Abstract
Estimates suggest that over 350,000 deaths and more than 20 million severe disabilities result from the complications of pregnancy, childbirth or its management each year. Death and disability occur predominately among disadvantaged women in resource-poor settings and are largely preventable with adequate delivery care. This paper presents the substantive findings and policy implications from a programme of PhD research, of which the overarching objective was to assess quality of, and access to, care in obstetric emergencies. Three critical incident audits were conducted in two rural districts on Java, Indonesia: a confidential enquiry, a verbal autopsy survey, and a community-based review. The studies examined cases of maternal mortality and severe morbidity from the perspectives of local service users and health providers. A range of inter-related determining factors was identified. When unexpected delivery complications occurred, women and families were often uninformed, unprepared, found care unavailable, unaffordable, and many relied on traditional providers. Midwives in villages made important contributions by stabilising women and facilitating referrals but were often scarce in remote areas and lacked sufficient clinical competencies and payment incentives to treat the poor. Emergency transport was often unavailable and private transport was unreliable and incurred costs. In facilities, there was a reluctance to admit poorer women and those accepted were often admitted to ill-equipped, under-staffed wards. As a result, referrals between hospitals were also common. Otherwise, social health insurance, designed to reduce financial barriers, was particularly problematic, constraining quality and access within and outside facilities. Health workers and service users provided rich and explicit assessments of care and outcomes. These were used to develop a conceptual model in which quality and access are conceived of as social processes, observable through experience and reflective of the broader relationships between individuals and health systems. According to this model, differential quality and access can become both socially legitimate (imposed by structural arrangements) and socially legitimised (reciprocally maintained through the actions of individuals). This interpretation suggests that in a context of commodified care provision, adverse obstetric outcomes will occur and recur for disadvantaged women. Health system reform should focus on the unintended effects of market-based service provision to exclude those without the ability to pay for delivery care directly.
Keywords: maternal mortality, maternal morbidity, audit, quality of care, access to care, Indonesia, decentralisation, health systems
In 2010, for the first time since measurement efforts began in the late 1980s, a decline in maternal mortality was detected at the global level. Two independent groups estimated that, in 2008, approximately 350,000 deaths occurred as a result of pregnancy, childbirth, or its management (1, 2). Previously, global estimates indicated a higher and relatively static level of approximately 550,000 deaths per annum (3–6). In 2012, new data were published suggesting further reductions, with 287,000 maternal deaths estimated globally (7).
Despite this encouraging evidence, maternal mortality statistics are characterised by uncertainty and imprecision. Measurement is subject to technical and operational difficulties (underreporting, misclassification, incomplete vital registration and health information), and statistical modelling is often necessary (8). Moreover, even if the decline represents a real trend, the rate of reduction is likely to be slower than is necessary to meet the Millennium Development Goal (MDG) for maternal health (2).
Maternal mortality is a social phenomenon. Over 99% of deaths occur in resource-poor settings, and within (both rich and poor) countries, higher mortality is consistently recorded among disadvantaged groups (9) (2). In addition to mortality, over 20 million women suffer illness and long-term disabilities every year as a result of complications of pregnancy and childbirth (10).
Furthermore, maternal death and disability have social and economic consequences. These include the immediate and long term costs of care, sales of assets, loans and debt (11), losses in economic productivity (12), stigma and social isolation caused by conditions such as obstetric fistula (13), depression, psychological illness (14), infertility (15), the disintegration of families, and the loss of care and education for infants (16).
In 1987, the Safe Motherhood Initiative (SMI) drew attention to the hitherto neglected issue of maternal health (17). SMI recommended preventative, holistic and familial approaches, as part of a broader sexual and reproductive health strategy (18). A decade later, despite every world region having developed a safe motherhood strategy, policies and programmes that adhered to the SMI agenda proved difficult to operationalise and sustain (19).
In response, two community-based interventions were prioritised. These were antenatal care (ANC) with risk screening, and the training of traditional birth attendants (TBAs) in safe delivery practices. Despite their initial endorsement, support for these strategies declined as evidence grew that most maternal deaths occur among healthy women who have received prenatal care, and that every delivery should occur in the presence of a skilled health professional (20).
Support for skilled birth attendance (SBA) grew towards the end of the 1990s based on clinical, historical, and observational evidence (21–26) At the same time, a package of medical interventions delivered in hospitals and health facilities and directed at the intrapartum period, termed emergency obstetric care (EmOC), was identified by WHO, UNICEF and UNFPA. EmOC treats the complications thought to be responsible for the majority of deaths at the time that they occur (27, 28). Monitoring availability, utilisation and performance of EmOC facilities is a key part of the strategy (29).
In 2000, the improvement of maternal health was prioritised in its own right as part of the MDGs, a series of internationally ratified goals to reduce poverty and improve education and health (30). Targets were associated with each goal. For maternal health, the targets are a 75% reduction in the 1990 levels of maternal mortality, and universal access to reproductive health by 2015 (31). Indicators for measuring progress towards the maternal mortality target are the maternal mortality ratio (MMR) and, due to the problems with measurement, the proportion of births attended by health personnel. The MDGs, combined with the policy messages of SMI and other groups (32) effectively endorsed intrapartum care as a central strategy for maternal mortality reduction.
Despite political advocacy and academic consensus regarding the content and efficacy of SBA and EmOC, equivalent knowledge on equitable provision is lacking. Recently, scholars have identified that the ‘implementation of maternal health services on the ground has been woefully neglected in the safe motherhood community’ (33) (p. 1384) and that implementation solutions are now required (34).
Aims
The research responded to this call. The overarching aim was to develop methods to inform the organisation and delivery of life-saving delivery care. The objectives were to describe and explain access to, and quality of, care in obstetric emergencies in rural areas through critical assessments of adverse outcomes derived from user and provider perspectives.
The empirical work was guided by a core premise that implied a particular methodological approach. This related to the analytical potential of the subjective perspectives of those for whom delivery care has direct relevance (those who provide and use it). The research had substantive and methodological outputs. This article presents the substantive findings and policy implications; a separate paper describes the methodological issues (35). The empirical studies and research questions are set out in Table 1.
Table 1.
Empirical studies and research questions
| Study | Perspective from which care examined | Research questions |
|---|---|---|
| 1. A confidential enquiry into maternal mortality and severe morbidity | Healthcare providers |
|
| 2. An extended verbal autopsy to investigate maternal deaths | Final caregivers |
|
| 3. A community-based review of maternal mortality and severe morbidity | Women of reproductive age and community members (families, village officials, TBAs and midwives) |
|
Study setting
The research was undertaken in two rural districts in Banten province on the island of Java, Indonesia. Indonesia ranks sixth in the world in numbers of maternal deaths (9,600 in 2010) (7). In 1989, in accordance with global advocacy for SBA, the Government launched the Bidan di Desa (midwife in the village) programme to post a qualified midwife in each of the country's 68,000 rural villages (36).
Training and deploying large numbers of midwives characterised the early years of the programme. Nursing graduates received one year of training, and originally had the authority to manage only normal deliveries. Because the rural villages in which midwives practise demand high levels of autonomy, however, the Government has recently extended midwives’ responsibilities, allowing them to perform life-saving functions. Competency-based in-service training has also been introduced (37).
Qualified midwives receive government contracts that reduce their public salary incrementally over 3–6 years. Over this time, midwives are expected to remain in villages and develop private practices (38). The potential of this remuneration mechanism to act as a disincentive to treat the poor has been observed, as have problems of social isolation, and retention in remote villages (39, 40).
Making Pregnancy Safer (MPS) is a WHO health sector initiative to reduce maternal and perinatal morbidity that was translated into national policy in Indonesia in 2000. The MPS Strategic Plan has four elements:
Improve access to and quality of obstetric and neonatal services;
Develop partnerships between sectors, programmes and other parties;
Facilitate empowerment of women and families for healthy behaviours and care utilisation, and
MPS is delivered through various programmes, including PONED and PONEK. PONED (Pelayanan Obstetri dan Neonatal Emergensi Dasar) is basic emergency obstetric and neonatal care and PONEK (Pelayanan Obstetri dan Neonatal Emergensi Komprehensif) refers to comprehensive emergency obstetric and neonatal care.† Health centres with beds provide PONED, and district and provincial hospitals provide PONEK. Each sub-district has at least one health centre, and various public, private, military and religious groups administer hospitals (43).
The village midwife programme, MPS, PONED and PONEK represent sustained state commitments to the provision of SBA and EmOC. Although reductions in neonatal mortality and improvements in child health have been attributed to the village midwife programme (44, 45), its effect on maternal mortality is difficult to determine.
MMR appears to be in decline in Indonesia, falling from an estimated 650 maternal deaths per 100,000 live births in 1990 (3), to 228 in 2008 (46). Recent sub-national estimates, however, have been reported as high as 621 in remote and rural areas (47), with extremely high levels of 2,303 detected among poor women delivering in hospitals (48).
In addition, two thirds of all deliveries still occur in the home (49), and poor women have been observed to be seven times less likely to have access to professional delivery care (48). These data suggest that the equitable provision and uptake of delivery care remain relevant issues for poor and rural women in this context.
Methods
Study 1: a confidential enquiry into maternal mortality and severe morbidity
If, as the evidence suggests, SBA, and EmOC have the potential to reduce avoidable mortality and morbidity, then the quality of this care can be regarded as a necessary condition for success. This was the rationale for adopting QOC as an initial area of study. Quality assessment (QA) in healthcare typically focuses on technical and clinical elements of care (50). More recently, conceptualisations of QOC (and QA) have broadened to incorporate interpersonal, organisational, and societal elements of care (51–53).
Study 1 was an adapted confidential enquiry assessing QOC. Confidential enquiries identify and address substandard care provision in adverse maternal and child health (MCH) events (54–56). Three adaptations were made to the traditional approach. Firstly, cases of severe obstetric morbidity (‘near-miss’) were reviewed as well as cases of maternal death. Near miss is a more common outcome than death, and allows exploration of a wider range of outcomes (57). Secondly, favourable (as well as substandard) factors were assessed to foster constructive accountability, and address the punitive nature often associated with clinical audit (58). Finally, qualitative interviews with individuals involved in the emergencies were the basis of the assessments in place of medical records. This step was taken due to the focus of the research on subjective perspectives, and due to a lack of complete health records at village level.
Sixteen cases, identified from existing sub-district registers and in facilities, were selected to represent a range of delivery complications and outcomes. For each case, in-depth interviews were conducted with the woman (if she survived), her family, community members and health providers. The interviews focussed on background characteristics of the woman, the onset of the delivery complication, delivery attendance, referral to, and care inside a facility (if this occurred).
Two segregated panels of community midwives and obstetrician/gynaecologists were recruited to evaluate the cases (as represented in the interviews) in a series of weekly meetings. The meetings were based on a structured case assessment framework in which QOC was considered in terms of the technology and application of care, and in terms of its institutional and social distribution.
Study 2: an extended verbal autopsy to investigate maternal deaths
The second empirical study examined access to care. Theoretically, access can be considered as a negotiation, representing the interplay between the needs, perceptions, and behaviours of individuals, and the responsiveness of the health system towards these (59–61). Contemporary theory considers access to care as a dynamic and relativistic process, as a phenomenon of the disadvantaged (62), and as a core component of the human right to health (63).
Study 2 was an adapted verbal autopsy (VA) survey. VA is a method to investigate mortality in populations where deaths occur outside health facilities, or without proper registration (64). VAs are structured interviews with final caregivers(s) (65) to establish a medical cause of death (COD) (66). VAs can also be used to investigate underlying and contributory factors (67). VA does not depend upon vital registration and health information systems, and so is responsive to contexts where deaths occur outside facilities. The methodological debates relate to standardising the VA interview and data interpretation method to generate COD data amenable to cross-national comparison and analysis (65), and applying the method to investigate the social situations surrounding deaths (68).
Study 2 sought to elicit the perspectives of relatives of women who had died during pregnancy or childbirth. Extended VA interviews were conducted with close relatives of 104 women who died during pregnancy or delivery or within six weeks of a pregnancy ending, who either had no contact with health services at the time of death, or for whom case notes and/or medical records were not available. The cases were selected from an earlier survey in the province to reflect the cause-specific profile previously detected (48).
The interviews collected information on medical signs and symptoms of the deceased based on the standard VA instrument (65) and, through an extended section, on circumstances and events surrounding the deaths, and on preventability and cause. The extended section was semi-structured and invited free narrative. The three-delays framework of delayed treatment in delivery emergencies (69), the ‘candidacy’ concept of access to care (62) and an analytical framework derived from the right to health (70) were used analyse the narratives.
Study 3: a community-based review of maternal mortality and severe morbidity
Study 3 was a community-based evaluation of both quality of, and access to, care in obstetric emergencies. The study engaged people typically involved in obstetric emergencies in villages to conduct participatory assessments of care, and to generate recommendations for reform.
Evidence for participatory, community-based interventions for MCH is converging (71–75). Despite this however, a distinct lack of conceptual, implementation and evaluatory coherence exists for community participation in health (CPH) (76). Scholars have also asserted that CPH is not simply an intervention, but instrumental and substantive, a dynamic and interchangeable means and end (77). Given its nature, contextualised documenting of participatory practices has been called for, to identify and share practical experiences (78).
Study 3 sought to identify issues that communities themselves identified as relevant in the provision of delivery care in villages. The study also documented the participatory process according to theoretical and planning frameworks of CPH (76, 77). Six cases were selected from Study 1, and four independent groups of formal and traditional village health providers, families, village leaders and women were convened. The groups participated in a series of weekly meetings, conducting semi-structured case assessments based on the three-delays framework (69). Discussions were conducted according to the focus group discussion (FGD) method (79).
Data analysis
A qualitative approach to data collection and analysis was appropriate given the central assertion regarding subjective perspectives. Qualitative research subscribes to distinct ontological, epistemological and methodological assumptions. These include that reality and the nature of knowledge are subjective, multiple and socially constructed (80), implying the use of methods such as in-depth interviewing and FGDs that seek to understand perspectives and meanings as they are situated in particular contexts.
In all three studies, interviews and FGDs were audio-recorded, transcribed verbatim, and translated from Bahasa Indonesian and indigenous languages of Sundanese and Javanese into English for analysis. The InterVA method of interpreting VA interview data (66) was used to determine medical CODs in Study 2. In Studies 1 and 3, completed and translated case assessment frameworks were also analysed. In all studies, observational field notes were also taken and analysed. Otherwise, the analysis was based on an adapted (combined inductive/deductive) framework analysis approach (81) that involved a series of analytical steps of increasing abstraction from data to findings and theories (Table 2).
Table 2.
A combined inductive/deductive framework analysis approach [adapted, (81)]
| Stage | Description |
|---|---|
| 1. Immersion and organisation | An initial organisation of data according to pre-determined (deductive) categories, as well as to preliminary emergent (inductive) themes |
| 2. Development of coding frameworks | The development of thematic, or coding frameworks that resulted from Stage 1 |
| 3. Application of coding frameworks | The thematic frameworks applied to data to code or index. This is done iteratively, until no new themes emerge (‘thematic saturation’) |
| 4. Preparation of thematic summary grids | Preparation of thematic summaries, whereby grids of dominant and recurrent themes prepared with related themes and sub-themes in columns and respondents (or groups of respondents) as rows. This allows large volumes of narrative data to be distilled, and for the identification of patterns within and between narratives |
| 5. Interpretation | Interpretation involves establishing associations between themes to construct sequentially descriptive and explanatory accounts of the phenomena of interest. Additional, relevant theoretical frameworks can be applied at this stage |
NVIVO software was used to support data management, coding analysis and in the construction of coding frameworks (82). Data analysis was conducted in parallel to, and following completion of, the data collection to allow preliminary findings to influence subsequent data collection. Similarly, the research questions, areas of empirical interest, and methods were sequential and iterative. They were not constructed a priori, allowing the experiences and findings of Study 1 to inform the development of Study 2, and so on, in a stepwise manner.
Ethical considerations
Informed consent was sought from all participants. Participants were informed of the purpose of the studies, and on the risks and benefits of participating. Participants were also assured that taking part would have no bearing on the healthcare available to themselves or their families, and that they could leave the studies at any time and for any reason. Participants were assured anonymity and were reimbursed (with money or a token gift) for their time. Institutional ethics committees at the Universities of Indonesia and Aberdeen (UK) also reviewed and approved all study protocols.
Results
In Study 1, assessing QOC, the panellists quickly established that village midwives were not available in the emergencies. Other midwives present in villages, or nearby, who were available by virtue of circumstance or chance, typically attended. Attending midwives made many important contributions: diagnosing conditions, stabilising women, convincing families of the need for referral, and facilitating admissions to facilities. Some clinical management competencies were found to be substandard, however.
In Study 1, strong preferences for TBAs were also identified among women and families, as was poor knowledge of social health insurance (SHI). Otherwise, communities were not collectively prepared for emergencies, but actively participated in mobilising resources when they occurred. In facilities, shortages in blood supplies for transfusions were common, and blood, others medications, and care, were often unavailable. As a result, tertiary care was often sought in more than one location (83).
In three of the cases selected for Study 1, the woman had not made contact with care in the acute situation. These cases were excluded from the enquiry because the panellists felt that there was no care to assess. The excluded cases were all deaths that had occurred in the home, with TBA assistance, and all from postpartum haemorrhage.
Although the decision to exclude these cases was not challenged (so as not to compromise panellists’ ownership over the process), it highlighted a potential for the systematic exclusion of certain (more severe) circumstances and events from QA enquiries. And (assuming QA influences health service organisation and delivery), the potential for resulting services to become inadvertently configured to maintain the exclusion of particular groups, by failing to account for and address their needs.
As a result, and based on the findings suggestive of the determining effects of events that occur outside facilities, access to care was considered in its own right in Study 2.
In Study 2, over 70% of respondents reported delays in seeking, reaching and/or receiving care. When unexpected complications occurred, families were often unprepared, TBAs were usually called, and midwives were generally unavailable. The financial costs of care were identified as highly influential. Most families had serious concerns about the costs of midwifery and hospital care. Since most were also uninsured and uninformed about SHI, arranging it in the acute situation was often complicated and time-consuming. In addition, transport was often unavailable and unaffordable. Where they were used, ambulances were reportedly unstaffed and ill-equipped.
Serious barriers to access were also identified inside facilities. Difficulties related to the admissions of women with SHI, partially arranged SHI, or no insurance, and no ability to pay were frequently recounted. Facilities were also reported as inadequately staffed and equipped, and shortages of crucial supplies such as blood products were again apparent. Many families had to embark on additional journeys (and pay associated costs) to locate and purchase medications and/or blood. Several second referrals that incurred further delays were also reported. Referral was less favourably reported in Study 2; midwives were described as poorly equipped, and several did not accompany women to hospitals (84).
In terms of CODs, Study 2 revealed that pregnancy-related sepsis accounted for 28% of the deaths (associated conditions included genital tract sepsis and indirect infectious causes, e.g. typhoid). Haemorrhage and malaria accounted for 3 and 8%, respectively. Small proportions were attributed to pregnancy-induced hypertension (4%), unsafe abortion (2%), and obstructed labour (2%). The apparent burden of infectious disease (of obstetric and non-obstetric origin) including HIV, malaria, TB, and pregnancy-related sepsis was considerable, accounting for over 40% of the deaths.
Infectious causes can have long durations of onset, potentially requiring several presentations for care, incurring direct and indirect costs for women and families several times over. If serious and multiple barriers to access exist, then these may be encountered several times over for the treatment of infectious diseases. Haemorrhage, by contrast, has a rapid onset and can be fatal without prompt treatment (85). Timely diagnosis and treatment of the main CODs depends upon available services, albeit in different ways, underscoring the necessity of a functioning referral system to ensure access to life-saving care.
In Study 2, the extended interviews also yielded information on culturally-derived systems of explanation, causation and behaviour. Some respondents described delivery complications in terms of curses or supernatural forces, and most attributed the deaths to fate, destiny or God's will. Examination of these perspectives revealed a simultaneous recognition of the failures of the health system among family members, coupled with fatalism and passivity regarding the deaths. This may have been a consequence of families’ inability to question systems of authority, and/or due to feelings of powerlessness in the face of multiple barriers to access (86). Otherwise, the theoretical framework derived from the right to health identified that none of the essential elements of the right were upheld (87).
The narratives gained in Study 2 offered complementary insights into care and outcomes, and revealed marked differences between the explanatory frameworks of service users and providers. This suggested that broader empirical frameworks, examining the socio-economic and cultural landscapes in which healthcare is situated and sought from a range of stakeholder perspectives could potentially provide more robust interpretations of complex health problems. This informed the development of a participatory, community-based review of care in obstetric emergencies in the third and final study, in which service users and providers collectively assessed care. The three cases excluded from Study 1 were also included in Study 3.
A repeated and persistent theme in the community assessments (Study 3) related to ‘poor care for poor people’, and, in particular, problems with SHI. Here, SHI was often viewed as instrumental in constraining access to quality care. Problems included bureaucratic and complex administration, inequitable and incomplete distribution, and a pervasive lack of knowledge regarding SHI entitlements and how to use it in an emergency. Study 3 also revealed that women using SHI in facilities were explicitly discriminated against, often refused entry and/or treated with hostility and contempt. As a result, several women discharged themselves from hospital early, or before treatment was complete, to avoid the poor QOC, as well as spiralling costs (88).
The participatory approach yielded rich and explicit assessments, and multi-level explanations of care and outcomes, relating individual perceptions and behaviours to broader contextual features. For example, the preferences for TBAs previously identified were attributed to factors related to tradition, availability and cost, which when combined, resulted in the ‘dominance’ of TBAs as the first choice of delivery provider. Study 3 also revealed that TBAs and midwives fail to collaborate due to their having competitive roles in the market for MCH care in villages, and that hospitals discriminate against poor women in critical conditions due to the resource implications of providing care.
Theoretical frameworks of CPH conceive of a continuum of passive to active participation, and in terms of approaches that foster agency versus responsibility. Analysis of the discussion narratives according to these frameworks helped to document key features of the process: that participation was complex and dynamic, and changed considerably over the course of the study (89). Study 3 also suggested that CPH configured to foster agency (political resourcing) may provide a means to enable individual responsibility.
Studies 1–3 yielded a range of critical perspectives that triangulated, at times converging (validating) the findings. At other times divergent views served to provide a more complete picture of the phenomena under investigation. In general, despite state provisions for delivery services, care in obstetric emergencies was seen to be predominately available on a fee-for-service basis. In a context of poor and uninsured patients, this led to difficult decisions for women, families and providers in medical emergencies, balancing the costs of care against the likelihood of a positive outcome. The multitude of delays incurred added a further constraint whereby, as the woman's condition deteriorated, higher levels of care that were more expensive were required further intensifying the cost/payment issues. Where they could be made, payments often secured only sub-optimal, and in some cases downright discriminatory care.
Discussion
Recommendations for policy
The SHI system, designed to reduce the catastrophic effects of costs of care for poor people, urgently requires reform to extend entitlements and to improve coverage, distribution, knowledge, awareness and use among poor and vulnerable women and families. Given the problems with coverage and utilisation, health facilities should also be staffed and resourced to cater for those without the ability to pay for care directly.
Ensuring adequate numbers of village midwives, and providing them with the resources and training for effective coverage is also implied. Midwives should be encouraged to work more closely with TBAs, as a mechanism to reach women typically excluded from professional delivery services, and to be provided with incentives to accept and treat women without the ability to pay directly.
A network of over one million volunteer community health workers (CHWs) exists in Indonesia (94). This cadre represents a unique human resource with the potential to mediate linkages between poorer women and healthcare. Many of the recommendations could be effectively implemented by capitalising on this cadre of provider to broker the relationships between TBAs, women and midwives.
Given the critical roles they played in the emergencies, and considering the influence of cultural constructions of health and illness families should be provided with information for, health promotion, birth preparedness, emergency readiness, and particularly health insurance.
More broadly, the analysis suggests that the root causes of adverse outcomes relate to the operating conditions of health system. In Indonesia, the health system is characterised by decentralisation. Implemented in the late 1990s following the Asian economic crisis, decentralisation was heavily influenced by the World Bank and International Monetary Fund, whose rescue packages were conditional on the deregulation and privatisation of public services (43), imposing the ideology of the free market on healthcare (95).
Decentralisation seeks to build local governance by devolving political and economic power from central to district level (96–98). Although the efficiency gains of decentralised management have been described (99), many problems have also been observed. These relate to insufficient revenue at central level to fund both district-level governance and repay national debt, and the absence of an adequate legal framework for central control. At district level, insufficient institutional capacity, conflicts between local elites, a lack of transparency and accountability, pervasive corruption and self-interest have also been documented (43, 99, 100).
Moreover, under decentralisation, it has become necessary for hospitals and health facilities to generate sufficient capital to cover operational costs, and district governments rely on them for revenue (101, 102). Decentralisation has also been characterised by increased numbers of private insurers, the privatisation of public services and reductions in public health spending (43, 103–107), as well as withdrawal of support and resources for CHWs (108, 109).
A converging corpus of research suggests that decentralisation, and a move towards a market-based healthcare, may introduce multiple barriers to access that arise from the financial costs (commodification) of care. Kristiansen and Santoso describe a distinctly negative experience of decentralisation as a means to liberate a market economy in the health sector in Latin America:
The dominant results of privatisation and deregulation of health services in Latin America, as documented in numerous reports, are rampant, unethical behaviour of health insurers and multiple neglect and exclusion of poor people, especially in remote areas. (43) (p. 252)
Decentralisation grants districts full autonomy and authority for health and welfare, but may have overlooked the administrative capacities of districts. Critical views point to the lack of any real power and control at the village governance level, as well as a direct withdrawal of funding from district health authorities.
Decentralisation should seek to account for the connectivity between central, district and village levels for the provision of services, the extent of effective coverage, and the protection of the poor from its costs. The final recommendation therefore relates to a focus on the health system as an overall mechanism within which the recommendations can be situated to ensure the equitable provision of emergency delivery care (Table 3). Specific recommendations were developed and disseminated from each study (90–93).
Table 3.
Recommendations for policy
| Human resources |
|
| Community-based care |
|
| Facility-based care |
|
| Financial access |
|
| Health systems |
|
Conceptualising quality and access
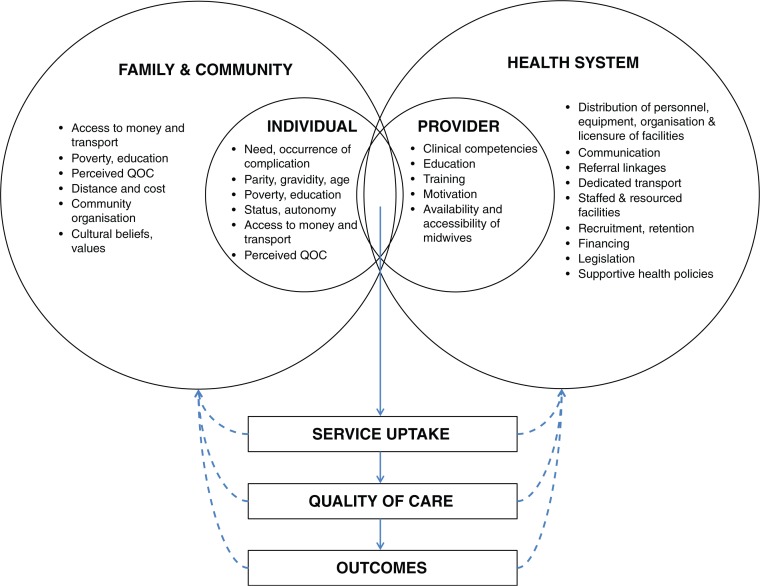
The research also sought to contribute to the theoretical debates on quality and access. Contemporary debates conceive of QOC as a multi-dimensional construct, comprised of social, organisational, interpersonal, technical and clinical elements. Study 1 suggested that these dimensions can be reconciled by considering QOC as an event that occurs when users and providers interact, and that this interaction is embedded within broader social and health systems contexts (Fig. 1). This conceptualisation adopts a dynamic view of Donabedian's structure-process-outcome QA model (53), examining actions and interactions, whilst considering the influence of context. The conceptualisation also adheres to the relativistic model proposed by Chin and Muramatsu (52).
Fig. 1.
A conceptual model of quality of care (83). The model posits that QOC is an event that occurs when service users (represented by left innermost circles) and providers (right innermost circles) interact. Determining this interaction are broader factors related to the sociocultural and health systems environment (examples are provided in the left and right outer circles, respectively). These factors individually and collectively determine the uptake of services. QOC occurs when services and utilized, and outcomes result. Outcomes, QOC and uptake also operate through feedback mechanisms to their determinants.
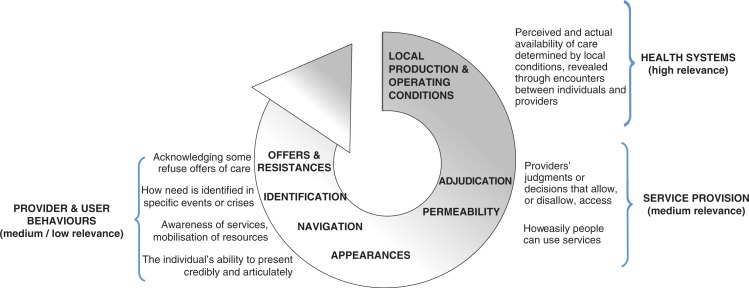
Study 2 applied the VA method to investigate access to care as a necessary condition for QOC to occur. Study 2 revealed the extent of financial in-accessibility of emergency delivery care. The semi and unstructured narratives revealed a further effect whereby the perceptions, attitudes, and behaviours of individuals reciprocally maintained these exclusionary conditions. Theoretical debates on access to care conceive of the concept as an interaction between users, systems, and services (60–61, 110). Study 2 suggested that this interaction may be structurally determined by the operating conditions of the health system and reciprocally maintained through the actions of individuals (Fig. 2). This develops Frenk's notion of ‘resistances and impediments’ to access that arise from healthcare resources themselves (61).
Fig. 2.
A conceptual model of access to care (62, 86). Elements of the eligibility to access concept (62) were applied to the thematic analysis of the narratives gained in Study 2. The analysis revealed a hierarchical arrangement of the relevance of the dimensions of access, whereby the organisation of health systems dictates service provision, and provider and service user behaviours, i.e. the locus of control over eligibility for access to care, lies within the macro-level operating conditions of the health system. A reciprocal effect was also identified whereby the behaviours and attitudes of service users’ feedback into the operating conditions, maintaining the social norms that shape exclusion from access.
Study 3 adopted a participatory approach to elicit the collective perspective of individuals involved in delivery emergencies in villages. This study derived particularly vivid assessments of care, considerable detail on the micro-processes of care seeking, and informed a multi-level analysis. SHI was seen to be particularly problematic in Study 3, constraining access to good quality care in both communities and facilities. An important finding in Study 3 was that many of the problems identified were beyond the control of individuals (despite being enacted through their actions and attitudes) and could be attributed to broader health system arrangements. Study 3 also highlighted the potential of CPH for healthcare evaluation, as well as an intervention to promote individual responsibility for health through political participation in the health system.
Freedman and colleagues have proposed a conceptualisation of the health system as a core social institution that functions at the interface between individuals and wider structures of power (95, 111). Building on this model, quality and access can be considered as a distinct third element, a social process, observable through experience and reflective of the broader relationships between individuals and health systems (112).
According to this model, poor quality and access for poor women becomes both socially legitimate (imposed by structural arrangements) and socially legitimised (reciprocally maintained through the actions of individuals). The model also suggests that poor access and quality will occur and recur for disadvantaged women in a context of commodified care, fee-for service care provision, and inadequate district health funding.
Conclusions
There may be an implicit assumption in the SBA and EmOC approaches regarding the uniform distribution of access to, and quality of care. As such, the research examined the role of quality of, and access to care in obstetric emergencies. The assumptions underpinning the research were that social, cultural, health systems and biomedical factors determine service uptake, QOC and health outcomes, and that valid insights into these relationships can be gained from the perspectives of those who directly provide and receive this care. The research sought to contribute to a more complete understanding of the nature and influence of these processes, mechanisms and the dynamics between them.
A wide range of factors were identified that affected access and quality. These factors primarily related to the availability of village midwives, the configuration of maternal health services in communities, the financial accessibility of care, and the lack of functioning referral facilities. In this setting, a market-based healthcare system coupled with low investment in public maternal healthcare has resulted in providers without responsibility to the poor and rural, and exclusion from access to quality care on this basis.
An important finding was that the problems with access and quality were often beyond the control of individual women, families and providers, and could be related to the operating conditions of the health system. The analyses suggest that the manner in which services are organised and delivered via the health system may socially legitimise and, through the actions of individual women and providers, actively maintain, constrained access to good quality care in obstetric emergencies.
The analysis suggests that the health system may be considered as a target for reform and as an enabling mechanism capable of mediating and maintaining relationships between poor women and access to life-saving healthcare. Given the experience of decentralisation in other transitional and low income countries, the Indonesian government should carefully consider whether decentralisation is coupled with sufficient financial resource and administrative capacity at district level, and how liberation of the healthcare market may affect poor and rural groups of women who require care in obstetric emergencies.
Acknowledgements
This paper was developed within the Umeå Centre for Global Health Research, with support from FAS, the Swedish Council for Working Life and Social Research (grant no. 2006-1512). The research was funded as part of the Initiative for Maternal Mortality Programme Assessment (Immpact), supported by the Bill & Melinda Gates Foundation, UK Department for International Development, European Commission and USAID, and coordinated by the University of Aberdeen, Scotland. The views expressed herein are solely those of the author. The author would like to acknowledge PhD supervisors, Dr. Julia Hussein and Dr. Alice Kiger, University of Aberdeen, UK, Prof. Peter Byass, University of Umea, Sweden and Dr. Anna Coates, Gender Equality and Women's Empowerment Section, Social Development Division United Nations ESCAP, Thailand. At the University of Indonesia, acknowledgement is made to Prof. Anhari Achadi, Dr. Endang Achadi, Dr. Asri Adisasmita, Trisari Anggondowati, Poppy Deviany, Kamaluddin Latief, Dr. Mardiati Nadjib, Fitri Nandiaty, Eko Pambudi, Meidy Prameswari, Tetty Rachmawati, Dr. Dyah Suslam, Prof. Budi Utomo, Widyaningsih and Nathya S. Yahya. Special thanks go to Yulia Izati, Dr. Siti Nurul Qomariyah, and Dr. Evi Martha at the University of Indonesia and Krystyna Makowiecka at the London School of Hygiene and Tropical Medicine who made significant contributions to the fieldwork and analysis. Thanks to Dr. Lukman H.L. at the Ministry of Health in Jakarta, to Dr. Sri Nurhayati, Serang District Health Office, to the staff at Pandeglang District Health Office and Kramat Watu and Ciruas Puskesmas, Serang, who provided invaluable support, advice and practical assistance. Thanks to Study 1 panellists Dr. M.J.N. Mamahit, Tangerang Hospital, Tangerang, Dr. M. Baharuddin Budi Kemulyaan Hospital, Jakarta, Dr. Didi Danukusumo, Fatmawati Hospital, Jakarta, Dr. Eddy Harianto, Cipto Mangunkusumo Hospital, Dr. A. Sastrowardoyo, Fatmawati Hospital, Jakarta, Dr. A. Sulistomo, Facility of Medicine, University of Indonesia (Hospital OBGYN Specialist Practitioner Panel), Dr. T. Lestaria, Tangerang District Health Office, Dr. Meis, Balaraja Puskesmas, Tangerang, Dr. Yully, Curug Puskesmas, Tangerang, Bidan Henalusti, Balaraja Puskesmas, Tangerang, Bidan A. Mulyani, Balaraja Puskesmas, Tangerang, Bidan Nasih S., Tangerang District Health Office, Bidan N. Hanum, Teluknaga Puskesmas, Tangerang (Community Midwife Practitioner Panel) for their inputs, commitment, and for championing the method. Special thanks also go to the data collectors, Lupthi Tri Utari, Sri Rahmi, Kray S. Asa and Agus Khomeini (Study 2), and Indah Ayu Permata Sary, Dendi Hendarsyah and Reny Setiawaty (Study 3) for their hard work, enthusiasm and insights into the perspectives of study participants. Finally, sincere thanks go to the study participants for their time, hospitality, good humour and for sharing personal information about relatives and patients.
Biography

Footnotes
†Basic EmOC facilities provide administration of parenteral antibiotics, oxytocic drugs and anticonvulsants, manual removal of placenta, removal of retained products and assisted vaginal delivery. Comprehensive EmOC facilities perform all basic EmOC signal functions as well as surgery (Caesarean section) and blood transfusion (27)
Conflict of interest and funding
No conflicts of interest are stated.
References
- 1.Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609–23. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- 2.WHO, UNICEF, UNFPA, World Bank. Geneva: World Health Organization; 2010. Trends in maternal mortality: 1990 to 2008 estimates developed by WHO, UNICEF, UNFPA and The World Bank. Available from: http://www.who.int/reproductivehealth/publications/monitoring/9789241500265/en/index.html [cited 12 July 2012] [Google Scholar]
- 3.WHO, UNICEF. Geneva: World Health Organization; 1996. Revised 1990 estimates of maternal mortality: a new approach by WHO and UNICEF. WHO/FRH/MSM/96.11. Available from: http://whqlibdoc.who.int/hq/1996/WHO_FRH_MSM_96.11.pdf [cited 12 July 2012] [Google Scholar]
- 4.WHO, UNICEF, UNFPA. Geneva: World Health Organization; 2001. Maternal mortality in 1995: estimates developed by WHO, UNICEF, UNFPA. WHO/RHR/01.9. Available from: http://www.who.int/reproductivehealth/publications/monitoring/RHR-01-9/en/index.html [cited 12 July 2012] [Google Scholar]
- 5.WHO, UNICEF, UNFPA. Geneva: World Health Organization; 2004. Maternal mortality in 2000: estimates developed by WHO, UNICEF and UNFPA. Available from: http://www.who.int/reproductivehealth/publications/monitoring/9241562706/en/index.html [cited 12 July 2012] [Google Scholar]
- 6.WHO, UNICEF, UNFPA, World Bank. Geneva: World Health Organization; 2007. Maternal mortality in 2005: estimates developed by WHO, UNICEF, UNFPA, and The World Bank. Available from: http://www.who.int/whosis/mme_2005.pdf [cited 12 July 2012] [Google Scholar]
- 7.WHO, UNICEF, UNFPA, World Bank. Geneva: World Health Organization; 2012. Trends in maternal mortality: 1990 to 2010 WHO, UNICEF, UNFPA and The World Bank estimates. Available from: http://www.who.int/reproductivehealth/publications/monitoring/9789241503631/en/.[cited 12 July 2012]. [Google Scholar]
- 8.AbouZahr C. New estimates of maternal mortality and how to interpret them: choice or confusion? Reprod Health Matters. 2011;19:117–28. doi: 10.1016/S0968-8080(11)37550-7. [DOI] [PubMed] [Google Scholar]
- 9.NICE, Scottish Executive Health Department, Department of Health, Social Services and Public Safety Northern Ireland. London: RCOG Press; 2001. Why mothers die 1997–1999: the fifth report of the confidential enquiries into maternal deaths in the United Kingdom. Available from: http://www.rcog.org.uk/image/lewis-why-mothers-die-1997-1999 [cited 12 July 2012] [Google Scholar]
- 10.Filippi V, Ronsmans C, Campbell OM, Graham WJ, Mills A, Borghi J, et al. Maternal health in poor countries: the broader context and a call for action. Lancet. 2006;368:1535–41. doi: 10.1016/S0140-6736(06)69384-7. [DOI] [PubMed] [Google Scholar]
- 11.Storeng KT, Baggaley RF, Ganaba R, Ouattara F, Akoum MS, Filippi V. Paying the price: the cost and consequences of emergency obstetric care in Burkina Faso. Soc Sci Med. 2008;66:545–57. doi: 10.1016/j.socscimed.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 12.WHO. Moving towards universal coverage: issues in maternal-newborn health and poverty. Geneva: World Health Organization; 2006. The costs of maternal-newborn ill-health and mortality. Available from: http://whqlibdoc.who.int/publications/2006/9241594497_eng.pdf [cited 12 July 2012] [Google Scholar]
- 13.Donnay F, Weil L. Obstetric fistula: the international response. Lancet. 2004;363:71–2. doi: 10.1016/S0140-6736(03)15177-X. [DOI] [PubMed] [Google Scholar]
- 14.Filippi V, Ganaba R, Baggaley RF, Marshall T, Storeng KT, Sombie I, et al. Health of women after severe obstetric complications in Burkina Faso: a longitudinal study. Lancet. 2007;370:1329–37. doi: 10.1016/S0140-6736(07)61574-8. [DOI] [PubMed] [Google Scholar]
- 15.de Kok BC, Widdicombe S. ‘I really tried’: management of normative issues in accounts of ‘responses’ to infertility. Soc Sci Med. 2008;67:1083–93. doi: 10.1016/j.socscimed.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Gill K, Pande R, Malhotra A. Women deliver for development. Lancet. 2007;370:1347–57. doi: 10.1016/S0140-6736(07)61577-3. [DOI] [PubMed] [Google Scholar]
- 17.Rosenfield A, Maine D. Maternal mortality – a neglected tragedy: where is the M in MCH? Lancet. 1985;326:83–5. doi: 10.1016/s0140-6736(85)90188-6. [DOI] [PubMed] [Google Scholar]
- 18.Starrs A. Preventing the tragedy of maternal deaths: a report on the International Safe Motherhood Conference; Nairobi: World Bank, World Health Organization & UNFPA; 1987. [Google Scholar]
- 19.Starrs AM. Safe motherhood initiative: 20 years and counting. Lancet. 2006;368:1130–2. doi: 10.1016/S0140-6736(06)69385-9. [DOI] [PubMed] [Google Scholar]
- 20.FCI. The safe motherhood action agenda: priorities for the next decade. Report on the Safe Motherhood Technical Consultation; 18–23 October 1997; Colombo, Sri Lanka. New York: FCI; 1998. [Google Scholar]
- 21.Loudon I. Death in childbirth: an international study of maternal care and maternal mortality, 1800–1950. Oxford: Oxford University Press; 1992. [Google Scholar]
- 22.Shiffman J. Can poor countries surmount high maternal mortality? Stud Fam Plann. 2000;31:274–89. doi: 10.1111/j.1728-4465.2000.00274.x. [DOI] [PubMed] [Google Scholar]
- 23.Graham W, Bell J, Bullough CHW. Can skilled attendance at delivery reduce maternal mortality in developing countries? Stud Health Serv Organ Policy. 2001;17:97–130. [Google Scholar]
- 24.Van Lerberghe W, De Brouwere V. Of blind alleys and things that have worked: history's lessons on reducing maternal mortality. Stud Health Serv Organ Policy. 2001;17:7–33. [Google Scholar]
- 25.Pathmanathan I, Liljestrand J, Martins JM, Rajapaksa LC, Lissner C, de Silva A, et al. Investing in maternal health; learning from Malaysia and Sri Lanka. Washington: World Bank, Human Development Network; 2003. [Google Scholar]
- 26.Gulmezoglu AM, Forna F, Villar J, Hofmeyr GJ. Prostaglandins for prevention of postpartum haemorrhage. Cochrane Database Syst Rev. 2004;1 doi: 10.1002/14651858.CD000494.pub2. CD000494. Available from: http://apps.who.int/rhl/reviews/CD000494.pdf [cited 12 July 2012] [DOI] [PubMed] [Google Scholar]
- 27.UNICEF, WHO, UNFPA. Geneva: World Health Organization; 1997. Guidelines for monitoring the availability and use of obstetric services. Available from: http://www.unicef.org/health/files/guidelinesformonitoringavailabilityofemoc.pdf [cited 12 July 2012] [Google Scholar]
- 28.Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 29.WHO, UNICEF, UNFPA, AMDD. Geneva: World Health Organization; 2009. Monitoring emergency obstetric care: a handbook. Available from: http://www.who.int/reproductivehealth/publications/monitoring/9789241547734/en/index.html [cited 12 July 2012] [Google Scholar]
- 30.UN. A/RES/55/2. New York: United Nations; 2000. United Nations Millennium Declaration. Available from: http://www.un.org/millennium/declaration/ares552e.pdf [cited 12 July 2012] [Google Scholar]
- 31.UN. New York: United Nations; 2010. Millennium Development Goals. Available from: http://www.un.org/millenniumgoals/ [Google Scholar]
- 32.Lancet. Maternal Survival Series; London: Lancet; 2006. [Google Scholar]
- 33.Freedman LP, Graham WJ, Brazier E, Smith JM, Ensor T, Fauveau V, et al. Practical lessons from global safe motherhood initiatives: time for a new focus on implementation. Lancet. 2007;370:1383–91. doi: 10.1016/S0140-6736(07)61581-5. [DOI] [PubMed] [Google Scholar]
- 34.Penn-Kekana L, McPake B, Parkhurst J. Improving maternal health: getting what works to happen. Reprod Health Matters. 2007;15:28–37. doi: 10.1016/S0968-8080(07)30335-2. [DOI] [PubMed] [Google Scholar]
- 35.D'Ambruoso L, Izati Y, Adisasmita A, Qomariyah SN, Achadi E, Byass P. Accountability and agency: the positive potential of local audit. Unpublished manuscript. Sweden: Umeå University; 2012. [Google Scholar]
- 36.Shankar A, Sebayang S, Guarenti L, Utomo B, Islam M, Fauveau V, et al. The village-based midwife programme in Indonesia. Lancet. 2008;371:1226–9. doi: 10.1016/S0140-6736(08)60538-3. [DOI] [PubMed] [Google Scholar]
- 37.Hennessy DA, Hicks CM, Kawonal Y, Hilan A. A methodology for assessing the professional development needs of nurses and midwives in Indonesia: paper 1 of 3. Hum Resour Health. 2006;4 doi: 10.1186/1478-4491-4-8. Available from: http://www.biomedcentral.com/1478-4491/4/8 [cited 12 July 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gani A. Improving quality in public sector hospitals in Indonesia. Int J Health Plan Manag. 1996;11:275–96. doi: 10.1002/(SICI)1099-1751(199607)11:3<275::AID-HPM436>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 39.Daly P, Sadah F. Indonesia: facing the challenge to reduce maternal mortality. Watching brief. Washington, DC: World Bank East Asia and Pacific Region; 1999. [Google Scholar]
- 40.Ensor T, Quayyum Z, Nadjib M, Sucahya P. Level and determinants of incentives for village midwives in Indonesia. Health Policy Plan. 2008;24:26–35. doi: 10.1093/heapol/czn040. [DOI] [PubMed] [Google Scholar]
- 41.MOH. National Strategic Plan on Making Pregnancy Safer (MPS) Indonesia 2001–2010; Jakarta: Republic of Indonesia; 2001. [Google Scholar]
- 42.Hermiyanti S. Jakarta: Republic of Indonesia; 2008. The challenges of making safe motherhood a reality: community midwives in Indonesia. Available from: http://www.searo.who.int/LinkFiles/FCH_d3-7challenges-msm-ino.pdf [cited 12 July 2012] [Google Scholar]
- 43.Kristiansen S, Santoso P. Surviving decentralisation? Impacts of regional autonomy on health service provision in Indonesia. Health Policy. 2006;77:247–59. doi: 10.1016/j.healthpol.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 44.Frankenberg E, Suriastini W, Thomas D. Can expanding access to basic healthcare improve children's health status? Lessons from Indonesia's ‘midwife in the village’ programme. Popul Stud. 2005;59:5–19. doi: 10.1080/0032472052000332674. [DOI] [PubMed] [Google Scholar]
- 45.Shrestha R. New York: Population Association of America; 2007. The village midwife program and the reduction in infant mortality in Indonesia. Available from: http://paa2007.princeton.edu/download.aspx?submissionId=71863 [cited 12 July 2012] [Google Scholar]
- 46.BPS, Macro. Calverton, MD: BPS and Macro International; 2008. Indonesia Demographic and Health Survey 2007. Available from: http://www.measuredhs.com/publications/publication-fr218-dhs-final-reports.cfm [cited 12 July 2012] [Google Scholar]
- 47.Bell J, Qomariyah SN. London: Presentation at Immpact International Symposium’ Delivering Safer Motherhood; Sharing the Evidence’; 2007. Immpact – tools and methods: selected findings on maternal mortality. Available from: http://www.immpact-international.org/uploads/files/Session19_section3_Immpact_JBell_MM.pdf [cited 12 July 2012] [Google Scholar]
- 48.Ronsmans C, Scott S, Qomariyah SN, Achadi E, Braunholtz D, Marshall T, et al. Professional assistance during birth and maternal mortality in two Indonesian districts. Bull World Health Organ. 2009;87:416–23. doi: 10.2471/BLT.08.051581. Available from: http://www.who.int/bulletin/volumes/87/6/08-051581/en/index.html [cited 12 July 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Achadi E, Scott S, Pambudi ES, Makowiecka K, Marshall T, Adisasmita A, et al. Midwifery provision and uptake of maternity care in Indonesia. Trop Med Int Health. 2007;12:1490–7. doi: 10.1111/j.1365-3156.2007.01957.x. [DOI] [PubMed] [Google Scholar]
- 50.Pirkle CM, Dumont A, Zunzunegui M-V. Criterion-based clinical audit to assess quality of obstetrical care in low- and middle-income countries: a systematic review. Int J Qual Health Care. 2011;23:456–63. doi: 10.1093/intqhc/mzr033. [DOI] [PubMed] [Google Scholar]
- 51.Hulton LA, Matthews Z, Stones RW. Applying a framework for assessing the quality of maternal health services in urban India. Soc Sci Med. 2007;64:2083–95. doi: 10.1016/j.socscimed.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 52.Chin MH, Muramatsu N. What is the quality of quality of medical care measures? Rashomon-like relativism and real-world applications. Perspect Biol Med. 2003;46:5–20. doi: 10.1353/pbm.2003.0002. [DOI] [PubMed] [Google Scholar]
- 53.Donabedian A. An introduction to quality assurance in health care. London: Oxford University Press; 2003. [Google Scholar]
- 54.Suleiman AB, Mathews A, Jegasothy R, Ali R, Kandiah N. A strategy for reducing maternal mortality. Bull World Health Organ. 1999;77:190–3. Available from: http://www.who.int/bulletin/archives/77(2)190.pdf [cited 12 July 2012] [PMC free article] [PubMed] [Google Scholar]
- 55.Campbell O, Gipson R, Hakim Issa A, Matta N, El Deeb B, El Mohandes A, et al. National maternal mortality ratio in Egypt halved between 1992–93 and 2002. Bull World Health Organ. 2005;83:462–73. Available from: http://www.who.int/bulletin/volumes/83/6/campbell0605abstract/en/index.html [cited 12 July 2012] [PMC free article] [PubMed] [Google Scholar]
- 56.South Africa Every Death Counts Writing Group. Every death counts: use of mortality audit data for decision making to save the lives of mothers, babies, and children in South Africa. Lancet. 2008;371:1294–304. doi: 10.1016/S0140-6736(08)60564-4. [DOI] [PubMed] [Google Scholar]
- 57.Pattinson RC, Hall M. Near misses: a useful adjunct to maternal death enquiries. Br Med Bull. 2003;67:231–43. doi: 10.1093/bmb/ldg007. [DOI] [PubMed] [Google Scholar]
- 58.Drife J. Fifty years of the confidential enquiry into maternal deaths. Br J Hosp Med. 2006;67:121–5. doi: 10.12968/hmed.2006.67.3.20611. [DOI] [PubMed] [Google Scholar]
- 59.Andersen RM. Research Series No. 25. Chicago: Center for Health Administration Studies, University of Chicago; 1968. Behavioural model of families’ use of health services. [Google Scholar]
- 60.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–40. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 61.Frenk J. The concept and measurement of accessibility. In: White KL, editor. Health services research: an anthology. Washington: Pan American Health Organization; 1992. pp. 822–55. [Google Scholar]
- 62.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. doi: 10.1186/1471-2288-6-35. Available from: http://www.biomedcentral.com/1471-2288/6/35 [cited 12 July 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.CESCR. General Comment No. 14. New York: United Nations; 2000. The right to the highest attainable standard of health: 11/08/2000. E/C.12/2000/4. Available from: http://www.cetim.ch/en/documents/codesc-2000-4-eng.pdf [cited 12 July 2012] [Google Scholar]
- 64.Fottrell E, Byass P. Verbal autopsy: methods in transition. Epidemiol Rev. 2010;32:1–18. doi: 10.1093/epirev/mxq003. [DOI] [PubMed] [Google Scholar]
- 65.WHO. Geneva: World Health Organization; 2007. Verbal Autopsy Standards: ascertaining and attributing causes of death. Available from: http://www.who.int/healthinfo/statistics/verbalautopsystandards/en/index.html [cited 12 July 2012] [Google Scholar]
- 66.Byass P, Fottrell E, Huong DL, Berhane Y, Corrah T, Kahn K, et al. Refining a probabilistic model for interpreting verbal autopsy data. Scand J Public Health. 2006;34:26–31. doi: 10.1080/14034940510032202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fantahun M, Fottrell E, Berhane Y, Wall S, Högberg U, Byass P. Assessing a new approach to verbal autopsy interpretation in a rural Ethiopian community: the InterVA model. Bull World Health Organ. 2006;84:204–10. doi: 10.2471/blt.05.028712. Available from: http://www.who.int/bulletin/volumes/84/3/204.pdf [cited 12 July 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kalter HR, Salgado R, Babille M, Koffi A, Black R. Social autopsy for maternal and child deaths: a comprehensive literature review to examine the concept and the development of the method. Popul Health Metrics. 2011;9:45. doi: 10.1186/1478-7954-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 70.CESCR. General Comment No. 14. New York: United Nations; 2000. The right to the highest attainable standard of health: 11/08/2000. E/C.12/2000/4. Available from: http://www.unhchr.ch/tbs/doc.nsf/(symbol)/E.C.12.2000.4.En [cited 12 July 2012]. [Google Scholar]
- 71.Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364:970–9. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 72.Borghi J, Thapa B, Osrin D, Jan S, Morrison J, Tamang S, et al. Economic assessment of a women's group intervention to improve birth outcomes in rural Nepal. Lancet. 2005;366:1882–4. doi: 10.1016/S0140-6736(05)67758-6. [DOI] [PubMed] [Google Scholar]
- 73.Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M, Awasthi S, et al. Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008;372:1151–62. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- 74.Rath S, Nair N, Tripathy P, Barnett S, Rath S, Mahapatra R, et al. Explaining the impact of a women's group led community mobilisation intervention on maternal and newborn health outcomes: the Ekjut trial process evaluation. BMC Int Health Hum Rights. 2010;10:25. doi: 10.1186/1472-698X-10-25. Available from: http://www.biomedcentral.com/content/pdf/1472-698X-10-25.pdf [cited 12 July 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, et al. Effect of a participatory intervention with women's groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. 2010;375:1182–92. doi: 10.1016/S0140-6736(09)62042-0. [DOI] [PubMed] [Google Scholar]
- 76.Rifkin SB. Health planning and community participation: case studies from South-East Asia. London: Croom Helm; 1985. [Google Scholar]
- 77.Cohen JM, Uphoff NT. Participation's place in rural development: seeking clarity through specificity. World Dev. 1980;8:213–35. [Google Scholar]
- 78.Cornwall A. Unpacking ‘participation’: models, meanings and practices. Community Dev J. 2008;43:269–83. [Google Scholar]
- 79.Krueger RA. Focus groups: a practical guide for applied research. London: Sage Publications; 2000. [Google Scholar]
- 80.Dahlgren L, Emmelin M, Winkvist A. Qualitative methodology for international public health. Umeå: Umeå University; 2007. [Google Scholar]
- 81.Pope C, Mays N. Qualitative research in health care. Oxford: Blackwell Publishing; 2006. [Google Scholar]
- 82.QSR International. NVIVO [software package]; Doncaster, Victoria: QSR International Pty Ltd; 2007. [Google Scholar]
- 83.D'Ambruoso L, Achadi E, Adisasmita A, Izati Y, Makowiecka K, Hussein J. Assessing quality of care provided by Indonesian village midwives with a confidential enquiry. Midwifery. 2009;25:528–39. doi: 10.1016/j.midw.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 84.D'Ambruoso L, Byass P, Qomariyah SN, Ouédraogo M. A lost cause? Extending verbal autopsy to investigate biomedical and sociocultural causes of maternal death in Burkina Faso and Indonesia. Soc Sci Med. 2010a;71:1728–38. doi: 10.1016/j.socscimed.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 85.Geller SE, Adams MG, Kelly PJ, Kodkany BS, Derman RJ. Postpartum hemorrhage in resource-poor settings. Int J Gynaecol Obstet. 2006;92:202–11. doi: 10.1016/j.ijgo.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 86.D'Ambruoso L, Byass P, Qomariyah SN. Maybe it was her fate and maybe she ran out of blood’: final caregivers’ perspectives on access to care in obstetric emergencies rural Indonesia. J Biosoc Sci. 2010b;42:213–41. doi: 10.1017/S0021932009990496. [DOI] [PubMed] [Google Scholar]
- 87.D'Ambruoso L, Byass P, Qomariyah SN. Can the right to health inform public health planning in developing counties? A case study for maternal healthcare from Indonesia. Glob Health Action. 2008;1:1. doi: 10.3402/gha.v1i0.1828. Available from: http://www.globalhealthaction.net/index.php/gha/article/view/1828 [cited 12 July 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.D'Ambruoso L, Martha E, Izati Y, Kiger A, Coates A. Maternal mortality and severe morbidity in rural Indonesia Part 1: the community perspective. Sweden: Unpublished manuscript. Umeå University; 2012a. [Google Scholar]
- 89.D'Ambruoso L, Martha E, Izati Y, Kiger A, Coates A. Maternal mortality and severe morbidity in rural Indonesia Part 2: implementation of a community audit. Sweden: Umeå University; 2012b. Unpublished manuscript. [Google Scholar]
- 90.Departemen Kesehatan, Immpact. Improving village based emergency obstetric care in Indonesia: a confidential enquiry into maternal death and disability: recommendations for practice; Jakarta: Immpact Indonesia; 2008. [Google Scholar]
- 91.Immpact. Aberdeen: University of Aberdeen; 2008. Extending verbal autopsy to examine social and medical causes of maternal mortality. Indonesia Briefing Note. Available from: http://www.immpact-international.com/uploads/files/Indonesia%20EVA%20briefing%20note%20Nov%20182008.pdf [cited 12 July 2012] [Google Scholar]
- 92.Kemitraan Kesehatan Masyarakat (Community Health Partnerships Project) Jakarta: Immpact Indonesia; 2008. Power in partnerships: official record of the Community Health Partnerships Project conducted by Immpact, University of Indonesia. [Google Scholar]
- 93.Kemitraan Kesehatan Masyarakat (Community Health Partnerships Project) Jakarta: Immpact Indonesia. Policy Brief; 2010. Realities and priorities: a community-based audit of maternal mortality and severe morbidity in rural Indonesia. [Google Scholar]
- 94.Berman PA. Village health workers in Java, Indonesia: coverage and equity. Soc Sci Med. 1984;19:411–22. doi: 10.1016/0277-9536(84)90199-0. [DOI] [PubMed] [Google Scholar]
- 95.Freedman L. Achieving the MDGs: health systems as core social institutions. Development. 2005;48:19–24. [Google Scholar]
- 96.Smoke P, Lewis BD. Fiscal decentralization in Indonesia: a new approach to an old idea. World Dev. 1996;24:1281–99. [Google Scholar]
- 97.Hadiz VR. Decentralization and democracy in Indonesia: a critique of neo-institutionalist perspectives. Dev Change. 2004;35:697–718. [Google Scholar]
- 98.Thabrany H. Human resources in decentralised health systems in Indonesia. Reg Health Forum. 2006;10:75–86. [Google Scholar]
- 99.Devas N. Indonesia: what do we mean by decentralization? Public Adm Dev. 1998;17:351–67. [Google Scholar]
- 100.McCarthy JF. Changing to gray: decentralization and the emergence of volatile socio-legal configurations in Central Kalimantan, Indonesia. World Dev. 2004;32:1199–223. [Google Scholar]
- 101.Almonte J. Indonesia's future challenges and implications for the region. Jakarta: CSCAP International Seminar; 2000. [Google Scholar]
- 102.Rabasa A, Chalk P. Reinventing Indonesia: the challenge of decentralization. In: Heller Jeanne, Wirtz Phillip., editors. Indonesia's transformation and the stability of Southeast Asia. Santa Monica: RAND; 2001. Available from: http://www.rand.org/content/dam/rand/pubs/monograph_reports/2001/MR1344.pdf [cited 12 July 2012] [Google Scholar]
- 103.Bebbington A, Dharmawan L, Fahmi E, Guggenheim S. Village politics, culture and community-driven development: insights from Indonesia. Prog Dev Stud. 2004;4:187–205. [Google Scholar]
- 104.Baso ZA. The emerging impact of decentralisation on health systems. In: Thanenthiran Sivananthi, Khan Ayesha., editors. Rights and realities: monitoring reports on the status of Indonesian women's sexual and reproductive health and rights. Kuala Lumpur: Asian-Pacific Resource and Research Centre for Women (ARROW); 2007. Available from: http://www.arrow.org.my/index.php/publications/researchamonitorin.html [cited 12 July 2012] [Google Scholar]
- 105.Thanenthiran S, Racherla SJ. Kuala Lumpur: Asian-Pacific Resource and Research Centre for Women (ARROW); 2007. Reclaiming and redefining rights – ICPD+15: status of sexual and reproductive health and rights in Asia. Available from: http://www.arrow.org.my/index.php/publications/researchamonitorin.html [cited 12 July 2012] [Google Scholar]
- 106.Sparrow R, Suryahadi A, Widyanti W. Cape Town: Annual Bank Conference on Development Economics; 2008. Public health insurance for the poor in Indonesia: targeting and impact of Indonesia's Askeskin programme. Available from: http://ihea2009.abstractbook.org/presentation/450/ [cited 12 July 2012] [Google Scholar]
- 107.Halabi SF. Participation and the right to health: lessons from Indonesia. Health Hum Rights: Int J. 2009;11:1. Available from: http://www.hhrjournal.org/index.php/hhr/article/viewFile/129/206 [cited 12 July 2012] [PubMed] [Google Scholar]
- 108.Berman PA, Gwatkin DR, Burger SE. Community-based health workers: head start or false start towards health for all? Soc Sci Med. 1987;25:443–59. doi: 10.1016/0277-9536(87)90168-7. [DOI] [PubMed] [Google Scholar]
- 109.Walt G. CHWs: are national programmes in crisis? Health Policy Plan. 1988;3:1–21. [Google Scholar]
- 110.Aday LA, Andersen R. A framework for the study of access to medical care. Health Services Research. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]
- 111.Freedman LP, Waldman RJ, de Pinho H, Wirth ME, Chowdhury AM, Rosenfield A. Transforming health systems to improve the lives of women and children. Lancet. 2005;365:997–1000. doi: 10.1016/S0140-6736(05)71090-4. [DOI] [PubMed] [Google Scholar]
- 112.Giddens A. The constitution of society: outline of the theory of structuration. Cambridge: Polity Press; 1984. [Google Scholar]