Abstract
Sub acute sclerosing pan encephalitis (SSPE) is a rare neurodegenerative disorder related to a persistent and aberrant measles virus infection. It is associated with poor prognosis and high mortality. We report a case of a seven- year-old boy who manifested the disease despite proper vaccination and with no documented past history of measles. The case is being reported for its atypical presentation, rarity and its possibility of occurrence in young vaccinated subjects, possibly due to undocumented pre-vaccination measles infection.
Keywords: Subacute sclerosing pan encephalitis, measles, wild type virus, vaccine
Implications for practice
What is known about such cases? Sub acute sclerosing panencephalitis (SSPE) is a rare neurodegenerative disorder related to a persistent and aberrant measles virus infection.
What is the key finding reported in this case report? We report a case of a seven-year old boy who manifested the disease despite proper vaccination and with no documented past history of measles.
What are the implications for future practice? The case is being reported for its atypical presentation, rarity and its possibility of occurrence in young vaccinated subjects, possibly due to undocumented pre-vaccination measles infection.
Background
Sub acute sclerosing pan encephalitis (SSPE) is a devastating progressive inflammatory disorder of the central nervous system (CNS) caused by a persistent infection of the brain by a mutant measles virus. It occurs five to ten years after measles infection.1 The pathogenesis remains enigmatic but the possible factors include defective measles virus (missing the matrix or M protein) which promotes virus propagation within neuronal cells for long periods and an immature immune system.2 Incidence of the disease is 1 per 100,000 to 500,000 measles cases worldwide.3 The incidence is higher in males with a ratio of 2-4:1 females.4 The condition is more common in rural and low socioeconomic populations.5 The disease goes through four characteristic stages, beginning with cognitive and behavioural changes, rapidly followed by myoclonus, choreoathetosis, dystonia, rigidity and a vegetative state. SSPE is a slowly progressing disorder with death occurring within a few months to three years. Since the widespread use of vaccination the incidence of SSPE has markedly decreased but SSPE has been described in patients with no prior history of measles infection and only exposure to the vaccine virus.2
Case details
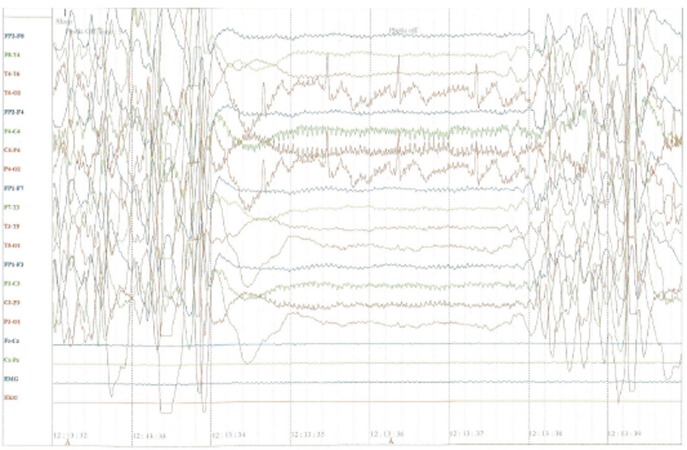
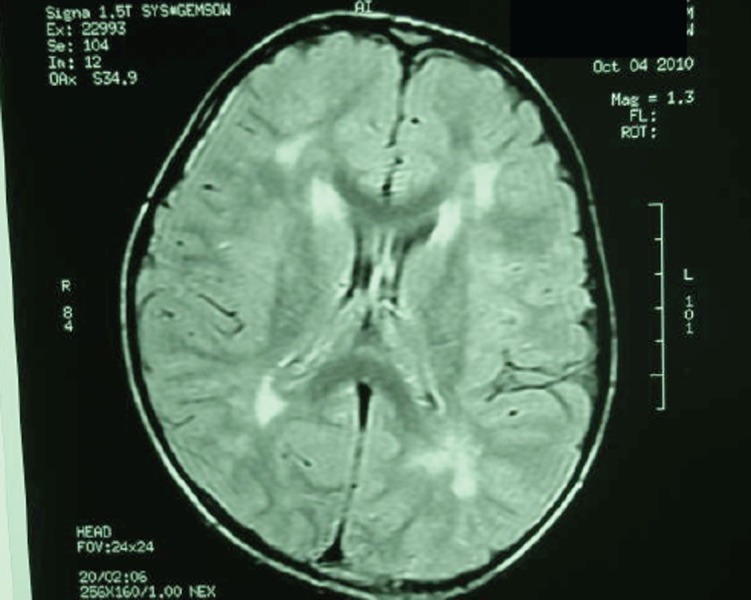
A previously healthy and developmentally normal seven- year-old boy presented with history of behavioural disturbances, decreased attention span and headache which started 18 months ago and was followed by myoclonic seizures, progressively worsening behavioural pattern with associated speech, cognitive and locomotor impairment. The patient also developed bowel and bladder incontinence suggestive of autonomic disturbance. There was no previous history of exanthematous fever, jaundice or vision abnormality. Immunisation history was normal, including vaccination against measles at age nine and measles, mumps and rubella (MMR) at 15 months, with no family background of neurological disorders. Physical examination revealed altered sensorium with Glasgow Coma Scale of 10/15, persistent myoclonic jerks, increased muscular tone, diffuse rigidity and mutism. Meningeal signs were absent and cranial nerves were normal. Other systemic examination including psychiatric evaluation and examination of fundus oculi was normal. Slit-lamp examination excluded the presence of Kayser-Fleischer ring. Our working differential diagnosis was directed to exclude multiple sclerosis, acute demyelinating encephalomyelitis, Hashimoto’s encephalopathy, paraneoplastic limbic encephalitis, lafora disease, mitochondrial diseases and other rare neurodegenerative disorders including SSPE. A complete blood count, erythrocyte sedimentation rate, biochemical parameters including blood sugar, urea, creatinine, electrolytes, lipid profile, liver function tests, copper, ceruloplasmin, antinuclear factor, lactic acid, parathyroid and thyroid hormones were all within normal limits; 24-hr urine copper excretion was also in normal range. Abdominal ultrasonography was normal. Cerebro- spinal fluid (CSF) cytology, biochemistry and microbial analysis were normal but globulin levels were greater than 20% of total CSF protein with raised titres of measles antibodies in blood and CSF. Scalp electroencephalography (EEG) (Figure 1) showed frequent bursts of generalised spikes, polyspikes and sharp wave discharges. Magnetic resonance imaging (MRI) brain (Figure 2) revealed ill- defined irregular areas of altered signal intensity involving white matter of bilateral periventricular, centrum-semiovale and fronto-parietal regions. The patient was treated with valproic acid and isoprinosine along with supportive therapy in the form of passive exercises of all four limbs and care of bowel and bladder for two months in the hospital. In spite of all measures only partial control of seizure activity was achieved and there was no improvement in his behavioural, locomotor and cognitive status. He succumbed to his illness during an episode of generalised seizure resulting in cardio- respiratory arrest.
Figure 1. EEG showing waves and polyspikes.
Figure 2. MRI brain showing periventricular altered signal intensity of white matter.
Discussion
The diagnosis of SSPE can be reliably established if at least three of the following five criteria are met: (a) progressive sub-acute mental deterioration with typical signs like myoclonus; (b) periodic, stereotyped, high voltage discharges on EEG; (c) CSF globulin levels greater than 20% of total CSF protein; (d) raised titres of measles antibodies in blood and/or CSF in the absence of other antibodies, including against Herpes simplex virus (HSV) and Varicella zoster virus (VZV); and (e) typical histopathological findings on brain biopsy or autopsy. Our patient met the first four diagnostic criteria for SSPE, so brain biopsy was not indicated for diagnosis.3 When the disease occurs in immunised children, as in our patient, it is thought to result from a subclinical measles infection that occurred before one year of age, when immunisation usually begins.6 The typical clinical picture of measles may have been altered by the presence of maternal antibodies.7,8 It has also been suggested that the infection in this circumstance may be due to infection by a wild strain, which is not included in the vaccine used.6,9 MRI profile of SSPE includes focal abnormalities in the subcortical white matter early in the course of disease and diffuse cerebral atrophy at later stages of the disease, as observed in our patient.10 Although no treatment has proven effective, pharmacologic management of SSPE can be divided into disease-modifying agents to prolong survival and supportive therapies, the former includes oral Isoprinosine and intraventricular administration of α-interferon and the latter are largely directed at seizure control. Many regimens of antiviral and immunomodulating therapy in SSPE have been described, usually in small, uncontrolled case series.11 In spite of adequate symptomatic and supportive management the reported case succumbed to his illness within two years of becoming symptomatic.
ACKNOWLEDGEMENTS
We thank the patient and his family for giving us the permission and consent to publish this case report. We acknowledge the help of all the medical, nursing and paramedical staff who helped in the care of this patient.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
FUNDING
No sources of funding applicable.
PATIENT CONSENT
- They have obtained written, informed consent for the publication of the details relating to the patient(s) in this report.
- All possible steps have been taken to safeguard the identity of the patient(s).
- This submission is compliant with the requirements of local research ethics committees.
Please cite this paper as: Malik B, Sharma PD, Bhardwaj AK, Sharma A. Sub acute pan encephalitis despite adequate vaccination. AMJ 2012, 5, 7, 359-361. http//dx.doi.org/10.4066/AMJ.2012.1262.
References
- 1.Garg RK. Sub acute sclerosing pan encephalitis. J Neurol. 2008;255:1861–71. doi: 10.1007/s00415-008-0032-6. [DOI] [PubMed] [Google Scholar]
- 2.Wilbert HM. Behrman RE, Kliegman RM, Jenson HB. Nelson Textbook of Pediatrics. 18th. Philadelphia PA: W.B. Saunders; 2007. Measles. [Google Scholar]
- 3.Honarmand S, Glaser CA, Chow E, Sejvar JJ, Preas CP, Cosentino GC, Hutchison HT, Bellini WJ. Sub acute sclerosing panencephalitis in the differential diagnosis of encephalitis. Neurology. 2004;63:1489–1493. doi: 10.1212/01.wnl.0000142090.62214.61. [DOI] [PubMed] [Google Scholar]
- 4.Garg RK, Karak B, Sharma AM. Sub acute sclerosing pan encephalitis. Indian Pediatrics. 1998;35:337–344. [PubMed] [Google Scholar]
- 5.Gascon GG. Sub acute sclerosing pan encephalitis. Semin Pediatr Neurol. 1996;3:260–269. doi: 10.1016/s1071-9091(96)80030-1. [DOI] [PubMed] [Google Scholar]
- 6.Bellini WJ , Rota JS, Lowe LE, Katz RS, Dyken PR, Zaki SR, Shieh WJ, Rota PA. Sub acute sclerosing pan encephalitis: more cases of this disease are prevented by measles immunization than was previously recognized. J Infect Dis. 2005;192:1686–1693. doi: 10.1086/497169. [DOI] [PubMed] [Google Scholar]
- 7.Zinkernagel RM. Maternal antibodies, childhood infections, and autoimmune diseases. N Engl J Med. 2001;345(18):1331–5. doi: 10.1056/NEJMra012493. [DOI] [PubMed] [Google Scholar]
- 8.Albrecht P, Ennis FA, Saltzman EJ, Krugman S. Persistence of maternal antibody in infants beyond 12 months: mechanism of measles vaccine failure. J Pediatr. 1977;91(5):715–8. doi: 10.1016/s0022-3476(77)81021-4. [DOI] [PubMed] [Google Scholar]
- 9.Bellini WJ, Rota JS, Lowe LE, Katz RS, Dyken PR, Zaki SR, Shieh WJ, Rota PA. Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. J Infect Dis. 2005;192(10):1686–93. doi: 10.1086/497169. [DOI] [PubMed] [Google Scholar]
- 10.Anlar B, Saatci I, Kose G, Yalaz K. MRI findings in Subacute sclerosing panencephalitis. Neurology. 1996;47:1278–83. doi: 10.1212/wnl.47.5.1278. [DOI] [PubMed] [Google Scholar]
- 11.Yamani S, Crowell J. et al. Combined oral isoprinosine- intra-ventricular α-interferon therapy for subacute sclerosing panencephalitis. Brain Dev. 1993;15:346–355. doi: 10.1016/0387-7604(93)90120-w. [DOI] [PubMed] [Google Scholar]