Abstract
Background
Success rates with emergent endotracheal intubation (ETI) improve with increasing provider experience. Few objective metrics exist to quantify differences in ETI technique between providers of various skill levels. We tested the feasibility of using motion capture videography to quantify variability in the motions of the left hand and the laryngoscope in providers with various experience.
Methods
Three providers with varying levels of experience (attending physician (experienced), Emergency Medicine resident (intermediate), and post doctoral student with no previous ETI experience (novice)) each performed ETI four times on a mannequin. A Vicon, 16-camera system tracked the 3D orientation and movement of markers on the providers, handle of the laryngoscope, and mannequin. Attempt duration, path length of the left hand and the inclination of the plane of the laryngoscope handle (mean squared angular deviation from vertical) were calculated for each laryngoscopy attempt. We compared inter-attempt and inter-provider variability of each measure
Results
All ETI attempts were successful. Mean (SD) duration of laryngoscopy attempts in seconds differed between experienced 5.50 (0.68), intermediate 6.32 (1.13) and novice 12.38 (1.06) providers (p=0.021). Mean path length of the left hand did not differ between providers (p=0.37). Variability of the plane of the laryngoscope (degrees2) differed between providers: 8.3 (experienced), 28.7 (intermediate) and 54.5 (novice).
Conclusion
Motion analysis can detect inter-provider differences in hand and laryngoscope movements during ETI which may be related to provider experience. This technology has potential to objectively measure training and skill in ETI.
Introduction
Endotracheal intubation (ETI) is a critical procedure that requires significant psychomotor skill. While providers who routinely perform ETI can gain and maintain adequate skill early in their career through many repetitions, paramedics and non-critical care physicians also perform ETI [1–3]. These providers have less frequent opportunities for maintenance of skill and have shorter initial training opportunities [4–7]. Techniques are needed to optimize training, and to assess adequately the psychomotor skill of providers who must perform ETI with low frequency.
Few modalities are available for evaluating procedural skill in trainees who are learning to perform ETI. Typically, proficiency is evaluated through the successes per number of ETI attempts. However this metric has no granularity to detect what aspect of the procedure failed and provides little directive feedback to improve trainee learning. Moreover, it is unsafe to rely on procedure failure as a metric to assess procedural competency when providers move to clinical care. Surveys have been used to assess clinical skills of anesthesia residents but provide little objective data on their procedural competency [1]. Surveys also provide limited opportunities for impactful feedback.
Videography may improve procedure assessment. For example, video laryngoscopy allows for more detailed analysis of ETI variables within the airway including time intervals during ETI [2]. Videography of movements during ETI external to the airway may also provide information about why an ETI attempt was successful or unsuccessful. Motion capture videography uses small reflective markers placed on an object or a subject to track three dimensional movements through a set of calibrated, near-infrared cameras. Detailed and quantitative analysis of sequences of movements can be performed. Motion capture has been used to evaluate kinematics of medical procedures such as intraocular surgery. For example, although novice and expert surgeons have equal success rates, experienced surgeons complete tasks more rapidly, with fewer movements, and with less variability in trajectory [3–6].
We speculate that motion capture can be used to detail the kinematics of ETI technique. Useful measurements for assessing procedural competency would be measurements that differ between providers with different levels of experience. Therefore, in this feasibility study, we quantified the movements of the left hand and the laryngoscope in providers of differing skill level while intubating a mannequin. We sought to identify aspects of the ETI procedure where there was significant inter-provider variability that may be associated with procedural expertise.
Materials and Methods
Study Design
The Institutional review board at Carnegie Mellon University approved this study, and participant provided informed consent for the study. Studies were completed in the Motion Capture Laboratory at the Robotics Institute at Carnegie Mellon University. Participants included one experienced (attending physician with joint appointments in the Department of Anesthesia and Emergency Medicine with over 500 ETI attempts in the clinical setting), one intermediate (resident in Emergency Medicine with 75 ETI attempts in the clinical setting) and one novice provider (post-doctoral student with no previous ETI experience or medical experience). At the beginning of the study, the novice was instructed on the following: proper use of the laryngoscope, clinically relevant airway anatomy and correct insertion of endotracheal tube [7]. The novice was also allowed to practice on the mannequin for 30 minutes prior to the study.
Materials
Intubations were accomplished on the AirMan Advanced Airway Simulator (Laerdal Corp, Wappinger Falls, NY) using a C-MAC video laryngoscope (Karl Storz Corp, El Segundo, CA). The C-MAC uses a traditional #3 Macintosh laryngoscope blade with a video camera adjacent to the light source and digitally records the procedure to a flash memory card that can be retrieved after the intubation for off-line review and can be used as either a direct or video laryngosocpe. The subjects used the C-MAC as a direct laryngoscope. The mannequin was intubated four times by each provider using an 8.0 endotracheal tube and correct placement was confirmed via video review of the C-MAC recordings.
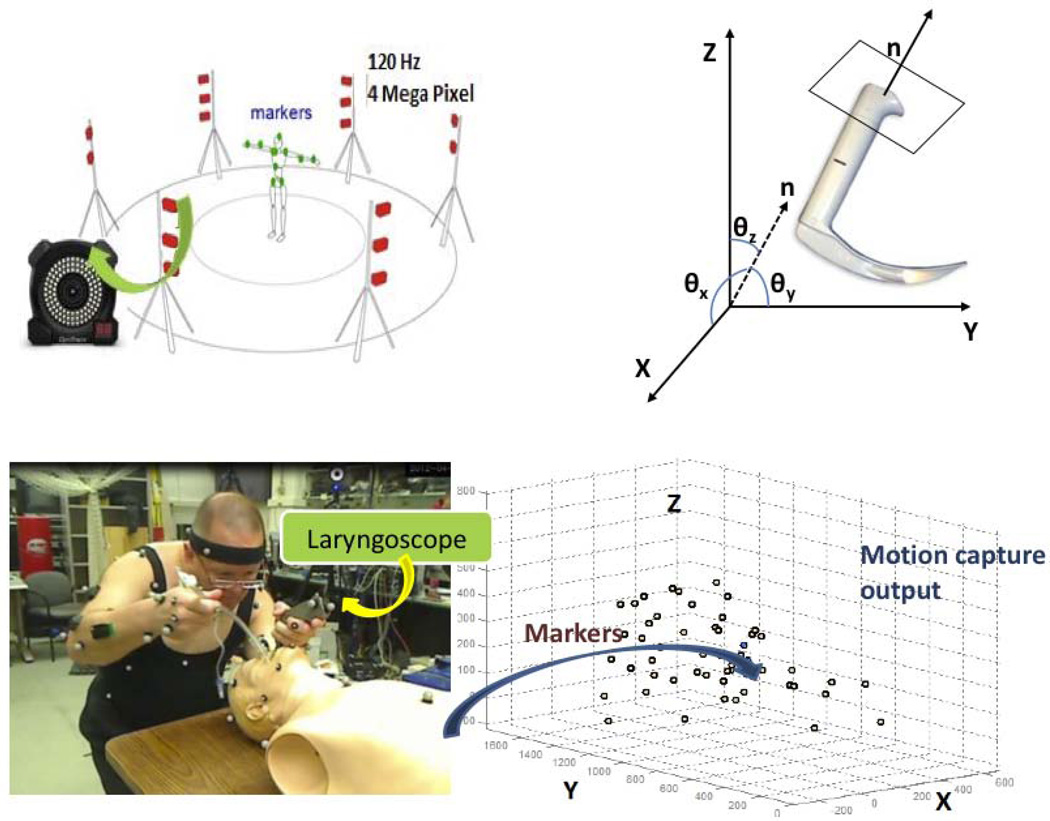
Subjects were outfitted with 50 reflective markers, 14 mm in diameter (Figure 1). Three markers were placed on the handle of the laryngoscope (front, side and back) and 18 markers were placed on the mannequin. We recorded the movement with 16 near-infrared cameras (Vicon Inc, Los Angeles, CA) at a rate of 120 Hz with 4 mega-pixel resolution. This system allowed localization of markers with 1 mm precision. The marker trajectory was reconstructed using Vicon iQ software (Vicon Inc, Los Angeles, CA). The cameras were synchronized and transmitted to a Windows PC via a video synchronization system (MX Giganet, Vicon Inc, Los Angeles, CA). The intubations were also recorded using a traditional video camera synchronized with the motion capture data, for reference during data analysis.
Figure 1.
We used a 16 camera system with 50 markers on the subject (upper left). The reflective markers (tiny white spheres) can be seen on the provider, mannequin and laryngoscope (bottom left). The corresponding marker locations in the 3D space are recorded in C3D format (bottom right). The plane of the handle of the laryngoscope was analyzed from the markers on the laryngoscope (upper right).
Measurement
Each attempt started with the provider placing both hands in the air and clapping three times to correctly identify the beginning of each trial. The laryngoscope started to the left of the mannequin head, lying on its side. This neutral starting position was the same for all providers and identified the reference angle of the laryngoscopic plane. The laryngoscopic plane (LP) was defined as the plane containing the front, side and back markers on the laryngoscope during motion capture. The duration of the laryngoscopic attempt was defined as the time (in seconds) from when the blade of the laryngoscope entered the mouth until the endotracheal tube passed the vocal cords. We calculated the deviation (f(θ))of the normal (n) to the LP as a time series during the entire laryngoscopic attempt, where f(θ) = f ([θx, θy, θz]T) =√(θx2 + θy2 + θz2). As depicted in the Figure 1, θx, θy and θz are the angles made by the LP normal n at any given instant. We defined the inter-trial variability as the variance of f(θ) over multiple trials for each provider.
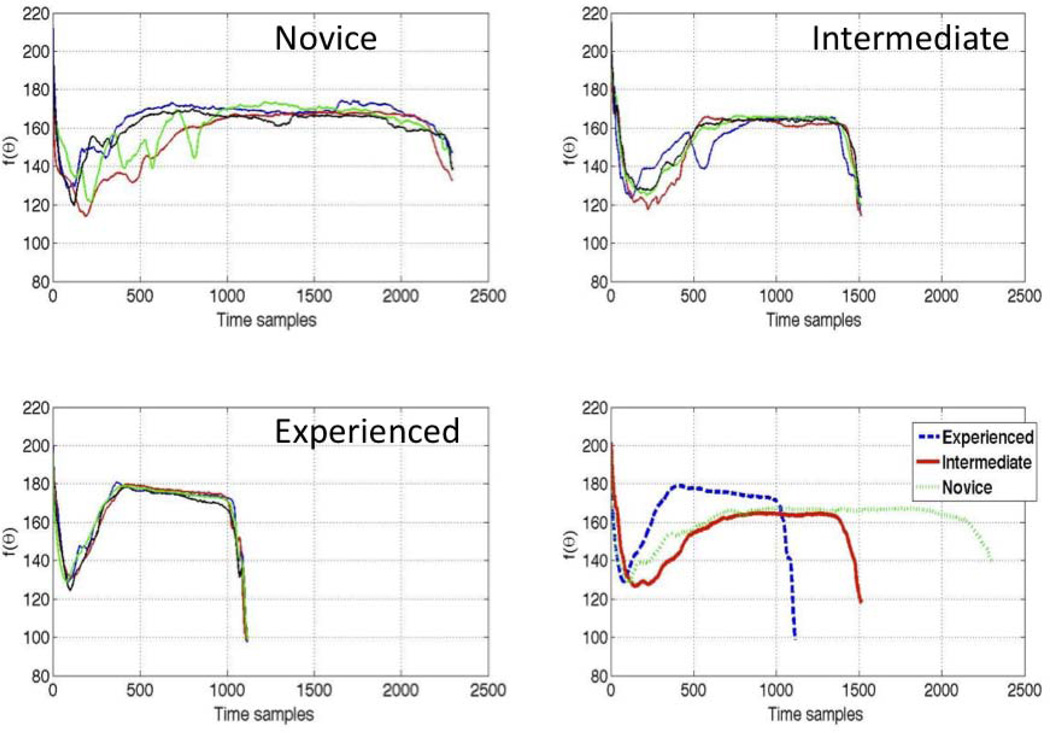
Generalized Time Warping (GTW) was used to align sequences (LP deviation profiles) of different time lengths for individual providers [8]. We computed the average time-warped f(θ) curve (i.e. time series) for the deviation of the LP (i.e. look at how f (θ) varies over time). We defined inter-provider variability as the variance of time-warped f(θ) between the providers.
To perform quantitative comparison between the LP profiles of providers, we transformed the average curves of the LP variation profile using the 40 dimensional Discrete Cosine Transform (DCT) and used Euclidean distances in the DCT space to determine the similarity in the curves between providers [9]. Simply, this signal processing technique determines the components of the curve that define its shape and then calculate the distance between these critical components across different curves (e.g experienced, intermediate and novice). Similar curves have shorter distances (the critical portions of the curves are close to each other in this theoretical space) and dissimilar curves have greater distances. The distance measure D(x, y) is defined as D(x, y) = ‖DCT (x) − DCT(y)‖2 where ‖.‖2 denotes l2 norm or the Euclidean norm. These distances are calculated in a multidimensional model and therefore do not correspond to distances in 3 dimensional space or have units associated with them (i.e an Euclidean distance of 800 does not imply 800mm).
Finally, we compared the average path lengths of the left hand trajectories for each subject during the intubation attempts. We computed the path length (define as L) as where Tstart corresponds to the time when the laryngoscope enters the mouth and Tstop corresponds to the time corresponding to the completion of the intubation.
Statistical Analysis
Continuous variables were described using means and standard deviations. Ordinal variables were described using medians with interquartile ranges. Data were analyzed using ANOVA with the Bonferroni correction when parametric and Kruskal-Wallis when non-parametric. Statistical analysis was accomplished using Stata v. 11 (StataCorp, College Station, TX)
Results
All 12 ETI attempts were successful. Mean duration of laryngoscopy attempt (SD) in seconds was 5.50 (0.68) for the experienced, 6.32 (1.13) for the intermediate and 12.38 (1.06) for the novice provider (p=0.021). Mean path length (in mm +/− SD) of the left hand did not differ between providers: 739 +/−37.9 (experienced), 765 +/− 52.4 (intermediate) and 800 +/− 104.8 (novice), p=0.37.
LP Deviation
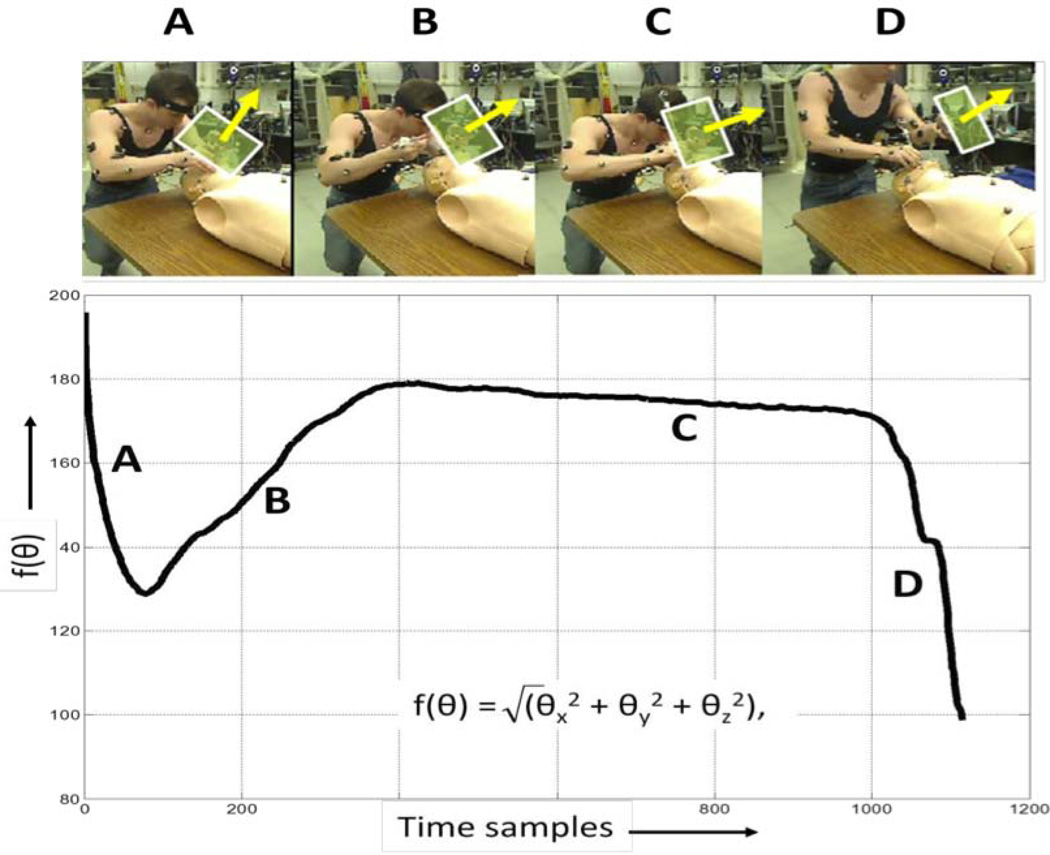
Comparing motion capture data and the concurrent videos, we identified portions of the deviation curves that correspond to steps during ETI (Figure 2). The first falling portion of the curve corresponds to the laryngoscope entering the mouth (2 A). The rising portion corresponds to obtaining the view of the vocal cords (2 B). The plateau corresponds to holding the view constant while placing the endotracheal tube (2 C). The final falling portion represents removal of the laryngoscope after successfully placing the endotracheal tube (2 D).
Figure 2.
The first down sloping portion of the curve corresponds to the laryngoscope entering the mouth (A). The upslope corresponds to obtaining the view of the vocal cords (B). The plateau corresponds to holding the view constant while placing the endotracheal tube (C). The final downslope represents removal of the laryngoscope after successfully placing the endotracheal tube (D). The arrows correspond to the orientation of the laryngoscopic plane.
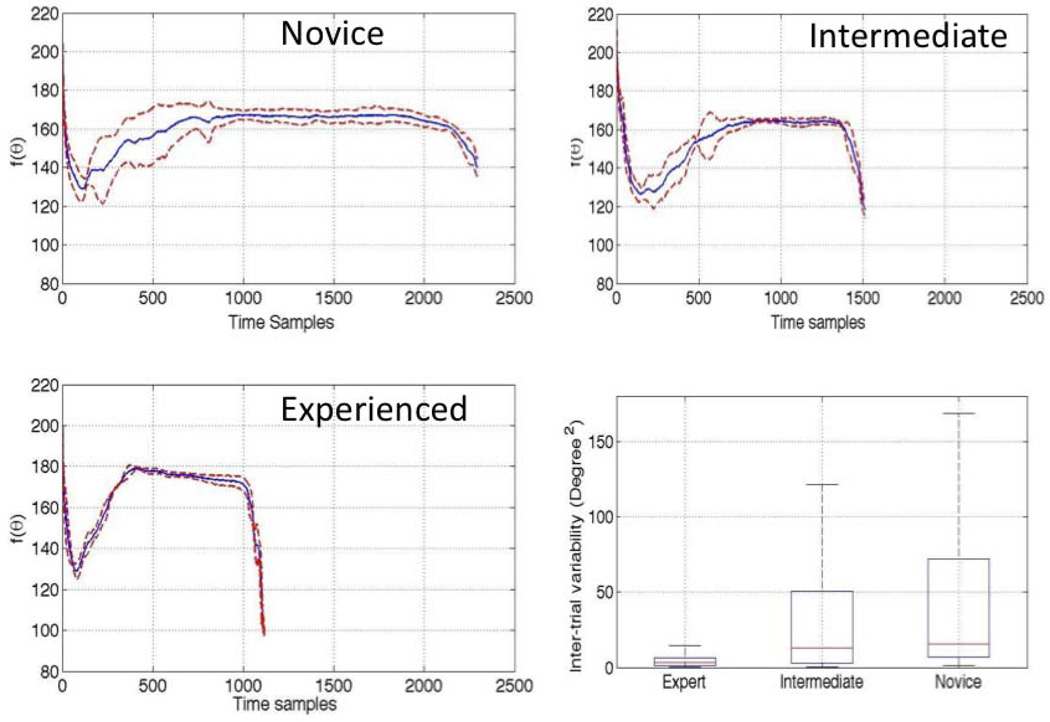
Inter-trial Variability in LP Deviation
The inter-trial variability of the three subjects was compared using the deviations of the LP, measured in degrees2, during intubation (Figures 3). Mean deviation (SD) of the LP, differed between experienced providers: 8.3 (15.2), intermediate 28.7 (33.9) and novice 54.5 (74.3), p<0.0001 (Figure 4). All pairwise comparisons of variability were different (p<0.0001). After transforming the LP variation curves to a 40 dimensional Discrete Cosine Transform, the Euclidean distances between providers were: D(experienced, novice) 2177, D(experienced, intermediate) 547, and D(intermediate, novice) 1740 (Figure 4).
Figure 4.
The variation of laryngoscope orientation for novice (upper left), intermediate (upper right) and the experienced (lower right) providers over multiple intubation attempts showing mean curves (solid line) and the standard deviation (dotted lines). The box plot compares the inter-trial variability between the experienced, intermediate and novice providers (lower right).
Discussion
This study demonstrated how motion capture provides very granular information about the technique of ETI. In very few trials, we were able to quantify the mean path that a provider makes with their left arm to achieve ETI, the duration of the ETI attempt, and the variability in the handling of the laryngoscope. Duration and laryngoscope angle were consistently different between providers with different experience levels. We found the intermediate and experienced providers have similar patterns of laryngoscope movement that are quantitatively distinct from the novice.
Endotracheal intubation is a challenging skill and opportunities for various providers to maintain this skill are limited [10]. As a result, success rates vary significantly by provider experience. However, few objective data are available for discerning the differences in provider technique by experience level. One previous study evaluated the use of force/torque sensors and showed differences in the entry angle of the laryngoscope between novice and experienced providers capture [11]. Motion capture provides more granular details as to the movements, variability and change in angles not evaluated previously. Based on this study, motion capture may allow for quantitative assessment of provider skill. Perhaps of greater impact, motion capture may be useful for developing more high-fidelity simulators and incorporated into training sessions as a way to generate specific, objective feedback to the novice learning ETI.
To our knowledge, this is the first study of ETI using adult simulators and high fidelity motion capture systems. We are aware of one study using wired transmitters to track the motions of the laryngoscope during pediatric mannequin intubations [7], however, motion capture provides more granular detail than these transmitters, allowing for more precise procedural assessment. A video showing the textured detail available from the motion capture output is available at http://emergencymedicine.health.pitt.edu/research/clinical-research/simulation-and-motion-capture.
Rahman et al. showed that experienced ETI providers required greater time and a greater number of movements with a significant amount of “rocking” of the laryngoscope compared to novice providers. The authors hypothesized this “rocking” may have been due to difficulties moving the tongue of the mannequin out of the way and question whether this finding would be experienced in “in the OR with real patients.” Other studies using high fidelity motion capture systems to study other procedures have results similar to our study, where the experienced provider performs the task in less time and with fewer movements [3–6].
The mean path lengths increased from experienced to intermediate to novice but did not reach statistically significant levels. This is consistent with other studies [11] however we did fine a statistically significant difference between the variability of the angle highlighting the granular detail available with motion capture technology. This difference in angle variability without difference in mean path lengths may be analogous to driving a car. When driving from point A to point B (say 200 miles), a novice driver may swerve more while learning to drive than an experienced driver however the distance driven may not be statistically different while the variability would be. Movements of a few millimeters of the handle of the laryngoscope are relatively small changes over the course of the ETI attempt (i.e. they contribute little to the overall path length) however they can have significant changes in the angle resulting in differences in variability without differences in path length.
There are several limitations to this study. First, this demonstration of the feasibility of using motion capture had a very small sample size. Larger studies will be required to determine if the differences between individual providers are actually related to experience level of the provider. Second, this study used a mannequin model, which may not translate completely to ETI on actual patients. Nevertheless, this project identified specific measurements that may be useful in future studies and in developing future high-fidelity simulators. After testing large number of markers and measurements in the simulation setting, the data may allow future studies using motion capture technology during clinical care with more focused and portable instrumentation.
The advent of video laryngoscopy may alter the frequency with which providers perform direct laryngoscopy however, direct laryngoscopy is still taught and practiced by a wide number of specialties and there is still demand for high proficiency with this potentially lifesaving skill. We had no failed ETI attempts in this pilot study. While it is important to provide feedback to providers when unsuccessful, there may also be deficiencies in novice providers even when successful. Motion capture has potential to objectively track these deficiencies. Larger studies will be needed to determine kinematic differences between successful and unsuccessful attempts across a range of provider skills. Finally, there are multiple factors outside of provider experience that impact provider performance with ETI, including patient factors (e.g. body habitus, blood/emesis/secretions in the airway) and environmental factors (e.g. vehicle entrapment). These factors were not considered in this simulation.
Future Directions
Motion capture has the ability objectively track and detail movement patterns. We have shown that these patterns differ between providers of various skill however future work will be need to determine the extent of variability both within and between experienced and novice providers. We look at the movements as a whole. There may be key steps or portions of ETI that distinguish experienced from novice providers. Future studies will be needed to determine if the overall movements or simply key portions of the ETI attempt are different between these groups. As this technology develops, it will be important to develop impactful feedback mechanisms for novice providers learning ETI. Future studies will be needed to determine the optimal method for feedback delivery of ETI deficiencies noted by motion capture to novice providers. These kinetics will also require evaluation across different direct laryngoscopic techniques (macintosh vs. miller blade) and in a variety of airway settings (limited neck mobility, tongue swelling, trismus, etc). Finally, Intubation has two components, glottic exposure and successful passage of the endotracheal tube. Our analysis focused primarly on the movement of the laryngoscope as a surrogate for glottic exposure. Future studies will be needed to analyze the key movements that are required for successful passage of the endotracheal tube such as the way the tube is inserted.
Conclusion
Motion capture can assess attempt duration, motions of the left hand and deviations in the angle of the laryngoscope during ETI of a mannequin between providers of various experience. Motion capture technology can provide granular detail and quantitative descriptions of the ETI procedure that may be useful for research, training, assessment of competency and developing more advanced simulators.
Figure 3.
The variation of laryngoscope orientation for novice (upper left), intermediate (upper right) and the experienced (lower left) providers over multiple intubation attempts (4 trials each). The average curve of LP variations (lower right) for the expert, intermediate and the novice.
Acknowledgments
Financial Disclosure:
Drs. Das, De la Torre and Hodgins are supported by a grant from the National Science Foundation (No. 0931999)
Dr. Callaway is supported by a grant from the National Heart Lung and Blood Institute (1K12HL109068-01) and through a collaborative grant from the Resuscitation Outcome Consortium (5U01HL077871-07)
Dr. Phrampus is supported as a consultant for Karl Stroz Endoskopy who provided equipment for the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at National Association of Emergency Medical Service Physicians Annual Meeting, Tucson, AZ January, 2012
References
- 1.Baker K. Determining resident clinical performance: getting beyond the noise. Anesthesiology. 2011;115(4):862–878. doi: 10.1097/ALN.0b013e318229a27d. [DOI] [PubMed] [Google Scholar]
- 2.Carlson JN, Quintero J, Guyette F, Callaway C, Menegazzi J. Variables Associated With Successful Intubation Attempts Using Video Laryngoscopy: A Preliminary Report in a Helicopter Emergency Medical Service. Prehospital Emergency Care. 2011 doi: 10.3109/10903127.2011.640764. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saleh GM, Gauba V, Sim D, Lindfield D, Borhani M, Ghoussayni S. Motion analysis as a tool for the evaluation of oculoplastic surgical skill: evaluation of oculoplastic surgical skill. Arch Ophthalmol. 2008;126(2):213–216. doi: 10.1001/archophthalmol.2007.62. [DOI] [PubMed] [Google Scholar]
- 4.Saleh GM, Lindfield D, Sim D, Tsesmetzoglou E, Gauba V, Gartry DS, Ghoussayni S. Kinematic analysis of surgical dexterity in intraocular surgery. Arch Ophthalmol. 2009;127(6):758–762. doi: 10.1001/archophthalmol.2009.137. [DOI] [PubMed] [Google Scholar]
- 5.Bann SD, Khan MS, Darzi AW. Measurement of surgical dexterity using motion analysis of simple bench tasks. World J Surg. 2003;27(4):390–394. doi: 10.1007/s00268-002-6769-7. [DOI] [PubMed] [Google Scholar]
- 6.McBeth PB, Hodgson AJ, Nagy AG, Qayumi K. Quantitative methodology of evaluating surgeon performance in laparoscopic surgery. Stud Health Technol Inform. 2002;85:280–286. [PubMed] [Google Scholar]
- 7.Rahman T, Chandran S, Kluger D, Kersch J, Holmes L, Nishisaki A, Deutsch ES. Tracking Manikin Tracheal Intubation Using Motion Analysis. Pediatr Emerg Care. 2011;27(8):701–705. doi: 10.1097/PEC.0b013e318226c7f4. [DOI] [PubMed] [Google Scholar]
- 8.Zhou F, De la Torre F. Canonical Time Warping. Neural Information Processing System. 2009 [Google Scholar]
- 9.Ahmed N, Nataraja T, Rao KR. Discrete Cosine Transform. Ieee Transactions on Computers. 1974;C 23(1):90–93. [Google Scholar]
- 10.Wang HE, Abo BN, Lave JR, Yealy DM. How would minimum experience standards affect the distribution of out-of-hospital endotracheal intubations? Ann Emerg Med. 2007;50(3):246–252. doi: 10.1016/j.annemergmed.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 11.Delson NJ, Koussa N, Hastings RH, Weinger MB. Quantifying expert vs. novice skill in vivo for development of a laryngoscopy simulator. Stud Health Technol Inform. 2003;94:45–51. [PubMed] [Google Scholar]