Video abstract
Video
Keywords: prophylactic collagen cross-linking, laser-assisted in situ keratomileusis, high-risk, post-LASIK ectasia
Abstract
Background
The purpose of this study was to evaluate the safety and efficacy of ultraviolet A irradiation cross-linking on completion for cases of high myopic laser-assisted in situ keratomileusis (LASIK).
Methods
Forty-three consecutive LASIK cases treated with femtosecond laser flap and the WaveLight excimer platform were evaluated perioperatively for uncorrected visual acuity, best corrected spectacle visual acuity, refraction, keratometry, topography, total and flap pachymetry, corneal optical coherence tomography, and endothelial cell count. All eyes at the completion of LASIK had cross-linking through the repositioned flap, with higher fluence (10 mW/cm2) ultraviolet light of an average 370 μm wavelength and 10 mW/cm2 fluence applied for 3 minutes following an earlier single instillation of 0.1% riboflavin within the flap interface. Mean follow-up duration was 3.5 (range 1.0–4.5) years.
Results
Mean uncorrected visual acuity changed from 0.2 to 1.2, best corrected spectacle visual acuity from 1.1 to 1.2, spherical equivalent from −7.5 diopters (D) to −0.2 D, keratometry from 44.5 D to 38 D, flap pachymetry from 105 μm to, total pachymetry from 525 to 405, and endothelial cell count from 2750 to 2800. None of the cases developed signs of ectasia or significant regression during follow-up.
Conclusion
Prophylactic collagen cross-linking for high-risk LASIK cases appears to be a safe and effective adjunctive treatment for refractive regression and potential ectasia. This application may be viewed as prophylactic customization of the biomechanical behavior of corneal collagen.
Introduction
Ectasia is a well recognized and serious complication following laser-assisted in situ keratomileusis (LASIK).1,2 Several risk factors and preventive measures for ectasia have been identified and investigated.3–8 A number of treatment modalities have been historically described, and include contact lenses,9 intracorneal ring segments,10 conductive keratoplasty,11 and, more recently, collagen cross-linking.12–14
We have introduced the concept of collagen cross-linking in post-LASIK ectasia,12,13 and have had long experience in utilizing novel cross-linking techniques following progressive keratoconus and ectasia. We have also pioneered the concept of prophylactic cross-linking after LASIK and photorefractive keratectomy, largely as a result of practicing in a patient population that appears to have a high rate of keratoconus. We have discovered that several patients whom we have treated in the past with LASIK had siblings or close relatives with topographically or tomographically diagnosed keratoconus that we did not know of at the time of the original LASIK procedure. We have also reported on performing in situ intrastromal higher fluence cross-linking in progressive keratoconus and corneal edema facilitated by a femtosecond laser-created intrastromal pocket.15,16 We used CXL in a prophylactic fashion in this consecutive case series.
Materials and methods
All patients provided their written informed consent prior to treatment, in agreement with the tenets of the Declaration of Helsinki. These were 23 consecutive LASIK patients with high myopia and/or myopic astigmatism, defined as myopia > −6 diopters (D) of spherical equivalent. All cases had a 110 μm LASIK flap created with the IntraLase FS60 femtosecond laser (Abbott Medical Optics, Irvine, CA) and LASIK ablation using the WaveLight 400 Hz IQ excimer laser (WaveLight, Erlagen, Germany). Perioperatively, we evaluated uncorrected distance visual acuity, corrected distance visual acuity, subjective refraction, keratometry, Placido disc-generated corneal topography (Topolyzer, WaveLight), Scheimpflug-generated corneal topometry (Oculyzer, WaveLight) intraoperative subtraction flap ultrasound pachymetry (Sonogage, Cleveland, OH), corneal optical coherence tomography (Optovue, W Fremont, CA), and preoperative and postoperative endothelial cell counts.
Surgical technique
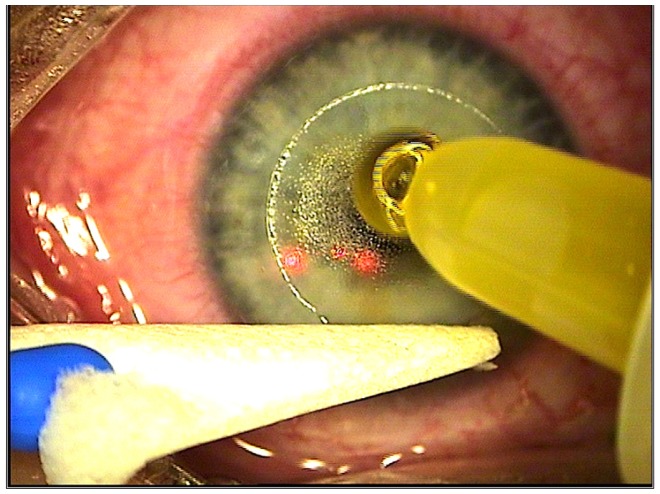
On completion of the LASIK excimer ablation procedure, a drop of customized 0.1% riboflavin sodium phosphate solution (Leiter’s Pharmcy, San Jose, CA) was placed on the bare stromal bed, and left to soak in for 60 seconds. Special care was taken not to allow the riboflavin solution to come into contact with the already folded LASIK flap (Figure 1). After the 60-second riboflavin soak, the LASIK flap was reflected into place, copiously irrigated, and ironed with a Johnston applanator (Rhein Medical, St Petersburg, FL). Figure 2 shows the LASIK flap repositioned and the riboflavin yellow tinge visualized within the corneal stroma.
Figure 1.
Riboflavin solution applied over the bare stroma without contact with the LASIK flap for 60 seconds.
Abbreviation: LASIK, laser-assisted in situ keratomileusis.
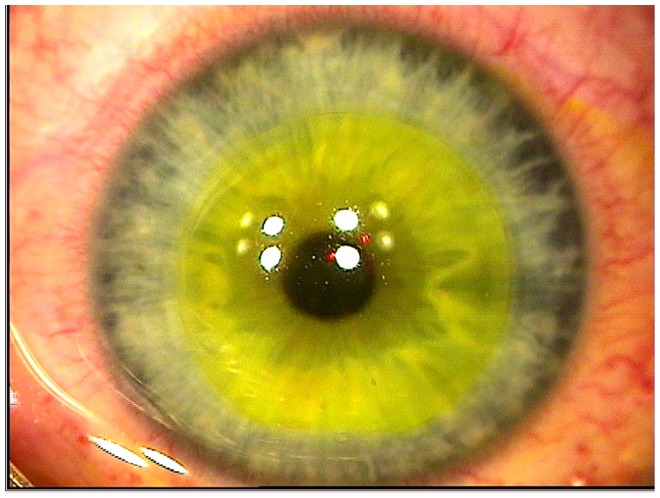
Figure 2.
Flap is repositioned, and the riboflavin-yellow tinge is visualized in the corneal stroma prior to application of higher fluence ultraviolet light.
Following flap repositioning, the surface was kept moist with a drop of ofloxacin solution (Ocuflox®, Allergan, Dublin, Ireland) and irradiated with 10 mW/cm2 ultraviolet light (Priavision, Menlo Park, CA) of average wavelength 370 nm, for a total of three minutes. No further drops of riboflavin were administered. During the ultraviolet irradiation phase, the corneal surface was kept moist with a few drops of ofloxacin solution.
A bandage contact lens was then placed on the ocular surface and the patient was treated with ofloxacin and 0.1% dexamethasone solution four times a day for a week. Patients were followed up on the first day following contact lens removal. Further follow-up examinations were performed at the end of week 1, months 1, 3, and 6, and annually thereafter.
Results
The mean age of the patients was 26 ± 7 years, with 14 being female and nine being male. Mean uncorrected distance visual acuity showed an improvement from 0.2 ± 0.2 to 1.2 ± 0.07 logMAR. Best spectacle-corrected visual acuity to corrected distance visual acuity improved from 1.1 ± 0.8 to 1.2 ± 0.9. Spherical equivalent improved from an average of −7.5 ± 2.5 D to −0.2 ± 0.5 D.
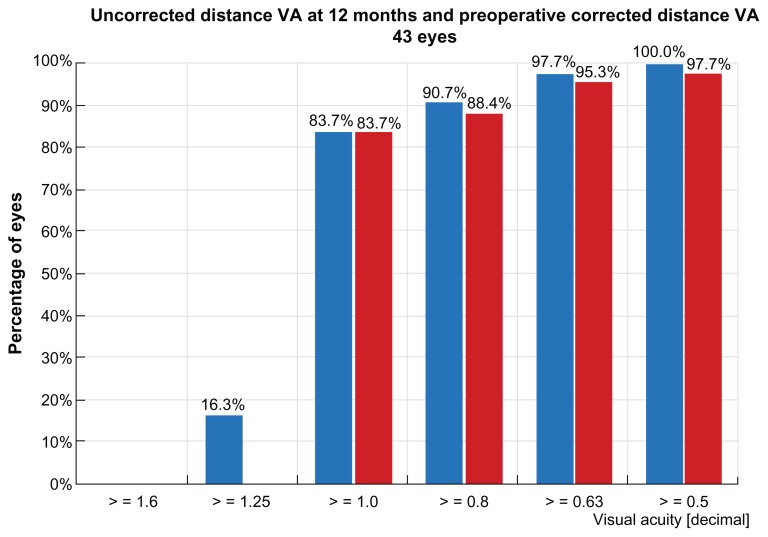
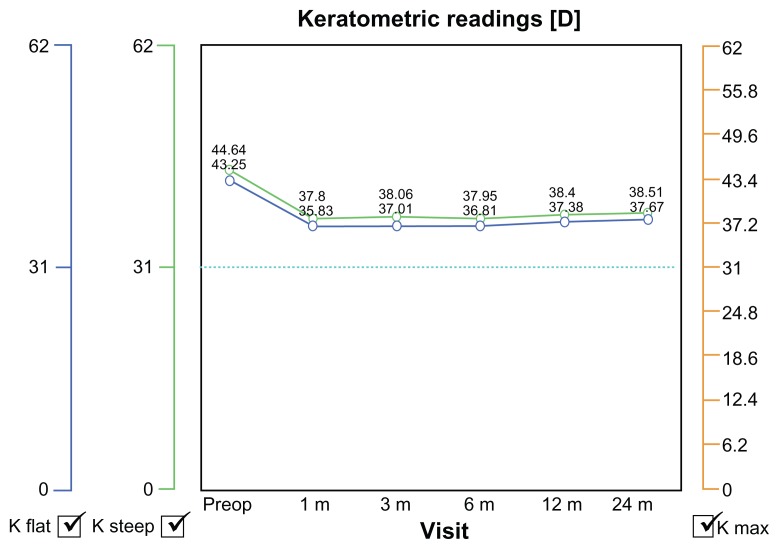
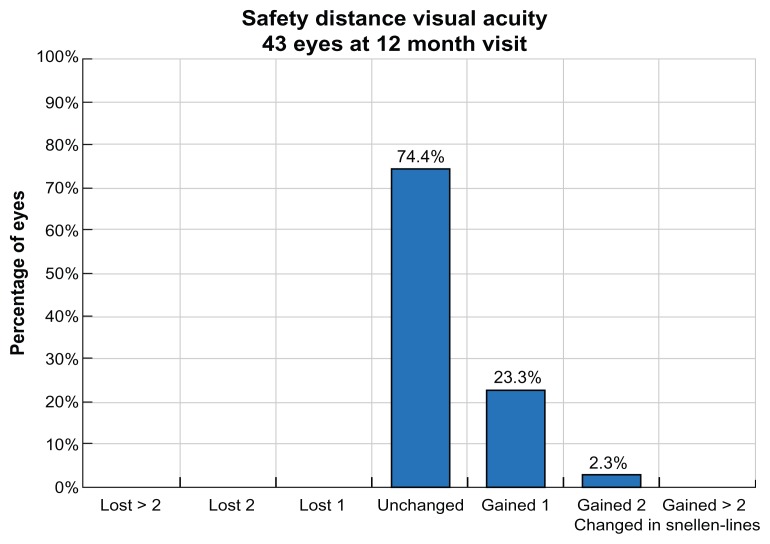
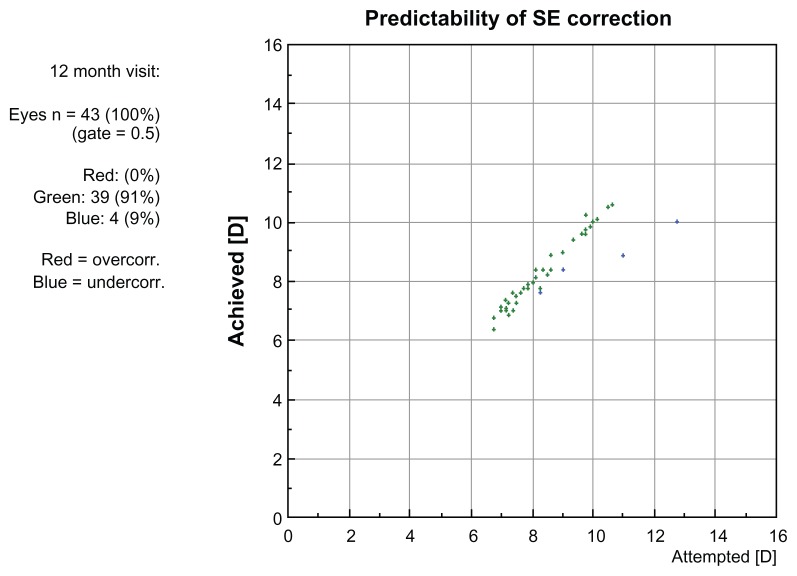
Figure 3 demonstrates postoperative uncorrected distance visual acuity and corrected distance visual acuity at 12 months. Cornea keratometry was 44.5 ± 2.4 D on average preoperatively and reduced to 38 ± 2.1 D postoperatively. Figure 4 shows the keratometric stability of the group during the first 24 months postoperatively. Figure 5 shows the safety data for the group at the 12-month postoperative follow-up. Figure 6 shows the group efficacy data at 12 months.
Figure 3.
Postoperative uncorrected and corrected distance visual acuity at 12 months.
Figure 4.
Image showing keratometric stability over the first 24 months for the group measured by Scheimpflug-based tomography.
Figure 5.
Safety data for the group at 12 months.
Figure 6.
Spherical equivalent correction predictability for the group at 12 months.
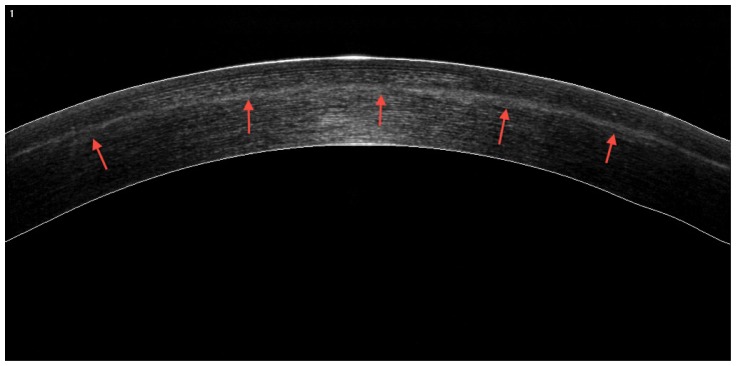
Mean flap thickness was measured intraoperatively to be 105 ± 7 μm. Mean minimal cornea thickness evaluated by Scheimpflug tomography was 525 μm preoperatively and 455 μm measured at 12 months after surgery. Mean endothelial cell counts were 2750 ± 250 preoperatively and 2800 ± 220 postoperatively, with the change possibly attributable to discontinuation of contact lens use after surgery. None of the patients had developed signs of ectasia at a mean 3.5 ± 1.6 years of follow-up. Cornea optical coherence tomography showed signs of hyper-reflectivity surrounding the flap interface in the majority of cases, as seen in Figure 7.
Figure 7.
Anterior segment OCT image of a treated cornea.
Note: There is hyper-reflectivity evident over and under the LASIK flap (red arrows).
Abbreviations: OCT, optical coherence tomography; LASIK, laser-assisted in situ keratomileusis.
Discussion
For over 10 years now, we have treated patients relatively successfully combining cross-linking with laser refractive normalization of the ocular surface, a technique known locally as the Athens protocol.17–23 As noted earlier, it is well known that LASIK reduces the biomechanical stability of the cornea by intersecting with structural lamellae in the anterior cornea and, of course, by removing some of the structural lamellae in lieu of ablation.
Although post-LASIK ectasia continues to be an extremely rare occurrence, we have long advocated the potential benefit of cross-linking at the completion of LASIK to prevent this complication. We introduced this concept mainly as a result of practicing in a population with a particularly high rate of keratoconus24 and after discovering that several patients whom we have treated in the past with LASIK have siblings or close relatives with clinical keratoconus that we did not know of at the time of the original LASIK procedure. The rationale of treatment using a LASIK flap (as opposed to irradiating the riboflavin-soaked stroma) is to reduce stromal exposure time and the risk of flap dehydration.
In the Southern Mediterranean region, specifically in our clinical setting in Athens, it would probably be justified to take measures to prevent corneal ectasia, in addition to screening for irregular topography and topometry and ensuring an adequate residual stromal bed (we use 320 μm as the minimum planned residual stroma bed after LASIK) in patients who are undergoing LASIK for high myopia, are of young age, and/or have a corneal thickness that would prompt us to do so (original corneal thickness less than 530 μm).
There is no published literature to date evaluating the effect of prophylactic collagen cross-linking in routine LASIK cases. As noted previously, prophylactic cross-linking may offer a significant benefit, especially in younger patients with unknown family member corneal status, especially in younger patients in countries with high incidence of keratoconus. The risk of a family member or sibling having irregular topograohically corneas may be higher and thus an increased risk for post-LASIK ectasia may exist, even when all parameters evaluated in the specific patient apopear normal. We generally employ prophylactic CXL routinely in LASIK cases with one or more of the below: a-over 6 diopters of myopia, b-cases with over 1 diopter of astigmatism, c-patients under 30 years old and last d-when co=minimal cornea pachymetry is under 520 μm. It is our understanding that some of the so-called LASIK “regressions” may actually be biomechanical responses to thinning of the cornea and interruption of the collagen lamellae in the surface of the corneal stroma. These changes may create a “controlled” rather than ectasia-like change of the cornea, making it steeper with time. This phenomenon may be a mechanical effect on the cornea from one or a combination of several mechanisms, ie, blinking, eye rubbing, intraocular pressure pushing from in towards out, continuous pulsating mechanical change onto the cornea induced by the heartbeat pulse pressure wave in the body, and eye collagen content in the years following the procedure.
In this small study, we established that prophylactic collagen cross-linking is safe in routine LASIK cases. We had seen no adverse effects or overcorrection in any of our patients, nor any significant unpredicted refractive result. It would be interesting to use one eye as a control in a prospective study in regard to prophylactic cross-linking, but this unfortunately was not done in the present study. Technology such as the Corvis® ST (Oculus, Germany) or the ORA could be used in controlled one-eye studies, to document the efficacy of cross-linking. We have recently switched to using the KXL (Avedro, Waltham, MA) and applying 30 mW/cm2 for just one minute, given that this device delivers the same total fluence of ultraviolet light to the corneal stroma and reduces treatment time, and reduces treatment time. We have since emloyed yet higher fluence of UV light for this purpose. We currently utililize the KXL device (Avedro, Waltham, MA) with settings of 30 mW/cm2 for 90 seconds instead of the 10 mW/cm2 for 5 minutes described herein.
Of course, one would wonder why there is a need for prophylactic collagen cross-linking when corneal ectasia is an extremely rare occurrence. Nonetheless, this concept should be evaluated in larger studies to establish the possibility that this intervention may offer greater stability of the LASIK effect, which has shown surprising changes in a large proportion of patients in several long-term studies. Almost 10% of patients who have had high myopia corrected show changes over a period of 10 years.25,26 Prophylactic cross-linking may reduce the possibility of such changes.
In general, it could be said that one of the major disadvantages of LASIK compared with photorefractive keratectomy is the reductions of the biomechanical stability of the cornea. If one could then establish that biomechanical stability has recurred after use of collagen cross-linking in routine LASIK cases, then that would further enforce LASIK as the primary refractive procedure because it has a favorable safety record, is tolerated by patients very well, and enables a rapid return into daily activities. Although not tested in this small group, it would be interesting to study the potential difficulty of retreatment in patients who have undergone LASIK with prophylactic cross-linking. Larger studies and better follow-up would establish the efficacy and safety of this proposed novel intervention.
Footnotes
Disclosure
Part of this work was presented as a paper at the American Academy of Ophthalmology annual meeting in San Francisco, CA, October 24–27, 2009, and as a poster at the annual meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, FL, May 3–7, 2009. Otherwise, the author reports no conflict of interest in this work.
References
- 1.Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998;14(3):312–317. doi: 10.3928/1081-597X-19980501-15. [DOI] [PubMed] [Google Scholar]
- 2.Geggel HS, Talley AR. Delayed onset keratectasia following laser in situ keratomileusis. J Cataract Refract Surg. 1999;25(4):582–586. doi: 10.1016/s0886-3350(99)80060-1. [DOI] [PubMed] [Google Scholar]
- 3.Uzbek AK, Kamburoğlu G, Mahmoud AM, Roberts CJ. Change in biomechanical parameters after flap creation using the Intralase femtosecond laser and subsequent excimer laser ablation. Curr Eye Res. 2011;36(7):614–619. doi: 10.3109/02713683.2010.546952. [DOI] [PubMed] [Google Scholar]
- 4.Padmanabhan P, Radhakrishnan A, Natarajan R. Pregnancy-triggered iatrogenic (post-laser in situ keratomileusis) corneal ectasia – a case report. Cornea. 2010;29(5):569–572. doi: 10.1097/ICO.0b013e3181bd9f2d. [DOI] [PubMed] [Google Scholar]
- 5.Meghpara B, Nakamura H, Macsai M, et al. Keratectasia after laser in situ keratomileusis: a histopathologic and immunohistochemical study. Arch Ophthalmol. 2008;126(12):1655–1663. doi: 10.1001/archophthalmol.2008.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Binder PS. Analysis of ectasia after laser in situ keratomileusis: risk factors. J Cataract Refract Surg. 2007;33(9):1530–1538. doi: 10.1016/j.jcrs.2007.04.043. [DOI] [PubMed] [Google Scholar]
- 7.Condon PI, O’Keefe M, Binder PS. Long-term results of laser in situ keratomileusis for high myopia: risk for ectasia. J Cataract Refract Surg. 2007;33(4):583–590. doi: 10.1016/j.jcrs.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Randleman JB. Post-laser in-situ keratomileusis ectasia: current understanding and future directions. Curr Opin Ophthalmol. 2006;17(4):406–412. doi: 10.1097/01.icu.0000233963.26628.f0. [DOI] [PubMed] [Google Scholar]
- 9.Evans J, Hau S. The therapeutic and optical application of a rigid gas permeable semi-limbal diameter contact lens. Cont Lens Anterior Eye. 2009;32(4):165–169. doi: 10.1016/j.clae.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Piñero DP, Alio JL. Intracorneal ring segments in ectatic corneal disease – a review. Clin Experiment Ophthalmol. 2010;38(2):154–167. doi: 10.1111/j.1442-9071.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 11.Alió JL, Claramonte PJ, Cáliz A, Ramzy MI. Corneal modeling of keratoconus by conductive keratoplasty. J Cataract Refract Surg. 2005;31(1):190–197. doi: 10.1016/j.jcrs.2004.10.042. [DOI] [PubMed] [Google Scholar]
- 12.Kanellopoulos AJ. Post-LASIK ectasia. Ophthalmology. 2007;114(6):1230. doi: 10.1016/j.ophtha.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 13.Hafezi F, Kanellopoulos J, Wiltfang R, Seiler T. Corneal collagen crosslinking with riboflavin and ultraviolet A to treat induced keratectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33(12):2035–2040. doi: 10.1016/j.jcrs.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 14.Salgado JP, Khoramnia R, Lohmann CP, Winkler von Mohrenfels C. Corneal collagen crosslinking in post-LASIK keratectasia. Br J Ophthalmol. 2011;95(4):493–497. doi: 10.1136/bjo.2010.179424. [DOI] [PubMed] [Google Scholar]
- 15.Kanellopoulos AJ. Collagen cross-linking in early keratoconus with riboflavin in a femtosecond laser-created pocket: initial clinical results. J Refract Surg. 2009;25(11):1034–1037. doi: 10.3928/1081597X-20090901-02. [DOI] [PubMed] [Google Scholar]
- 16.Krueger RR, Ramos-Esteban JC, Kanellopoulos AJ. Staged intrastromal delivery of riboflavin with UVA cross-linking in advanced bullous keratopathy: laboratory investigation and first clinical case. J Refract Surg. 2008;24(7):S730–S736. doi: 10.3928/1081597X-20080901-17. [DOI] [PubMed] [Google Scholar]
- 17.Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocol. J Refract Surg. 2011;27(5):323–331. doi: 10.3928/1081597X-20101105-01. [DOI] [PubMed] [Google Scholar]
- 18.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25(9):S812–S818. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 19.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26(7):891–895. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 20.Kanellopoulos AJ, Skouteris VS. Secondary ectasia due to forceps injury at childbirth: management with combined topography-guided partial PRK and collagen cross-linking (Athens protocol) and subsequent phakic IOL implantation. J Refract Surg. 2011;27(9):635–636. doi: 10.3928/1081597X-20110901-05. [DOI] [PubMed] [Google Scholar]
- 21.Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reports. J Refract Surg. 2010;26(10):S827–S832. doi: 10.3928/1081597X-20100921-11. [DOI] [PubMed] [Google Scholar]
- 22.Kanellopoulos AJ. Long term results of a prospective randomized bilateral eye comparison trial of higher fluence, shorter duration ultraviolet A radiation, and riboflavin collagen cross linking for progressive keratoconus. Clin Ophthalmol. 2012;6:97–101. doi: 10.2147/OPTH.S27170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanellopoulos AJ. The management of cornea blindness from severe corneal scarring, with the Athens protocol (transepithelial topography-guided PRK therapeutic remodeling, combined with same-day, collagen cross-linking) Clin Ophthalmol. 2012;6:87–90. doi: 10.2147/OPTH.S27175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cho M, Kanellopoulos AJ. Safety and efficacy of prophylactic ultraviolet- A-induced crosslinking after high-risk myopic photorefractive leratectomy. Presented at the annual meeting of the Association for Research in Vision and Ophthalmology; Fort Lauderdale, FL. May 3–7, 2009. [Google Scholar]
- 25.Alià JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of photorefractive keratectomy for myopia of more than -6 diopters. Am J Ophthalmol. 2008;145:37–45. doi: 10.1016/j.ajo.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Alià JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of laser in situ keratomileusis for high myopia. Am J Ophthalmol. 2008;145(1):55–64. doi: 10.1016/j.ajo.2007.08.035. [DOI] [PubMed] [Google Scholar]