Abstract
OBJECTIVE:
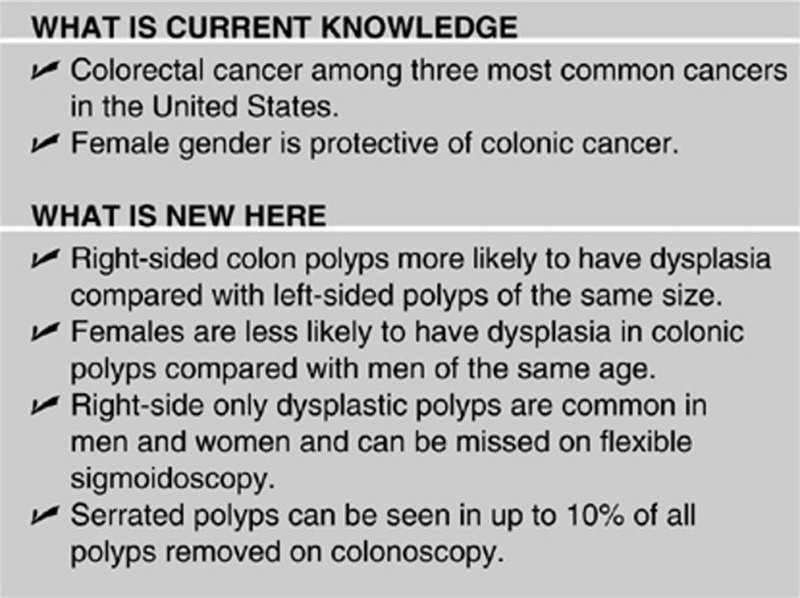
There is increasing evidence of significant clinical and biological differences between proximal and distal colorectal polyps, as well as possible differences based on patient gender. There is a need to optimize and individualize screening strategies. We studied the potential influence of gender and of polyp location on the presence of dysplasia in colon polyps.
METHODS:
We used a prospective database on adenoma detection to identify patients. The primary outcome was the presence of dysplasia in colonic polyps. Covariates include age, gender, race, lesion size and site, and use of aspirin. Multivariate logistic regression analysis was used to analyze the relationship between the primary outcome and covariates. Results were reported as odds ratios (ORs), 95% confidence intervals (CIs), and P-values.
RESULTS:
A total of 2,400 patients (50.5% females and 49.5% males) completed colonoscopy for various indications. A total of 3,045 polyps were removed in 1,237 patients. Of those polyps, 54% (n=1,636) were on the right compared with 46% (n=1,409) in the left colon. The proportion of adenomas was significantly greater on the right colon when compared with the left: 69.4% vs. 39.3% (P=<0.0001). Multivariate logistic regression analysis showed that the right colon did have a significant association with dysplasia when controlling for age, gender, polyp size, and use of aspirin (OR=3.1 (95% CI: 2.3–4), P=<0.0001). Female gender was associated with decreased odds of finding dysplasia (OR=0.6 (95% CI: 0.46–0.78), P=0.03).
CONCLUSION:
Patient characteristics (male gender) as well procedure findings (increase polyp size and right-sided lesions) are associated with increased odds of dysplasia.
INTRODUCTION
Colorectal cancer (CRC) remains one of the three most common cancers in the United States, with a lifetime incidence of about 5%.1, 2 Colonoscopy remains the gold-standard screening tool for colon cancer by removing precancerous adenomas, thus halting the adenoma-carcinoma sequence. Evidence suggests that colonoscopy has decreased the incidence of CRC in the United States.2, 3 Despite early reports,4, 5 colonoscopy appears to decrease the incidence of both right- and left-sided colon cancers.2 By definition, all adenomas are dysplastic.6 The presence of dysplasia on pathological specimen from colonic polyps is of great significance as it influences management and future surveillance colonoscopies.7, 8 It is well-established that larger polyps are more likely to be associated with dysplasia, including advanced dysplasia.9, 10, 11 In addition, older patients are more likely to have dysplasia.12
However, two more factors could have significant influence on the presence of dysplasia in colon polyps. One factor is the location of the polyp. Detecting right-sided polyps can be more challenging due to the shape of colonic folds and need for complete colonoscopy.13, 14 Right-sided lesions can be indicative of increased risk of recurrence of advanced adenomas.11 Difference in histology between right- vs. left-sided colon polyps has not been well-studied. Also, the gender of the patient can be of significance. Previous studies have suggested that female gender appears to be protective of colonic cancer.15 Similarly, post-menopausal women on hormonal therapy appear to have lower rates of CRC than women of the same age who are not on such therapy.12 One study suggested that male gender has a larger impact on the prevalence of colon cancer than family history of the disease.16
Therefore, the aim of this study is to assess the potential relationship between polyp's location and patient gender on the presence of dysplasia on colonic polyps detected on colonoscopy. We hypothesize that right-sided polyps are more likely to be adenomas when compared with left-sided polyps of the same size. We also hypothesize that women are less likely to have adenomas when compared with men.
METHODS
This study was based on the database of the Endoscopic Quality Improvement Program (EQUIP) trial.17 The EQUIP trial was a prospective randomized educational intervention trial in which we measured adenoma detection rates of 15 endoscopists on 2,400 colonoscopies. Colonoscopies were performed at the Mayo Clinic (in Jacksonville, Florida) ambulatory endoscopy center using high-definition colonoscopes (Olympus CF or PCF H180, Olympus Corp, Center Valley, NY) as well as high-definition video monitors. All endoscopists were board-certified gastroenterologists with significant experience in colonoscopy (median time since fellowship completion was 15 years). Endoscopists who performed less than 10 colonoscopies/quarter were excluded. All colonoscopies done in the ambulatory Gastrointestinal laboratory at the Mayo Clinic in Jacksonville between 8 February 2010 and 4 December 2011 were included in the study. Exclusion criteria for the study were as follows: inflammatory bowel disease or active colitis, hereditary polyposis syndromes, active overt GI bleeding, poor bowel preparation (based on Boston bowel preparation18 score <5), and history of colectomy. Polypectomies were done using standard biopsy forceps (for polyps <5 mm) or snare catheter (hot or cold) for larger polyps. Polyp size was measured by comparing a polyp to the biopsy forceps or snare catheter.
We used the database to extract the following data on each patient: patient age, gender, race, polyp sizes and histology, use of aspirins, location of the polyp, and preparation quality.19 Right-sided colon was defined as starting at the cecum and ending at the splenic flexure. Each polyp was classified as hyperplasic, adenoma (including sessile serrated), advanced adenoma, adenocarcinoma, or other (benign mucosa, inflammatory, leiomyoma, or lymphoid tissue). Dysplasia was defined as the presence of any of the following: adenoma (of any kind, including advanced adenomas), high-grade dysplasia, or adenocarcinoma. Advanced adenomas were those with the following features: ≥10 mm in size, tubulovillous, villous, or high-grade dysplasia. We defined a “flat polyp” as having <2.5 mm elevation above the mucosa (Paris class 0-II a-c). Sessile polyps and pedunculated polyps were also defined using the modified Paris classification.19 Serrated polyps were defined as those which were identified as serrated polyps by our pathologist. In addition, any hyperplastic polyp which was ≥1 cm and located in the right colon was also identified as a serrated polyp.20 In patients who had several polypectomies, the polyp with the worst degree of dysplasia and largest size was used for per-patient analysis. The primary outcome was the presence of dysplasia in colonic polyps. Covariates include patient age, gender, race, lesion size, lesion site (right colon vs. left colon), and use of aspirin.
Statistical analysis
We used SAS 9.2 (SAS Institute, Cary, NC) for statistical analysis. For continuous variables, we used the Wilk–Shapiro test to assess normality. For normal variables, we reported means and standard deviations. For non-normal data, we reported medians and interquartile ranges or ranges. For discrete data, we reported proportions. We used the Student's t-test to assess for differences between two means for normal data, whereas we used the Wilcoxon Ranks Sum test for continuous non-normal data. We used Fisher's exact or χ2 tests to asses for differences between proportions in different categories. To control clustering in the data and maximize the polyp data available, we used Generalized Estimating Equation modeling to test for the association between the primary outcome (presence of dysplasia) and potential confounders. Results were reported as odds ratios (OR) with 95% confidence intervals (CIs) and P-values. In addition, we also used multivariate logistic regression analysis to assess the association between the primary outcome and potential predictors on a per-patient level. Results from this analysis were also reported as OR with 95% CIs and P-values (value of <0.05 was used for statistical significance). This study was reviewed and approved by the Mayo Clinic Human Research Review Committee.
RESULTS
A total of 3,182 patients were studied. Of those, 782 were excluded for meeting at least one of the exclusion criteria. Only 3% (n=89) were excluded for incomplete colonoscopy. Therefore, 2,400 patients were included in the study. The proportions of males and females were similar: 50.5% (n=1,213) females vs. 49.5% (n=1,187) males. The indications for colonoscopy were various and included: screening (41.6%), surveillance (33.1%), or other indications (25.3%). Other indications included diarrhea, constipation, and abdominal pain. Most patients were middle-aged, with average patient age at 63 years (±12.5). In those 2,400, 52% (n=1,237) patients were found to have at least one colonic polyp (range: 1–16) and 38% (n=912) of patients were found to have at least one dysplastic/neoplastic lesion (adenoma, advanced adenoma, or adenocarcinoma). Baseline characteristics for the study patients are reported in Table 1. In total, 3,045 polyps were resected and analyzed.
Table 1. Baseline patient and procedure characteristics for 2,400 patients who had colonoscopy.
| Characteristic | No dysplasia (n=1,489) | Dysplasia (n=911) | P-value |
|---|---|---|---|
| Mean age (s.d.), years | 61 (+13) | 65.5 (+11) | <0.0001 |
| Median polyp size (IQR), mm | 5 (3–5) | 5 (4–10) | <0.0001 |
| Female | 839 (56%) | 374 (41%) | <0.0001 |
| History of aspirin use | 569 (38%) | 342 (38%) | NS |
| Patient race | |||
| White | 1,288 (87%) | 796 (87%) | NS |
| Black | 110 (7%) | 52 (6%) | NS |
| Hispanic | 45 (3%) | 36 (4%) | NS |
| Other | 46 (3%) | 27 (3%) | NS |
IQR, interquartile range; NS, non-significant.
Right vs. left colon polyps
Of the 3,045 polyps, slightly more polyps were found on the right colon compared with the left colon (54% vs. 46%, respectively). Of all polyps, median polyp size was similar on the right colon compared with the left colon: 5 vs. 5 mm, P=0.11. When reviewing the histological findings for the right vs. left colon, we found that the proportion of polyps that were adenomas was significantly higher on the right colon when compared with the left colon: 69.4% vs. 39.3% (P=<0.0001). However, there was no difference in the proportion of advanced adenomas (1.5% vs. 1.9%, P=0.4) or adenocarcinoma (0.6% vs. 0.4%, P=0.62) between the right and the left colon, respectively. Results are further summarized in Table 2. Per-patient analysis showed that 42% (381/912) of patients who had at least one dysplastic/neoplastic lesion had the lesion on the right side of the colon only (no dysplasia on the left side of the colon). Similarly, 22% (198/912) of patients had dysplasia/neoplasia on the left side only. The remaining 36% (33/912) of patients had dysplasia/neoplasia on both sides of the colon.
Table 2. Histological findings on colonic polyps in the right vs. left colon for 3,045 polyps found on 2,400 patients who underwent colonoscopy.
| Histology | Left colon (n=1,409) | Right colon (n=1,636) | P-value |
|---|---|---|---|
| Hyperplasic | 50.7% (715) | 29.8 % (n=303) | <0.0001 |
| Adenoma | 39.3% (n=553) | 69.4% (n=1,135) | <0.0001 |
| Advanced adenoma | 1.9% (n=27) | 1.5% (n=24) | NS |
| Adenocarcinoma | 0.4% (n=6) | 0.6% (n=10) | NS |
| Other | 7.7% (n=108) | 10% (n=164) | 0.026 |
NS, non-significant.
Other: benign mucosa, inflammation, leiomyoma, or lymphoid tissue.
Gender differences
Table 3 summarizes gender differences in polyp detection. Univariate analysis showed that females were less likely to have adenomas (P=0.001). The rates of serrated adenomas, advanced adenomas, and cancers were also lower for females but did not reach statistical significance.
Table 3. Histological findings on colonic polyps in the males vs. females for 3,045 polyps found on 2,400 colonoscopies.
| Histology | Women (n=1,263) | Men (n=1,782) | P-value |
|---|---|---|---|
| Hyperplastic polyps | 350 (28%) | 20.5% (n=366) | NS |
| Serrated polypsa | 10% (127) | 10 % (n=175) | NS |
| Adenoma | 52% (n=656) | 58% (n=1,032) | 0.0011 |
| Advanced adenoma | 1% (n=15) | 2% (n=36) | NS |
| Adenocarcinoma | 0.4% (n=6) | 0.5% (n=10) | NS |
| Other | 8.6% (n=109) | 9% (n=163) | NS |
NS, non-significant.
Other: benign mucosa, inflammation, leiomyoma, or lymphoid tissue.
Hyperplastic polyps more than 1 cm in size in the right colon were counted as serrated polyps.
In order to assess whether a flexible sigmoidoscopy approach was more appropriate in one group, we determined the prevalence of dysplasia/neoplasia in the right colon among patients who had no dysplastic lesions in the left colon. For women, this prevalence was 13.6% (165/1,213) for all dysplasia/neoplasia and 1.2% (14/1,213) for advanced adenoma. Corresponding numbers from men were 18% (216/1,187) and 1.6% (19/1,213).
Serrated polyps
As discussed earlier, all hyperplastic polyps >1 cm in size in the right colon were considered to be serrated polyps. Only one polyp was identified as sessile serrated adenoma by our pathologist. An additional 302 polyps were identified as serrated polyps based on the above definition. Therefore, the total rate of serrated polyps in our population was 10% (303/3,045).
Predictors of dysplasia/neoplasia
We used Generalized Estimating Equation to assess predictors of dysplasia/neoplasia. Such modeling uses a per polyp analysis while accounting for clustering of polyps found in the same patient. Male sex (OR=1.3 (95% CI: 1.1–1.6), P=0.034), and right-sided polyp location (OR=3 (95% CI: 2.3–3.3), P<0.0001), were both associated with increase risk of dysplasia/neoplasia while controlling for patient age, polyp side, and use of aspirin. Therefore, a right-sided polyp is three times as likely to have dysplasia when compared with left-sided polyp of the same size in a patient of the same age and gender. Similarly, a polyp in a male is 1.3 times more likely to have dysplasia/neoplasia than a polyp in a female when controlling for patient age and polyp size.
In a sub-analysis, we analyzed the results for patients who had undergone colonoscopy for screening purposes only. The results were identical to the larger group showing male sex (OR=1.4 (95% CI: 1.1–2), P=0.018), and right-sided polyp location (OR=2.3 (95% CI: 1.7–3.55), P<0.0001) to be associated with increase risk of dysplasia/neoplasia while controlling for patient age, polyp side, and use of aspirin.
In addition, we performed a per-patient analysis using multivariate logistic regression modeling to assess the data in per-patient analysis. For this analysis, we used the polyp of worst histology and largest dimension to analyze the data per patient. Multivariate logistic regression analysis showed that the right colon (OR 3.1 (95% CI: 2.3–4), P=<0.0001) did have a significant association with dysplasia when controlling for age, gender, polyp size, and use of aspirin. Similarly, female sex was associated with decreased odds of finding dysplasia (OR=0.6 (95% CI: 0.46–0.78), P=0.03) while controlling for the above confounders. As expected, polyp size (OR 1.04 (95% CI: 1.01–1.07), P=0.0089) and patient age (OR 1.03 (95% CI: 1.02–1.04), P=<0.0001) were both associated with increased risk of dysplasia.
Advanced adenomas and adenocarcinoma
Out of 2,400 patients, 6.4% (n=154) of patients had advanced adenomas on final pathology. Of those advanced adenomas, more were from males compared with females: 68% (n=104) vs. 32% (n=50), respectively (P<0.0001). The distribution of these advanced adenomas in men was as follows: 18% (n=19) on the right side only, 9% (n=9) in the left side only, and 73% (n=76) on both sides. In women, the distribution of advanced adenomas was as follows: 28% (n=14) on right side only, 8% (n=4) on the left side only, and 64% (n=32) on both sides. Therefore, among patients with advanced adenomas, females were more likely to have right only lesions compared with men: 28% vs. 18%, respectively, P=0.006.
Adenocarcinoma was found in 0.68% (n=16) of all patients. The rate of cancer in men was similar to women: 0.8% (10/1187) vs. 0.5% (6/1213), P=0.3. Most cancers were on the right side of the colon compared with the left: 81% (13/16) vs. 19% (3/16), respectively, P=0.0003. In a sub-analysis, we investigated the relationship between patient's sex and polyp location on the presence of advanced ademomas. When controlling for age, polyp size, and use of aspirin, male gender was again associated with increased risk of advanced adenoma (OR=2.2 (95% CI: 1.02–4.7), P=0.046). However, right-sided polyp was not associated with increased risk of advanced adenoma is this analysis (P=0.08).
DISCUSSION
In this study, we found that females were less likely to have dysplasia in colonic polyps when controlling for potential confounders, including patient age, polyp size, and use of aspirin. Similarly, we also found that right-sided lesions are more likely to be dysplastic when compared with left-sided lesions of the same size.
The effect of patient's sex on the risk of colon cancer has been previously studied. Hoffmeister et al. studied 3,349 German patients who underwent screening colonoscopies.16 Using a log-binomial regression model, they concluded that women are less likely to have CRC, advanced adenomas, and non-advanced adenomas. Such findings are in agreement with our results, showing female gender to be protective of dysplasia (all adenomas) and advanced adenomas. Brenner et al. used the SEER database to investigate the issue of gender and CRC.21 They found that women's 10-year cumulative incidence and mortality for CRC seem to lag behind that of men's by 4–8 years. Similarly, Wei et al. used data from the women's health study and found a decrease in CRC in women using oral contraceptives (23% decrease in the risk of CRC).12 In addition, a Polish study of more than 50,000 people found that advanced adenomas are more common in men than women.22 These findings are again similar to the finding in our study. These data strongly suggest that women are at lower risk of CRC. One possible explanation for this is a hormonal protection to women pre-menopause, which would explains the lag in CRC incidence in women compared with men of the same age.
Adding to the complexity of the discussion, a study by Schoenfeld et al. of 1,463 women found that 4.9% (n=72) had advanced adenomas.23 Of those patients with advanced adenomas, 65% (n=47) were on the right side of the colon. When compared with men, the authors concluded that women were more like to have proximal (right) colon advanced adenoma in the absence of advanced adenoma in the distal (left) colon. Our results are in agreement with Schoenfeld et al. Women with advanced adenomas were more likely to have only right-sided lesions when compared with men. We conclude that, advanced adenomas are more common in men. Yet, if a women has advanced adenoma, it is more likely to be on the right only (with no advanced adenomas on the left colon) when compared with men. As a result, a full colonoscopy is imperative in both genders to avoid missing advanced adenomas. In addition, a polyp was more likely to be dysplastic if it was on the right colon when compared with a polyp of the same size in the left colon (regardless of gender).
Whether screening for CRC should be gender-specific continues to be a topic of discussion. Some would argue that it might be safe for women to start screening for CRC at a later age than men or that women should be screened with a flexible sigmoidoscopy only. Yet, our data shows that both men and women can have dysplasia on the right side of the colon in the absence of any dysplasia on the left side. Those lesions can then develop into a carcinoma if a colonoscopy is never done. Therefore, we believe that a full colonoscopy, rather than a flexible sigmoidoscopy is warranted in both men and women. For women with negative risk factors for CRC, increasing the age at which colonoscopy is started may be reasonable, but will require larger prospective studies.
There has been continued debate on the strategy of using optical methods to diagnose hyperplastic and adenomatous polyps with non-removal if hyperplastic. This again is aimed at reducing the cost of screening colonoscopies. The current threshold for considering non-removal of a hyperplastic appearing polyp are >90% negative predictive value.24 As the negative predictive value is affected by both the pre-test probability as well as test accuracy, it is important to understand that left-sided polyps have higher pre-test probability of benign hyperplastic and are thus more appropriate to consider optical diagnosis with no removal. On the other hand, a right-sided polyp in a male patient is very likely to be adenoumatous, even if it is small or if it looks benign, and should be removed. Such arguments may be especially appealing at a time when the cost of healthcare in the United States continues to increase. One of the possible limitations for such changes is the added complexity to CRC screening, which is already a complicated algorithm.
The issue of serrated adenomas continues to generate significant interest. Currently, serrated adenomas are thought to include four subtypes: sessile serrated adenomas, traditional serrated adenomas, large hyperplasic polyps in the right colon, and mixed serrated polyps. Serrated polyps' progression to cancer is through the serrated pathway (which is different from the adenoma-carcinoma pathway of traditional adenomas).25 Serrated polyps are important for several reasons: they are more common on the right side of the colon, they are commonly sessile (or flat), they can be covered with mucus or stool particles, and they can have a benign appearance.26 All of those factors make serrated polyps harder to detect by the endoscopist.20 Previous studies have reported the rate of serrated polyps to be 2–5.3% of all polyps removed during colonoscopy.25, 27, 28, 29, 30 In our study, we noted that 10% of all polyps were serrated. This is higher than in reported literature. However, our definition of serrated polyps includes all large hyperplastic polyps in the right colon. Such definition, though accurate, was not routinely used by previous studies, which can explain the higher rate of serrated adenomas in our study. Based on our study, women seem less likely to have serrated polyps compared with men, but this did not reach statistical significance.
Our study has several limitations. The retrospective design of the study makes it prone to possible confounders. In addition, the study was done in a single-referral center with high adenoma detection rates, which may not be as applicable to community-based colonoscopies with lower adenoma detection rates.17 Also, we were unable to control for smoking status. Such information was not collected during the EQUIP study. We know that smoking increases the risk of dysplasia and advanced adenomas.16, 31, 32 We have no reason to believe that smoking rates in our patient population is different from other studies; therefore, the affect of smoking is unlikely to change our final conclusions.
Our study has several strengths. These include the high quality of the data that was gathered in a prospective manner. In addition, the number of patients (2,400) and polyps (3,045) were large and allowed for greater power to detect differences between groups.
In conclusion, polyps in the right colon seem to have a similar size to those of the left colon. Yet they are more likely to have dysplasia when compared with polyps on the left side of the colon. Therefore, missing a small polyp in the right colon is likely more significant than missing one in the left colon, where most polyps are hyperplastic. Improved examination of the right colon is needed in order to detect and resect adenomatous polyps. Patient characteristics (male gender) and procedure findings (increased polyp size and right-sided lesions) are associated with increased odds of dysplasia. In older males, extra time/attention should be devoted to detection and removal of right-sided lesions, which are more likely to have dysplasia.
Study Highlights
Acknowledgments
Editorial assistance for the preparation of the article was provided by Victoria L. Jackson, MLIS (Academic and Research Support, Mayo Clinic, Jacksonville, FL).
Guarantor of the article: Michael B. Wallace, MD.
Specific author contributions: Study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis: Bashar J. Qumseya; acquisition of data, drafting of the manuscript: Susan Coe; study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis, and study supervision: Michael B. Wallace.
Financial support: None.
Potential competing interests: Dr Wallace is a consultant for Ninepoint Medical. He receives research funding from Olympus America, Inc., American BioOPTICS, and Fujinon.
References
- Merrill RM, Anderson AE. Risk-adjusted colon and rectal cancer incidence rates in the United States. Dis Colon Rectum. 2011;54:1301–1306. doi: 10.1097/DCR.0b013e3182242bd3. [DOI] [PubMed] [Google Scholar]
- Siegel RL, Ward EM, Jemal A. Trends in colorectal cancer incidence rates in the United States by tumor location and stage, 1992–2008. Cancer Epidemiol Biomarkers Prev. 2012;21:411–416. doi: 10.1158/1055-9965.EPI-11-1020. [DOI] [PubMed] [Google Scholar]
- Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687–696. doi: 10.1056/NEJMoa1100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner H, Hoffmeister M, Arndt V, et al. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010;102:89–95. doi: 10.1093/jnci/djp436. [DOI] [PubMed] [Google Scholar]
- Baxter NN, Goldwasser MA, Paszat LF, et al. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1–8. doi: 10.7326/0003-4819-150-1-200901060-00306. [DOI] [PubMed] [Google Scholar]
- Rex DK, Ulbright TM, Cummings OW. Coming to terms with pathologists over colon polyps with cancer or high-grade dysplasia. J Clin Gastroenterol. 2005;39:1–3. [PubMed] [Google Scholar]
- Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–1595. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Davila RE, Rajan E, Baron TH, et al. ASGE guideline: colorectal cancer screening and surveillance. Gastrointest Endosc. 2006;63:546–557. doi: 10.1016/j.gie.2006.02.002. [DOI] [PubMed] [Google Scholar]
- van Stolk RU, Beck GJ, Baron JA, et al. Adenoma characteristics at first colonoscopy as predictors of adenoma recurrence and characteristics at follow-up. The Polyp Prevention Study Group. Gastroenterology. 1998;115:13–18. doi: 10.1016/s0016-5085(98)70359-2. [DOI] [PubMed] [Google Scholar]
- Noshirwani KC, van Stolk RU, Rybicki LA, et al. Adenoma size and number are predictive of adenoma recurrence: implications for surveillance colonoscopy. Gastrointest Endosc. 2000;51:433–437. doi: 10.1016/s0016-5107(00)70444-5. [DOI] [PubMed] [Google Scholar]
- Martinez ME, Sampliner R, Marshall JR, et al. Adenoma characteristics as risk factors for recurrence of advanced adenomas. Gastroenterology. 2001;120:1077–1083. doi: 10.1053/gast.2001.23247. [DOI] [PubMed] [Google Scholar]
- Wei EK, Colditz GA, Giovannucci EL, et al. Cumulative risk of colon cancer up to age 70 years by risk factor status using data from the Nurses' Health Study. Am J Epidemiol. 2009;170:863–872. doi: 10.1093/aje/kwp210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rex DK. Maximizing detection of adenomas and cancers during colonoscopy. Am J Gastroenterol. 2006;101:2866–2877. doi: 10.1111/j.1572-0241.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- Rex DK. Colonoscopic withdrawal technique is associated with adenoma miss rates. Gastrointest Endosc. 2000;51:33–36. doi: 10.1016/s0016-5107(00)70383-x. [DOI] [PubMed] [Google Scholar]
- Giovannucci E. Obesity, gender, and colon cancer. Gut. 2002;51:147. doi: 10.1136/gut.51.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmeister M, Schmitz S, Karmrodt E, et al. Male sex and smoking have a larger impact on the prevalence of colorectal neoplasia than family history of colorectal cancer. Clin Gastroenterol Hepatol. 2010;8:870–876. doi: 10.1016/j.cgh.2010.07.004. [DOI] [PubMed] [Google Scholar]
- Coe STC, Diehl N, Wallace MB. A Randomized Controlled Trail of an Endoscopic Quality Improvement Program (EQUIP) Results in Improved Detection of Colorectal Adenomas. Am J Gastroenterol. 2011;106:s576. [Google Scholar]
- Lai EJ, Calderwood AH, Doros G, et al. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69:620–625. doi: 10.1016/j.gie.2008.05.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endoscopic Classification Review Group Update on the paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy. 2005;37:570–578. doi: 10.1055/s-2005-861352. [DOI] [PubMed] [Google Scholar]
- Snover DC, Jass JR, Fenoglio-Preiser C, et al. Serrated polyps of the large intestine: a morphologic and molecular review of an evolving concept. Am J Clin Pathol. 2005;124:380–391. doi: 10.1309/V2EP-TPLJ-RB3F-GHJL. [DOI] [PubMed] [Google Scholar]
- Brenner H, Hoffmeister M, Arndt V, et al. Gender differences in colorectal cancer: implications for age at initiation of screening. Br J Cancer. 2007;96:828–831. doi: 10.1038/sj.bjc.6603628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regula J, Rupinski M, Kraszewska E, et al. Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N Engl J Med. 2006;355:1863–1872. doi: 10.1056/NEJMoa054967. [DOI] [PubMed] [Google Scholar]
- Schoenfeld P, Cash B, Flood A, et al. Colonoscopic screening of average-risk women for colorectal neoplasia. N Engl J Med. 2005;352:2061–2068. doi: 10.1056/NEJMoa042990. [DOI] [PubMed] [Google Scholar]
- Rex DK, Kahi C, O'Brien M, et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;73:419–422. doi: 10.1016/j.gie.2011.01.023. [DOI] [PubMed] [Google Scholar]
- Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088–2100. doi: 10.1053/j.gastro.2009.12.066. [DOI] [PubMed] [Google Scholar]
- Kahi CJ, Hewett DG, Norton DL, et al. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy. Clin Gastroenterol Hepatol. 2011;9:42–46. doi: 10.1016/j.cgh.2010.09.013. [DOI] [PubMed] [Google Scholar]
- Teriaky A, Driman DK, Chande N. Outcomes of a 5-year follow-up of patients with sessile serrated adenomas. Scand J Gastroenterol. 2012;47:178–183. doi: 10.3109/00365521.2011.645499. [DOI] [PubMed] [Google Scholar]
- Lash RH, Genta RM, Schuler CM. Sessile serrated adenomas: prevalence of dysplasia and carcinoma in 2139 patients. J Clin Pathol. 2010;63:681–686. doi: 10.1136/jcp.2010.075507. [DOI] [PubMed] [Google Scholar]
- Gurudu SR, Heigh RI, De Petris G, et al. Sessile serrated adenomas: demographic, endoscopic and pathological characteristics. World J Gastroenterol. 2010;16:3402–3405. doi: 10.3748/wjg.v16.i27.3402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min YW, Lee JH, Lee SH, et al. Prevalence of proximal colon serrated polyps in a population at average risk undergoing screening colonoscopy: a multicenter study. Clin Res Hepatol Gastroenterol. 2012. [DOI] [PubMed]
- Botteri E, Iodice S, Raimondi S, et al. Cigarette smoking and adenomatous polyps: a meta-analysis. Gastroenterology. 2008;134:388–395. doi: 10.1053/j.gastro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- Lieberman DA, Prindiville S, Weiss DG, et al. Risk factors for advanced colonic neoplasia and hyperplastic polyps in asymptomatic individuals. JAMA. 2003;290:2959–2967. doi: 10.1001/jama.290.22.2959. [DOI] [PubMed] [Google Scholar]


