Abstract
BACKGROUND:
Hypertension prevention and control are among the most important public health priorities. We evaluated the impacts of a workplace intervention project “Stop Hypertension in Mobarakeh Steel Company” (SHIMSCO) on controlling hypertension in industrial workers.
METHODS:
The study was carried out in Mobarakeh Steel Company in Isfahan among 7286 male workers and employees. All individuals were evaluated for the presence of hypertension (HTN). According to examinations, 500 subjects with systolic blood pressure (SBP) ≥ 140 mmHg, and/or diastolic blood pressure (DBP) ≥ 90 mmHg, and/or those using antihypertensive medications were confirmed to have HTN and thus included in this study. They were questioned for sociodemographic characteristics, past medical history and medication use. They received an educational program including healthy lifestyle and self-care recommendations of HTN management and control as well as training for accurate blood pressure measurement and home monitoring for two years. SBP, DBP, weight, height and routine lab tests were measured for all hypertensive subjects before and after the interventions. Paired t-test, generalized estimation equation (GEE) and ordinary linear regression (OLR) were used for statistical analysis in SPSS.
RESULTS:
The comparison of SBP and DBP before and after the educational program showed significant reductions in both parameters (−7.97 ± 14.72 and −2.66 ± 9.96 mmHg, respectively). However, a greater decrease was detected in case of DBP. GEE showed SBP and DBP to decrease about −0.115 and −0.054 mmHg/month. OLR also revealed reductions of 4.88 and 2.57 mmHg respectively in SBP and DBP upon adding each antihypertensive drug.
CONCLUSION:
SHIMSCO, a 3-year interventional project in workplaces, was effective in reducing SBP and DBP among hypertensive employees and workers. We conclude that implementing simple educational programs in worksites can improve the management and control of hypertension and perhaps other chronic diseases.
Keywords: Hypertension, Worksite, Industrial, Blood Pressure, Control
Introduction
Cardiovascular diseases (CVDs) are a major cause of mortality and morbidity in Iran.1 Although the overall prevalence of hypertension in Iran is 17.8%, the rate increases to 23% and 50% in 30–55 and > 55-year-old population, respectively.2 However, the complication is less common in rural areas than urban areas.3 On the other hand, low detection rates, high treatment drop-out, and poor compliance with medications have led to increased prevalence of uncontrolled hypertension and its complications in the recent years.4 Physicians seem to be unable to control more than 30% of the total hypertensive population in their private offices.5 Therefore, alternative medical care approaches such as workplace interventions have been suggested.6,7 Several studies designed to evaluate population-based approaches have showed unclear results.8,9 In a meta-analysis by Lim et al. health promotion was not found to be significantly beneficial in developed countries.10 In contrast, in developing countries such as Mauritius and India, successful models have been designed and used in health promotion activities.11–14 Easy access to big proportions of population, ability to repeat the interventions in workplaces, and cost-effectiveness of these models are among their success reasons. Considering the high prevalence of hypertension and poor control in our country (Iran),15 the “Stop Hypertension in Mobarakeh Steel Company” (SHIMSCO) study was conducted to evaluate the impacts of the “Workplace Intervention Project”,16 as one of the interventional projects of the “Isfahan Healthy Heart Program” (IHHP),17 on hypertension management and control among employees and workers in the biggest industry in Isfahan, Iran.
Materials and Methods
IHHP, a community-based study, was conducted with the aim of CVD prevention and health promotion.17,18 The current study was a part of the “Workplace Intervention Project” which in turn has been one of ten interventional projects of IHHP carried out in “Mobarakeh Steel Company” with more than 14000 employees and workers in Isfahan. Totally, 7286 male employees and workers participated in the annual medical exam performed by the company. After examinations, 959 (13%) persons with systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) was ≥ 90 mmHg, or those who were using antihypertensive medications were invited to participate in this study by workplace follow up Unit. Blood pressure (BP) was re-assessed in these subjects to confirm their hypertension and 500 subjects (6.9%) were defined as confirmed hypertensives.19 All hypertensives underwent routine lab tests and physical exams in the workplace follow up center. During 2008 to 2009, the participants and their spouses were referred to Isfahan Cardiovascular Research Institute (ICRI), a WHO (World Heart Organization) collaborating center), for more evaluation. However, only 293 individuals took part in the ICRI educational sessions while the rest participated in workplace clinics where the ICRI team delivered them the same educational program.
Demographic data including age, employment duration, educational level, and marital status was collected from all participants. They also completed a questionnaire regarding lifestyle behaviors such as unhealthy nutrition, physical inactivity and smoking. Height and weight were measured by Seca scales with light clothes and no shoes on. Body mass index (BMI) was then calculated as weight (kg) divided by height squared (m2). Subjects with BMI ≥ 25 kg/m2 were considered as overweight and obese. Patients were treated based on available hypertension treatment guidelines. The follow-up intervals were determined depending on the status of BP and associated risk factors in each patient individually. All study subjects received an educational program for management, treatment and control of hypertension. The program consisted of three educational interactive 4-hour sessions. The educational content included reducing salt and fat intake, adhering to diet for stopping hypertension (DASH) recommendations,20 increasing physical activity and having regular aerobic exercise, smoking cessation of any type of tobacco products, decreasing daily calorie intake to reduce weight. It also covered information on the role of stresses in hypertension and how to cope with stress, risk factors for hypertension, recommendations for accurate BP measurements at home, advice to control other risk factors such as obesity and overweight, diabetes and lipid disorders, following and measuring BP at determined intervals in the follow-up clinic, the importance of adherence to treatment, medication side effects and evaluating the need for changes in drug regimens. All educations were delivered by trained physicians, nurses and dietitians and sometimes physical activity experts. A booklet including most of the educational content was provided to all participants. The patients were referred to cardiologists for further evaluations when needed. The whole baseline studies were repeated for each participant after finishing the educational sessions. The Ethics Committee of ICRI approved the study. In addition, all participants signed informed consents after they were explained about the aims and protocol of the study.
Data analysis
Data was analyzed in SPSS15. Paired t-test was used to compare mean values of SBP and DBP before and after the study in each group. Generalized estimating equations (GEE) were used to model correlated and longitudinal data for investigating the predictors of longitudinal changes in BP after controlling the confounding factors. The medication effect was assessed by ordinary linear regression (OLR). P values less than 0.05 were considered as significant.
Results
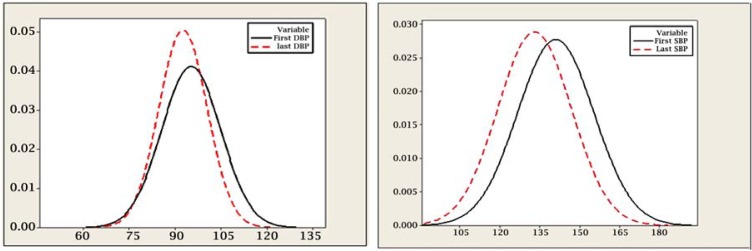
During 2008 to 2010, out of 7286 workers and employees who underwent the annual evaluation by the factory, 500 (6.9%) subjects with confirmed hypertension were included in our study. The demographic data of all participants is presented in table 1. Most subjects aged 45–54 years and 36.6% had 6–20 years of employment history. In addition, more than 78.0% had 12–16 years of education. The comparisons of SBP and DBP before and after the intervention program along with changes in associated risk factors are presented in table 2. After the intervention, a significant reduction in SBP (−7.97 ± 14.72 mmHg), DBP (−2.66 ± 9.96 mmHg) and mean arterial BP (−4.43 ± 10.60 mmHg) were seen (P < 0.001). However, SBP decreased less than DBP (Figure 1). After adjusting for confounding variables like age, education level, work shift, and BMI, GEE showed that SBP and DBP decreased about 0.115 and 0.054 mmHg/per month, respectively (Table 3). According to OLR on the other hand, SBP and DBP decreased about 4.88 and 2.57 mmHg upon adding each antihypertensive drug in the study. figure 2 shows the changes of SBP and DBP during the follow-up period.
Table 1.
Baseline characteristics of all participants*
| Employment duration (years) | ≤ 5 | 6–10 | 16–20 | 21–25 | 26+ |
| 12 (2.4) | 19 (3.8) | 183 (36.6) | 150 (30) | 136 (27.2) | |
|
| |||||
| Age groups (years) | 25–34 | 35–44 | 45–54 | 55+ | |
| 23 (4.6) | 106 (21.2) | 313 (2.6) | 58 (11.6) | ||
|
| |||||
| Work Shift | Day worker | Routine shift worker | Weekly shift worker | ||
| 271 (54.2) | 204 (40.8) | 25 (5) | |||
|
| |||||
| Educational level (years) | < 12 | 12–16 | 16+ | ||
| 105 (21) | 390 (78) | 5 (1) | |||
|
| |||||
| Marital Status | Single | Married | |||
|
| |||||
| 13 (2.6) | 487 (97.4) | ||||
Data is expressed as N (%).
Table 2.
Systolic and diastolic blood pressure and associated risk factors before and after the study
| Variable | Before | After | Difference | P-value |
95% CI Difference
|
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| SBP | 141.15 ± 14.36 | 133.17 ± 13.81 | −7.97 ± 14.72 | < 0.001 | −9.276 | −6.671 |
| DBP | 95.26 ± 9.67 | 92.60 ± 7.89 | −2.66 ± 9.91 | < 0.001 | −3.535 | −1.780 |
| MAP | 110.55 ± 10.28 | 106.12 ± 8.98 | −4.43 ± 10.60 | < 0.001 | −5.3681 | −3.49 |
| FBS (mg/dl) | 101.30 ± 27.94 | 102.82 ± 33.29 | 1.52 ± 26.94 | 0.220 | −0.912 | 3.97 |
| Triglyceride (mg/dl) | 192.49 ± 125.93 | 178.43 ± 99.77 | −14.06 ± 108.98 | 0.006 | −24.02 | −4.11 |
| Total Cholesterol (mg/dl) | 202.91 ± 39.13 | 191.84 ± 35.16 | −11.07 ± 35.52 | < 0.001 | −14.32 | −7.82 |
| BMI (kg/ m2) | 27.45 ± 3.79 | 28.43 ± 4.66 | 0.99 ± 2.60 | 0.200 | 0.742 | 1.23 |
SBP: Systolic blood pressure; DBP: Diastolic blood pressure; MAP: Mean arterial pressure; FBS: Fasting blood sugar; BMI: Body mass index
Figure 1.
Systolic and diastolic blood pressure changes before and after the interventions
Table 3.
The effects of the intervention and medications on changes in blood pressure over time
| Fixed factors |
Systolic Blood Pressure
|
Diastolic Blood Pressure
|
||||
|---|---|---|---|---|---|---|
| Beta | Std. Error | P | Beta | Std. Error | P | |
| Participation time (Months) * | −0.115 | 0.0268 | < 0.001 | −0.054 | 0.0171 | 0.002 |
| Medication (n)† | −4.88 | 0.771 | < 0.001 | −2.57 | 0.521 | < 0.001 |
Generalized estimating equations (GEE)
Ordinary linear regression (OLR)
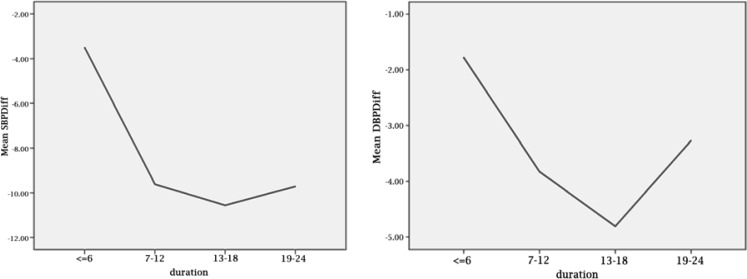
Figure 2.
Systolic and diastolic blood pressure changes during the study
Discussion
We found interventions in workplaces to be effective in reducing both SBP and DBP, especially SBP, among employees and workers. A previous study reported no significant differences in clinical outcomes between hypertensive patients receiving care at workplace from occupational health physicians, patients receiving programmed instructions about hypertension control and adherence, and those receiving a combination of both strategies.21 We used a combination of pharmacological and non-pharmacological recommendations in our educational content. Many studies showed that worksites are appropriate places in which a huge population can be educated about health-related behaviors like overweight and obesity.22 Therefore, in some countries, competitive and consecutive models have been designed and used in controlling hypertension in worksites.21 Like our study, Chen et al. evaluated two previous workplace intervention programs in the Capital Steel Iron Company and Beijing Fangshan Community in China. They indicated that the rates of treatment and control of BP in hypertensive participants in the intervention sites were 98.1% and 72.0%, compared with 51.8% and 37.5% in the control sites, respectively.23
Similar to our program, two other multidisciplinary intervention programs, involving provision of care at the worksite, special pill containers, counseling, reminders, self-monitoring, support groups, feedback and reinforcement reported positive effects on both adherence and clinical outcomes in patients with hypertension.24,25 It seems that having higher educational levels can improve the efficiency of intervention and also drug compliance. Our study population had a high educational level since 78% of them had secondary school education or more.
Our interventions decreased DBP significantly which is different from other studies. However, consistent with IHHP as a whole, we observed significant reductions in other risk factors such as serum triglyceride and cholesterol levels, while BMI did not change among our participants. The reduction in BP might have been caused by the intensive educational interventions or improvement of nonpharmacological treatment and patients' compliance to pharmacological treatment by the assistance of well-trained health professionals. The results of GEE showed the reductions in SBP and DBP to increase over time. OLR also revealed reductions by adding each antihypertensive medication (Table 3). In other words, hypertension was better controlled in patients who took part in our program and were followed for a longer time. Furthermore, adding more drug components could lead to more desirable control, a finding that may support the recent concept of using several components in one pill to increase the compliance of hypertension patients.
Some studies suggested gender-related differences in BP reduction levels. Wu et al. reported an average decrease in SBP by 0.8 mmHg and 4 mmHg respectively for men and women following a workplace intervention program. However, DBP remained the same as baseline for both sexes.26 This finding was not supported by other studies and our study cannot confirm it since we only evaluated male workers and employees. Furthermore, our study showed significant reductions in both SBP and DBP. In contrast, our previous reports showed significant decreases only in SBP while DBP remained constant after implementing the Workplace Project of IHHP in factories and offices in Isfahan and Najaf Abad.16 Several reasons including differences in the dose, type and duration of the interventions, improper design to evaluate the benefits, frequency of follow-up, multidisciplinary approach and a declining trend of hypertension during the intervention period have been attributed to these equivocal results.27–29 Furthermore, less change in DBP than SBP observed in most lifestyle intervention studies can probably be explained by the amount of salt consumption, lack of regular exercise, smoking, and having a family history of hypertension.27 We faced fewer problems with lack of exercise as the majority of positions in Mobarakeh Steel Company are non-sedentary.
Both SBP and DBP reductions were observed until the end of the first year (Figure 2). During the second year however, less change in SBP and an increase in DBP were detected. Less patient compliance and follow-up after the first year seem to be important factors related to these changes. An active reminder system may thus be effective.
Conclusion
SHIMSCO, a Three-year interventional project in workplaces, was effective in reducing SBP and DBP among hypertensive employees and workers. The annual screening of the workers combined with proper management and control by health professionals and appropriate self-care by patients as well as regular worksite follow-up scan would lead to having better control over BP. The project can be applied as a model for management and prevention of other chronic diseases and hence health improvement in large industries.
Acknowledgments
This study was supported by a grant from Mobarakeh Steel Company and Isfahan Cardiovascular Research Institute. We would like to express our sincere thanks to Dr. A. Nazari (director of the occupational health center) and M. Ashtari [Manager of HSE (Health Safty and Environment)]; Mobarakeh Steel Company) as well as all the participating staffs and general physicians of occupational health center.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Sarraf-Zadegan N, Boshtam M, Malekafzali H, Bashardoost N, Sayed-Tabatabaei FA, Rafiei M, et al. Secular trends in cardiovascular mortality in Iran, with special reference to Isfahan. Acta Cardiol. 1999;54(6):327–33. [PubMed] [Google Scholar]
- 2.Sarraf-Zadegan N, Boshtam M, Mostafavi S, Rafiei M. Prevalence of hypertension and associated risk factors in Isfahan, Islamic Republic of Iran. East Mediterr Health J. 1999;5(5):992–1001. [PubMed] [Google Scholar]
- 3.SarrafZadegan N, AminiNik S. Blood pressure pattern in urban and rural areas in Isfahan, Iran. J Hum Hypertens. 1997;11(7):425–8. doi: 10.1038/sj.jhh.1000448. [DOI] [PubMed] [Google Scholar]
- 4.Haynes RB, Sackett DL, Taylor DW. Practical management of low compliance with antihypertensive therapy: a guide for the busy practitioner. Clin Invest Med. 1978;1(3–4):175–80. [PubMed] [Google Scholar]
- 5.Neaton JD, Grimm RH, Prineas RJ, Stamler J, Grandits GA, Elmer PJ, et al. Treatment of Mild Hypertension Study. Final results. Treatment of Mild Hypertension Study Research Group. JAMA. 1993;270(6):713–24. [PubMed] [Google Scholar]
- 6.Runyan JW. The Memphis chronic disease program. Comparisons in outcome and the nurse's extended role. JAMA. 1975;231(3):264–7. [PubMed] [Google Scholar]
- 7.Alderman MH, Schoenbaum EE. Detection and treatment of hypertension at the work site. N Engl J Med. 1975;293(2):65–8. doi: 10.1056/NEJM197507102930203. [DOI] [PubMed] [Google Scholar]
- 8.Therapeutic control of blood pressure in the Hypertension Detection and Follow-up Program Hypertension Detection and Follow-up Program Cooperative Group. Prev Med. 1979;8(1):2–13. doi: 10.1016/0091-7435(79)90024-0. [DOI] [PubMed] [Google Scholar]
- 9.Manuel DG, Lim J, Tanuseputro P, Anderson GM, Alter DA, Laupacis A, et al. Revisiting Rose: strategies for reducing coronary heart disease. BMJ. 2006;332(7542):659–62. doi: 10.1136/bmj.332.7542.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim SS, Gaziano TA, Gakidou E, Reddy KS, Farzadfar F, Lozano R, et al. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet. 2007;370(9604):2054–62. doi: 10.1016/S0140-6736(07)61699-7. [DOI] [PubMed] [Google Scholar]
- 11.Gupta R, Gupta VP. Meta-analysis of coronary heart disease prevalence in India. Indian Heart J. 1996;48(3):241–5. [PubMed] [Google Scholar]
- 12.Gupta A, Lokhandwala Y. Delayed unexplained capture failure. Indian Heart J. 1996;48(4):429. [PubMed] [Google Scholar]
- 13.Gupta R, Gupta VP, Sarna M, Prakash H, Rastogi S, Gupta KD. Serial epidemiological surveys in an urban Indian population demonstrate increasing coronary risk factors among the lower socioeconomic strata. J Assoc Physicians India. 2003;51:470–7. [PubMed] [Google Scholar]
- 14.Mohan V, Shanthirani S, Deepa R, Premalatha G, Sastry NG, Saroja R. Intra-urban differences in the prevalence of the metabolic syndrome in southern India-the Chennai Urban Population Study (CUPS No. 4) Diabet Med. 2001;18(4):280–7. doi: 10.1046/j.1464-5491.2001.00421.x. [DOI] [PubMed] [Google Scholar]
- 15.Khosravi A, Mehr GK, Kelishadi R, Shirani S, Gharipour M, Tavassoli A, et al. The impact of a 6-year comprehensive community trial on the awareness, treatment and control rates of hypertension in Iran: experiences from the Isfahan healthy heart program. BMC Cardiovasc Disord. 2010;10:61. doi: 10.1186/1471-2261-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boshtam M, Zarea K. Effects of 5-year interventions on cardiovascular risk factors of factories and offices emloyees of Isfahan and Najaf Abad: Worksite Intervention Project-Isfahan Healthy Heart Program. ARYA Atherosclerosis J. 2010;6(3):69–74. [PMC free article] [PubMed] [Google Scholar]
- 17.Sarraf-Zadegan N, Sadri G, Malek AH, Baghaei M, Mohammadi FN, Shahrokhi S, et al. Isfahan Healthy Heart Programme: a comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58(4):309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 18.Sarrafzadegan N, Sadri GH, Kelishadi R, Malekafzali H, Boshtam M, Amani A, et al. Isfahan Healthy Heart Program: Evaluation of comprehensive, community-based interventions for non-communicable disease. Prevention and Control J. 2006;2(2):73–84. [Google Scholar]
- 19.Khan NA, McAlister FA, Lewanczuk RZ, Touyz RM, Padwal R, Rabkin SW, et al. The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: part II - therapy. Can J Cardiol. 2005;21(8):657–72. [PubMed] [Google Scholar]
- 20.Dash . 1998. Your guide to lowering your blood pressure with DASH [Online] [cited 2006 Apr]; Available from: URL: www.nhp.nih.gor/heathpublicy/heart/hbp/dash/new_dash.pdf/ [Google Scholar]
- 21.McMahon A, Kelleher CC, Helly G, Duffy E. Evaluation of a workplace cardiovascular health promotion programme in the Republic of Ireland. Health Promot Int. 2002;17(4):297–308. doi: 10.1093/heapro/17.4.297. [DOI] [PubMed] [Google Scholar]
- 22.Van Wier MF, Ariens GA, Dekkers JC, Hendriksen IJ, Pronk NP, Smid T, et al. ALIFE@Work: a randomised controlled trial of a distance counselling lifestyle programme for weight control among an overweight working population [ISRCTN04265725] BMC Public Health. 2006;6:140. doi: 10.1186/1471-2458-6-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen J, Wu X, Gu D. Hypertension and cardiovascular diseases intervention in the capital steel and iron company and Beijing Fangshan community. Obes Rev. 2008;9(Suppl 1):142–5. doi: 10.1111/j.1467-789X.2007.00456.x. [DOI] [PubMed] [Google Scholar]
- 24.Haynes RB, Sackett DL, Gibson ES, Taylor DW, Hackett BC, Roberts RS, et al. Improvement of medication compliance in uncontrolled hypertension. Lancet. 1976;1(7972):1265–8. doi: 10.1016/s0140-6736(76)91737-2. [DOI] [PubMed] [Google Scholar]
- 25.Logan AG, Milne BJ, Achber C, Campbell WP, Haynes RB. Work-site treatment of hypertension by specially trained nurses. A controlled trial. Lancet. 1979;2(8153):1175–8. doi: 10.1016/s0140-6736(79)92397-3. [DOI] [PubMed] [Google Scholar]
- 26.Wu XG, Gu DF, Wu YF, Yu XH, Wang SY, Wang N, et al. An evaluation on effectiveness of worksite-based intervention for cardiovascular disease during 1. Zhonghua Yu Fang Yi Xue Za Zhi. 2003;37(2):93–7. [PubMed] [Google Scholar]
- 27.Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Mannisto S, Sundvall J, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol. 2010;39(2):504–18. doi: 10.1093/ije/dyp330. [DOI] [PubMed] [Google Scholar]
- 28.Sellers DE, Crawford SL, Bullock K, McKinlay JB. Understanding the variability in the effectiveness of community heart health programs: a meta-analysis. Soc Sci Med. 1997;44(9):1325–39. doi: 10.1016/s0277-9536(96)00263-8. [DOI] [PubMed] [Google Scholar]
- 29.Sackett DL, Haynes RB, Gibson ES, Hackett BC, Taylor DW, Roberts RS, et al. Randomised clinical trial of strategies for improving medication compliance in primary hypertension. Lancet. 1975;1(7918):1205–7. doi: 10.1016/s0140-6736(75)92192-3. [DOI] [PubMed] [Google Scholar]