of 82% carbohydrate, 15% protein, and 6% fat, by nasoduodenal tube. During the first week of hospitalization, intake was calculated to deliver 1,500 kcal/m2 TBSA + 1,500 kcal/m2 TBSA burned. The dietary replacement was then modified after the first week of treatment to 1.4 times the resting energy expenditure (REE) (see Indirect Calorimetry below). Caloric intakes remained constant throughout hospitalization. Albumin, pre-albumin, and retinol-binding protein served as indicators of nutritional status during the acute hospitalization period. Parents received nutritional counseling from the hospital nutritionist prior to discharge. In the outpatient setting, the patient’s caretakers were interviewed regarding intake every day when the patient returned to the tub room, weekly while the patient remained in apartments and residencies in the hospital vicinity, and during each long term follow-up visit. After discharge from the ICU, patients received the commercial formula Boost® (Nestle Health Care Nutrition, Nestlé S.A., Vevey, Switzerland), which is composed of 41 grams of carbohydrate, 10 grams of protein, and 4 grams of fat, three times per day. Supplementation continued until the nutritionist confirmed that the regular diet met the patient’s caloric requirements.
Patient Demographics and Injury Characteristics
Patient age, sex, and injury characteristics including the size and depth of the burn were recorded at the time of admission. Age-appropriate diagrams were used to determine burn size. [20] Conditions such as inhalation injury, sepsis, morbidity, and mortality were also recorded during the acute hospitalization. Inhalation injury was diagnosed by confirmation of the presence of soot, charring, mucosal necrosis, airway edema, or inflammation during fiber optic bronchoscopy, which was performed on all patients 24 hours after admission. Chest scintiphotograms, estimation of extra vascular lung water, and measurements of serum carboxyhemoglobin were also used for diagnostic purposes.
Indirect Calorimetry
All patients underwent weekly REE measurements during their acute hospitalization using the Sensor-Medics Vmax 29 metabolic cart (Yorba Linda, CA). Studies were performed while the patients were asleep between midnight and 5 AM. Inspired and expired gas compositions were sampled and analyzed at 60-second intervals. Values for carbon dioxide production and oxygen volume consumption were recorded when they were at a steady state for 5 min. Measured values were compared with predicted normal values based on the Harris-Benedict equation and body mass index (BMI). [21–23]
Anthropometric Measures
Measurements of height and body weight were obtained at admission, throughout the acute stay, and at all follow-up visits out to 5 years post injury. A standard calibrated scale was used to measure body weight. A wall-mounted stadiometer was used to measure height to the nearest 0.1 cm. Height and weight percentiles were calculated using growth charts specific for age and sex (obtained from the Centers for Disease Control and Prevention or National Center for Health Statistics, respectively). [24] Percent change in height- or weight- for-age percentiles was used to compare and interpret the results.
In order to eliminate seasonal differences in growth between children, height and weight velocities were calculated as whole year increments. Percentiles for those individual increments were obtained for age to determine whether the growth rate was within normal ranges. Maximal yearly height gains were used to determine annual height velocity for each patient, which were then plotted on standard and gender-specific growth velocity charts [25] at 1, 2, 3, 4, and 5 years post burn. In addition, the percentages of patients with growth velocities more than two standard deviations (SDs) below the mean (<3rd percentile) were determined at each time point.
Body Composition
Dual energy x-ray absorptiometry (DEXA) was used to measure whole body fat, LBM, BMC, and bone mineral density (BMD) (QDR-4500W Hologic, Waltham, MA). Calibration was performed daily using a spinal phantom in the lateral, anteroposterior, and single beam modes. A tissue bar phantom was used to calibrate individual pixels to accurately identify air, lean mass, bone, or fat. [26]
Measurement of Hormones, Proteins, and Cytokines
Blood and urine were collected from each patient for analysis of hormone, protein, liver enzyme, and cytokine levels at admission; during the acute stay; at discharge; and at follow-up appointments. Blood was collected in serum-separator collection tubes and centrifuged for 10 minutes at 1,320 rpm. The serum was removed and stored at −80°C until assayed. IGF-I, IGFBP-3, testosterone, parathyroid hormone (PTH), osteocalcin, albumin, and total protein were determined using HPLC and ELISA as previously published. [27–29] The Bio-Plex Human Cytokine 17-Plex panel was used with the Bio-Plex Suspension Array System (Bio-Rad, Hercules, CA) to profile expression of the following seventeen inflammatory mediators: IL-1β, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-12, IL-13, IL-17, granulocyte colony-stimulating factor, granulocyte-macrophage colony stimulating factor, interferon-γ, monocyte chemoattractant protein-1, macrophage inflammatory protein-1β, and tumor necrosis factor. The manufacturer's protocol was followed as previously published. [27–29] Catecholamines were measured as previously published. [27–29]
Cardiac and Liver Measures
Heart rate (HR), stroke volume (SV), cardiac index (CI), mean arterial pressure (MAP), and cardiac output (CO) were determined for each patient. Cardiac and liver ultrasound measurements were made with a HP SONOS 100 CF echocardiogram (Hewlett Packard Imaging System, Andover, MA) equipped with a 3.5-MHz transducer. M-mode tracings were obtained at the level of the tips of the mitral leaflets in the parasternal long axis position, and measurements were performed according to the American Society of Echocardiography recommendations. Stroke volume and CO were calculated using left ventricular end-systolic and end-diastolic volumes measures. Rate pressure product (RPP) was obtained as a correlate of the myocardial oxygen consumption by multiplying Mean Arterial Pressure (MAP) × HR. The MAP was obtained by continuous arterial monitoring during the ICU stay, and RPP was calculated during the long term period using blood pressure measurements obtained at each follow up visit. The liver was scanned using an Eskoline B-scanner, a modified HP diagnostic sounder 7214A, and a modified 3.5-MHz transducer probe. Liver size and weight were calculated using a previously published formula. [30] Measurements were performed during the acute stay and at follow-up time points.
Rehabilitation Program
Because we have previously shown that completion of an exercise program improves LBM, muscle strength, and cardiovascular function, patients aged 7–18 years were also randomized to receive the standard of care (SOC) or to participate in an exercise program within 6 months of discharge per our published protocol. [31] The SOC consisted of a home based physical and occupational therapy instructions without exercise. The exercise program consisted of 12 weeks of in-hospital, supervised, and individualized aerobic and resistance exercise training carried out five days a week in addition to standard occupational and physical therapy regimens. Aerobic conditioning exercises were performed on a treadmill or cycle ergometer five times a week. A standardized treadmill exercise test was conducted using the modified Bruce protocol to assess cardiovascular fitness and peak aerobic endurance time. Patients exercised at 70% to 80% of their previously determined peak aerobic capacity (VO2 peak). Patients also performed resistance exercises such as bench press, leg press, and leg curls three times a week. Strength assessments were performed using the Biodex System 3 dynamometer (Biodex Medical Systems, Shirley, NY) according to instructions provided by the manufacturer. Peak torque values were calculated with the Biodex software system and were corrected for gravitational movements of the lower leg and the lever arm.
Additional Measurements
At each follow-up time point, X-rays of the patient’s hand and knee were obtained for bone age assessments and monitoring of the closure of the epiphyseal plate. In addition, psychosocial function was assessed at each follow-up time point. Patients participated in a structured clinical interview and were administered several self-report inventories.
Statistical Analysis
The distribution of the data was evaluated using QQ plots and the Kolmogorov-Smirnov normality test. Normally distributed data are presented as the mean ± standard deviation (SD) or standard error of the mean (SEM). Non-normally distributed data (i.e., cytokines) are presented as the median ± median absolute deviation (median±MAD). Frequency data are expressed as counts or percentages. We did not control for differences between the groups in sex, age, or weight, except in the case of muscle strength, which is corrected for body weight. Two-sided equal-variance t-tests were used to compare normally distributed continuous data. All trends in the data were calculated using the loess smoother. [32] Standard errors were calculated using the loess functionality in R. To test for differences between the curves, we calculated and tested the maximum t-statistic using the permutation distribution. [33] A step-down procedure was used to adjust the family-wise error rate. [34] Two-sided Wilcoxon exact tests were used for non-normally distributed. Repeated measures Friedman’s test was used to determine differences between intervals; if a difference were detected, a post hoc pairwise multiple comparisons (Dunn’s) test was also performed. SAS (version 9.2) was used for data analysis and hypothesis testing. Fisher’s exact test was used for frequency data. P values less than 0.05 were considered significant.
RESULTS
Patient Disposition and Demographics
Of the 222 patients enrolled in this study, 29 were lost to follow-up (control, n=20; oxandrolone, n=9), and 39 withdrew from study participation (control, n=28; oxandrolone, n=11). Demographics did not differ significantly between the oxandrolone and control groups (Table 1). Two-thirds of the patients were male, which is typical of burn injury in children. Almost half of the patients in each group were diagnosed with inhalation injuries. The length of hospital stay was approximately a half day per percent TBSA burned for patients in both groups. Mortality was low in both groups. No differences were noted in the number or time between operations when comparing the oxandrolone and control groups. Thirty-five patients participated in a 12-week exercise program during the rehabilitation period (control, n=21; oxandrolone, n=14), and 187 patients received SOC (controls n=131; oxandrolone n=56).
TABLE 1.
Patient Demographics
| Variable | Control (n=152) |
Oxandrolone (n=70) |
p Value |
|---|---|---|---|
| Age, y* | 8±5 | 8±5 | 0.68 |
| Male, n (%) | 99 (65%) | 45 (63) | 0.80 |
| Hispanics, n (%) | 133 (88) | 63 (89) | 0.52 |
| % TBSA Burned* | 57±15 | 54±15 | 0.11 |
| Inhalation injury, n (%) | 54 (50) | 22 (42) | 0.33 |
| Length of stay in ICU, d* | 30±35 | 24±16 | 0.19 |
| Length of stay per % burn* | 0.5±0.8 | 0.4±0.2 | 0.28 |
| Operations— acute, n* | 4.0±2.8 | 3.6±2.2 | 0.18 |
| Time between operations, d* | 6.6±3.5 | 6.4±2.4 | 0.27 |
| Operations— long term, n* | 5.9±4.6 | 4.3±3.3 | 0.21 |
| Mortality, n (%) | 13 (9) | 3 (4) | 0.24 |
Data are expressed as mean ± SEM.
TBSA, total body surface area.
Indirect Calorimetry
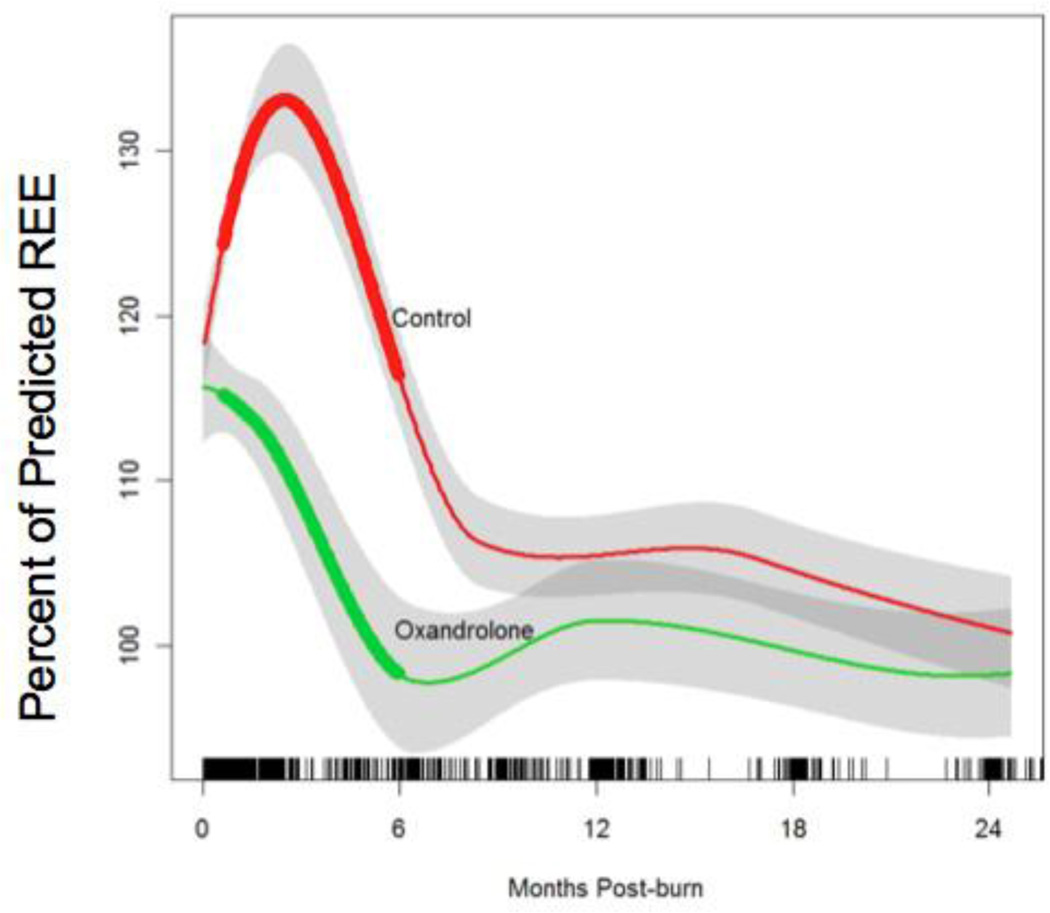
Oxandrolone significantly decreased percent of predicted REE (P<0.01), and this effect was sustained until approximately 6 months post burn, indicating that hypermetabolism was significantly decreased. Although REE decreased over time in both groups, these values remained elevated for over 12 months after burn in the control group (Figure 2).
FIGURE 2.
Effect of oxandrolone on percent predicted resting energy expenditure. Data are represented the loess-smoothed trend in resting energy expenditure (REE) with shading indicating +/− standard error. Hatch marks across the bottom represent the density of sampled data at each time point (1,427 total observations). Time points at which differences are significant are indicated with wider lines (p<0.004).
Anthropometric Measures
In the control group, the percentage of children below two standard deviations (SDs) of the mean for height velocity was 48% at 1 year post burn; 32% at 2 years post burn; and ~20% at 3, 4, and 5 years post burn (Table 2). In the oxandrolone group, the percentage of patients falling more than two SDs below the mean for height velocity was only 8% at 1 year post burn and 7% at 2 years post burn. These values were significantly lower than those in controls (Table 2); however, this difference was not significant at 3, 4, or 5 years post burn.
TABLE 2.
Growth Distribution at Admission and 1–5 Years Post Burn
| Variable | Admission, % | Post burn year, % |
||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| >2 SDs below mean height velocity | ||||||
| Control | 20 | 48* | 32* | 18 | 22 | 27 |
| Oxandrolone | 20 | 8† | 7† | 16 | 15 | 9 |
| >2 SDs below mean weight velocity | ||||||
| Control | 4 | 46* | 26* | 19* | 18* | 21* |
| Oxandrolone | 7 | 28*† | 25* | 21 | 20 | 19 |
p<0.05 vs. admission.
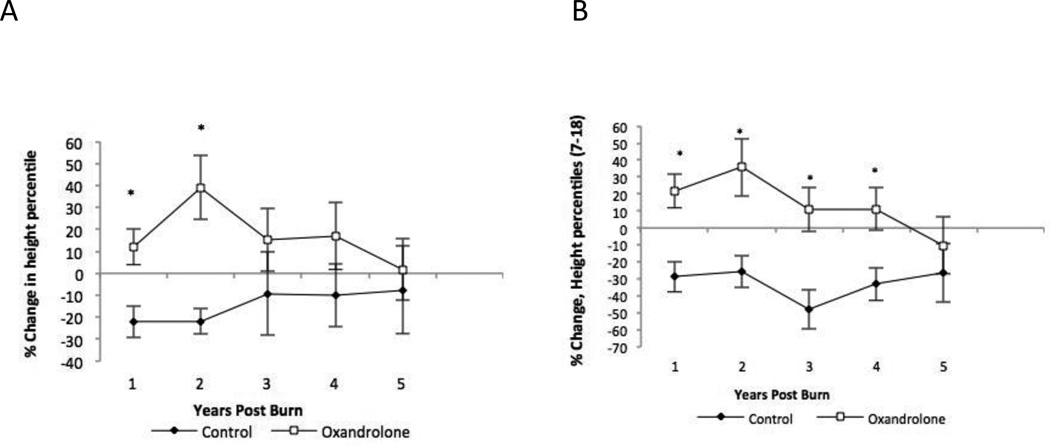
p<0.05 vs. control.
Patients in the oxandrolone group exhibited a positive percent change in height percentiles at 1 year post burn, with a maximal change of ~40% seen at the second year (Figure 3A). These changes were significantly higher than those seen in controls at corresponding time points. In contrast to oxandrolone-treated patients, controls exhibited a negative percent change in height percentiles that was maximal at 1 and 2 years post burn, and these values remained negative at all time points. No significant differences were detected between groups at 3, 4 and 5 years post burn. As shown in Figure 3B, the effect of oxandrolone was maximal in children between the ages of 7 and 18 years, and the percent change in height percentile was significantly different up to 4 years post burn (P<0.05). Controls, on the other hand, showed a loss in height percentile over time.
FIGURE 3.
Percent change in height percentile from 1 to 5 years post burn in (A) all patients and in (B) patients aged 7–18 years. Data are expressed as mean ± SEM. *p<0.05 vs control.
An analysis of the percentage of children with weight velocities more than two SDs below the mean revealed that this percentage was lower in the oxandrolone group than in the control group at 1 year post burn, but not at 2, 3, 4, or 5 years post burn (Table 2).
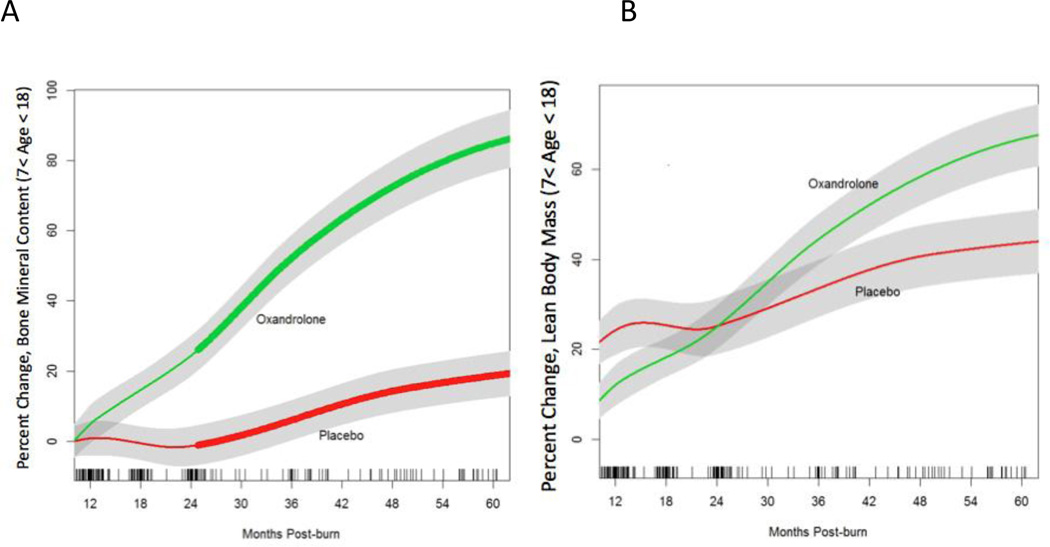
Body Composition
Oxandrolone-treated patients who were 7–18 years old at the time of the injury had a significantly higher percent change in BMC than their control counterparts, beginning 2 years after injury and lasting until 5 years post burn (P<0.001) (Figure 4). No significant differences were detected between groups for children less than 7 years of age. Significant differences in BMC were also seen between children who received oxandrolone and participated in the exercise program and exercising control patients (P<0.01). BMD did not significantly differ between oxandrolone-treated patients and controls, regardless of age (data not shown). LBM approached significance at all time points (P=0.06). However, significance was reached only in exercising, oxandrolone-treated children, with differences between this group and exercising control patients at 2 years post burn, remaining significant throughout the remainder of the study period (P=0.01) (Figure 5B). No significant correlation was detected between percent change in LBM and percent change in BMC at any time post burn.
FIGURE 4.
Percent change in (A) total body bone mineral content and (B) lean body mass. Data are represented as the loess-smoothed trend in BMC and in LBM with shading indicating +/− standard error. Hatch marks across the bottom represent the density of the sampled data at each time point (572 total observations). Time points at which differences are significant are indicated with wider lines (p<0.001).
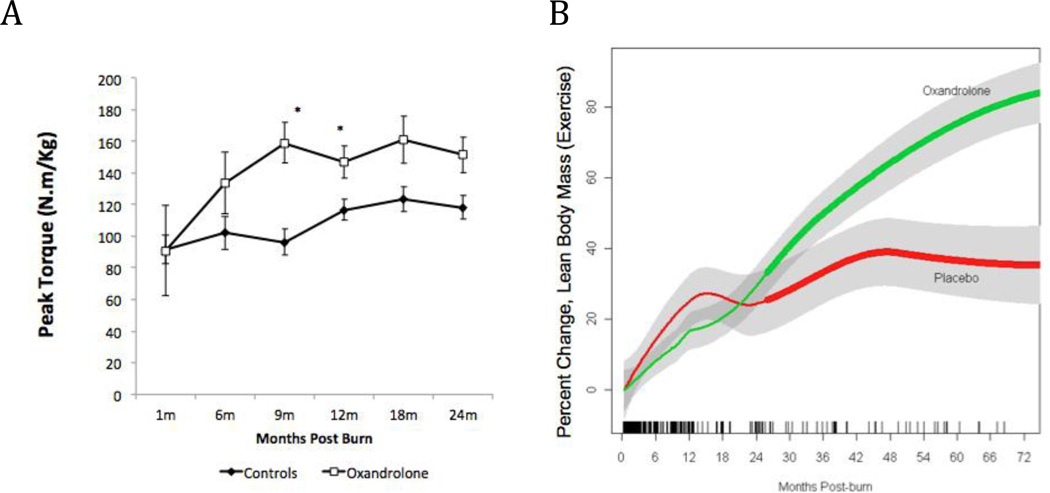
FIGURE 5. Exercise.
Combined effect of oxandrolone and exercise on percent change in (A) total lean body mass and (B) muscle strength. In (A), data are represented by the loess-smoothed trend in LBM with shading indicating +/− standard error. Hatch marks across the bottom represent the density of the sampled data at each time point (279 total observations). Time points at which differences are significant are indicated with wider lines (p<0.05). In (B), data are expressed as mean ± SEM. *p<0.05 vs control.
Hormones, Proteins, and Cytokines
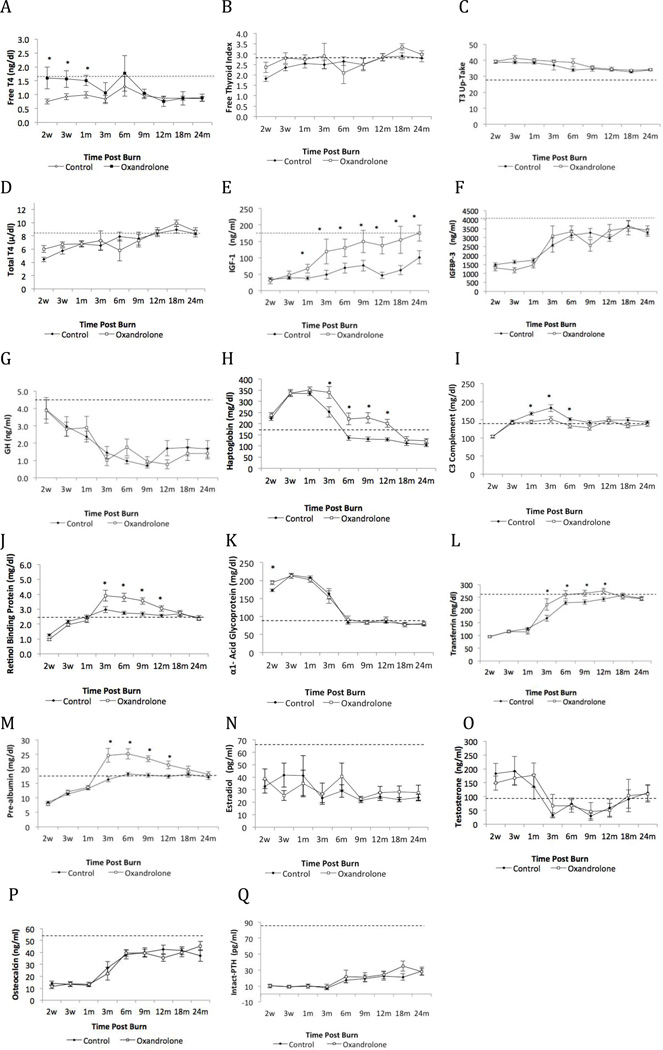
Although catecholamines were elevated by burn injury, there were no differences between the groups. Serum constitutive proteins, pre-albumin, retinol-binding protein, and transferrin were significantly higher in oxandrolone-treated patients than controls from 2 to 12 months after burn injury (Figure 6 J, L, M). Serum albumin and total protein remained within normal limits and were not significantly different between groups (Figure 7D, H). Acute-phase proteins were significantly elevated in both groups during acute hospitalization (Figure 6). Complement C3 was markedly increased in the control group when compared to the oxandrolone group from discharge until 6 months post burn. Haptoglobin levels were significantly elevated in both groups until 6 months post burn, with oxandrolone-treated patients showing significant differences for 1 year following discharge when compared to controls. No differences were detected between the groups in α-2 macroglobulin and free fatty acid levels. In both groups, levels of C-reactive protein and α-1 acid glycoprotein returned to normal levels by 6 months after burn injury.
FIGURE 6.
Effect of oxandrolone on serum levels of (A) free T4, (B) free thyroid index, (C) T3 uptake, (D) total T4, (E) IGF-1, (F) IGFBP-3, (G) growth hormone, (H) haptoglobin, (I) C3 complement, (J) retinol-binding protein, (K) α1 acid glycoprotein, (L) transferrin, (M) pre-albumin, (N) estradiol, (O) testosterone, (P) osteocalcin, and (Q) intact parathyroid hormone. Data are expressed as mean±SEM. *p<0.05 vs control, w: week, m: month.
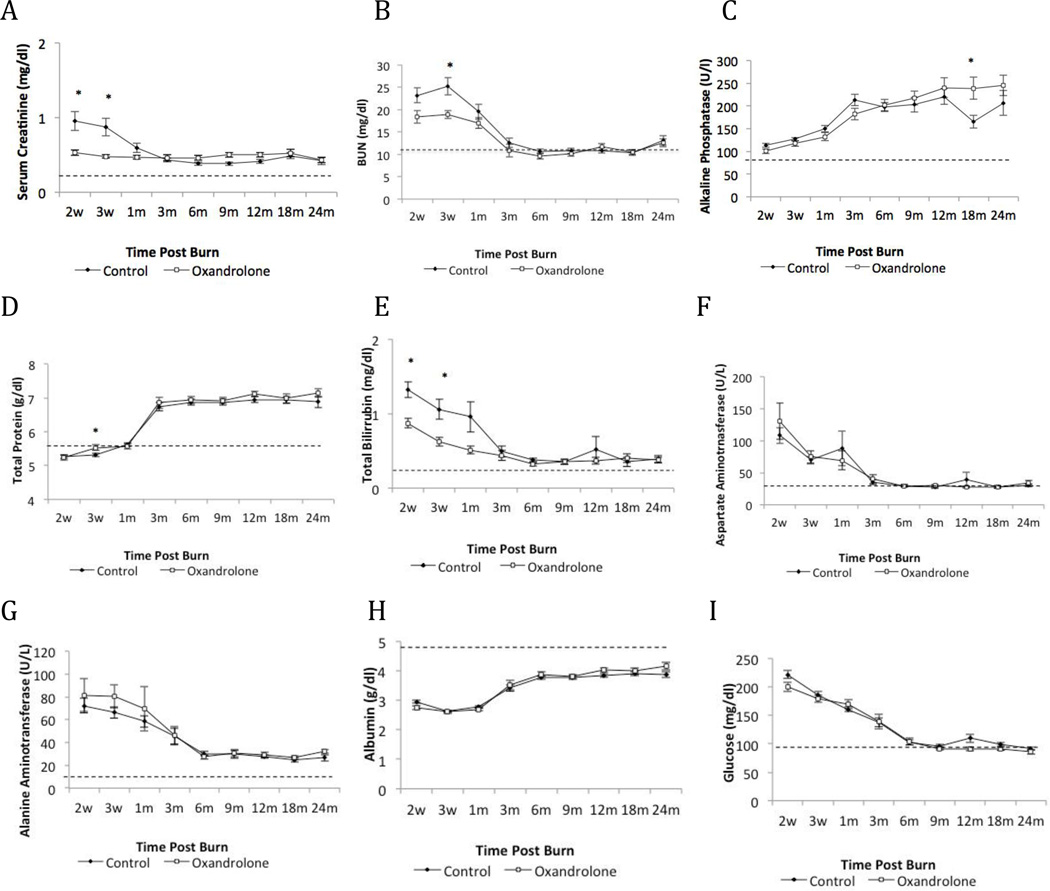
FIGURE 7.
Effect of oxandrolone on levels of (A) serum creatinine, (B) BUN, (C) alkaline phosphatase, (D) total protein, (E) total bilirubin, (F) aspartate aminotransferase, (G) alanine aminotransferase, (H) albumin, and (I) glucose. Data are expressed as mean±SEM. *p<0.05 vs control, w: week, m: month.
Confirming previous studies [2, 13, 35], IGF-1, IGFBP-3, testosterone, growth hormone, β-estradiol, and total T4 levels were decreased after injury (Figure 6). Oxandrolone induced significant positive and persistent up-regulation of IGF-1 (Figure 6E); IGF-I was significantly higher in the oxandrolone group than the control group from discharge to 2 years post burn, with no differences in IGFBP-3 between the groups (Figure 6F). Exercise did not alter IGF-1 levels. Serum i-PTH and osteocalcin levels were dramatically decreased in both groups compared to normal values for over 2 years post burn and did not significantly differ between the groups (Figure 6P, Q). Free thyroid index and T3 uptake remained constant over time and did not differ between the groups (Figure 6B, C). Free T4 was significantly higher during the acute period in the oxandrolone group, although free T4 levels fell within normal range. Progesterone was consistently elevated in both groups but was not significantly different between them. All blood chemistry values were within normal limits, and no differences between the groups were detected. As in previous studies, [2, 36] glucose and insulin levels were above normal limits during acute hospitalization in both groups, with no significant differences detected between oxandrolone-treated and controls.
At most, serum cytokine levels significantly differed between the two groups at one or two time points after burn injury. These alterations were not sustained; therefore the overall inflammatory response did not differ between the groups.
Cardiac and Liver Changes
Absolute and percent of predicted CO, SV, and HR as well as CI and RPP were assessed up to 2 years following burn injury (Table 3). At 1 year post burn, CO, percent of predicted CO, and percent of predicted HR were significantly lower in the oxandrolone group compared to the control group (P<0.05). A significant decrease in RPP was observed in the oxandrolone group up to 1 year post burn (p<0.05). At 2 years post burn, percent of predicted CO and HR were significantly lower in the oxandrolone group than in the control group (P<0.05 for both). Liver length and weight were not significantly different between the control and oxandrolone groups (Table 3).
TABLE 3.
Cardiac and Liver Ultrasound Measurements
| Variable | Control (n=152) | Oxandrolone (n=70) | ||||
|---|---|---|---|---|---|---|
| Discharge | 1 year | 2 years | Discharge | 1 year | 2 years | |
| CO (L/min) | 5.1±0.3 | 4.9±0.3 | 4.4±0.3 | 5.2±0.4 | 4.0±0.3* | 3.9±0.3 |
| % Predicted CO | 150.7±7.4 | 148.1±7.2 | 128.6±9.2 | 145.6±14.6 | 115.5±12.4* | 98.3±10.9* |
| CI (L/min/m2) | 5.6±0.4 | 8.9±3.0 | 9.8±4.9 | 6.0±0.7 | 4.6±0.5 | 3.9±0.5 |
| SV (mL/m2) | 38.2±2.5 | 47.4±3.0 | 43.7±3.0 | 40.1±3.1 | 41.9±4.7 | 43.3±4.1 |
| % Predicted SV | 100.5±5.7 | 121.2±5.4 | 108.5±6.9 | 92.8±10.4 | 103.7±9.2 | 87.5±8.7 |
| HR (beats/min) | 140.4±2.5 | 111.3±3.6 | 109.5±5.1 | 133.6±3.9 | 105.2±5.5 | 94.8±4.7* |
| % Predicted HR | 155.8±3.7 | 123.1±3.4 | 121.2±4.8 | 155.1±5.0 | 110.1±4.4† | 109.5±4.3* |
| Liver size (cm) | 12.2±0.4 | 11.6±0.4 | 11.4±0.4 | 12.6±0.4 | 11.5±0.6 | 12.4±0.5 |
| Liver weight (g) | 3346.8±292.3 | 3018.5±329.1 | 2432.2±302.1 | 3457.9±329.5 | 2899.2±481.2 | 3311.8±416.8 |
Data are expressed as mean±SEM.
p<0.05 vs control.
HR, heart rate; SV, stroke volume; CI, cardiac Index; CO, cardiac output.
Rehabilitation Program
Significant increases in LBM, BMC, and muscle strength were seen in the oxandrolone + exercise group when compared to the control + exercise, control + SOC, or the oxandrolone + SOC groups. These effects persisted for up to 5 years post burn (Figure 5). Muscle strength, expressed as peak torque/kg body weight, was significantly greater in the oxandrolone + exercise group than the control + exercise group, the control + SOC group, or the oxandrolone + SOC group (P<0.05) at 9, 12, 18, and 24 months post burn. No significant difference in muscle strength was detected between oxandrolone + SOC and control + SOC.
Safety Profile
Our patients were closely monitored for adverse events for up to 1 year after discontinuation of oxandrolone. Thereafter, patients were assessed during annual follow-up visits. No signs of virilization were noted. Three female patients who had perineal burns developed clitoral hood edema, which resolved within 3 months. Chi-Square analyses revealed that oxandrolone did not affect acute and long-term psychosocial outcomes, including the prevalence of post-traumatic stress disorder, general anxiety, and depression between groups. Monitoring of liver and renal function included measures of serum creatinine, BUN, total protein, liver enzymes, total bilirubin, liver size, and liver weight (Table 3) (Figure 7). Alanine aminotransaminase and gamma glutamyl transpeptidase were elevated during the acute period in the control and oxandrolone groups, returning to normal levels 3 to 6 months post burn. However, levels of constitutive proteins were significantly increased in the oxandrolone group, indicating that liver function was not affected. The control group showed significantly higher levels of serum creatinine, total bilirubin, and BUN during the acute period than the oxandrolone group. Although these values were statistically significant, some fell within normal ranges. Alkaline phosphatase and total protein tended to increase with time in both groups and were not different between the groups. The rest of the parameters did not differ between the groups at any of the time points. There was no significant advancement in bone age versus chronological age over the post burn observation period, and no difference between oxandrolone-treated patients (0.93±0.16) and controls (0.94±0.24) was detected.
DISCUSSION
Advances in burn care over the past several decades have dramatically decreased mortality, [37] leading to multiple challenges in long-term care of the burned victim, ranging from wound healing and hypertrophic scarring to physical disabilities and psychosocial difficulties. Burns covering over 30% TBSA are associated with a continuous hypermetabolic response that lasts for 2 years following the initial insult. [2, 21–22, 35] This was confirmed by our study, in which the control group showed a dramatic increase in REE during the convalescent period that remained above normal levels for as long as 18 months after burn. The present study revealed clear differences in the percent of predicted REE between oxandrolone and control patients up to 6 months after burn injury, indicating a sustained attenuation of the hypermetabolic state by oxandrolone. In this study, we have demonstrated that this prolonged attenuation of the hypermetabolic response is accompanied by long-term improvements in total body BMC and increased height velocity in massively burned children.
Severe burn is associated with marked retardation of linear growth and abnormal bone loss in the pediatric population. [38–39] Since the beginning of the 1960s, oxandrolone has been safely administered to pediatric patients with growth retardation. In 1965, a randomized controlled trial conducted by Ray and colleagues revealed that children with Down’s syndrome exhibited significant improvements in height after oxandrolone treatment for 1 and 2 years at a dose of 0.5 and 0.25 mg/kg respectively. [7, 9] In 1965, Danowski reported that administration of 10–40 mg oxandrolone for 13–37 months induced a two-fold acceleration in height in children 3–17 years old who were below the third percentile for height. [6, 10] The use of oxandrolone in patients with Turner’s syndrome as an adjunctive therapy to prevent constitutional growth delay has been well described. A randomized, double blind, placebo-controlled trial following a large cohort of girls with Turner’s syndrome receiving growth hormone over a 10-year period showed that 0.05 mg/kg/day oxandrolone improved final height in these individuals. [8]
In this study, we were interested in examining the patients with growth arrest, as seen by height velocities below normal limits. Our data showed that a much larger percentage of patients with significant growth arrest were present in the control group than in the oxandrolone group (48 vs. 8%, P<0.01), similar results were found at the second year post burn (32 vs. 7%) (P<0.05).
We have previously shown that oxandrolone significantly improved growth in severely burned children after 1 year of treatment, with this increase maintained a full year after discontinuation of therapy. [18] This finding is supported by the current study, which revealed that oxandrolone-treated patients went from their baseline height percentile to higher ones, while control patients exhibited a loss in height percentile. This was more pronounced in children who were 7–18 years of age at the time of the burn injury, with oxandrolone-treated children in this age range having a significantly increased percent change in height percentiles for up to 4 years post burn. Importantly, these increases in height were associated with improvements in BMC, as assessed by DEXA. This study was not powered to determine ultimate height in these severely burned children. Therefore, a larger study in a larger group of individuals to look at ultimate stature is necessary.
Bone loss occurs quickly following a severe burn, as manifested by an approximate 2% loss of total body BMC by 2 months post burn, increasing to about 3.5% by 6 months, with lumbar spine BMC falling about 8% and remaining low for up to 24 months post burn. [39] The recovery of bone from the catabolic effects of burn injury occurs relatively slowly. In previous studies of small groups of children, we have shown that a significant increase in BMC occurs at 12 months post burn. [17–18] Our study extends these observations by showing that oxandrolone continues to increase BMC for up to 5 years. In this study, we have provided evidence of a gradual increment in bone mass that reaches and remains significant after 2 years post injury. We speculate that this long-term increase in BMC results from the significant increase in IGF-1 levels as well as the protective effect of oxandrolone during the first year after burn, where ongoing stress and inflammation results in increased endogenous glucocorticoid production, abnormal calcium metabolism, and resorptive cytokine stimulation. The normal circulating levels of the chief binding protein for IGF-1, IGFBP3, could suggest an increase in IGFBP5, the main binding protein that transports IGF-1 to bone. [40] Interestingly, this effect is most pronounced in patients who were 7–18 years old at the time of the burn. This 2-year peak in BMC and height seen in oxandrolone-treated patients represents the beginning of the pre-pubertal growth spurt. The temporal aspect of changes in height percentiles seen here suggests that oxandrolone stimulates rather than impairs epiphyseal cartilage proliferation, possibly triggering ossification at these sites. In vitro, oxandrolone can up regulate the androgen receptor and concomitantly stimulate human osteoblasts to produce a significant but modest increase in type I collagen, alkaline phosphatase, and osteocalcin. These data suggest that there may be a weak direct effect of oxandrolone on osteoblasts. [41] However, burn victims have little to no osteoblastic activity from 14 days post burn to 1 year post burn. [42–44] As previously reported, oxandrolone had little to no effect on BMD. [17] However, the addition of exercise to oxandrolone therapy led to a significant increase in BMC concomitantly with an increase in LBM. This finding, as well as the finding that oxandrolone stimulates IGF-1, suggests that an increase in LBM brought about by oxandrolone and exercise could increase skeletal loading and in this particular setting, further increasing bone formation and BMC.
Severe burns accelerate catabolism of skeletal muscle. Previous studies have clearly shown that short-term oxandrolone treatment during the acute phase significantly increases LBM and net balance of muscle protein. [1, 13–15] Oxandrolone appears to achieve these effects by enhancing the efficiency of muscle protein synthesis. [1, 15] In previous studies, we have shown an improved net deposition of leg muscle protein through increased amino acid utilization after 6 months of oxandrolone treatment, [16] and significant improvement in LBM after 1 year of oxandrolone treatment.[17–18] Here, we found only a trend (P<0.06) toward improved LBM throughout the time studied.
The combination of a 12-week exercise program with oxandrolone therapy increased LBM to levels above that seen with oxandrolone therapy alone. Significant effects on muscle strength (measured by peak torque) were recorded only in the oxandrolone and exercise group. These results agree with our previous finding that combining exercise with oxandrolone produces more significant effects on LBM and weight gain. [19] The current findings are notable in that they show that the benefits of exercise are maintained for years after burn injury. In contrast, exercise seems to have little or no effect in BMC. This in agreement with a previous study where we evaluated the long-term effect of growth hormone, and found no effect in BMC in patients who participated in a similar exercise program. [45]
Oxandrolone and exercise probably affect body composition through different mechanisms. As already mentioned, oxandrolone likely increases total body BMC through IGF-1. However, the failure of oxandrolone and exercise to increase IGF-1 to significantly greater levels than oxandrolone alone suggests that the exercise effect is not mediated by IGF-1. The increase in LBM with exercise and oxandrolone suggests that the increase in BMC is secondary to increased skeletal loading, an effect different from that of IGF-1.
Assessment of cardiac function revealed that the oxandrolone group exhibited significant decreases in CO, percent predicted CO, percent predicted HR, and RPP at 1 year post burn as well as significant decreases in percent predicted CO and HR at 2 years post burn compared with the control group. These findings provide new evidence in favor of a more efficient utilization of energy by the myocardium of patients who received oxandrolone. Interestingly, these findings coincide with the increases seen in height and BMC during the same time period, suggesting that an attenuation of the hypermetabolic response occurred in oxandrolone-treated patients while the controls remained hypermetabolic. Considering the marked contributions by the heart to the overall daily energy expenditure, we speculate that the effect exerted by oxandrolone on cardiac physiology could explain the decrease in percent predicted REE as measured by indirect calorimetry. Additional studies are needed to further elucidate the mechanism by which oxandrolone decreases REE.
Special attention has been given to sex as a predictor of outcome following injury. Controversies have arisen regarding whether administration of androgens or estrogens can positively impact outcomes. Differential effects of sex hormones on immunity, organ function, and cellular response have been reported and continue to be extensively investigated. [46–50] We found that the effect of oxandrolone on height velocity was the same in females and in the overall group. The positive effect in girls persists alongside that seen in boys.
Assessment of safety showed that there were no long-lasting deleterious effects associated with oxandrolone use in our patients. Three female patients with perineal burns developed clitoral hood edema, and this condition was resolved within 3 months of discontinuation of treatment. Although we previously reported an elevation of AST and ALT between 17 and 40 days post burn in patients treated with oxandrolone, here we show that there are no long-term elevations in these markers. Bone age was not affected; premature closure of the epiphyses was not found. Anxiety, pain and mood disorders were not different between the groups. Taken together, this data indicate that oxandrolone can be safely used in severely burned children.
In conclusion, our findings provide strong evidence that oxandrolone is efficacious in attenuating the hypermetabolism elicited by burn injury, significantly improving the long-term recovery of severely burned children in height, bone mineral content, and muscle strength. This, taken with the safety profile of this drug, supports the use of oxandrolone as an adjunct therapy to the current standard of burn care.
ACKNOWLEDGMENT
The authors thank Eva Diaz MD, Laura Rosenberg PhD, Marta Rosenberg PhD, Ted Huang MD, Rene Przkora MD PhD, Elisabet Børsheim, PhD, Sandeep Ramawat, and Spogmai Komak MD for their significant contributions in collecting, analyzing, and interpreting the data, as well as their contributions toward the production of this manuscript. We also thank Deborah Benjamin, Wes Benjamin, Maria Cantu, Mario Celis, Tabatha Elliot, Kathryn Epperson, Ashley Harris, Samir Hasan, Eric Henry, Holly Goode, Kara Hougen, Joanna Huddleston, Mary Kelly, Xuyang Liang, Maria Magno, Liz Montemayor, Marc Nicolai, Sylvia Ojeda, Maricela Pantoja, Cathy Reed, Lisa Richardson, Lucile Robles, Pam Stevens, Sierra Tinney, Judith Underbrink, Becky Whitlock, the nutrition department, and the respiratory therapy team for their assistance in obtaining the study measurements. We extend a special acknowledgement to Hal Hawkins, MD for his advice regarding data safety. Finally, we also thank Kasie Cole-Edwards for editing and proofreading the manuscript.
This study was supported by grants from the National Institute for Disabilities and Rehabilitation Research (H133A070026 and H133A70019), the National Institutes of Health (P50-GM60338, R01-HD049471, R01-GM56687-11S1, and T32-GM8256), and Shriners Hospitals for Children (84080, 84309, 8510, 8740, 8741, 8660, 9145, 8760, 71009, and 71008). CCF is an ITS Career Development Scholar supported, in part, by NIH KL2RR029875 and NIH UL1RR029876. This study is registered at clinicaltrials.gov, NCT00675714.
ABBREVIATIONS
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- AIDS
acquired immune deficiency syndrome
- BMC
bone mineral content
- BMD
bone mineral density
- CI
cardiac index
- CO
cardiac output
- DEXA
dual energy x-ray absorptiometry
- HR
heart rate
- LBM
Lean body mass
- MAP
mean arterial pressure
- PTH
parathyroid hormone
- REE
resting energy expenditure
- RPP
rate pressure product
- SD
standard deviation
- SEM
standard error of the mean
- SOC
standard of care
- SV
stroke volume
- TBSA
total body surface area
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure information: Nothing to disclose.
Presented at the Southern Surgical Association 123rd Annual Meeting, Hot Springs, VA, December 2011.
REFERENCES
- 1.Hart DW, Wolf SE, Ramzy PI, et al. Anabolic effects of oxandrolone after severe burn. Ann Surg. 2001;233:556–564. doi: 10.1097/00000658-200104000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jeschke MG, Gauglitz GG, Kulp GA, et al. Long-term persistance of the pathophysiologic response to severe burn injury. PLoS One. 2011;6:e21245. doi: 10.1371/journal.pone.0021245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orr R, Fiatarone Singh M. The anabolic androgenic steroid oxandrolone in the treatment of wasting and catabolic disorders: Review of efficacy and safety. Drugs. 2004;64:725–750. doi: 10.2165/00003495-200464070-00004. [DOI] [PubMed] [Google Scholar]
- 4.Gullett NP, Hebbar G, Ziegler TR. Update on clinical trials of growth factors and anabolic steroids in cachexia and wasting. Am J Clin Nutr. 2010;91:1143S–1147S. doi: 10.3945/ajcn.2010.28608E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varness T, Seffrood EE, Connor EL, et al. Oxandrolone improves height velocity and bmi in patients with cystic fibrosis. Int J Pediatr Endocrinol. 2009;2009:826895. doi: 10.1155/2009/826895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Danowski TS, Lee FA, Cohn RE, et al. Oxandrolone therapy of growth retardation. Am J Dis Child. 1965;109:526–532. doi: 10.1001/archpedi.1965.02090020528006. [DOI] [PubMed] [Google Scholar]
- 7.Gault EJ, Perry RJ, Cole TJ, et al. Effect of oxandrolone and timing of pubertal induction on final height in turner's syndrome: Randomised, double blind, placebo controlled trial. BMJ. 2011;342:d1980. doi: 10.1136/bmj.d1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ray CG, Kirschvink JF, Waxman SH, Kelley VC. Studies of anabolic steroids. Ii. The effect of oxandrolone on height and skeletal maturation in mongoloid children (a preliminary report) Am J Dis Child. 1963;106:375–380. [PubMed] [Google Scholar]
- 9.Ray CG, Kirschvink JF, Waxman SH, Kelley VC. Studies of anabolic steroids. 3. The effect of oxandrolone on height and skeletal maturation in mongoloid children. Am J Dis Child. 1965;110:618–623. doi: 10.1001/archpedi.1965.02090030646005. [DOI] [PubMed] [Google Scholar]
- 10.Zangeneh F, Steiner MM. Oxandrolone therapy in growth retardation of children. Am J Dis Child. 1967;113:234–241. doi: 10.1001/archpedi.1967.02090170098010. [DOI] [PubMed] [Google Scholar]
- 11.Berger JR, Pall L, Hall CD, et al. Oxandrolone in aids-wasting myopathy. AIDS. 1996;10:1657–1662. doi: 10.1097/00002030-199612000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Demling RH, DeSanti L. Oxandrolone, an anabolic steroid, significantly increases the rate of weight gain in the recovery phase after major burns. J Trauma. 1997;43:47–51. doi: 10.1097/00005373-199707000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Jeschke MG, Finnerty CC, Suman OE, et al. The effect of oxandrolone on the endocrinologic, inflammatory, and hypermetabolic responses during the acute phase postburn. Ann Surg. 2007;246:351–360. doi: 10.1097/SLA.0b013e318146980e. discussion 360–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheffield-Moore M, Urban RJ, Wolf SE, et al. Short-term oxandrolone administration stimulates net muscle protein synthesis in young men. J Clin Endocrinol Metab. 1999;84:2705–2711. doi: 10.1210/jcem.84.8.5923. [DOI] [PubMed] [Google Scholar]
- 15.Wolf SE, Thomas SJ, Dasu MR, et al. Improved net protein balance, lean mass, and gene expression changes with oxandrolone treatment in the severely burned. Ann Surg. 2003;237:801–810. doi: 10.1097/01.SLA.0000071562.12637.3E. discussion 810–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tuvdendorj D, Chinkes DL, Zhang XJ, et al. Long-term oxandrolone treatment increases muscle protein net deposition via improving amino acid utilization in pediatric patients 6 months after burn injury. Surgery. 2011;149:645–653. doi: 10.1016/j.surg.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy KD, Thomas S, Mlcak RP, et al. Effects of long-term oxandrolone administration in severely burned children. Surgery. 2004;136:219–224. doi: 10.1016/j.surg.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 18.Przkora R, Jeschke MG, Barrow RE, et al. Metabolic and hormonal changes of severely burned children receiving long-term oxandrolone treatment. Ann Surg. 2005;242:384–389. doi: 10.1097/01.sla.0000180398.70103.24. discussion 390–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Przkora R, Herndon DN, Suman OE. The effects of oxandrolone and exercise on muscle mass and function in children with severe burns. Pediatrics. 2007;119:e109–e116. doi: 10.1542/peds.2006-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mlak RP, Buffalo MC. Pre-hospital management, transport, and emergency care. In: Herndon DH, editor. Total burn care. 3rd ed. Philadelphia: Saunders; 2007. pp. 81–92. [Google Scholar]
- 21.Suman OE, Mlcak RP, Chinkes DL, Herndon DN. Resting energy expenditure in severely burned children: Analysis of agreement between indirect calorimetry and prediction equations using the bland-altman method. Burns. 2006;32:335–342. doi: 10.1016/j.burns.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 22.Mlcak RP, Jeschke MG, Barrow RE, Herndon DN. The influence of age and gender on resting energy expenditure in severely burned children. Ann Surg. 2006;244:121–130. doi: 10.1097/01.sla.0000217678.78472.d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hart DW, Wolf SE, Herndon DN, et al. Energy expenditure and caloric balance after burn: Increased feeding leads to fat rather than lean mass accretion. Ann Surg. 2002;235:152–161. doi: 10.1097/00000658-200201000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. Cdc growth charts: United states. Adv Data. 2000:1–27. [PubMed] [Google Scholar]
- 25.Tanner JM, Davies PS. Clinical longitudinal standards for height and height velocity for north american children. J Pediatr. 1985;107:317–329. doi: 10.1016/s0022-3476(85)80501-1. [DOI] [PubMed] [Google Scholar]
- 26.Przkora R, Barrow RE, Jeschke MG, et al. Body composition changes with time in pediatric burn patients. J Trauma. 2006;60:968–971. doi: 10.1097/01.ta.0000214580.27501.19. discussion 971. [DOI] [PubMed] [Google Scholar]
- 27.Finnerty CC, Herndon DN, Chinkes DL, Jeschke MG. Serum cytokine differences in severely burned children with and without sepsis. Shock. 2007;27:4–9. doi: 10.1097/01.shk.0000235138.20775.36. [DOI] [PubMed] [Google Scholar]
- 28.Finnerty CC, Herndon DN, Przkora R, et al. Cytokine expression profile over time in severely burned pediatric patients. Shock. 2006;26:13–19. doi: 10.1097/01.shk.0000223120.26394.7d. [DOI] [PubMed] [Google Scholar]
- 29.Finnerty CC, Jeschke MG, Herndon DN, et al. Temporal cytokine profiles in severely burned patients: A comparison of adults and children. Mol Med. 2008;14:553–560. doi: 10.2119/2007-00132.Finnerty. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barrow RE, Mlcak R, Barrow LN, Hawkins HK. Increased liver weights in severely burned children: Comparison of ultrasound and autopsy measurements. Burns. 2004;30:565–568. doi: 10.1016/j.burns.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 31.Suman OE, Spies RJ, Celis MM, et al. Effects of a 12-wk resistance exercise program on skeletal muscle strength in children with burn injuries. J Appl Physiol. 2001;91:1168–1175. doi: 10.1152/jappl.2001.91.3.1168. [DOI] [PubMed] [Google Scholar]
- 32.Cleveland WS. Robust locally weighted regression and smoothing scatterplots. Journal of the American Statistical Association. 1979;74:829–836. [Google Scholar]
- 33.Chung EY, Romano JP. Exact and asymptotically robust permutation tests. Stanford University; 2011. [Google Scholar]
- 34.Romano JP, Wolf M. Exact and approximate stepdown methods for multiple hypothesis testing. Journal of the American Statistical Association. 2004;100:94–108. [Google Scholar]
- 35.Jeschke MG, Chinkes DL, Finnerty CC, et al. Pathophysiologic response to severe burn injury. Ann Surg. 2008;248:387–401. doi: 10.1097/SLA.0b013e3181856241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gauglitz GG, Herndon DN, Kulp GA, et al. Abnormal insulin sensitivity persists up to three years in pediatric patients post-burn. J Clin Endocrinol Metab. 2009;94:1656–1664. doi: 10.1210/jc.2008-1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Herndon DN, Tompkins RG. Support of the metabolic response to burn injury. Lancet. 2004;363:1895–1902. doi: 10.1016/S0140-6736(04)16360-5. [DOI] [PubMed] [Google Scholar]
- 38.Rutan RL, Herndon DN. Growth delay in postburn pediatric patients. Arch Surg. 1990;125:392–395. doi: 10.1001/archsurg.1990.01410150114021. [DOI] [PubMed] [Google Scholar]
- 39.Klein GL. Burn-induced bone loss: Importance, mechanisms, and management. J Burns Wounds. 2006;5:e5. [PMC free article] [PubMed] [Google Scholar]
- 40.Klein GL, Wolf SE, Langman CB, et al. Effects of therapy with recombinant human growth hormone on insulin-like growth factor system components and serum levels of biochemical markers of bone formation in children after severe burn injury. J Clin Endocrinol Metab. 1998;83:21–24. doi: 10.1210/jcem.83.1.4518. [DOI] [PubMed] [Google Scholar]
- 41.Bi LX, Wiren KM, Zhang XW, et al. The effect of oxandrolone treatment on human osteoblastic cells. J Burns Wounds. 2007;6:e4. [PMC free article] [PubMed] [Google Scholar]
- 42.Klein GL, Bi LX, Sherrard DJ, et al. Evidence supporting a role of glucocorticoids in short-term bone loss in burned children. Osteoporos Int. 2004;15:468–474. doi: 10.1007/s00198-003-1572-3. [DOI] [PubMed] [Google Scholar]
- 43.Klein GL, Herndon DN, Goodman WG, et al. Histomorphometric and biochemical characterization of bone following acute severe burns in children. Bone. 1995;17:455–460. doi: 10.1016/8756-3282(95)00279-1. [DOI] [PubMed] [Google Scholar]
- 44.Przkora R, Herndon DN, Sherrard DJ, et al. Pamidronate preserves bone mass for at least 2 years following acute administration for pediatric burn injury. Bone. 2007;41:297–302. doi: 10.1016/j.bone.2007.04.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Branski RC, Barbieri SS, Weksler BB, et al. Effects of transforming growth factor-beta1 on human vocal fold fibroblasts. Ann Otol Rhinol Laryngol. 2009;118:218–226. doi: 10.1177/000348940911800310. [DOI] [PubMed] [Google Scholar]
- 46.Choudhry MA, Bland KI, Chaudry IH. Trauma and immune response--effect of gender differences. Injury. 2007;38:1382–1391. doi: 10.1016/j.injury.2007.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Angele MK, Schwacha MG, Ayala A, Chaudry IH. Effect of gender and sex hormones on immune responses following shock. Shock. 2000;14:81–90. doi: 10.1097/00024382-200014020-00001. [DOI] [PubMed] [Google Scholar]
- 48.Ananthakrishnan P, Cohen DB, Xu DZ, et al. Sex hormones modulate distant organ injury in both a trauma/hemorrhagic shock model and a burn model. Surgery. 2005;137:56–65. doi: 10.1016/j.surg.2004.04.037. [DOI] [PubMed] [Google Scholar]
- 49.Sperry JL, Minei JP. Gender dimorphism following injury: Making the connection from bench to bedside. J Leukoc Biol. 2008;83:499–506. doi: 10.1189/jlb.0607360. [DOI] [PubMed] [Google Scholar]
- 50.Sperry JL, Nathens AB, Frankel HL, et al. Characterization of the gender dimorphism after injury and hemorrhagic shock: Are hormonal differences responsible? Crit Care Med. 2008;36:1838–1845. doi: 10.1097/CCM.0b013e3181760c14. [DOI] [PubMed] [Google Scholar]