Abstract
Objective
To describe general practitioners’ (GPs’) evaluation of and management strategies in relation to patients who seek medical advice because of multiple chemical sensitivity (MCS).
Design
A nationwide cross-sectional postal questionnaire survey. The survey included a sample of 1000 Danish GPs randomly drawn from the membership list of GPs in the Danish Medical Association.
Setting
Denmark.
Results
Completed questionnaires were obtained from 691 GPs (69%). Within the last 12 months 62.4% (n = 431) of the GPs had been consulted by at least one patient with MCS. Of these, 55.2% of the GPs evaluated the patients’ complaints as chronic and 46.2% stated that they were rarely able to meet the patients’ expectations for healthcare. The majority, 73.5%, had referred patients to other medical specialties. The cause of MCS was perceived as multi-factorial by 64.3% of the GPs, as somatic/biologic by 27.6%, and as psychological by 7.2%. Partial or complete avoidance of chemical exposures was recommended by 86.3%. Clinical guidelines, diagnostic tools, or more insight in the pathophysiology were requested by 84.5% of the GPs.
Conclusion
Despite the lack of formal diagnostic labelling the patient with MCS is well known by GPs. The majority of the GPs believed that MCS primarily has a multi-factorial explanation. However, perceptions of the course of the condition and management strategies differed, and many GPs found it difficult to meet the patients’ expectations for healthcare. The majority of the GPs requested more knowledge and clinical guidelines for the management of this group of patients.
Keywords: Family practice, general practitioner, healthcare management, multiple chemical sensitivity, MCS, primary healthcare
Knowledge of management strategies among GPs in relation to provision of healthcare for patients who attribute symptoms to common airborne chemicals is limited.
Despite the lack of formal diagnostic labelling the patient with multiple chemical sensitivity (MCS) is well known by GPs, but many find it difficult to meet the expectations for healthcare expressed by these patients.
The majority of the GPs advise patients to avoid partial or complete exposure to common airborne chemicals.
There is a need for research to generate evidence for recommendations and management strategies in relation to this group of patients.
Multiple chemical sensitivity (MCS) is a condition characterized by a range of non-specific somatic and cognitive symptoms which the patient attributes to common airborne chemicals [1]. More case definitions have been suggested but there are no internationally accepted criteria [2–4]. Despite research within different areas of medicine, findings concerning the aetiology of MCS have largely remained inconsistent [1], [5] and although a recent prospective study suggests that MCS may be a chronic and disabling condition [6] the course is still poorly understood.
It has been suggested that MCS is best understood within the spectrum of functional somatic syndromes due to the reporting of non-specific symptoms and findings of high rates of psychiatric disorders in patients who report these symptoms [7]. More studies have examined this hypothesis by evaluating the association between personality traits typically associated with functional somatic syndromes and MCS [6], [8]. These studies have provided some evidence for a role of personality traits in some cases of MCS.
The controversy and lack of diagnostic possibilities may challenge the healthcare system and result in different management strategies depending on empirical knowledge and attitudes towards MCS. Denmark has a tax-financed public healthcare system and the general practitioner (GP) acts as gatekeeper to more areas of the healthcare system. Insight into GPs’ experience with MCS and the strategies they apply in consultations with patients who report these symptoms is limited. However, the subject is important in terms of describing the current practice, knowledge, and future demands among GPs in relation to provision of healthcare for this group of patients.
The objectives of the present study were to describe (1) whether GPs are familiar with patients who seek medical advice because of self-reported MCS, (2) GPs’ referral practice and their clinical advice to patients on how to manage the condition, (3) their perceptions of aetiology and prognosis, (4) their ability to meet the patients’ expectations for healthcare, and (5) requests in relation to provision of healthcare to patients who report MCS.
Material and methods
Participants
In February 2007 a nationwide cross-sectional postal questionnaire survey was carried out including 1000 Danish GPs. Participants were randomly selected from the Medical Associations member list that contains all (approximately 3600) GPs in Denmark. The selection criterion was at least one year of experience as GP.
Questionnaire
A questionnaire was developed in collaboration between the authors of this article. The questionnaire included 11 questions. Two initial questions on gender and length of working experience as a GP were followed by nine questions on: estimated frequency of consultations with this group of patients, perceptions of aetiology and prognosis, referral practice, type of information provided, patients’ satisfaction with consultations, and clinical requests. The term “MCS” was not used in the questionnaire but after the initial two questions examples of eliciting agents were provided as follows: The following nine questions concern patients who seek medical advice because of symptoms attributed to inhalation of common airborne chemicals (e.g. perfume, freshly printed papers or magazines, or new furniture). In a covering letter the GPs were informed about the study. The questionnaire was pilot tested for relevance, comprehension, and ease of completion by individual interviews with eight GPs, resulting in minor linguistic adjustments.
Collection of data
All questionnaire data were double entered in SPSS Data Entry Builder 4.0. Mismatch was identified and corrected by comparing the two data files. Missing values in the final data sheet were those with blank answers.
Statistical analysis
Data were analysed using SPSS 15.0 for Windows. Groups were compared using χ2 test and independent sample t-test. Statistical significance was defined as p < 0.05.
Approval
The study was approved by the Research Committee of the Danish College of General Practitioners. The study was reported to the Danish Data Protection Agency but did not need approval.
Results
Completed questionnaires were obtained from 691 GPs (69%) after one reminder. Among the respondents 37.9% (n = 262) were women, which corresponds to the sex distribution among non-responders with OR 1.18 (0.9–1.57, 95 %CI).
Within the last 12 months 62.5% (n = 431/691) of the GPs had been consulted by at least one patient with symptoms that were attributed to common airborne chemicals. No differences in sex (p = 0.5) between GPs who had been consulted (36.9% women) and who had not been consulted (39.6% women) was found. Years of experience of general practice among the 431 GPs were 15.4 years (SD 9.2) which did not differ from the length of experience among respondents who reported not having seen such a patient (15.2 years, SD 9.4, p = 0.8).
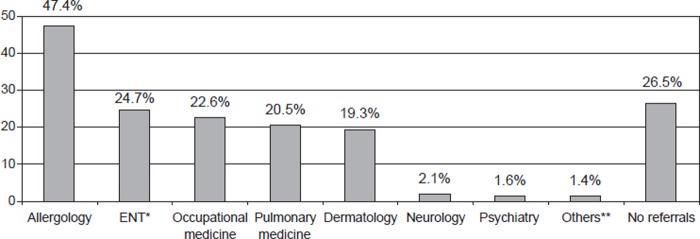
Referrals to other medical specialties were reported by 73.5% (n = 317/431) with allergology being the most frequent specialty that GPs referred to and psychiatry the least frequent (Figure 1). Regarding the question about ability to meet patients’ expectations for healthcare, 46.2% of the GPs reported experiencing that they were rarely able to meet the patients’ expectations (Table I). In terms of aetiology 64.3% of the GPs perceived the symptoms as multi-factorial, 27.6% believed the symptoms primarily had a somatic/biologic explanation, and 7.2% that the symptoms primarily had a psychological explanation (Table I). Male GPs as compared with females ascribed a psychological explanation for the symptoms more frequently, OR 2.6 (95% CI 1.0–6.5). No differences were found between GPs’ attitudes in terms of their perceptions of aetiology and their recommendations to patients. The majority recommended either partial or complete avoidance of chemical exposures (Table I). However, those GPs who recommended the patients not to avoid exposure to common airborne chemicals (n = 12) were significantly more likely (p < 0.05) to perceive the condition as psychological. The condition was described as chronic by 55.2% of the GPs. Clinical guidelines were requested by 52.9% of the GPs and diagnostic tools by 59.4%. More insight into the pathophysiology of MCS was requested by 43.6% and altogether 84.5% requested either of the above.
Figure 1.
Proportion of GPs who have referred patients reporting symptoms attributed to common airborne chemicals to other medical specialties in order of frequency (responses to the question on referral practice were given by ticking off a list of the medical specialties presented in Figure 1. Each GP could tick off more than one medical specialty). Values are shown as percentages of the 431 respondents who had seen at least one patient within the last 12 months.Notes: *Ear-Nose-Throat specialists. **Other specialists such as psychologists.
Table I.
GPs’ experiences with patients who report symptoms attributed to common airborne chemicals.
GPs consulted by at least one patient with symptoms attributed to common airborne chemicals within the last 12 months (n = 431).
| Evaluation of experiences with: | n (% of total) |
| Ability to meet patients’ expectations for health are: | |
| Most often | 93 (21.6) |
| Rarely | 199 (46.2) |
| Do not know | 136 (31.6) |
| Missing | 3 (0.7) |
| Aetiology: | |
| Somatic/biological | 119 (27.6) |
| Multi-factorial | 277 (64.3) |
| Psychological | 31 (7.2) |
| Missing | 4 (0.9) |
| Course of symptoms: | |
| Most often reversible | 44 (10.2) |
| Chronic | 238 (55.2) |
| Do not know | 148 (34.3) |
| Missing | 1 (0.2) |
| Clinical advice for the patients: | |
| Avoid chemical exposures associated with symptoms | 321 (74.5) |
| Avoid all exposure to chemicals | 51 (11.8) |
| Do not avoid chemical exposures | 12 (2.8) |
| No clinical advice for these patients | 44 (10.2) |
| Missing | 3 (0.7) |
Discussion
Despite the diagnostic uncertainty our data suggest that MCS is well known by Danish GPs. Overall the results point to a pragmatic approach among GPs in relation to both attitude towards MCS and clinical advice on how to manage the condition. Nevertheless many GPs find it difficult to meet the expectations for healthcare expressed by these patients and the majority request more knowledge and diagnostic tools.
Since there is no accepted case definition we chose to include a brief case description using examples of symptom-eliciting agents in the questionnaire instead of the term “MCS”. This might have given rise to bias in the GPs’ interpretation of the group of patients the questionnaire was referring to and instead they may have answered from a more general perspective on patients who report non-specific somatic and cognitive symptoms. Recall bias is another possible issue to consider when interpreting the present data since we asked the GPs to describe their clinical practice retrospectively. However, the high response rate (69%) may suggest that the GPs recognize this patient and the questionnaire was pilot-tested by conducting individual interviews with GPs, and found to be relevant, comprehensive, and easy to complete.
The number of non-responders to the questionnaire was 31% and given the diagnostic uncertainty of MCS the non-response rate could be high in GPs with no or less experience in MCS. This may have biased our results and led to an overestimation of the extent of the problem in primary healthcare. We have no data on non-responders but the response rate was high, and despite the possible limitations we believe that the present data provide insight into attitudes among Danish GPs and management strategies in relation to MCS.
The diagnostic uncertainty of MCS is likely to leave the question of management strategies to be determined by the individual patients’ reports, and the empirical knowledge of the GP. The majority of the GPs perceived the aetiology of MCS as multi-factorial, indicating a pragmatic approach to these patients. Dichotomization of medically unexplained symptoms in either organic or functional terms may be difficult [9] and it has been reported that symptoms with a biomedical explanation coexist with unexplained symptoms in a ratio of 1 to 4 [9]. Almost half (47.4%) of the GPs who had seen at least one patient within the last 12 months had referred such patients to other medical specialities with allergology being the most common, and psychiatry the least common speciality. Respiratory symptoms and skin problems are prevalent in people who report these symptoms [10], and respiratory symptoms attributed to fragrance products have been associated with perfume contact allergy, hand eczema, and asthma [11]. Moreover, reporting of symptoms has been associated with social and occupational restraints [10], [12], and self-reported initial onset includes stress and factors in the indoor environment [10]. This could offer some explanation for the list of medical specialities that GPs report referring to. Studies have reported that anxiety, somatisation, and depressive symptoms are more frequent among people who report these symptoms when compared with a normal population [13–15]. Trait anxiety and somatic attribution have been suggested to contribute to the maintenance of symptoms and influence the course of the condition [6]. However, the number of GPs who reported having referred to a psychiatrist was low when compared with other specialities.
It has been suggested that MCS overlap with other descriptive conditions such as chronic fatigue syndrome, and thus in terms of classification, belong to a larger group of functional somatic syndromes [16], [17]. However, uncertainty seems to exist regarding the diagnostic criteria for somatoform disorders in both DSM-IV and ICD-10 since a diagnosis is not based on positive criteria but on the exclusion of organic disease, and is not supported by substantial empirical evidence [18]. In other areas of medicine labels like sensory hyper-reactivity[19] or descriptive terms like MCS or idiopathic environmental intolerance (IEI) are common [2], [20]. At this point it may seem that arguments for labelling MCS as a functional somatic disorder are not sufficiently supported by the current criteria. Whether a diagnostic label benefits patients who suffer from unclarified disorders is debatable [21]. However, it has been suggested that a label that respects the patients’ perceptions of the condition is both pragmatically and instrumentally the most reasonable approach [17].
Treatment and recommendations are more important issues in the management of MCS. Psychological/behavioural approaches have been suggested in order for the patient to gradually learn to tolerate exposure to common airborne chemicals [1]. In the present study 2.8% of the GPs advised the patients not to avoid being exposed, which would be in accordance with the understanding of MCS as a functional somatic disorder [22]. As opposed to this 11.8% of the GPs advised their patients to avoid all exposure. MCS has in some cases been associated with social and occupational restraints [10], and suggesting complete avoidance might promote social and occupational restraints and eventually lead to a more disabling condition. The majority (74.5%) of the GPs advised the patients only to avoid exposure to the chemicals that provoked symptoms, which may again seem the most pragmatic approach and at this point perhaps the most acceptable advice to offer patients as long as the implications for daily life are manageable. This apparent dilemma suggests a need for further research and cooperation between different areas of medicine in order to provide evidence-based guidelines for the future management of MCS. It seems especially relevant to clarify the possible effects of psychological/behavioural approaches as suggested by Jayati Das-Munshi el al., since elevated scores on psychometric scales for, for example, somatisation and depression that may perpetuate the condition have been reported in other studies [6], [14], [23], [24].
In terms of expectations for healthcare 46.2% of the GPs reported that they were rarely able to meet the expectations expressed by these patients. The majority of the GPs requested clinical guidelines and diagnostic tools which further warrant more research in order to provide more optimal management options.
Conclusion
Patients who report MCS are well known by Danish GPs. Most GPs perceive the cause to be multi-factorial and recommend either partial or complete avoidance of exposure to chemicals. Many GPs find it difficult to meet the expectations for healthcare expressed by these patients, and evidence-based guidelines and diagnostic tools are needed.
References
- 1.Das-Munshi J, Rubin GJ, Wessely S. Multiple chemical sensitivities: Review. Curr Opin Otolaryngol Head Neck Surg. 2007;15:274–80. doi: 10.1097/MOO.0b013e328259c360. [DOI] [PubMed] [Google Scholar]
- 2.Cullen MR. The worker with multiple chemical sensitivities: An overview. Occup Med. 1987;2:655–61. [PubMed] [Google Scholar]
- 3.Lacour M, Zunder T, Schmidtke K, Vaith P, Scheidt C. Multiple chemical sensitivity syndrome (MCS) – suggestions for an extension of the U.S. MCS-case definition. Int J Hyg Environ Health. 2005;208:141–51. doi: 10.1016/j.ijheh.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 4.Multiple chemical sensitivity: A 1999 consensus. Arch Environ Health. 1999;54:147–9. doi: 10.1080/00039899909602251. [DOI] [PubMed] [Google Scholar]
- 5.Das-Munshi J, Rubin GJ, Wessely S. Multiple chemical sensitivities: A systematic review of provocation studies. J Allergy Clin Immunol. 2006;118:1257–64. doi: 10.1016/j.jaci.2006.07.046. [DOI] [PubMed] [Google Scholar]
- 6.Bailer J, Witthoft M, Rist F. Psychological predictors of short- and medium term outcome in individuals with idiopathic environmental intolerance (IEI) and individuals with somatoform disorders. J Toxicol Environ Health A. 2008;71:766–75. doi: 10.1080/15287390801985562. [DOI] [PubMed] [Google Scholar]
- 7.Bornschein S, Forstl H, Zilker T. Idiopathic environmental intolerances (formerly multiple chemical sensitivity) psychiatric perspectives. J Intern Med. 2001;250:309–21. doi: 10.1046/j.1365-2796.2001.00870.x. [DOI] [PubMed] [Google Scholar]
- 8.Witthoft M, Rist F, Bailer J. Evidence for a specific link between the personality trait of absorption and idiopathic environmental intolerance. J Toxicol Environ Health A. 2008;71:795–802. doi: 10.1080/15287390801985687. [DOI] [PubMed] [Google Scholar]
- 9.Aiarzaguena JM, Grandes G, Salazar A, Gaminde I, Sanchez A. The diagnostic challenges presented by patients with medically unexplained symptoms in general practice. Scand J Prim Health Care. 2008;26:99–105. doi: 10.1080/02813430802048662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berg ND, Linneberg A, Dirksen A, Elberling J. Prevalence of self-reported symptoms and consequences related to inhalation of airborne chemicals in a Danish general population. Int Arch Occup Environ Health. 2008;81:881–7. doi: 10.1007/s00420-007-0282-0. [DOI] [PubMed] [Google Scholar]
- 11.Elberling J, Linneberg A, Mosbech H, Dirksen A, Frolund L, Madsen F, Nielsen NH, Johansen JD. A link between skin and airways regarding sensitivity to fragrance products? Br J Dermatol. 2004;151:1197–1203. doi: 10.1111/j.1365-2133.2004.06251.x. [DOI] [PubMed] [Google Scholar]
- 12.Koch L, Rumrill P, Hennessey M, Vierstra C, Roessler RT. An ecological approach to facilitate successful employment outcomes among people with multiple chemical sensitivity. Work. 2007;29:341–9. [PubMed] [Google Scholar]
- 13.Eis D, Helm D, Muhlinghaus T, Birkner N, Dietel A, Eikmann T, et al. The German Multicentre Study on multiple chemical sensitivity (MCS) Int J Hyg Environ Health. 2008;211:658–81. doi: 10.1016/j.ijheh.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Bailer J, Witthoft M, Bayerl C, Rist F. Syndrome stability and psychological predictors of symptom severity in idiopathic environmental intolerance and somatoform disorders. Psychol Med. 2007;37:271–81. doi: 10.1017/S0033291706009354. [DOI] [PubMed] [Google Scholar]
- 15.Osterberg K, Persson R, Karlson B, Carlsson EF, Orbaek P. Personality, mental distress, and subjective health complaints among persons with environmental annoyance. Hum Exp Toxicol. 2007;26:231–41. doi: 10.1177/0960327107070575. [DOI] [PubMed] [Google Scholar]
- 16.Fink P, Toft T, Hansen MS, Ornbol E, Olesen F. Symptoms and syndromes of bodily distress: An exploratory study of 978 internal medical, neurological, and primary care patients. Psychosom Med. 2007;69:30–9. doi: 10.1097/PSY.0b013e31802e46eb. [DOI] [PubMed] [Google Scholar]
- 17.Kanaan RA, Lepine JP, Wessely SC. The association or otherwise of the functional somatic syndromes. Psychosom Med. 2007;69:855–9. doi: 10.1097/PSY.0b013e31815b001a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowe B, Mundt C, Herzog W, Brunner R, Backenstrass M, Kronmuller K, et al. Validity of current somatoform disorder diagnoses: Perspectives for classification in DSM-V and ICD-11. Psychopathology. 2008;41:4–9. doi: 10.1159/000109949. [DOI] [PubMed] [Google Scholar]
- 19.Johansson A, Millqvist E, Nordin S, Bende M. Relationship between self-reported odor intolerance and sensitivity to inhaled capsaicin: Proposed definition of airway sensory hyperreactivity and estimation of its prevalence. Chest. 2006;129:1623–8. doi: 10.1378/chest.129.6.1623. [DOI] [PubMed] [Google Scholar]
- 20.Carlsson F, Karlson B, Orbaek P, Osterberg K, Ostergren PO. Prevalence of annoyance attributed to electrical equipment and smells in a Swedish population, and relationship with subjective health and daily functioning. Public Health. 2005;119:568–77. doi: 10.1016/j.puhe.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 21.Undeland M, Malterud K. The fibromyalgia diagnosis: Hardly helpful for the patients? A qualitative focus group study. Scand J Prim Health Care. 2007;25:250–5. doi: 10.1080/02813430701706568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Magill MK, Suruda A. Multiple chemical sensitivity syndrome. Am Fam Physician. 1998;58:721–8. [PubMed] [Google Scholar]
- 23.Papo D, Eberlein-Konig B, Berresheim HW, Huss-Marp J, Grimm V, Ring J, et al. Chemosensory function and psychological profile in patients with multiple chemical sensitivity: Comparison with odor-sensitive and asymptomatic controls. J Psychosom Res. 2006;60:199–209. doi: 10.1016/j.jpsychores.2005.06.075. [DOI] [PubMed] [Google Scholar]
- 24.Simon GE, Daniell W, Stockbridge H, Claypoole K, Rosenstock L. Immunologic, psychological, and neuropsychological factors in multiple chemical sensitivity: A controlled study. Ann Intern Med. 1993;119:97–103. doi: 10.7326/0003-4819-119-2-199307150-00001. [DOI] [PubMed] [Google Scholar]