Abstract
Objective
To compare the results of laser in situ keratomileusis for myopia using WaveLight® Allegretto Wave® Eye-Q® and Technolas® 217z excimer lasers.
Method
A retrospective, comparative case series of 442 eyes matched for age and myopia: half each were treated with Allegretto’s wavefront-optimized algorithm and Technolas PlanoScan. Outcome measures were postoperative mean logarithm of the minimum angle of resolution (logMAR) uncorrected visual acuity (UCVA), manifest refraction spherical equivalent (MRSE), cylinder, safety and efficacy indices, refractive predictability, and optical zone size selection. Refractive predictability of a subgroup treated for −2.50 to −4.0 diopter (D) was analyzed separately.
Results
At mean follow-up of 80.5 days, mean logMAR UCVA, mean MRSE and mean postoperative cylinder were 0.02 ± 0.07 (range −0.12 to 0.30), 0.27 ± 0.36 D (range −1.25 to 1.50 D) and −0.33 ± 0.30 D (range 0.00 to −1.50 D) for Allegretto versus 0.02 ± 0.08 (range −0.12 to 0.40), 0.095 ± 0.47 D (range −1.25 to 1.13 D) and −0.44 ± 0.5 2 D (range 0.00 to −2.25 D) for Technolas (P = 0.98, 0.80 and 0.006). Mean safety and efficacy indices were 1.05 ± 0.13 (0.75–1.33) and 0.97 ± 0.13 (0.50–1.33) for Allegretto and 1.07 ± 0.14 (0.75–1.49) and 0.97 ± 0.17 (0.40–1.49) for Technolas (P = 0.23 and 0.69). Proportions of eyes achieving postoperative MRSE within ±1.0 D, ±0.5 D, and ±0.25 D were 98.2%, 91.9% and 75.6% for Allegretto and 99.1%, 97.8% and 72.4% for Technolas (P = 0.68, 0.20 and 0.51). Mean optical zone size selected was 6.48 ± 0.10 mm (range 6.0–6.5 mm) for Allegretto and 6.38 ± 0.19 mm (range 5.6–6.6 mm) for Technolas (P < 0.001). Of the subgroup with treatment between −2.5 and −4.0 D, 86.8% and 58.5% of eyes treated with Allegretto achieved postoperative MRSE within ±0.50 D and ±0.25 D versus 70.4% and 44.4% for Technolas (P = 0.006 and 0.057).
Conclusion
No differences were seen in postoperative mean logMAR UCVA, MRSE, safety and efficacy indices between the two lasers. Allegretto produced less residual astigmatism, possibly improved refractive predictability, and required smaller optical zone selection.
Keywords: LASIK, myopia, laser vision correction, conventional laser algorithm
Introduction
Laser in situ keratomileusis (LASIK) is among the most widely performed ophthalmic operations worldwide.1,2 Clinical results of LASIK have improved over the past decade, because of advancements in technique and technology.3 The introduction of femtosecond laser flap creation significantly reduced flap-related complications.4,5 Newer generations of excimer laser machines have also contributed to improved results of LASIK in recent years.6
The first-generation excimer lasers were “broad beam lasers” that created less uniform surface profiles than the newer generations. These newer-generation excimer lasers use scanning beams or flying spots, with smaller spot sizes and more efficient eye trackers. Although excimer machines from different manufacturers converge in technology, individual lasers differ in laser ablation algorithm, eye-tracking technology, frequency of laser ablation, corneal thickness ablated, duration of treatment, and physical design.7–9
As new lasers emerge, it is important to assess and compare their results with existing technologies. Therefore, the aim of this study was to compare the clinical outcome of LASIK between the WaveLight® Allegretto Wave® Eye-Q® 400 Hz excimer laser (WaveLight GmbH, Alcon, Fort Worth, TX) and the Technolas® 217z100 (Bausch and Lomb Surgical, Irvine, CA) for correction of myopia and myopic astigmatism. The results of the most commonly performed conventional laser algorithms of these two excimers were compared. These were the PlanoScan algorithm of the Technolas and the wavefront-optimized algorithm of the WaveLight.
Material and methods
Patient population
This was a retrospective, comparative cohort study of all patients at the Singapore National Eye Centre who underwent LASIK between March 3 and March 30, 2010, using either the Technolas or the WaveLight Allegretto Wave excimer. All data were obtained from the computerized database of the Clinical Audit Department of the Singapore National Eye Centre, with Institutional Review Board approval. The inclusion criterion for entry into the study was that cases had complication-free LASIK. Cases were matched for age and degree of preoperative myopia, which was categorized into low (spherical equivalent (SE), ≤5.00 D), moderate (SE, ≥5.00 D and ≤10.00 D), or high myopia (SE, ≥10.00 D).
All patients underwent a comprehensive preoperative ophthalmic consultation and eye examination by the ophthalmologist at least 1 day prior to surgery. Preoperative evaluation included manifest and cycloplegic refraction by qualified optometrists, ultrasound corneal pachymetry ( Topcon Corporation, Tokyo, Japan), Orbscan® II (Bausch and Lomb, Dornach, Germany) corneal topography, and a dilated fundoscopy. Inclusion criteria for LASIK were as follows: (1) absence of soft contact lens wear for 1 week prior to surgery and of rigid contact lens wear for 2 weeks prior to surgery; (2) stable refractive error for at least 12 months before surgery (not fluctuating more than 0.5 D for preoperative myopia of −6.0 D or less and not fluctuating more than 1 D for myopia of greater than −6.0 D); (3) no amblyopia; (4) no previous ocular surgery, nor corneal diseases such as herpetic ulceration; (5) no glaucoma; (6) no cataract; (7) no history of ocular trauma; and (8) normal peripheral retina. Exclusion criteria for LASIK were as follows: (1) keratoconus or forme fruste keratoconus based on corneal topography, (2) active ocular disease, (3) systemic connective tissue diseases or endocrine diseases likely to affect corneal wound healing, (4) pregnancy or nursing, (4) calculated postoperative corneal residual stromal thickness of less than 250 μm, (5) untreated retinal breaks.
Following a thorough explanation of the LASIK procedure, its risks and possible complications, and a detailed discussion of the patient’s lifestyle requirements, informed consent was obtained from each patient.
Surgical technique
Of the 442 eyes that underwent LASIK, half were treated with the Technolas and half with the WaveLight Allegretto Wave excimer laser. A team of twelve surgeons performed the treatment; the Technolas LASIK cases were treated from March to December 2009, while the Wave- Light Allegretto Wave LASIK cases were treated from September 2009 (upon installation of the laser machine) to March 2010.
All cases performed with the WaveLight excimer laser used the WaveLight Allegretto Wave’s company-supplied nomogram. Optical zone selected was usually a standard size of 6.5 mm, but this was sometimes reduced to 6.0 mm for correction of high myopia to ensure adequate residual cornea stromal thickness. The WaveLight laser underwent a fluence test daily prior to the first case of the day.
For cases performed with the Technolas laser, surgeons used their own nomograms, which usually take into consideration surgical time and technique. This typically involved a 10%–15% reduction in treatment for higher myopia. Age and accommodation were similarly taken into account for target refraction. Optical zone size was adjustable in steps of 0.1 mm. Each case of Technolas excimer laser was preceded by a fluence test.
All flaps were created with femtosecond lasers. The femtosecond laser used was either the VisuMax® 500 kHz (Carl Zeiss Meditec, Jena, Germany) or the IntraLase® (Abbott Medical Optics Inc, Santa Ana, CA).
Postoperative regimes were the same for all patients and included a combination of 0.5% moxifloxacin ophthalmic solution (Vigamox®; Alcon) and 0.1% dexamethasone (Maxidex®; Alcon) eyedrops in a tapering dose for a week and frequent preservative-free artificial tear supplements for a month.
Postoperative evaluation
Patients returned for follow-up 1 day, 1 week, 1 month, and 3 months after the LASIK procedure. Postoperative examinations included uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BCVA) using a standard Snellen acuity chart at 6 m, manifest refraction, and slit lamp biomicroscopy. Visual acuity results were converted and analyzed in the logarithm of the minimum angle of resolution (logMAR) equivalent. Manifest refraction was performed at 1 and 3 months, and measurements were computed as manifest refraction, cylinder and MRSE. If the patient defaulted at the 3-month visit, then the last follow-up results were recorded. Refraction was performed at the spectacle plane and results were converted to the corneal plane for analysis of refractive predictability.
Safety index was defined as postoperative BCVA/preoperative BCVA; efficacy index was defined as postoperative UCVA/preoperative BCVA. Mean refractive predictability was defined as the difference between the achieved and the target MRSE (ie, achieved minus target MRSE). Target MRSE was defined as difference between preoperative MRSE and treatment MRSE (preoperative MRSE minus treatment MRSE).
Outcome measures analyzed include postoperative mean log MAR UCVA, and BCVA MRSE, cylinder, safety and efficacy indices, refractive predictability, and optical zone size selection. The refractive predictability of a separate subgroup treated for −2.50 to −4.0 D was also analyzed.
Statistical analysis
Outcome measures were compared between the Technolas and Allegretto Wave eyes. Data were analyzed using SPSS software (v 15; SPSS, Inc, Chicago, IL). The sample size of the study was calculated to ensure 80% power and a P-value of 0.05 for all the main outcome measures. Using a previous published study on the outcome of the Technolas laser,3 the authors were able to calculate that to show equivalence of safety of 0.035, 217 eyes were needed in each group in the present study, while for analysis of efficacy, 220 eyes were needed in each group to allow an equivalence of 0.04. To detect a 12% difference in predictability 200 eyes in each group were needed. The Mann-Whitney U test for statistical significance was used to calculate for difference in optical zone sizes, the nonparametric Kruskal-Wallis test was used to calculate intersurgeon difference and subgroup refractive predictability, and regression analysis was used for correlation studies.
Results
Patient data
The mean age of the patients was 32.6 ± 7.2 years (range 20.9–52.7 years). Mean age of the WaveLight patients was 32.5 ± 7.0 years (range 21.4–50.9 years) and that of the Technolas patients was 32.7 ± 7.3 years (range 20.9–52.7 years), with no statistically significant difference between the two groups. Of all patients, 174 (39.4%) were male and 268 (60.6%) were female. The majority of patients were of Oriental racial origin, with 74.2% identifying as Chinese, 5.7% identifying as Indian, and 2.7% identifying as Malay; 17.4% of the cases were of other races.
The mean preoperative cycloplegic SE corrected was −4.3 ± 2.0 D for all cases; the median SE corrected was −4.0 D. The mean preoperative SE for the Allegretto Wave group was −4.47 ± 1.89 D (range −0.75 to −11.25 D) and for the Technolas group it was −4.16 ± 2.0 D (range −1.0 to −10.63 D). The mean manifest cylinder corrected was −0.78 ± 0.62 D (range 0 to −3.5 D) for the Allegretto Wave group, while for the Technolas group it was −0.74 ± 0.66 D (range 0 to −4.5 D). Mean follow-up duration was 80.5 ± 33.5 days (range 19–146 days); median follow-up was 90 days. There were no statistically significant differences in preoperative cycloplegic SE, cylinder, and mean follow-up duration between the two groups.
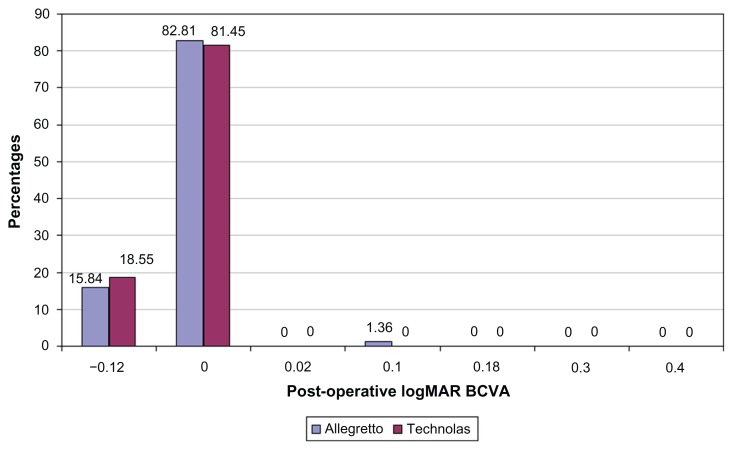
Visual and refractive results
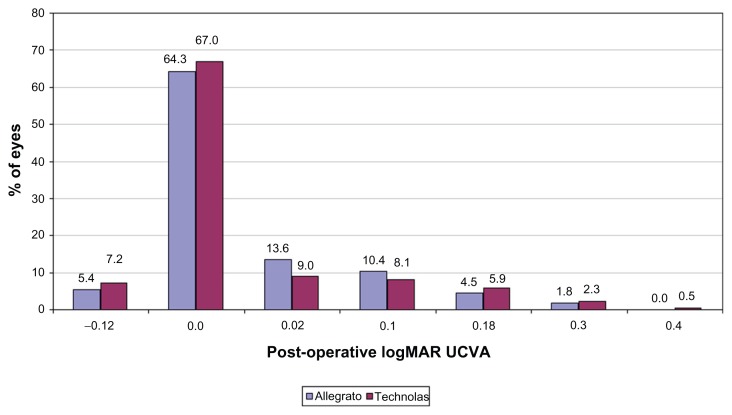
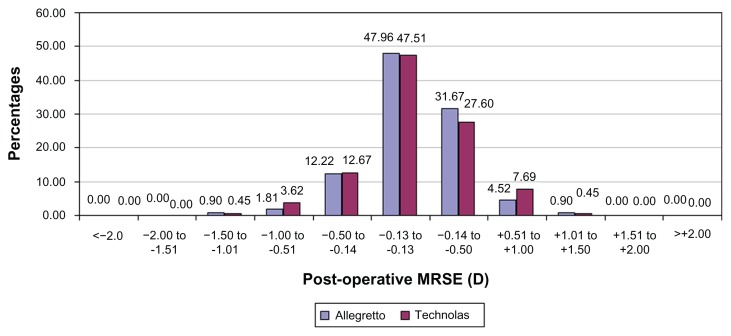
The postoperative mean logMAR UCVA for the Allegretto Wave LASIK eyes was 0.02 ± 0.07 (range −0.12 to 0.30), while for the Technolas LASIK eyes it was 0.02 ± 0.08 (range −0.12 to 0.40) (P = 0.98). The postoperative mean logMAR BCVA for the Allegretto Wave was −0.02 ± 0.04 (range −0.12 to 0.1), and for Technolas it was −0.02 ± 0.05 (range −0.12 to 0.00; P = 0.40). The mean postoperative MRSE for Allegretto Wave LASIK was 0.27 ± 0.36 D (range −1.25 to 1.50 D), while for Technolas it was 0.095 ± 0.47 D (range −1.25 to 1.13 D) (P = 0.80). There was no statistically significant intersurgeon difference in mean postoperative MRSE outcome overall or in the individual excimer groups. Comparisons of percentages of eyes versus postoperative logMAR UCVA, logMAR BCVA, and MRSE between the two lasers are shown in Figures 1–3.
Figure 1.
Comparison of postoperative logarithm of the minimum angle of resolution (logMAR) uncorrected visual acuity (UCVA) between Allegretto Wave® wavefront-optimized and Technolas® PlanoScan treatment.
Figure 3.
Comparison of postoperative manifest refraction spherical equivalents between Allegretto Wave® wavefront-optimized and Technolas® PlanoScan treatment.
Abbreviation: D, diopter.
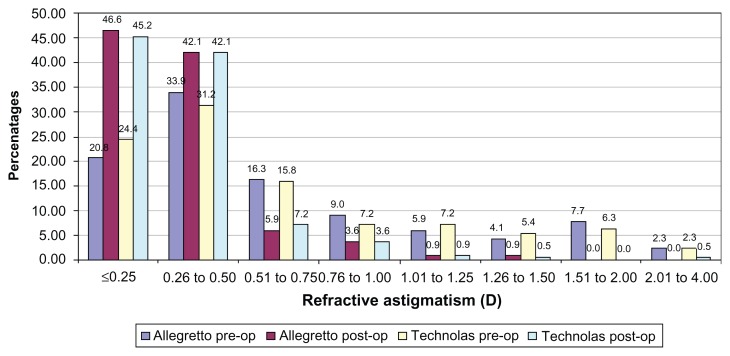
Mean post-operative cylinder was −0.44 ± 0.52 D (range 0.00 to −2.25 D) in the Technolas group and −0.33 ± 0.30 D (range 0.00 to −1.50 D) in the Allegretto group (P = 0.006). The percentages of eyes versus pre-operative and postoperative cylinder are shown in Figure 4.
Figure 4.
Comparison of pre- and postoperative refractive astigmatism in diopter (D) between Allegretto Wave® wavefront-optimized and Technolas® PlanoScan treatment.
Abbreviation: D, diopter.
Optical zone size
The mean optical zone size selected on the Allegretto Wave was 6.48 ± 0.10 mm (range 6.0–6.5 mm) while that on the Technolas was 6.38 ± 0.19 mm (range 5.6–6.6 mm). This difference was statistically significant (P < 0.001). Optical zone size was not correlated with the postoperative MRSE outcome for the Allegretto Wave (P = 0.55), but was positively correlated with the postoperative MRSE outcome in the Technolas group (P = 0.02).
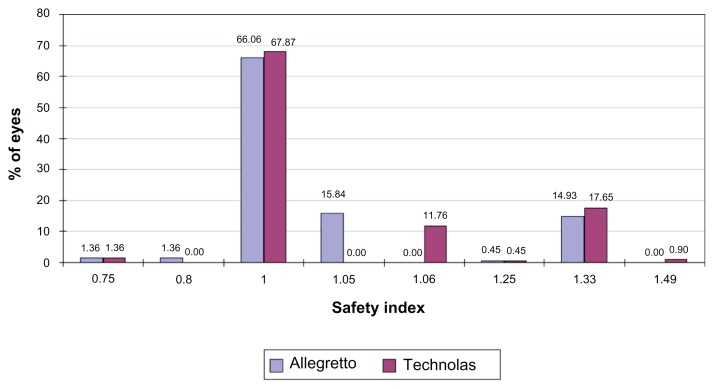
Safety
The mean safety indices of Allegretto Wave and Technolas LASIK were 1.05 ± 0.13 (range 0.75–1.33) and 1.07 ± 0.14 (range 0.75–1.49) respectively (P = 0.23) (Figure 5).
Figure 5.
Comparison of safety indices between Allegretto Wave® wavefront-optimized and Technolas® PlanoScan treatment.
Efficacy
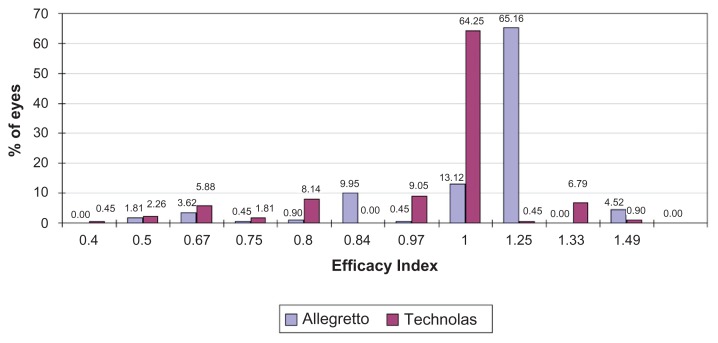
The mean efficacy index of Allegretto Wave LASIK was 0.97 ± 0.13 (range 0.50–1.33), while that of Technolas LASIK was 0.97 ± 0.17 (range 0.40–1.49) (P = 0.69) (Figure 6).
Figure 6.
Comparison of efficacy indices between Allegretto Wave® wavefront-optimized and Technolas® PlanoScan treatment.
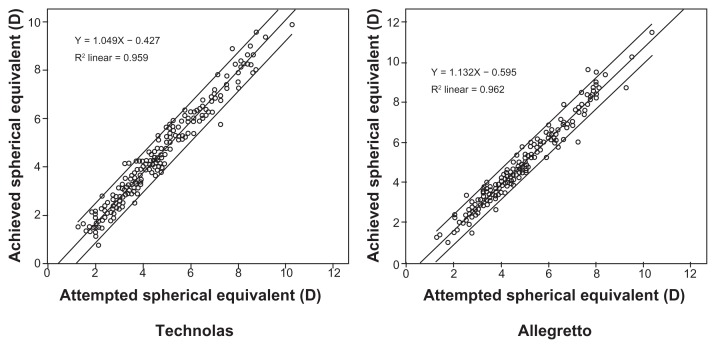
Predictability
The proportion of eyes treated with the Allegretto Wave that achieved postoperative MRSE of ±1.0 D, ±0.5 D, and ±0.25 D were 98.2%, 91.9%, and 75.6%, respectively, while for Technolas it was 99.1%, 97.8%, and 72.4%, respectively. The differences between the percentages of the Allegretto Wave–treated eyes and the Technolas-treated eyes were not statistically significant (P-values were 0.68, 0.20, and 0.51, respectively).
The predictability curve gave coefficient of determination values of 0.962 for Allegretto Wave–treated eyes and 0.959 for Technolas-treated eyes, with no statistically significant difference between the two (Figure 6).
The mean refractive predictability for Allegretto Wave– treated eyes was −0.17 ± 0.38 D (range −1.62 to 1.34 D), while for Technolas-treated eyes it was −0.21 ± 0.46 D (range −2.25 to 2.13 D; P = 0.22). There was no statistically significant intersurgeon difference in mean refractive predictability in either the Allegretto Wave (P = 0.18) or the Technolas groups (P = 0.18).
Of the subgroup of patients treated with excimer ablation of SE between −2.50 and −4.00 D for whom no nomogram adjustment was required for the Allegretto Wave (n = 106 for the Allegretto Wave; n = 81 for the Technolas), the percentages of eyes with postoperative MRSE of within ±1.0, within ±0.50, and within ±0.25 D were 98.1%, 86.8%, and 58.5%, respectively, for the Allegretto Wave and 97.5%, 70.4%, and 44.4%, respectively, for the Technolas (P = 1.0, 0.006, and 0.057, respectively). However, there was no statistically significant intersurgeon difference in mean refractive predictability in either Allegretto Wave (P = 0.21) or Technolas (P = 0.40) subgroups.
Discussion
The Bausch and Lomb Technolas 217z excimer system is part of an overall platform that integrates multiple diagnostic devices and the excimer machine. Although the 217z is one of the most recent laser machines from Bausch and Lomb, its PlanoScan conventional excimer laser was available in the Technolas 217A version, which has been approved for clinical use by the US Food and Drug Administration (FDA) since 2000.10–12 The Technolas 217z offers several other advanced card-based treatment modules, such as the Zyoptix® tissue-saving treatment mode, the Zyoptix aspheric treatment mode, and the Zyoptix personalized (wavefront-guided) treatment mode, all available in combination with an optional dynamic rotational eye tracker. Its nonaspheric PlanoScan mode, the subject of this study, uses a 2.0 mm flying spot beam with a truncated Gaussian profile, with treatment delivered at 50 Hz. Surgeons usually devise their own nomograms after a period of use to provide for variations in surgical time and technique. The nomogram adjustment typically involves reducing treatment power by up to 10%–15% for higher degrees of myopic correction.13
The WaveLight Allegretto Wave laser was introduced first in Europe just over 10 years ago and was then approved by the FDA in 2003. Its Eye-Q version was approved by the FDA in 2006; the wavefront-optimized treatment uses flying spot technology with a 0.68 mm Gaussian beam and 0.95 mm spot diameter, with a higher frequency rate of 400 Hz than the previous version at 200 Hz.14,15 It has a short treatment time of 2 seconds per diopter. It produces an aspheric treatment profile when operating in its wavefronto-ptimized mode. The wavefront-optimized mode provides more treatment to the periphery than centrally, to reduce spherical aberration, but it is not wavefront-guided. The company supplies a nomogram chart, which recommends a standardized reduction in treatment for high degrees of myopia and cylinder. For low myopia, an increase in treatment is recommended instead.
This is the first study comparing the Technolas® 217z and the WaveLight® Allegretto Wave® Eye-Q® 400 Hz excimer laser. Previous studies have demonstrated that the Wave- Light wavefront-optimized laser platform achieved a better outcome in postoperative unaided LogMAR visual acuity in myopic spherocylinder eyes than the VISX® Star S4 and LADARVision® 4000 lasers,7 while in hyperopic eyes the WaveLight wavefront-optimized laser resulted in more rapid visual recovery and less residual cylinder than LADARVision 4000’s conventional ablation.8 Other studies have not cited any statistically significant differences in the outcome of LASIK performed for spherocylindrical errors9,16 between the WaveLight Allegretto Wave and SCHWIND ESIRIS®, VISX, or NIDEK® excimer lasers.
This study showed that the WaveLight Allegretto Wave wavefront-optimized excimer treatment performed equally with the Technolas planoscan platform in terms of postoperative UCVA, MRSE, and safety and efficacy indices. In addition, the WaveLight Allegretto Wave produced slightly lower postoperative astigmatism than the Technolas excimer laser (Figure 7). This study also suggests that the Allegretto Wave produces slightly greater refractive predictability, and Allegretto Wave surgeons were able to select larger optical zones.
Figure 7.
Refractive predictability curves for Allegretto Wave® and Technolas® excimer lasers.
Abbreviation: D, diopter.
In Anderson et al’s13 study, larger optical zone sizes were correlated with a more hyperopic outcome using the Technolas laser. Camellin and Arba Mosquera’s study17 showed that a nomogram adjustment should be used for smaller optical zones using the SCHWIND AMARIS®. In the present study, even though the effective optical zone size was not calculated, the planned optical zone size was positively correlated with postoperative MRSE for Technolas, while it was not so with the Allegretto Wave. This suggests possibly greater unpredictability and the possible need for a nomogram for optical zone sizes for the Technolas.
In the present study, the planned optical zone size of Technolas laser ablation was significantly smaller and with a wider range than that of the Allegretto Wave laser. It has to be noted that although gradation of optical zone size by 0.1 mm is possible with the Allegretto Wave’s Q-adjusted algorithm, the Allegretto Wave wavefront-optimized program can only be used to adjust this by steps of 0.5 mm. Hence, the more uniform optical zone size of the Allegretto Wave LASIK eyes, where only selections of 6.0 and 6.5 mm diameter are used, may be a contributory factor to the possibly improved refractive predictability of the Allegretto Wave. The lack of variability in fluence testing with the Allegretto Wave laser may also have improved the consistency of laser calibration and energy output, thereby resulting in greater refractive predictability.
The much shorter treatment time of the WaveLight Allegretto Wave system could have similarly contributed to the slightly greater refractive predictability and reduced residual astigmatism shown in this study, as longer ablation time results in stromal bed drying, which may affect the treatment result. It typically takes 6 seconds for each diopter of treatment for myopia at an optical zone of 6.0 mm for the Technolas PlanoScan, while the Allegretto Wave takes 2 seconds for each diopter of treatment for myopia at an optical zone of 6.5 mm. The effect of the shorter treatment time is multiplied and made more significant at higher dioptric power of treatment. For instance, at SE of −2 D of treatment, treatment time of the Allegretto Wave 400 Hz is 4 seconds, while that of the Technolas PlanoScan is 12 seconds, producing a difference of 8 seconds between them. At SE of −8 D, treatment time becomes 16 seconds for the former and 48 seconds for the latter, a difference of 32 seconds. This is a considerable difference and may influence a patient’s fixation of gaze during treatment, which in turn influences refractive and visual outcomes.
Published reports have quoted an advantage in astigmatism control by the Allegretto Wave system.18 The Technolas PlanoScan algorithm has a 240 Hz video-based infrared eye tracker with active x-and y-axis and passive z-axis tracking, and static compensation of cyclotorsion occurring when the patient moves from the upright to the supine position. The Advanced Control Eyetracking technology with iris registration and static plus dynamic cyclotorsion compensation is available for the Technolas Zyoptix treatment. The Allegretto Wave operates with a 400 Hz closed-loop eye tracker with automatic pupil centering and has an integrated cross-line projector for alignment of the head and eye position, with a “NeuroTracker” for cyclotorsion control for the wavefront-optimized algorithm. Its eye-tracker system and laser trigger are synchronized. The present study showed a statistically significant difference in the postoperative astigmatism of eyes between those treated with the Allegretto Wave and those treated with the Technolas PlanoScan, with the mean residual astigmatism by the Allegretto Wave being −0.33 ± 0.3 D and that by the Technolas being −0.44 ± 0.52 D (P = 0.006). This may be partly due to the difference in eyetracker and cyclotorsion control between the two lasers.
In this study, within the subgroups treated for −2.5 to −4.0 D, the percentages of eyes achieving ±0.50 and within ±0.25 D from plano (meaning “flat” – ie, no vision correction needed) for Allegretto Wave were 86.8% and 58.5%, respectively, versus 70.4% and 44.4%, respectively, for Technolas (P = 0.006 and 0.057, respectively), indicating a possibly better refractive predictability with the Allegretto Wave. In the authors’ opinion, improved refractive predictability of an excimer machine is an advantage, since significant over- or undercorrection will surely affect the visual acuity and efficacy results. Concerns regarding desired improvement in refractive predictability of excimer lasers are not new.19,20 Causes influencing refractive predictability are multifactorial. Refractive predictability may be affected by factors such as duration of open-flap surgery and the state of corneal stromal hydration, which in turn are closely related to surgical technique and excimer laser ablation rate.21 Other factors such as optical zone sizes and preoperative SE refraction are also relevant, as these also affect the treatment duration. Anderson et al13 previously reported on nomogram adjustments of the Technolas excimer laser. No statistically significant difference in postoperative MRSE was found between five different surgeons using the same surgical technique and a common nomogram; however, preoperative SE refraction and optical zone size were correlated with LASIK predictability outcome.
Another advantage of the Allegretto Wave wavefront-optimized excimer laser is its corneal stromal tissue requirement. For instance, from calculation according to company-supplied information, for the same optical zone size of 6.5 mm diameter, the Allegretto Wave ablates approximately 4 μm less corneal tissue per diopter of myopia correction than the Technolas PlanoScan. This can result in greater residual stromal thickness, particularly in treatment of cases with high myopia. It also indirectly facilitates the use of larger optical zone sizes with the Allegretto Wave, which could contribute to better quality of vision and reduce the incidence of postoperative glare and haloes.22,23
It is pertinent to emphasize that the present study is a multisurgeon study comparing the Technolas, an established laser within the Singapore National Eye Centre, with a newly installed WaveLight Allegretto Wave laser. The intention of this study was to compare the entry-level LASIK algorithms of the Technolas and the WaveLight Allegretto Wave – ie, a “classic” versus a wavefront-optimized or aspheric treatment. Previous studies of aberration-neutral or aspheric treatment showed excellent visual acuity, astigmatism, and refractive results in several machines including the SCHWIND ESIRIS and the more recent SCHWIND AMARIS24–26 (SCHWIND eye-tech-solutions GmbH and Co KG, Kleinostheim, Germany) and improved corneal wavefront aberration in comparison with standard treatment.27 Also, several previous studies have shown an advantage of the aspheric LASIK platform over conventional LASIK in residual and induced asphericity and contrast sensitivity, but no statistically significant difference in basic parameters such as UCVA, efficacy, and safety.28,29 Similarly, the present study did not reveal any significant difference in UCVA, efficacy, and safety between the two platforms. A comparison of higher-order aberrations between the two systems would have been useful, but the retrospective nature of the study meant that this was not possible.
The retrospective, nonrandomized nature of this study was a limitation. A prospective trial with one eye of each patient assigned to each group would be more powerful for any further analysis of outcome measures such as refractive predictability, which seemed to be surgeon dependent with the Technolas in the present study. Also, although two different femtosecond lasers were used for flap creation in this study, a previously conducted investigation by the Singapore National Eye Centre, presented at the 2010 American Society of Cataract and Refractive Surgery Symposium and Congress, showed no difference in the LASIK outcomes between the two lasers.
Conclusion
In this study, the WaveLight Allegretto Wave 400 Hz excimer laser’s wavefront-optimized treatment was comparable with the Technolas PlanoScan treatment in postoperative UCVA, MRSE, efficacy, and safety in a multisurgeon setting. As a basic entry-level treatment algorithm, the wavefront- optimized treatment of the Allegretto Wave produced slightly less residual astigmatism, it produced greater refractive predictability, and it operated on a smaller optical zone size than the Technolas PlanoScan treatment. Hence, the Allegretto Wave is a good alternative to the Technolas in myopia and myopic astigmatism LASIK excimer laser treatment.
Figure 2.
Comparison of postoperative logarithm of the minimum angle of resolution (logMAR) best spectacle-corrected visual acuity (BCVA) between Allegretto Wave® wavefront-optimized and Technolas® PlanoScan treatment.
Acknowledgments
The authors received a National Research Foundation–funded Translational and Clinical Research Programme Grant (NMRC/TCR/002-SERI/2008-TCR 621/41/2008).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sekundo W, Bönicke K, Mattausch P, Wiegand W. Six-year follow-up of laser in situ keratomileusis for moderate and extreme myopia using a first-generation excimer laser and microkeratome. J Cataract Refract Surg. 2003;29(6):1152–1158. doi: 10.1016/s0886-3350(03)00062-2. [DOI] [PubMed] [Google Scholar]
- 2.O’Doherty M, O’Keeffe M, Kelleher C. Five year follow up of laser in situ keratomileusis for all levels of myopia. Br J Ophthalmol. 2006;90(1):20–23. doi: 10.1136/bjo.2005.075127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yuen LH, Chan WK, Koh J, Mehta JS, Tan DT for SingLASIK Research Group. A 10-year prospective audit of LASIK outcomes for myopia in 37,932 eyes at a single institution in Asia. Ophthalmology. 2010;117(6):1236–1244. doi: 10.1016/j.ophtha.2009.10.042. [DOI] [PubMed] [Google Scholar]
- 4.Salomão MQ, Wilson SE. Femtosecond laser in laser in situ keratomileusis. J Cataract Refract Surg. 2010;36(6):1024–1032. doi: 10.1016/j.jcrs.2010.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan A, Ou J, Manche EE. Comparison of the femtosecond laser and mechanical keratome for laser in situ keratomileusis. Arch Ophthalmol. 2008;126(11):1484–1490. doi: 10.1001/archopht.126.11.1484. [DOI] [PubMed] [Google Scholar]
- 6.Stonecipher KG, Kezirian GM, Stonecipher K. LASIK for mixed astigmatism using the Allegretto Wave: 3- and 6-month results with the 200- and 400-Hz platforms. J Refract Surg. 2010;26(10):S819–S823. doi: 10.3928/1081597X-20100921-09. [DOI] [PubMed] [Google Scholar]
- 7.Binder PS, Rosenshein J. Retrospective comparison of 3 laser platforms to correct myopic sphere and spherocylinders using conventional and wavefront-guided treatments. J Cataract Refract Surg. 2007;33(7):1158–1176. doi: 10.1016/j.jcrs.2007.03.040. [DOI] [PubMed] [Google Scholar]
- 8.Durrie DS, Smith RT, Waring GO, 4th, Stahl JE, Schwendeman FJ. Comparing conventional and wavefront-optimized LASIK for the treatment of hyperopia. J Refract Surg. 2010;26(5):356–363. doi: 10.3928/1081597X-20090617-07. [DOI] [PubMed] [Google Scholar]
- 9.Dougherty PJ, Bains HS. A retrospective comparison of LASIK outcomes for myopia and myopic astigmatism with conventional NIDEK versus wavefront-guided VISX and Alcon platforms. J Refract Surg. 2008;24(9):891–896. doi: 10.3928/1081597X-20081101-07. [DOI] [PubMed] [Google Scholar]
- 10.US Food and Drug Administration. Premarket approval (PMA) Silver Spring, MA: US FDA; [Accessed April 2, 2012]. updated April 5, 2012. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMA/pma.cfm?id=19521. [Google Scholar]
- 11.Balazsi G, Mullie M, Lasswell L, Lee PA, Duh YJ. Laser in situ keratomileusis with a scanning excimer laser for the correction of low to moderate myopia with and without astigmatism. J Cataract Refract Surg. 2001;27(12):1942–1951. doi: 10.1016/s0886-3350(01)01017-3. [DOI] [PubMed] [Google Scholar]
- 12.Bailey MD, Zadnik K. Outcomes of LASIK for myopia with FDA-approved lasers. Cornea. 2007;26(3):246–254. doi: 10.1097/ICO.0b013e318033dbf0. [DOI] [PubMed] [Google Scholar]
- 13.Anderson NJ, Hardten DR, Davis EA, Schneider TL, Samuelson TW, Lindstrom RL. Nomogram considerations with the Technolas 217A for treatment of myopia. J Refract Surg. 2003;19(6):654–660. doi: 10.3928/1081-597X-20031101-07. [DOI] [PubMed] [Google Scholar]
- 14.US Food and Drug Administration. Premarket approval (PMA) Silver Spring, MA: US FDA; [Accessed April 2, 2012]. updated April 5, 2012. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMA/pma.cfm?id=9698. [Google Scholar]
- 15.Mrochen M, Donitzky C, Wüllner C, Löffler J. Wavefront-optimized ablation profiles: theoretical background. J Cataract Refract Surg. 2004;30(4):775–785. doi: 10.1016/j.jcrs.2004.01.026. [DOI] [PubMed] [Google Scholar]
- 16.Mearza AA, Muhtaseb M, Aslanides IM. Visual and refractive outcomes of LASIK with the SCHWIND ESIRIS and WaveLight Allegretto Wave Eye-Q excimer lasers: a prospective, contralateral study. J Refract Surg. 2008;24(9):885–890. doi: 10.3928/1081597X-20081101-06. [DOI] [PubMed] [Google Scholar]
- 17.Camellin M, Arba Mosquera S. Aspheric optical zones: the effective optical zone with the SCHWIND AMARIS. J Refract Surg. 2011;27(2):135–146. doi: 10.3928/1081597X-20100428-03. [DOI] [PubMed] [Google Scholar]
- 18.Lee YC. Active eye-tracking improves LASIK results. J Refract Surg. 2007;23(6):581–585. doi: 10.3928/1081-597X-20070601-08. [DOI] [PubMed] [Google Scholar]
- 19.Ditzen K, Handzel A, Pieger S. Laser in situ keratomileusis nomogram development. J Refract Surg. 1999;15(2 Suppl):S197–S201. doi: 10.3928/1081-597X-19990302-09. [DOI] [PubMed] [Google Scholar]
- 20.Kohnen T, Steinkamp G, Schnitzler E, et al. LASIK with a superior hinge and scanning spot excimer laser ablation for correction of myopia and myopic astigmatism: results of a prospective study on 100 eyes with a 1-year follow-up. Ophthalmologe. 2001;98(11):1044–1054. doi: 10.1007/s003470170023. [German] [DOI] [PubMed] [Google Scholar]
- 21.Dougherty PJ, Wellish KL, Maloney RK. Excimer laser ablation rate and corneal hydration. Am J Ophthalmol. 1994;118(2):169–176. doi: 10.1016/s0002-9394(14)72896-x. [DOI] [PubMed] [Google Scholar]
- 22.El Danasoury M. Prospective bilateral study of night glare after laser in situ keratomileusis with single zone and transition zone ablation. J Refract Surg. 1998;14(5):512–516. doi: 10.3928/1081-597X-19980901-08. [DOI] [PubMed] [Google Scholar]
- 23.Haw WW, Manche EE. Large optical ablation zone using the VISX S2 Smoothscan excimer laser. J Cataract Refract Surg. 2000;26(12):1742–1747. doi: 10.1016/s0886-3350(00)00707-0. [DOI] [PubMed] [Google Scholar]
- 24.Arbelaez MC, Vidal C, Jabri BA, Arba Mosquera S. LASIK for myopia with aspheric “aberration neutral” ablations using the ESIRIS laser system. J Refract Surg. 2009;25(11):991–999. doi: 10.3928/1081597X-20091016-04. [DOI] [PubMed] [Google Scholar]
- 25.Arbelaez MC, Vidal C, Arba Mosquera S. Excimer laser correction of moderate to high astigmatism with a non-wavefront-guided aberration-free ablation profile: six-month results. J Cataract Refract Surg. 2009;35(10):1789–1798. doi: 10.1016/j.jcrs.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 26.Arba Mosquera S, de Ortueta D. Analysis of optimized profiles for ‘aberration-free’ refractive surgery. Ophthalmic Physiol Opt. 2009;29(5):535–548. doi: 10.1111/j.1475-1313.2009.00670.x. [DOI] [PubMed] [Google Scholar]
- 27.De Ortueta D, Arba Mosquera S, Baatz H. Comparison of standard and aberration-neutral profiles for myopic LASIK with the SCHWIND ESIRIS platform. J Refract Surg. 2009;25(4):339–349. doi: 10.3928/1081597X-20090401-03. [DOI] [PubMed] [Google Scholar]
- 28.Ang RE, Chan WK, Wee TL, Lee HM, Bunnapradist P, Cox I. Efficacy of an aspheric treatment algorithm in decreasing induced spherical aberration after laser in situ keratomileusis. J Cataract Refract Surg. 2009;35(8):1348–1357. doi: 10.1016/j.jcrs.2009.03.039. [DOI] [PubMed] [Google Scholar]
- 29.Igarashi A, Kamiya K, Komatsu M, Shimizu K. Aspheric laser in situ keratomileusis for the correction of myopia using the Technolas 217z100: comparison of outcomes versus results from the conventional technique. Jpn J Ophthalmol. 2009;53(5):458–463. doi: 10.1007/s10384-009-0712-5. [DOI] [PubMed] [Google Scholar]