Abstract
Background and Purpose
Perfusion computerized tomography (PCT) has been used to assess the extent of blood brain barrier (BBB) breakdown. The purpose of this study was to determine the predictive value of (BBB) permeability (BBBP) measured using PCT for development of malignant middle cerebral artery infarction (MMCA) requiring hemicraniectomy (HC).
Methods
We retrospectively identified patients from our stroke registry that had MCA infarction and were evaluated with admission PCT. BBBP and cerebral blood volume (CBV) maps were generated and infarct volumes calculated. Clinical and radiographic characteristics were compared between those who underwent HC versus those who did not undergo hemicraniectomy (NHC).
Results
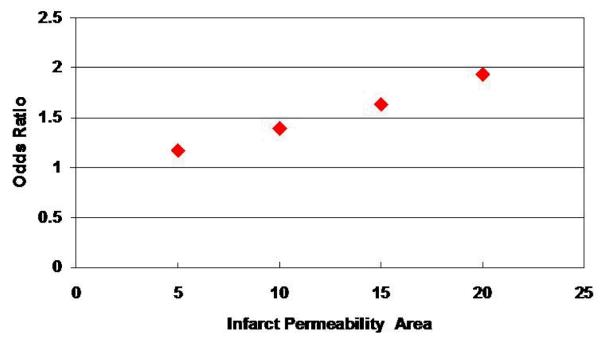
122 patients (12 (HC), 110 (NHC)) were identified. 12 patients who underwent HC had developed edema, midline shift or infarct expansion. Infarct permeability area (IParea), infarct CBV area (ICBVarea), and infarct volumes were significantly different (p<0.018, p<0.0211, p<0.0001, p<0.0014) between HC and NHC groups. Age (p=0.03) and admission National Institutes of Health Stroke Scale (NIHSS) (p=0.0029) were found to be independent predictors for HC. Using logistic regression modeling, there was an association between increased IParea and HC. The odds ratio for HC based on a 5, 10, 15 or 20 cm2 increase in IParea were 1.179, 1.390, 1.638 or 1.932, respectively (95% CI 1.035-1.343, 1.071-1.804, 1.108-2.423, 1.146-3.255).
Conclusion
Increased IParea is associated with an increased likelihood for undergoing HC. Since early HC for MMCA has been associated with better outcomes, the IParea on admission PCT might be a useful tool to predict MMCA and need for HC.
INTRODUCTION
About 10–15% of all patients with cerebral infarction in the territory of the middle cerebral artery (MCA) suffer from progressive clinical deterioration because of increasing brain swelling, raised intracranial pressure, and brain herniation. This patient population constitutes a particularly difficult challenge for clinicians charged with their care.1–3 Because of the limitations of medical therapies; decompressive surgery is an option for patients with neurological deterioration due to large hemispheric infarction and edema. The rationale of this therapy is to prevent brain tissue shifts and to normalize intracranial pressure, and thereby preserve cerebral blood flow and prevent secondary damage.4 Hemicraniectomy (HC) for malignant middle cerebral artery infarctions (MMCA) has been shown to be an effective treatment.5 Currently, clinical data and early cranial tomography (CT) does not reliably identify patients that will develop MMCA. Prognostic criteria that might permit early identification of patients at risk for such “malignant” infarction are important.6-8
Perfusion CT (PCT) is a modern imaging technique that has been proposed for evaluating acute stroke patients at the time of their emergent evaluation. PCT involves the sequential acquisition of CT images performed in cine mode during the intravenous administration of iodinated contrast material and has been reported to allow for accurate quantitative assessment of cerebral blood flow (CBF) and cerebral blood volume (CBV).9 It also has been validated in determining final infarct volumes and measuring potentially salvageable tissue using different PCT maps.10 By extending the PCT acquisition time window, blood-brain-barrier permeability (BBBP) can also be obtained.11 PCT techniques for measuring BBBP have been shown to be achievable in tumor models in animals12, 13 and in a small human series 14, but only recently has it been applied to acute stroke imaging.15
The aim of this retrospective study was to determine whether permeability maps, generated from admission PCT, can be used to predict MMCA. We hypothesized that patients with an increased area of permeability defect would be at higher risk for development of MMCA.
METHODS
We retrospectively reviewed our registry from 8/07 to 8/09 and identified 268 consecutive patients diagnosed with MCA infarctions (18 patients in the HC group and 250 patients in non-hemicraniectomy (NHC) group). We included in our analysis patients that underwent PCT on admission with interpretable permeability maps. Two patients in the HC and 31 patients in NHC group had uninterpretable PCT maps. Three patients in HC and 76 patients in the NHC groups did not have PCT. Patients who had their care withdrawn were also excluded from the analysis. In total, 122 patients fit our criteria: 12 underwent HC and 110 in the NHC group. Demographic characteristics and baseline clinical information including admission NIHSS, admission glucose level, HbA1c, lipids, the timing of MRI acquisition and PCT were extracted from the medical records. Clinical, laboratory and radiographic characteristics were analyzed between the two groups.
Calculation of Infarct Volumes
All MRI scans were performed before decompression in the HC group. One of the investigators was blinded to clinical outcomes and independently reviewed all the DWI images to verify infarct volumes. Infarct volumes were measured by hand-drawn regions of interest around each area of infarct in every slice separately. The regions of interest area were calculated automatically by the Picture Archiving and Communication Systems software (General Electric Centricity workstation) and then multiplied by the slice thickness (5 mm for DWI). Seven patients (58.3%) in the HC group and 85 patients (77.3%) in the NHC group had DWI.
Calculation of Permeability and CBV volume
Permeability color maps were retrospectively generated from PCT data using a modified Patlak method. PCT was performed on a Siemens Somatom Sensation 40 scanner. After intravenous administration of 40 cc iodinated contrast at 8cc/sec by a power injector into an antecubital vein (Omnipaque, 350/40 mL ), images were acquired without delay. PCT imaging parameters were 80 kVp, 270 mAs, 1.2 mm section collimation. Slice thickness was 9.6 mm acquired 3 slices at a time for 75 seconds. The modified Patlak model (in Siemens Syngo Neuro PCT) calculates vascular permeability (PS) with CT enhancement values after the peak contrast enhancement has been reached and utilizing a built-in delay correction algorithm. This allows estimation of PS during the end of the first-passage of contrast but avoids erroneous elevation of PS values secondary to delayed arrival of contrast which would occur in a standard application of the Patlak model to PCT data in the setting of acute cerebral ischemia16. From the PCT data, permeability maps were calculated using Syngo Neuro PCT software which sets the threshold for generating the permeability maps at 0.5 ml/10 ml/min. We defined the perfusion abnormality as the region analyzed on the permeability maps, IP as the weighted mean of the permeability value, and IParea as the area of the region that had perfusion abnormality. Each permeability map was analyzed by demarcating trace lines around the area of perfusion abnormality on each of the 3 slices. IP and IParea values were measured by hand-drawn regions of interest in every slice separately. The weighted mean of IP and IParea of the 3 slices were calculated, respectively and used for statistical analysis. Contra-lateral non-ischemic hemisphere was used as a control (CP).
Using the Siemens Syngo Neuro software, CBV was calculated along with CBF using the maximal slope model which has been shown to yield lesion volumes that are similar to delay-insensitive deconvolution techniques17.The hypoperfused areas on CBV maps were defined as volume abnormality. The infarct core was outlined on CBV maps as a severely hypoperfused area displayed by 2 colors in the color bar (eg, purple and blue). The CBV threshold was defined at 2.0 ml×100 g−1. Each CBV map was analyzed by demarcating trace lines around the area of volume abnormality on each of the 3 slices by hand-drawn regions of interest. The area of volume abnormality was defined as CBVarea. The weighted mean of CBV and CBVarea were calculated in each of the 3 slices respectively and used for statistical analysis. Representative images of CBV and permeability are shown in fig 1 from a patient who developed malignant infarction and underwent HC.
Figure 1.
A 75-year-old right-handed man who presented with sudden onset of left hemiparesis and dysarthria. (A)Admission CT; (B)Admission CBV color maps, showing hypoperfusion with right MCA acute ischemic stroke (AIS). (C)Admission Permeability color maps, showed permeability abnormality with right MCA AIS. (D)Subsequent head CT before HC, showing malignant MCA infarction.
Statistical Analysis
Means with standard deviations or medians for continuous variables and proportions for categorical variables were used. The differences were assessed using t-tests, chi-square tests, Fisher exact test or Mann-Whitney U test. A significance level of 0.05 was used to assess statistical difference. We used multivariate analysis using logistic regression to obtain odds ratios to determine associations, controlling for potential confounders. The statistical analysis was performed using SAS 9.2.
RESULTS
Patients
We included 122 patients in total, 12 HC and 110 NHC. Of the baseline characteristics analyzed, mean age (56.08+ 13.20 vs 65.40+13.66; p<0.03) was statistically different between the HC and NHC groups. Patients in the HC group were significantly younger than the NHC group. Other baseline characteristics such as gender, race and risk factors were not statistically different between the 2 groups (Table 1). Laboratory parameters (mean serum glucose at admission, Hb A1c level, serum total cholesterol level, triglyceride, HDL, LDL) assessed at baseline were not significantly different between HC and NHC groups.
Table 1.
Demographics and Preexisting Conditions
| Hemicraniectomy group (n=12) |
Non-Hemicraniectomy group (n=110) | P Value | |
|---|---|---|---|
|
Age in yrs (mean ±
SD) |
56.08 ± 13.20 | 65.40±13.66 | 0.03 * |
| Gender | 0.66 † | ||
| Female (%) | 7 (58.33) | 57(51.82) | |
| Male (%) | 5 (41.67) | 53 (48.18) | |
| Race | 0.11‡ | ||
| Black (%) | 4 (33.33) | 27 (25.71) | |
| Hispanic (%) | 4 (33.33) | 12 (11.43) | |
| White (%) | 4 (33.33) | 63 (60) | |
| Others (%) | 0 (0) | 3 (2.86) | |
| Risk factors | |||
| Hypertension (%) | 9(75) | 77(70) | 0.71† |
| Diabetes Mellitus (%) | 2( 16.67) | 29(26.36) | 0.72‡ |
| Coroner disease (%) | 3 (25) | 24 (21.82) | 0.72‡ |
| Atrial Fibrillation (%) | 4 (33.33) | 18 (16.36) | 0.22‡ |
| Smoking (%) | 3 (25) | 37 (33.64) | 0.74‡ |
TT=Student’s t test;
CS= chi-square test;
FET=Fisher’s Exact Test
Clinical Factors
Baseline stroke severity, as measured by median NIHSS scores, was significantly higher in the HC group than the NHC group (19 (11-29) vs 11 (0-40); p<0.0029). The mean time from stroke onset to PCT in minutes in the HC and NHC groups were 310.55±306.75 and 502.56 ±845.90, respectively. There was no significant difference in time to PCT scanning between two groups (p=0.19). Seven (58.3%) patients in the HC group and 85 (77.3%) patients in the NHC group had DWI (p<0.0035). Onset to acquired DWI images was not statistically different (877.6+ 712.7 vs 975.5 + 709.4 minutes, p=0.7680) (Table 2).
Table 2.
Clinical Characteristic
| Clinical Features | Hemicraniectomy group (n=12) |
Non-Hemicraniectomy group (n=110) | P Value |
|---|---|---|---|
| Admission NIHSS median (min-max) |
19 (11-29) | 11( 0- 40) | 0.0029§ |
| Onset to PCT in minutes (mean ± SD) |
310.55 ± 306.75 | 502.56 ± 845.90 | 0.19* |
| Onset to DWI in minutes (mean ± SD) |
877.6± 712.7 | 975.5 ± 709.4 | 0.76* |
| iv t-PA given (%) | 4 (33.33) | 60(54.55) | 0.22‡ |
NIHSS=National Institutes of Health Stroke Scale;
TT=Student’s t test;
TST= Two –sample test,
FET=Fisher’s Exact Test
Radiographic Characteristics
Mean DWI infarct volume was significantly larger in the HC group compared with the NHC group (162.206 + 81.20 vs 43.62 + 55.33 cc; p< 0.0014). Patients with infarct volumes greater than 145 cc were more likely to receive HC (62.5% vs 37.5%; p<0.0001).
No significant differences in IP were observed between the two groups (7.26 + 2.95 mL .min −1. [100 g] −1) vs 8.44+ 7.42 mL .min −1 .[100 g] −1), p=0.2950). Similarly, no significant differences in mean CBV were observed between HC and NHC groups (13.72+ 12.89 mL. [100 g] −1) vs. 16.55+ 12.15 mL. [100 g] −1, p= 0.4487) (Table 3). The mean IParea was significantly different between the two groups (61.97+ 27.10 vs 41.485 + 32.270; p<0.018). We used a logistic regression model to determine whether IParea is associated with the probability of having a HC, controlling for potential confounders. We found that the odds of receiving a HC was higher for patients with larger IParea (OR: 1.018(1.001, 1.036); p=0.0432). The odds ratios and 95% CI for HC based on a 5, 10, 15 or 20 cm2 increase in IParea were 1.179(1.035, 1.343), 1.390(1.071, 1.804), 1.638(1.108, 2.423) and 1.932 (1.146, 3.255), respectively). Thus, a patient with IParea of 50 would have a 39% higher odds of having HC compared to a patient with IParea 40 (Fig 2). The positive predictive value of IParea for HC was 10.4% and the negative predictive value 100%. There was a significant association between receiving HC and DWI volume (OR: 1.019(1.007, 1.031); p=0.0016) but not with CBV lesion volume (OR: 0.976(0.916, 1.040); p=0.4513). However, when controlling for the DWI volume, there was no association between receiving HC and IParea (OR: 1.008(0.975, 1.041); p=0.6391). There was no correlation between DWI volume and IParea (p=0.5219). We also did not find a correlation between IParea and admission NIHSS (p=0.0817), HbA1c levels (p=0.9072) or admission glucose levels. (p=0.6542).
TABLE 3.
Radiographic measurements
| Radiographic measurements | Hemicraniectomy (n=12) |
Non- hemicraniectomy (n= 110) |
P value |
|---|---|---|---|
| DWI infarct volumes ( mean ± SD) cm3 |
162.20 ± 81.20 (n=7) |
43.62 ± 55.33 (n=85) |
0.0014§ |
| DWI infarct volumes ≥ 145 cm3 (%) |
5 (83.33%) | 1(16.67%) | 0.0001† |
| Infarct permeability | 7.26mL.min−1.[100 g]−1 ±2.95 | 8.44mL.min−1.[100 g]−1±7.42 | 0.29* |
| Infarct permeability area | 61.97 cm2±27.10 | 41.48 cm2±32.27 | 0.018§ |
| Contralateral permeability | 2.80mL.min1.[100g]−1±1.88 | 2.71mL.min−1.[100 g]−1±3.11 | 0.92* |
| Infarct cerebral blood volume | 13.72 mL. [100 g ]−1±12.89 | 16.55 mL. [100 g ]−1±12.15 | 0.44* |
| Infarct cerebral blood volume area | 48.36 cm2±24.23 | 29.14 cm2±27.33 | 0.0211* |
| Contralateral cerebral blood volume |
29.80 mL. [100 g ]−1±10.04 | 28.86 mL. [100 g ]−1±10.72 | 0.77* |
CS= chi-square test,
TST= Two –sample test
TT=Student’s t test,
Figure 2.
Graphic 1: Change in Infarct Permeability Area vs Odds Ratio
DISCUSSION
Progressive deterioration of clinical status due to massive hemispheric edema occurs in 10% of patients and is described as the “MMCA.” Ischemic edema occurs within hours after stroke onset 18 and is initially cytotoxic characterized by intracellular water accumulation, and later vasogenic, in which water moves across the blood-brain barrier (BBB) into the extracellular interstitial space. The disruption of the BBB can be demonstrated as early as 20 minutes after brain ischemia in rats.18, 19
Over the past 15 years, several studies have shown that decompressive surgery is a possible treatment strategy for increased ICP after severe hemispheric stroke and can reduce the mortality to less than 50%.3,20-23 The clinical course of many patients with severe MCA stroke is predictable. Therefore, waiting for pupillary dilatation causes an unnecessary delay.24,25 However, there is little information to guide clinicians in selecting which patients are most suitable for this aggressive intervention.
The aim of this study was to define radiographic predictors of malignant MCA infarct in retrospectively evaluated MCA stroke patients and to provide early prognostic factors that may affect treatment decisions of clinicians. Patients that underwent HC were significantly younger than the NHC group. Wijdicks and colleagues26 suggested that ICP in younger patients might rise rather quickly due to less reserve to compensate for the increase in volume. Certain degrees of age-related cerebral atrophy might protect older patients from space-occupying brain swelling.2,7,8,27 Age is an important factor for deciding to pursue surgery and clinicians focus on younger patients before signs of herniation appear, such as stroke severity. Krieger et al reported that patients with malignant MCA strokes had a higher NIHSS score at admission and no single item or cluster of items in the NIHSS was a predictor of fatal brain edema than the total NIHSS score.8 Higher NIHSS scores at admission were found in our HC group as well.
DWI is increasingly being used for the early management of acute stroke.28 Oppenheim et al 28 had used DWI to study patients with impending malignant MCA infarction and found a mean DWI volume of 244 cm3 in patients with malignant MCA infarction and a cutoff value of 145 cm3 to predict massive brain edema within the first 14 hours after stroke.28 We identified a mean volume of infarct of 162.20 cm3 and a cut off value of 100 cm3 in the HC population. Quantitative measurement of DWI volumes is a reliable factor to decide for HC.
Other radiographic factors may play a role in determining the population at risk for subsequent fatal ischemic brain swelling.8 PCT is an imaging technique currently used to evaluate acute stroke patients at the time of their emergency evaluation.9 Dittrich et al have even reported that the blood flow and volume parameters of PCT might permit identifying patients at risk for malignant infarction.29 More recently, PCT has been used to characterize the BBBP.15, 30, 31 A relatively simple and frequently applied model to calculate BBBP is the Patlak model.32,33 Applying this model to PCT data 15,34-36 requires using arterial and parenchymal contrast enhancement curves to calculate the rate of contrast transfer from the intravascular to the extravascular compartment, which is a measure of BBBP. Microvascular permeability (expressed as the transendothelial transfer constant [kPS] or permeability surface area product [PS]) is a metric of BBB integrity. Similar to the standard perfusion metrics, PS can also be calculated using dynamic imaging by measuring the leakage of an intravascular tracer into the extravascular (interstitial) space.33, 37, 38
In the normal brain parenchyma, PS is 0 for relatively large hydrophilic molecules (such as a peripherally injected iodinated contrast agent), which reflects the tight regulation of the BBB.39-42 Evidence from animal and human studies suggests that increased permeability can occur in the first 2–4 hours of acute ischemia.43-45 In our study, the infarct permeability area and infarct cerebral blood volume area of the ischemic region determined by PCT were shown to be significantly larger in patients in the HC group. This result can be explained by the fact that the patients with larger infarct permeability developed malignant brain edema. Recently PCT data were also used to characterize the BBBP, in an effort to predict which stroke patients develop hemorrhagic transformation. 15 Lin et al showed that elevated PS had been detectable during the hyperacute period using first pass dynamic CT data and was predictive for hemorrhagic transformation in patients who received t-PA.15 Aviv et al evaluated the admission PS measurements of acute stroke patients and reported that a PS threshold of 0.23mL-(100 g) −1 had high sensitivity and specificity for predicting hemorrhagic transformation46 Taken together, these studies along with our results underscore the fact that a compromise in the BBB is a necessary but not sufficient criterion for hemorrhagic transformation. If the permeability of the BBB is not large enough for blood cellular elements (RBC, platelets) to pass, hemorrhage will not occur, but the BBB only needs to be permeable to much smaller molecules such as albumin in order for water to follow it into the interstitial space and cause edema. BBB permeability maps may therefore have even more utility than just predicting hemorrhage by showing which patients may develop malignant edema.
This study is limited by its retrospective design and small sample number in the HC group. There could also have been variations in the gravity of the MCA infarcts (e.g. ICA infarct with involvement of the ACA) which may have favored HC and thus may have introduced a systematic difference between the HC and NHC groups. In addition, we found that in multivariate regression, IParea was no longer predictive of HC when controlling for DWI lesion volume. While DWI lesion size may be more predictive for HC, MRI is not always available or feasible for all patients in the initial management period, particularly for patients with large strokes who are susceptible to malignant edema (as shown by our data where patients with deterioration were less likely to have DWI follow-up). Thus, the BBB permeability map might be useful in predicting patients who will develop MMCA especially in light of the result that the CBV (core) lesion area was not predictive of deterioration. Thus, the modified Patlak permeability map uniquely offers novel information over the conventional perfusion CT maps and PCT can be obtained rapidly when the patient first presents to the emergency department.
In conclusion, the IParea on admission PCT might be a useful tool to predict MMCA and need for HC. Given that studies suggest early rather than delayed HC for MMCA is associated with better outcomes,20,46,47 further prospective studies are needed to validate our findings.
ACKNOWLEDGMENTS AND FUNDING
This work was supported by National Institutes of Health (NIH) training grant T32NS04712 and P50 NS04422, the Notsew Orm Sands Foundation, and the Howard Hughes Medical Institute.
Footnotes
Disclosure: The authors have no disclosures.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hesna Bektas, Department of Neurology, University of Texas-Houston Medical School, Houston, TX, USA..
Tzu-Ching Wu, Department of Neurology, University of Texas-Houston Medical School, Houston, TX, USA..
Mallikarjunarao Kasam, Department of Neurology, University of Texas-Houston Medical School, Houston, TX, USA..
Nusrat Harun, Department of Neurology, University of Texas-Houston Medical School, Houston, TX, USA..
Clark W Sitton, Department of Radiology, University of Texas-Houston Medical School, Houston, TX, USA..
James C Grotta, Department of Neurology, University of Texas-Houston Medical School, Houston, TX, USA..
Sean I Savitz, Department of Neurology, University of Texas-Houston Medical School, Houston, TX, USA..
REFERENCES
- 1.Berrouschot J, Sterker M, Bettin S, Köster J, Schneider D. Mortality of space-occupying (‘malignant’) middle cerebral artery infarction under conservative intensive care. Intensive Care Med. 1998;24:620–3. doi: 10.1007/s001340050625. [DOI] [PubMed] [Google Scholar]
- 2.Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. ‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996;53:309–15. doi: 10.1001/archneur.1996.00550040037012. [DOI] [PubMed] [Google Scholar]
- 3.Rieke K, Schwab S, Krieger D, von Kummer R, Aschoff A, Schuchardt V, Hacke W. Decompressive surgery in space-occupying hemispheric infarction: results of an open, prospective trial. Crit Care Med. 1995;23:1576–87. doi: 10.1097/00003246-199509000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Schwab S, Rieke K, Aschoff A, Albert F, von Kummer R, Hacke W. Hemicraniotomy in space-occupying hemispheric infarction:Useful early intervention or desparate activism? Cerebrovasc Dis. 1996;6:325–329. [Google Scholar]
- 5.Schwab S, Steiner T, Aschoff A, Schwarz S, Steiner HH, Jansen O, Hacke W. Early hemicraniectomy in patients with complete middle cerebral artery infarction. Stroke. 1998;29:1888–93. doi: 10.1161/01.str.29.9.1888. [DOI] [PubMed] [Google Scholar]
- 6.Dávalos A, Toni D, Iweins F, Lesaffre E, Bastianello S, Castillo J, for the ECASS group Neurological deterioration in acute ischemic stroke: Potential predictors and associated factors in the European Cooperative Acute Stroke Study (ECASS) I. Stroke. 1999;30:2631–1636. doi: 10.1161/01.str.30.12.2631. [DOI] [PubMed] [Google Scholar]
- 7.Von Kummer R, Meyding-Lamadé U, Forsting M, Rosin L, Rieke K, Hacke W, Sartor K. Sensitivity and prognostic value of early CT in occlusion of the middle cerebral artery trunk. AJNR Am J Neuroradiol. 1994;15:9–15. [PMC free article] [PubMed] [Google Scholar]
- 8.Krieger DW, Demchuk AM, Kasner SE, Jauss M, Hantson L. Early clinical and radiological predictors of fatal brain swelling in ischemic stroke. Stroke. 1999;30:287–292. doi: 10.1161/01.str.30.2.287. [DOI] [PubMed] [Google Scholar]
- 9.Wintermark M, Maeder P, Thiran J-Ph, Schnyder P, Meuli R. Simultaneous measurements of regional cerebral blood flows by perfusion-CT and stable xenon-CT: a validation study. AJNR Am J Neuroradiol. 2001;22:905–914. [PMC free article] [PubMed] [Google Scholar]
- 10.Wintermark M, Reichhart M, Thiran J-P, Maeder P, Schnyder P, Bogousslavsky J, Meuli R. Prognostic accuracy of cerebral blood flow measurement by perfusion computed tomography, at the time of emergency room admission, in acute stroke patients. Ann Neurol. 2002;51:417–432. doi: 10.1002/ana.10136. [DOI] [PubMed] [Google Scholar]
- 11.Lee TY, Functional CT. physiological models. Trends Biotechnol. 2002;20:S3–S10. [Google Scholar]
- 12.Cenic A, Nabavi DG, Craen RA, Gelb AW, Lee TY. A CT method to measure hemodynamics in brain tumors: validation and application of cerebral blood flow maps. AJNR Am J Neuroradiol. 2000;21:462–470. [PMC free article] [PubMed] [Google Scholar]
- 13.Purdie TG, Henderson E, Lee TY. Functional CT imaging of angiogenesis in rabbit VX2 soft-tissue tumour. Phys Med Biol. 2001;46:3161–3175. doi: 10.1088/0031-9155/46/12/307. [DOI] [PubMed] [Google Scholar]
- 14.Roberts HC, Roberts TP, Lee TY, Dillon WP. Dynamic, contrast-enhanced CT of human brain tumors: quantitative assessment of blood volume, blood flow, and microvascular permeability-report of two cases. AJNR Am J Neuroradiol. 2002;23:828–832. [PMC free article] [PubMed] [Google Scholar]
- 15.Lin K, Kazmi KS, Law M, Babb J, Peccerelli N, Pramanik BK. Measuring elevated microvascular permeability and predicting hemorrhagic transformation in acute ischemic stroke using first-pass dynamic perfusion CT imaging. AJNR Am J Neuroradiol. 2007;28:1292–1298. doi: 10.3174/ajnr.A0539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dankbaar JW, Hom J, Schneider T, Cheng S, Lau B, van der Schaaf I, Virmani S, Pohlman S, Dillon WP, Wintermark M. Dynamic perfusion-CT assessment of the blood-brain barrier permeability: first-pass versus delayed acquisition. AJNR Am J Neuroradiol. 2008;29:1671–1676. doi: 10.3174/ajnr.A1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kudo K, Sasaki M, Yamada K, Momoshima S, Utsunomiya H, Shirato H, Ogasawara K. Differences in CT perfusion maps generated by different commercial software: quantitative analysis by using identical source data of acute stroke patients. Radiology. 2010;254:200–209. doi: 10.1148/radiol.254082000. [DOI] [PubMed] [Google Scholar]
- 18.Busto R, Dietrich WD, Globus MYT, Valdes I, Scheinberg P, Ginsberg MD. Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab. 1987;7:729–738. doi: 10.1038/jcbfm.1987.127. [DOI] [PubMed] [Google Scholar]
- 19.Ginsberg MD, Globus MYT, Dietrich D, Busto R. Temperature modulation of ischemic brain injury: a synthesis of recent advances. In: Kogure K, Hossmann KA, Siesjö BK, editors. Progress in Brain Research. Vol. 96. Elsevier Science Publishers; Copenhagen, Denmark: 1993. pp. 13–22. [DOI] [PubMed] [Google Scholar]
- 20.Carter BS, Ogilvy CS, Candia GJ, Rosas HD, Buonanno F. One-year outcome after decompressive surgery for massive nondominant hemispheric infarction. Neurosurgery. 1997;40:1168–1176. doi: 10.1097/00006123-199706000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Delashaw JB, Broaddus WC, Kassell NF, Haley EC, Pendleton GA, Vollmer DG, Maggio WW, Grady MS. Treatment of right hemispheric cerebral infarction by hemicraniectomy. Stroke. 1990;21:874–881. doi: 10.1161/01.str.21.6.874. [DOI] [PubMed] [Google Scholar]
- 22.Kondziolka D, Fazl M. Functional recovery after decompressive craniectomy for cerebral infarction. Neurosurgery. 1988;23:143–147. doi: 10.1227/00006123-198808000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Kalia KK, Yonas H. An aggressive approach to massive middle cerebral artery infarction. Arch Neurol. 1993;50:1293–1297. doi: 10.1001/archneur.1993.00540120010005. [DOI] [PubMed] [Google Scholar]
- 24.Doerfler A, Forsting M, Reith W, Staff C, Heiland S, Schäbitz WR, von Kummer R, Hacke W, Sartor K. Decompressive craniectomy in a rat model of “malignant” cerebral hemispherical stroke: experimental support for an aggressive therapeutic approach. J Neurosurg. 1996;85:853–859. doi: 10.3171/jns.1996.85.5.0853. [DOI] [PubMed] [Google Scholar]
- 25.Forsting M, Reith W, Schabitz WR, Heiland S, von Kummer R, Hacke W, Sartor K. Decompressive craniectomy for cerebral infarction: an experimental study in rats. Stroke. 1995;26:259–264. doi: 10.1161/01.str.26.2.259. [DOI] [PubMed] [Google Scholar]
- 26.Wijdicks EFM, Schievink WI, McGough PF. Dramatic reversal of the uncal syndrome and brain edema from infarction in the middle cerebral artery territory. Cerebrovasc Dis. 1997;7:349–352. [Google Scholar]
- 27.Kucinski T, Koch C, Grzyska U, Freitag HJ, Kromer H, Zeumer H. The predictive value of early CT and angiography for fatal hemispheric swelling in acute stroke. AJNR Am J Neuroradiol. 1998;19:839–846. [PMC free article] [PubMed] [Google Scholar]
- 28.Oppenheim C, Samson Y, Manai R, Lalam T, Vandamme X, Crozier S, Srour A, Cornu P, Dormont D, Rancurel G, Marsault C. Prediction of malignant middle cerebral artery infarction by diffusion-weighted imaging. Stroke. 2000;31:2175–2181. doi: 10.1161/01.str.31.9.2175. [DOI] [PubMed] [Google Scholar]
- 29.Dittrich R, Kloska SP, Fischer T, Nam E, Ritter MA, Seidensticker P, Heindel W, Nabavi DG, Ringelstein EB. Accuracy of perfusion –CT in predicting malignant middle cerebral artery brain infarction. JNeurol. 2008;255:896–902. doi: 10.1007/s00415-008-0802-1. [DOI] [PubMed] [Google Scholar]
- 30.Bisdas S, Hartel M, Cheong LH, Koh TS, Vogl TJ. Prediction of subsequent hemorrhage in acute ischemic stroke using permeabilityCT imaging and a distributed parameter tracer kinetic model. J Neuroradiol. 2007;34:101–108. doi: 10.1016/j.neurad.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Patlak CS, Blasberg RG. Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data: generalizations. J Cereb Blood Flow Metab. 1985;5:584–90. doi: 10.1038/jcbfm.1985.87. [DOI] [PubMed] [Google Scholar]
- 32.Patlak CS, Blasberg RG, Fenstermacher JD. Graphical evaluation of blood-tobrain transfer constants from multiple-time uptake data. J Cereb Blood Flow Metab. 1983;3:1–7. doi: 10.1038/jcbfm.1983.1. [DOI] [PubMed] [Google Scholar]
- 33.Bartolini A, Gasparetto B, Furlan M, Sullo L, Trivelli G, Albano C, Roncallo F. Functional perfusion and blood-brain barrier permeability images in the diagnosis of cerebral tumors by Angio CT. Comput Med Imaging Graph. 1994;18:145–50. doi: 10.1016/0895-6111(94)90023-x. [DOI] [PubMed] [Google Scholar]
- 34.Cianfoni A, Cha S, Bradley WG, Dillon WP, Wintermark M. Quantitative measurement of blood-brain barrier permeability using perfusion-CT in extra-axial brain tumors. J Neuroradiol. 2006;33:164–8. doi: 10.1016/s0150-9861(06)77254-6. [DOI] [PubMed] [Google Scholar]
- 35.Goh V, Halligan S, Bartram CI. Quantitative tumor perfusion assessment with multidetector CT: are measurements from two commercial software packages interchangeable? Radiology. 2007;242:777–82. doi: 10.1148/radiol.2423060279. [DOI] [PubMed] [Google Scholar]
- 36.Lee TY, Purdie TG, Stewart E. CT imaging of angiogenesis. Q J Nucl Med. 2003;47:171–87. [PubMed] [Google Scholar]
- 37.Tofts PS. Modeling tracer kinetics in dynamic Gd-DTPAMRimaging. J Magn Reson Imaging. 1997;7:91–101. doi: 10.1002/jmri.1880070113. [DOI] [PubMed] [Google Scholar]
- 38.Roberts HC, Roberts TP, Brasch RC, Dillon WP. Quantitative measurement of microvascular permeability in human brain tumors achieved using dynamic contrast-enhanced MR imaging: correlation with histologic grade. AJNR Am J Neuroradiol. 2000;21:891–9. [PMC free article] [PubMed] [Google Scholar]
- 39.Yang S, Law M, Zagzag D, Wu HH, Cha S, Golfinos JG, Knopp EA, Johnson G. Dynamic contrast-enhanced perfusion MR imaging measurements of endothelial permeability: differentiation between atypical and typical meningiomas. AJNR Am J Neuroradiol. 2003;24:1554–9. [PMC free article] [PubMed] [Google Scholar]
- 40.Law M, Yang S, Babb JS, Knopp EA, Golfinos JG, Zagzag D, Johnson G. Comparison of cerebral blood volume and vascular permeability from dynamic susceptibility contrast-enhanced perfusion MR imaging with glioma grade. AJNR Am J Neuroradiol. 2004;25:746–55. [PMC free article] [PubMed] [Google Scholar]
- 41.Cha S, Yang L, Johnson G, Lai A, Chen MH, Tihan T, Wendland M, Dillon WP. Comparison of microvascular permeability measurements, K(trans), determined with conventional steady-state T1-weighted and first-pass T2*-weighted MR imaging methods in gliomas and meningiomas. AJNR Am J Neuroradiol. 2006;27:409–17. [PMC free article] [PubMed] [Google Scholar]
- 42.Pluta R, Lossinsky AS, Wiśniewski HM, Mossakowski MJ. Early blood-brain barrier changes in the rat following transient complete cerebral ischemia induced by cardiac arrest. Brain Res. 1994;633:41–52. doi: 10.1016/0006-8993(94)91520-2. [DOI] [PubMed] [Google Scholar]
- 43.Belayev L, Busto R, Zhao W, Ginsberg MD. Quantitative evaluation of blood-brain barrier permeability following middle cerebral artery occlusion in rats. Brain Res. 1996;739:88–96. doi: 10.1016/s0006-8993(96)00815-3. [DOI] [PubMed] [Google Scholar]
- 44.Latour LL, Kang DW, Ezzeddine MA, Chalela JA, Warach S. Early blood-brain barrier disruption in human focal brain ischemia. Ann Neurol. 2004;56:468–77. doi: 10.1002/ana.20199. [DOI] [PubMed] [Google Scholar]
- 45.Aviv IR, D.d’Esterre C, Murphy BD, Hopyan JJ. Hemorrhagic transformation of ischemic stroke: Prediction with CT perfusion. Radiology. 2009;250:867–877. doi: 10.1148/radiol.2503080257. [DOI] [PubMed] [Google Scholar]
- 46.Holtkamp M, Buchheim K, Unterberg A, Hoffmann O, Schielke E, Weber JR, Masuhr F. Hemicraniectomy in elderly patients with space occupying media infarction:improved survival but poor functional outcome. J Neurol Neurosurg Psychiatry. 2001;70:226–8. doi: 10.1136/jnnp.70.2.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hofmeijer J, Kappelle LJ, Algra A, Amelink GJ, van Gijn J, van der Worp HB, HAMLET investigators Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurology. 2009;8:326–333. doi: 10.1016/S1474-4422(09)70047-X. [DOI] [PubMed] [Google Scholar]