Abstract
Objective
Chronic diseases interfere with the life situation of the affected person in different ways. The aim was to compare the burden of disease in three chronic diseases – chronic obstructive pulmonary disease (COPD), rheumatoid arthritis (RA), diabetes mellitus (DM) – and in healthy subjects, with a particular interest in physical activity, quality of life, and psychological health.
Design
Cross-sectional, observational study.
Setting and subjects
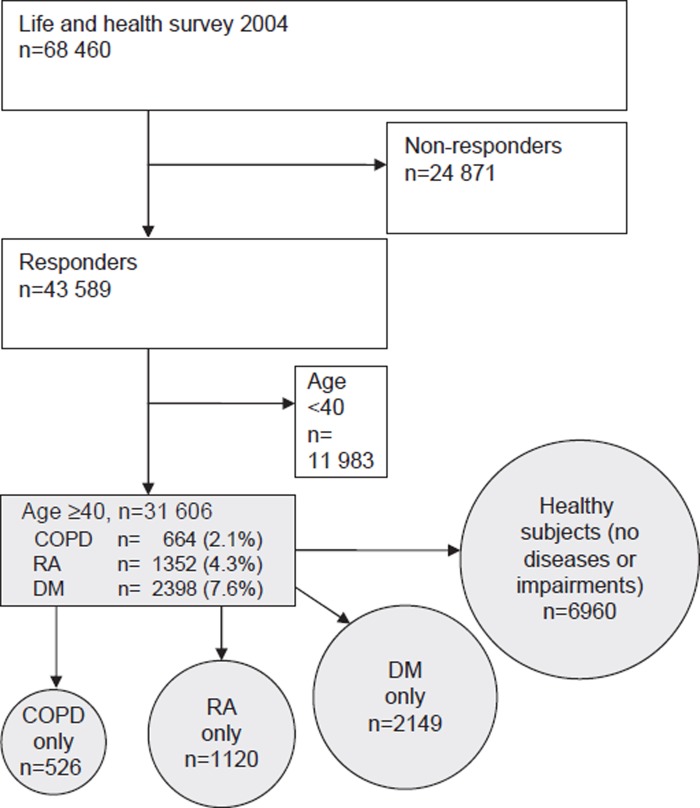
Postal survey questionnaire to a stratified, random population of 68 460 subjects aged 18–84 years in Sweden. The subjects included were 40–84 years old (n = 43 589) and data were analysed for COPD (n = 526), RA (n = 1120), DM (n = 2149) and healthy subjects (n = 6960).
Result
Some 84% of subjects with COPD, 74% (RA), 72% (DM), and 60% in healthy subjects (p < 0.001, COPD versus RA, DM, and healthy subjects) had a physical activity level considered too low to maintain good health according to guidelines. Quality of life (EuroQol five-dimension questionnaire, EQ-5D) was lower in COPD and RA than in DM. Anxiety/depression was more common in subjects with COPD (53%) than in those with RA (48%) and DM (35%) (p < 0.001, COPD versus RA and DM), whereas mobility problems were more common in RA (55%) than COPD (48%) and DM (36%) (p < 0.001, RA versus COPD and DM). All differences between groups remained significant after adjusting for age, sex, and socioeconomic background factors.
Conclusion
Subjects with chronic diseases had a low level of physical activity, most evident in subjects with COPD. COPD and RA had a higher negative impact on quality of life than DM. Our results indicate that increased attention regarding physical inactivity in subjects with chronic diseases is needed to minimize the burden of disease.
Keywords: COPD, diabetes mellitus, family practice, physical activity, quality of life, rheumatoid arthritis
Chronic diseases are important causes of morbidity in the adult population and are often treated in primary care.
In a Swedish population survey, subjects with COPD reported lower general health and level of physical activity than subjects with RA or diabetes mellitus.
Fatigue was a prominent symptom experienced by half of the subjects with COPD or RA.
Subjects with COPD or RA need special attention to physical inactivity, depressive symptoms, and symptoms of fatigue.
Chronic diseases are important causes of morbidity and mortality. An ageing population will result in an increased burden of disease and death. In 2005, all chronic diseases accounted for 72% of the total burden of disease (in terms of disability-adjusted life years, DALYs) in the population aged 30 years and older [1]. Thus, the consequences of chronic diseases are considerable for the well-being of the individual and for society.
Modern treatment of chronic diseases and lifestyle diseases should include promoting of a more healthy lifestyle, i.e. to prevent physical inactivity, tobacco use, and poor food habits [1], [2]. Physical activity is an important factor to prevent and treat chronic diseases [3–6]. It is recommended that physical activity should be performed for a minimum of 30 minutes on five days each week at a moderate intensity level or vigorous intensity aerobic activity for a minimum of 20 minutes on three days each week (or a combination) to promote and maintain health [3]. Health-related quality of life is low in many chronic conditions, and many subjects experience fatigue [7]. Moreover the combination of chronic disease and depression worsens health significantly [8].
No large population-based study has so far investigated and compared the level of physical activity and symptoms in subjects with the common chronic diseases: chronic obstructive pulmonary disease (COPD), rheumatoid arthritis (RA), and diabetes mellitus (DM). With greater knowledge about this, healthcare professionals will have a better ability to improve interventions and hopefully decrease the burden of disease.
The aim of this study was to describe and compare the level of physical activity, health-related quality of life, and psychological health in subjects with chronic obstructive pulmonary disease (COPD), rheumatoid arthritis (RA), and diabetes mellitus (DM), and in healthy subjects in a population-based study.
Material and methods
Data collection and analysis
A survey was performed in a population sample of 68 460 men and women aged 18–84 years. Data were obtained during August–November 2004 using a postal survey questionnaire in Swedish. The area investigated covered 55 municipalities in five counties in central Sweden with approximately one million inhabitants. The sampling was random after stratification for gender, age group, county, and municipality. Data collection was completed after two postal reminders. A total of 43 589 subjects answered the questionnaire. The overall response rate was 64%. Subjects ≥40 years old were included.
The study included subjects with self-reported COPD, RA, DM, and healthy subjects. To separate clearly the effect of each of the three chronic diseases on the measured variables, each disease group excluded all other groups: (1) COPD excluding RA and DM, (2) RA excluding COPD and DM, (3) DM excluding COPD, and RA. “Healthy subjects” consisted of individuals who reported not having any long-term disease, impairments, or other long-term health problem. The general outline of the survey is presented in Figure 1 (for the characteristics of the groups see Table I).
Figure 1.
Selection of the population surveyed. “Only” indicates that the index disease does not include any of the other diseases. Note: COPD = chronic obstructive pulmonary disease, RA = rheumatoid arthritis, DM = diabetes mellitus.
Table I.
Characteristics of the study population aged 40–84 years (n = 10 755).
| Diseases |
||||
| COPD n =526 | RA n =1 120 | DM n =2 149 | Healthy n =6 960 | |
| Age, yrs | 69.1 (68.3–69.9) | 65.4 (64.7–66.1) | 67.5 (67.1–68.0) | 58.0 (57.7–58.3) |
| Sex, females (%) | 44.3 (40.0–48.9) | 64.8 (62.0–67.6) | 42.8 (40.7–44.9) | 52.7 (51.5–53.9) |
| BMI (kg/m2) | 25.4 (25.1–25.8) | 26.2 (26.0–26.5) | 28.3 (28.1–28.6) | 25.3 (25.2–25.4) |
| Smoking status (%) | ||||
| Never smokers | 12.1 (9.3–15.0) | 45.3 (42.4–48.3) | 46.8 (44.7–49.0) | 52.5 (51.4–53.7) |
| Ex-smokers | 53.0 (48.7–57.4) | 31.1 (28.3–33.8) | 39.3 (37.3–41.4) | 27.3 (26.2–28.3) |
| Current smokers | 34.8 (30.7–39.0) | 23.6 (21.1–26.1) | 13.8 (12.3–15.3) | 20.2 (19.2–21.1) |
| Highest educational level (%) | ||||
| Compulsory school | 68.7 (64.7–72.8) | 56.3 (53.3–59.3) | 63.0 (60.9–65.1) | 38.7 (37.5–39.8) |
| Grammar school | 12.0 (9.2–14.9) | 20.8 (18.3–23.2) | 16.0 (14.4–17.6) | 29.8 (28.7–30.9) |
| University | 12.2 (9.3–15.1) | 14.6 (12.5–16.7) | 12.5 (11.1–13.9) | 25.9 (24.8–27.0) |
| Other | 7.0 (4.8–9.3) | 8.3 (6.7–10.0) | 8.4 (7.2–9.6) | 5.6 (5.1–6.2) |
| Employment (%) | ||||
| Employed or studying | 19.0 (15.6–22.4) | 27.1 (24.4–29.7) | 26.2 (24.3–28.1) | 66.6 (65.5–67.8) |
| Sick leave or sickness pension | 13.5 (10.6–16.4) | 18.7 (16.5–21.0) | 10.7 (9.4–12.0) | 1.7 (1.4–2.0) |
| Retired | 66.7 (62.7–70.8) | 52.9 (50.0–55.9) | 59.7 (57.7–61.8) | 28.0 (27.0–29.1) |
| Economic problems (%) | 15.6 (12.4–18.7) | 15.4 (13.3–17.6) | 9.5 (8.3–10.8) | 7.9 (7.2–8.5) |
| Living alone (%) | 36.3 (32.2–40.4) | 29.3 (26.6–32.0) | 26.7 (24.8–28.5) | 17.3 (16.4–18.2) |
Notes: Data are presented as percentage or mean with 95% confidence intervals in parentheses. COPD = chronic obstructive pulmonary disease (not RA, not DM), RA = rheumatoid arthritis (not COPD, not DM), DM = diabetes mellitus (not COPD, not RA), Healthy = subjects with no diseases or impairments, BMI = Body mass index.
Physical activity
Physical activity in leisure time was estimated on a four-category scale indicating (A) sedentary (mostly sitting down or low activity <2 hours a week); (B) moderate exercise (low activity > 2 hours a week); (C) moderate regular exercise (high activity >30 minutes, 1–2 times a week); (D) regular exercise and training (high activity >30 minutes ≥3 times a week) [9]. This variable was dichotomized into low activity level (A and B) and high activity level (C and D) corresponding to the recommended minimum level given by Nelson et al. [3].
Health-related quality of life
General health was assessed with the answer to the question “How do you rate your general health state?” with the alternatives; very good/good/neither good nor poor/poor/very poor [10].
The EuroQol five-dimension questionnaire (EQ-5D) consists of the dimensions mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, each of which offered three possible responses: no problems/some or moderate problems/extreme problems [11]. The index of EQ-5D was computed according to Burström et al. [12], (1 = full health, 0 = death).
Psychological health and symptoms
The General Health Questionnaire (GHQ) is a self-reported questionnaire designed to identify psychological disorders, mainly the anxiety/depression spectrum [13]. In the present study the 12-item version (GHQ12) was used [14]. Scores were calculated from dichotomizing the 12 items (0 = equal or better than usual, 1 = worse than usual), and psychological distress was defined as present when the total score was 3 or higher.
The following symptoms during the past three months were asked for; “anxiety and worry”, “fatigue”, “sleeping problems”, and “depression”. The four response alternatives were “have not been troubled/once in a while/many occasions/all the time”.
A question concerning the subject's view on her/his personal future was asked. The five alternatives were: “very optimistic/rather optimistic/neither optimistic nor pessimistic/rather pessimistic/very pessimistic”.
Subjects answering “Yes” to the question: “Has it happened during the past 12 months that you have had difficulties in managing your current expenditure for food, rent, bills, etc.” were defined as having economic problems.
Statistical methods
The chi-squared test was used to analyse the relationship between categorical variables. The 95% confidence interval was computed for means and proportions. Binary logistic regression was performed to calculate odds ratios adjusted for background data: sex, age, smoking, BMI, educational level, employment status, economic problems, and living alone. Subjects with COPD were compared with RA, DM, and healthy subjects. All statistical tests were two-sided with significance level of 5%. Analyses were carried out using SPSS 15.0 statistical software.
Ethics
According to the Swedish law of medical research ethics, population studies do not require ethical approval. The reason is that the respondent is supposed to have given consent when returning the questionnaire.
Results
Characteristics
Subjects with the three chronic diseases were older than healthy subjects and their educational level and employment status were significantly lower (Table I). There were more men in the COPD and DM groups and more women in the RA group. Current smokers and ex-smokers were most common among subjects with COPD. Economic problems were common for subjects with COPD and RA compared with subjects with DM and healthy individuals. More subjects with COPD lived alone.
Physical activity
Over 84% of the subjects with COPD had a low physical activity level. Compared with subjects with RA, DM, and healthy subjects, this was significantly lower, also when adjusting for background data (Table II).
Table II.
Physical activity level (n = 10 755).
| Diseases |
||||
| COPD n = 526 | RA n = 1120 | DM n = 2149 | Healthy n = 6960 | |
| High activity level1 | 15.8 | 25.6 | 27.5 | 39.8 |
| Low activity level2 | 84.2 | 74.4 | 72.5 | 60.2 |
| OR3 (95% CI) | 1 | 1.80 (1.33–2.45) | 2.17 (1.63–2.90) | 2.49 (1.88–3.28) |
Notes: Data are presented as percentage with odds ratio and 95% confidence intervals within parentheses. COPD = chronic obstructive pulmonary disease, RA = rheumatoid arthritis, DM = diabetes mellitus, OR = odds ratio, CI = confidence interval.
1Moderate regular exercise (high activity >30 minutes, 1–2 times a week) or regular exercise and training (high activity >30 minutes ≥3 times a week),
2sedentary lifestyle (mostly sitting down or low activity <2 hours a week) or moderate exercise (low activity >2 hours a week).
3The adjusted odds ratio expresses the likeliness of higher activity level in the non-COPD groups compared with the COPD group after adjusting for sex, age, smoking, BMI, educational level, employment status, economic problems, and living alone.
Health-related quality of life
General health was rated as poor or very poor by 31% of subjects with COPD and by 29% of subjects with RA, which was significantly higher than in subjects with DM (16%) (p < 0.001). Health-related quality of life, as assessed with the EQ-5D index, was worse (lower index) in subjects with the three chronic diseases compared with healthy subjects (Table III). Subjects with COPD had a significantly lower index than subjects with DM.
Table III.
The EQ-5D index and percentages of subjects reporting any problems (moderate or severe problems) in different dimensions of the EQ-5D (n = 10 755).
| Diseases |
||||
| COPD n = 526 | RA n = 1120 | DM n = 2149 | Healthy n = 6960 | |
| EQ-5D index value, mean (SD) | 0.62 (0.27) | 0.60 (0.27) | 0.72 (0.25) | 0.91 (0.12) |
| Present state of health (EQ-5D), any problems | ||||
| Mobility | 48.4 | 55.3 | 36.1 | 3.6 |
| OR1 (95% CI) | 1 | 1.75 (1.37–2.22) | 0.63 (0.50–0.79) | 0.10 (0.07–0.12) |
| Self-care | 9.1 | 12.1 | 7.2 | 0.3 |
| OR1 (95% CI) | 1 | 1.49 (0.98–2.22) | 0.84 (0.56–1.27) | 0.07 (0.04–0.13) |
| Usual activities | 38.5 | 38.0 | 23.4 | 0.9 |
| OR1 (95% CI) | 1 | 0.93 (0.72–1.20) | 0.48 (0.38–0.62) | 0.03 (0.02–0.04) |
| Pain/Discomfort | 87.3 | 96.1 | 74.8 | 34.8 |
| OR1 (95% CI) | 1 | 3.85 (2.50–5.88) | 0.43 (0.32–0.58) | 0.11 (0.08–0.14) |
| Anxiety/Depression | 52.6 | 47.4 | 34.9 | 15.5 |
| OR1 (95% CI) | 1 | 0.64 (0.50–0.81) | 0.47 (0.38–0.59) | 0.18 (0.14–0.22) |
Notes: Data are presented as mean and standard deviation (SD) or percentage with odds ratio and 95% confidence intervals within parentheses. EQ-5D = the EuroQol five-dimension questionnaire, COPD = chronic obstructive pulmonary disease, RA = rheumatoid arthritis, DM = diabetes mellitus, OR = odds ratio, CI = confidence interval. 1The adjusted odds ratio expresses the likeliness of reporting a problem in the non-COPD groups compared with the COPD group after adjusting for sex, age, smoking, BMI, educational level, employment status, economic problems, and living alone.
Subjects with COPD or RA generally had the highest prevalence of problems in each dimension. Odds ratios adjusted for background data indicated that subjects with COPD had significantly more anxiety/depression problems than the other groups, while subjects with RA had significantly more mobility problems and pain/discomfort than those with COPD and DM.
Psychological health and symptoms
Impaired psychological well-being, measured by GHQ12, was more common among subjects with COPD or RA than among subjects with DM or healthy subjects. Subjects with COPD had a significantly higher level of impairment than any of the other groups (Table IV), after adjusting for background data. Subjects with COPD also had a significantly higher prevalence of anxiety and depression. In addition, they were more likely to have a pessimistic view of the future than any of the other groups. Subjects with COPD or RA had a significantly higher prevalence of sleeping problems and fatigue than subjects with DM or healthy subjects.
Table IV.
Impaired psychological well-being, symptoms past three months, and personal future view (n = 10 755).
| Diseases |
||||
| COPD n = 526 | RA n = 1120 | DM n = 2149 | Healthy n = 6960 | |
| GHQ12 | ||||
| Impaired well-being (score ≥ 3) | 23.3 | 22.6 | 13.3 | 6.8 |
| OR1 (95% CI) | 1 | 0.71 (0.54–0.94) | 0.48 (0.36–0.63) | 0.18 (0.14–0.24) |
| Symptoms past three months | ||||
| Anxiety and worry | ||||
| Many occasions/all the time | 26.3 | 23.3 | 13.7 | 5.9 |
| OR1 (95% CI) | 1 | 0.61 (0.46–0.81) | 0.48 (0.36–0.63) | 0.17 (0.13–0.23) |
| Fatigue | ||||
| Many occasions/all the time | 49.6 | 51.7 | 31.9 | 8.4 |
| OR1 (95% CI) | 1 | 0.91 (0.71–1.16) | 0.49 (0.39–0.61) | 0.10 (0.08–0.13) |
| Sleeping problems | ||||
| Many occasions/all the time | 35.8 | 41.5 | 24.5 | 10.5 |
| OR1 (95% CI) | 1 | 1.12 (0.88–1.43) | 0.66 (0.52–0.84) | 0.26 (0.21–0.33) |
| Depression | ||||
| Many occasions/all the time | 26.1 | 21.8 | 12.7 | 4.0 |
| OR1 (95% CI) | 1 | 0.59 (0.44–0.78) | 0.46 (0.35–0.61) | 0.13 (0.10–0.18) |
| “Personal opinion on your future” | ||||
| Pessimistic | 19.8 | 12.1 | 8.3 | 2.1 |
| OR1 (95% CI) | 1 | 0.47 (0.32–0.68) | 0.36 (0.25–0.51) | 0.09 (0.06–0.12) |
Notes: Data are presented as percentage with odds ratio and 95% confidence intervals within parentheses. COPD = chronic obstructive pulmonary disease, RA = rheumatoid arthritis, DM = diabetes mellitus, GHQ12 = General Health Questionnaire 12-item version, OR = odds ratio, CI = confidence interval. 1The adjusted odds ratio expresses the likeliness of reporting a problem in the non-COPD groups compared with the COPD group after adjusting for sex, age, smoking, BMI, educational level, employment status, economic problems, and living alone.
Gender differences
Women had a significantly higher prevalence of anxiety, depression, and sleep disturbances than men in all disease groups as well as in the group of healthy subjects.
Discussion
In this population-based study of subjects with COPD, RA, DM, and of healthy subjects aged ≥40 years, differences between the groups were found for physical activity, quality of life, and psychological health. Subjects with COPD had the lowest physical activity level followed by subjects with RA, DM, and healthy subjects. In general, subjects with COPD or RA had a lower health-related quality of life and psychological well-being than subjects with DM and healthy subjects.
A strength of the present method is that it is population-based, i.e. health status in subjects in the general population is investigated. This is in contrast to other studies where study groups are mainly recruited from the healthcare system. This study reflects the subjects’ own perceptions of having or not having a diagnosis, which could be a strength but also raises questions about the precision of disease terms. A weakness is that the self-reported diseases in a large sample such as this cannot be validated by physical examinations at a reasonable cost.
The estimated prevalence of COPD at ages over 45 years in Sweden is 5–15% [15], in adults with RA 0.5–2.7% [16], and in adults (25–64 years) with DM 3% [17]. In addition the prevalence of DM increases sharply with increased age [18]. Thus, in our study an over-reporting of RA and under-reporting of COPD is present. Self-reported RA probably includes other polyarthritis, systemic autoimmune diseases, and subjects with arthropathies as well as osteoarthritis, whereas in population-based studies of COPD objective definitions tend to produce higher prevalence estimates than do patient-reported diagnoses [19]. Self-reported DM has in other studies been found to have a high specificity [20]. The high prevalence of DM was therefore probably explained by the relatively high mean age of our population. The higher than expected prevalence of RA and DM indicates that these two groups included individuals with fewer symptoms and thereby a better health status. On the other hand, the prevalence of COPD was lower than expected which implies that there is a selection of subjects with more comorbidity and a lower health status in this diagnostic group. A weakness regarding physical activity is the valuation by a single question describing activity in leisure time. However, physical strain in relation to work is not applicable in this study as 70–80% of the subjects with chronic diseases are either retired, on sick leave, or have a sickness pension. The physical activity question has been shown to be valid for categorizing people into different categories of activity [9].
Other studies confirm that patients with COPD are markedly physically inactive in daily life when compared with healthy subjects [21]. Recommendations encouraging and supporting healthy physical activity for people with RA [22] are motivated by increased mortality rates associated with activity limitation [23], and comorbidity from cardiovascular disease [24]. Recommendations for prevention are similar to therapeutic recommendations for many common diseases, including Type 2 diabetes and osteoarthritis. Evidence is broad and strong in favour of giving physical activity one of the highest priorities for both prevention and treatment of disease and disablement in older adults [3]. Physical activity is highlighted as a major form of treatment modality for DM for example, since disease outcomes are inversely related to regular physical activity in prospective observational studies [25]. The present study suggests that there is room to increase and promote physical activity and give subjects with chronic diseases support from healthcare professionals. The support can for example consist of physical activity on prescription, counselling in behaviour modification, and offering participation in exercise programmes.
Although the present study could not grade the severity of disease, it supports a high prevalence of anxiety and depressive symptoms, especially in subjects with COPD. Chronic medical illnesses have strong associations with anxiety and depression as reported in a review article [26]. Self-perceived depression is also associated with the metabolic syndrome [27]. The prevalence of fatigue in the present study was even higher than that of anxiety and depressive symptoms, with half of subjects with COPD or RA experiencing fatigue on many occasions or all the time. Similarly, in selected samples of patients with COPD, the prevalence of fatigue was of the order of 50% [28]. Fatigue in subjects with COPD has also been described as an important problem affecting daily activities [29].
In conclusion, subjects with chronic diseases often have a low level of physical activity. Of the three diseases, subjects with COPD had the lowest physical activity level. Subjects with COPD or RA reported a higher negative impact on quality of life variables than subjects with DM did. Our results indicate that increased attention regarding physical inactivity in subjects with chronic diseases is needed in order to minimize the burden of disease.
Acknowledgements
This study was supported by research grants from the Swedish Heart-Lung Foundation, the Swedish Heart and Lung Association and the County Council of Värmland.
Conflict of interest statement
No conflict of interest exists for any of the authors.
References
- 1.Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: How many lives can we save? Lancet. 2005;366:1578–82. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]
- 2.Preventing chronic diseases: A vital investment: WHO global report. 2005. [cited 3 February 2009]; Available at: http://www.who.int/chp.
- 3.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–45. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 4.Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C, White RD. Physical activity/exercise and type 2 diabetes: A consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:1433–8. doi: 10.2337/dc06-9910. [DOI] [PubMed] [Google Scholar]
- 5.Stenström CH, Minor MA. Evidence for the benefit of aerobic and strengthening exercise in rheumatoid arthritis. Arthritis Rheum. 2003;49:428–34. doi: 10.1002/art.11051. [DOI] [PubMed] [Google Scholar]
- 6.Pedersen BK, Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scand J Med Sci Sports. 2006;16:3–63. doi: 10.1111/j.1600-0838.2006.00520.x. [DOI] [PubMed] [Google Scholar]
- 7.Ream E, Richardson A. Fatigue: A concept analysis. Int J Nurs Stud. 1996;33:519–29. doi: 10.1016/0020-7489(96)00004-1. [DOI] [PubMed] [Google Scholar]
- 8.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet. 2007;370:851–8. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 9.Ekelund U, Sepp H, Brage S, Becker W, Jakes R, Hennings M, et al. Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutrition. 2006;9:258–65. doi: 10.1079/phn2005840. [DOI] [PubMed] [Google Scholar]
- 10.Molarius A, Berglund K, Eriksson C, Lambe M, Nordstrom E, Eriksson HG, et al. Socioeconomic conditions, lifestyle factors, and self-rated health among men and women in Sweden. Eur J Public Health. 2006;17:125–33. doi: 10.1093/eurpub/ckl070. [DOI] [PubMed] [Google Scholar]
- 11. EQ–5D; An instrument to describe and value health [cited 3 February 2009]; Available at: http://www.euroqol.org.
- 12.Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res. 2001;10:621–35. doi: 10.1023/a:1013171831202. [DOI] [PubMed] [Google Scholar]
- 13.Kilic C, Rezaki M, Rezaki B, Kaplan I, Ozgen G, Sagduyu A, et al. General Health Questionnaire (GHQ12 & GHQ28): Psychometric properties and factor structure of the scales in a Turkish primary care sample. Soc Psychiatry Psychiatr Epidemiol. 1997;32:327–31. doi: 10.1007/BF00805437. [DOI] [PubMed] [Google Scholar]
- 14.McDowell I. Newell C. Measuring health: A guide to rating scales and questionnaires. 2nd ed. New York:: Oxford University Press; 1996. [Google Scholar]
- 15.Lindberg A, Bjerg A, Rönmark E, Larsson L, Lundbäck B. Prevalence and underdiagnosis of COPD by disease severity and the attributable fraction of smoking: Report from the Obstructive Lung Disease in Northern Sweden Studies. Respir Med. 2006;100:264–72. doi: 10.1016/j.rmed.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 16.Simonsson M, Bergman S, Jacobsson L, Petersson I, Svensson B. The prevalence of rheumatoid arthritis in Sweden. Scand J Rheumatol. 1999;28:340–3. doi: 10.1080/03009749950155319. [DOI] [PubMed] [Google Scholar]
- 17.Eliasson M, Lindahl B, Lundberg V, Stegmayr B. No increase in the prevalence of known diabetes between 1986 and 1999 in subjects 25–64 years of age in northern Sweden. Diabet Med. 2002;19:874–80. doi: 10.1046/j.1464-5491.2002.00789.x. [DOI] [PubMed] [Google Scholar]
- 18.Jansson SP, Andersson DK, Svardsudd K. Prevalence and incidence rate of diabetes mellitus in a Swedish community during 30 years of follow-up. Diabetologia. 2007;50:703–10. doi: 10.1007/s00125-007-0593-4. [DOI] [PubMed] [Google Scholar]
- 19.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: Systematic review and meta-analysis. Eur Respir J. 2006;28:523–32. doi: 10.1183/09031936.06.00124605. [DOI] [PubMed] [Google Scholar]
- 20.Nilsson PM, Roost M, Engstrom G, Hedblad B, Berglund G. Incidence of diabetes in middle-aged men is related to sleep disturbances. Diabetes Care. 2004;27:2464–9. doi: 10.2337/diacare.27.10.2464. [DOI] [PubMed] [Google Scholar]
- 21.Pitta F, Troosters T, Spruit MA, Probst VS, Decramer M, Gosselink R. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171:972–7. doi: 10.1164/rccm.200407-855OC. [DOI] [PubMed] [Google Scholar]
- 22.Eurenius E, Stenstrom CH. Physical activity, physical fitness, and general health perception among individuals with rheumatoid arthritis. Arthritis Rheum. 2005;53:48–55. doi: 10.1002/art.20924. [DOI] [PubMed] [Google Scholar]
- 23.Wolfe F, Michaud K, Gefeller O, Choi HK. Predicting mortality in patients with rheumatoid arthritis. Arthritis Rheum. 2003;48:1530–42. doi: 10.1002/art.11024. [DOI] [PubMed] [Google Scholar]
- 24.Wolfe F, Freundlich B, Straus WL. Increase in cardiovascular and cerebrovascular disease prevalence in rheumatoid arthritis. J Rheumatol. 2003;30:36–40. [PubMed] [Google Scholar]
- 25.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 26.Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29:147–55. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 27.Miettola J, Niskanen LK, Viinamäki H, Kumpusalo E. Metabolic syndrome is associated with self-perceived depression. Scand J Prim Health Care. 2008;26:203–10. doi: 10.1080/02813430802117624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Theander K, Unosson M. Fatigue in patients with chronic obstructive pulmonary disease. J Adv Nurs. 2004;45:172–7. doi: 10.1046/j.1365-2648.2003.02878.x. [DOI] [PubMed] [Google Scholar]
- 29.Kapella MC, Larson JL, Patel MK, Covey MK, Berry JK. Subjective fatigue, influencing variables, and consequences in chronic obstructive pulmonary disease. Nurs Res. 2006;55:10–17. doi: 10.1097/00006199-200601000-00002. [DOI] [PubMed] [Google Scholar]