Abstract
Objective
To investigate whether the 2006 American Society for Colposcopy and Cervical Pathology guidelines for conservative management of minimally abnormal Pap tests (atypical squamous cells of undetermined significance human papillomavirus positive and low-grade squamous intraepithelial lesions) and moderate dysplasia (cervical intraepithelial neoplasia 2) in adolescents: 1) resulted in fewer colposcopies and loop electrosurgical excision procedures (LEEP) in adolescents; or 2) resulted in unintended management changes in older age groups.
Methods
We analyzed data from 1,806 women aged 18 and older attending one of six community health centers who were diagnosed with abnormal Pap tests between 1/1/2004–12/31/2008. We used multivariable logistic regression to examine management differences in women with minimally abnormal Pap tests prior to and after guideline changes. Variables included date of abnormality, site of care, race or ethnicity, language, and insurance type. We used Fisher exact tests to examine rates of LEEP in patients with moderate dysplasia prior to and after guideline publication.
Results
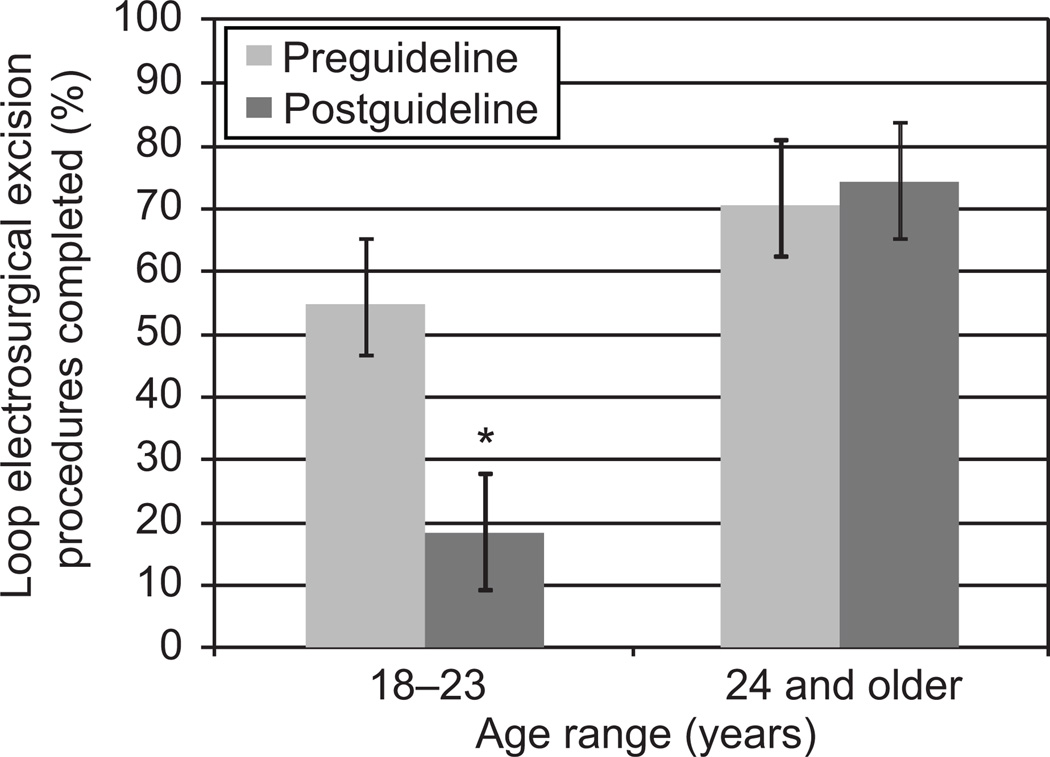
Among 206 women aged 18–20, rates of colposcopy after a minimally abnormal Pap test decreased from 78% (n=102) to 45% (n=34) after guideline changes (p<0.001). Colposcopy among women over age 21 (n=1542) remained unchanged (greater than 90%). Multivariable logistic regression indicated that both date of abnormality and site of care were associated with colposcopy referral. After guideline changes, management of moderate dysplasia with LEEP in women aged 18–23 decreased from 55% to 18% (p=0.04); rates remained stable in women ages 24 and over (70% vs. 74%) (p=0.72).
Conclusion
Health care providers quickly adopted new conservative management guidelines for low-income, minority adolescents which may reduce preterm deliveries in these high-risk populations.
Introduction
Although persistent human papillomavirus (HPV) infection causes nearly all cases of cervical dysplasia and cervical cancer (1), many mild and moderate dysplasias resolve without treatment in adolescent women (2–4). Prior to 2007, excision of moderate dysplasia was recommended for all women (5). However, excisional procedures such as Loop Electrosurgical Excision Procedures (LEEP), have been linked to adverse obstetrical outcomes including preterm delivery and preterm premature rupture of membranes (6, 7). These risks may be compounded in low-income and minority women, who have higher rates of both HPV infection and preterm delivery than the general population (8–10). In light of the evidence showing high rates of regression of cervical dysplasia in adolescents and increased risks of adverse obstetric outcomes after loop electrosurgical excision procedures (LEEP), the American Society for Colposcopy and Cervical Pathology published new clinical practice guidelines in 2006 recommending repeat Pap testing instead of colposcopy for females under 21 years old with minimally abnormal Pap tests, and repeat colposcopy instead of excisional procedures (LEEP) for management of moderate dysplasia (11).
Prior research indicated poor health care provider adherence with published guidelines in the area of cervical cancer screening (12, 13). Using a database that captured the follow-up of abnormal Pap tests in women aged 18 and over in six independent community health centers between 2004 and 2008, we investigated whether conservative management recommendations in the 2006 American Society of Colposcopy and Cervical Pathology consensus guidelines (11, 14) resulted in less aggressive management of minimally abnormal Pap tests and moderate dysplasia in adolescent women, and whether the guidelines had unintended management consequences in older age groups.
Materials and Methods
Study Design
Our study is a secondary data analysis of the Boston Patient Navigation Research Program. The Patient Navigation Research Program was a multi-site national trial that evaluated the effects of patient navigation, defined as providing support and guidance to vulnerable persons with cancer or abnormal cancer screening tests, on timeliness and quality of care received. The Boston Patient Navigation Research Program is a community-based intervention implemented at six of Boston’s neighborhood community health centers which serve a population of approximately 50,000 low-income and minority women ages 18 and over (17, 18). Eligible participants for the cervical cancer screening arm of the Boston Patient Navigation Research Program, which constituted the total subject pool for the current study, included non-pregnant women 18 years of age and older with a cervical cancer screening abnormality at one of the participating community health centers. Patient charts were reviewed up until the point where participants reached a definitive diagnosis of cancer or non-cancer or were lost to follow-up. Patient and clinic data were collected from electronic medical records between January 1, 2004 and December 31, 2008. New recommendations regarding the management of abnormal Pap tests were published in October 2007, midway through the Boston Patient Navigator Research program study period, creating the opportunity for a natural experiment comparing management prior to new guidelines (1/1/2004–10/31/2007) to management after the publication of new guidelines (11/1/2007–1/1/2009). This study was approved by the Boston University School of Medicine Institutional Review Board.
Data collection
Patient race and ethnicity were collected at the time of clinical registration. For those with missing race and ethnicity, race was imputed using language and birth country using a cross-tab table in SAS. Five race/ethnicity mutually exclusive categories were used: White, Black, Hispanic, Asian, and Other. Patient age was collected from the medical record at the time of abnormal Pap test and reported in years. Patient language was collected at the time of clinical registration. For those missing language, these data were pulled from the text of participant’s medical records. Insurance status was collected at the time of registration. Three insurance categories were used in analyses: public, private, and uninsured. The index abnormality for each patient was defined as the abnormal cervical cancer screening test that made the patient eligible for the study, and included minimally abnormal Pap tests (atypical squamous cells of undetermined significance (ASC-US) positive for HPV infection: ASC-US HPV+ and low-grade squamous intraepithelial lesion (LSIL) as well as high-grade squamous intraepithelial lesions (HSIL). Data were collected during two distinct time periods: 1/1/04–12/31/05 and 1/1/07–12/31/08. The first time period represents baseline data collection and the second represents the intervention portion of the patient navigation study. The patient navigation intervention did not seek to address whether or not health care providers adhered to new guidelines.
Data analysis
We examined 1) whether management of women aged 18–20 with minimally abnormal Pap tests (ASC-US HPV+ and LSIL) changed in response to new guidelines, specifically whether they were more likely to receive repeat Pap tests instead of colposcopy after guideline changes (defined as before or after 10/31/2007); 2) whether management of women ages 21 and over with minimally abnormal Pap tests (ASC-US HPV+ and LSIL) was inadvertently affected by the guidelines, specifically whether they were also more likely to be managed with repeat Pap test instead of colposcopy; 3) whether management of women ages 18–20 with moderate dysplasia (Cervical Intraepithelial Neoplasia grade 2: CIN2) changed in response to new guidelines, specifically whether they were more likely to be managed with repeat colposcopy instead of excisional procedures (LEEP); and 4) whether management of women ages 21 and over with moderate dysplasia (CIN2) was inadvertently affected by new guidelines, specifically whether they were also more likely to be managed with repeat colposcopy instead of excisional procedures (LEEP). To examine the outcomes related to the management of minimally abnormal Pap tests (ASC-US HPV+ and LSIL), patients were stratified by age into three groups: age 18–20, age 21–25, and age 26 and over. Within each age strata, we first performed univariable analyses to determine the relationships between socio-demographic and clinic characteristics of subjects and their receipt of repeat Pap test or colposcopy. Due to the clinical site differences suggested in univariable analyses, we used multivariable logistic regression to examine adjusted effects of the guidelines, patient characteristics, and clinic differences on study outcome. All variables were considered for inclusion in multivariable models. In addition, generalized estimating equation analysis was performed to estimate the effect of patient-level characteristics on adherence to guideline change while controlling for the clustering effect of clinical site of care.
To assess the outcomes related to the management of moderate dysplasia (CIN2), we analyzed differences in the completion of excisional procedures (LEEP) prior to and after guideline changes using the Fisher exact and Chi squared tests. Although guidelines recommend repeat colposcopy for women with moderate dysplasia (CIN2) under age 21 and excisional procedures (LEEP) for women ages 21 and over, literature on regression of lesions includes women up through age 25(6, 7), and some health care providers may choose to defer excisional procedures (LEEP) in nulliparous patients over age 21. Therefore, we performed separate analyses on women ages 18–20, 21–23, 24–25, and 26 and over. We found similar changes in the rates of excisional procedures (LEEP) prior to and after new guidelines in the 18–20 and 21–23 age groups, but different management patterns in women over age 23. Because of similar management outcomes, women ages 18–23 were compared to women ages 24 and over in the final analysis. Analyses were conducted with SAS 9.3.
Results
A total of 1806 women were included in the analysis; 264 (15%) were aged 18–20, and 1542 aged 21 and over. Demographic characteristics prior to and after guideline changes were similar with the exception of a larger proportion of 18–20 year old patients prior to the guideline changes (15% vs. 13%), and a larger proportion of patients from smaller health centers prior to the guideline changes (17% vs. 7% from Health Center F) (Table 1).
Table 1.
Demographics of Patients Whose Abnormal Pap Test Occurred Prior to or After the Release of New Guidelines
| Characteristics |
Preguideline n=1085 |
Postguideline n=721 | Chi-Square |
|---|---|---|---|
| n (%) | n (%) | P | |
| Age group, years | 0.007* | ||
| 18–20 | 169 (15) | 95 (13) | |
| 21–25 | 408 (38) | 234 (33) | |
| 26+ | 508 (47) | 392 (54) | |
| Race or ethnicity | 0.08 | ||
| Hispanic | 321 (30) | 233 (32) | |
| Black | 377 (35) | 222 (31) | |
| White | 307 (28) | 226 (31) | |
| Other | 80 (7) | 40 (6) | |
| Language | 0.23 | ||
| English | 768 (71) | 518 (72) | |
| Spanish | 188 (17) | 135 (19) | |
| Other | 129 (12) | 68 (9) | |
| Index abnormality | 0.11 | ||
| LSIL | 992 (91) | 674 (93) | |
| HSIL | 93 (9) | 47 (7) | |
| Insurance status | 0.06 | ||
| Uninsured | 343 (32) | 194 (27) | |
| Public | 395 (36) | 296 (41) | |
| Private | 347 (32) | 231 (32) | |
| Clinical site | [lt]0.01* | ||
| A | 250 (23) | 216 (30) | |
| B | 254 (24) | 161 (22) | |
| C | 69 (6) | 41 (6) | |
| D | 118 (11) | 94 (13) | |
| E | 209 (19) | 161 (22) | |
| F | 185 (17) | 48 (7) |
Some observed differences may be due to differences in data collection: data collected in 2004–2005 (baseline and feasibility study) included all patients with high grade lesions and a random selection of patients with low grade lesions, while data from 2007–2008 (intervention) included all patients with abnormal Pap tests.
Analysis of the management of minimally abnormal Pap tests (ASC-US HPV+ and LSIL) in women under age 21 revealed that most health care providers adopted the new guidelines. Prior to guideline changes, 78% of young women with minimally abnormal Pap tests (ASC-US HPV+ and LSIL) underwent colposcopy, compared with 45% after guideline changes. Multivariable logistic regression demonstrated a 10-fold increase in the likelihood of receiving a repeat Pap test instead of colposcopy after guideline changes (p<0.001) (See Table 2). Other factors associated with management of minimally abnormal Pap tests (ASC-US HPV+ and LSIL) in women ages 18–20 included clinical site, with patients attending Health Centers A and D being less likely to receive a repeat Pap test than those attending Health Center B. Women who spoke Spanish or were of Latina ethnicity were less likely to receive repeat Pap tests in univariable analyses, but not in multivariable analyses; 50% of Latina patients attended health centers with lower guideline adherence (A and D). Assignment to the control or intervention arm of the patient navigation study was not associated with guideline adherence. The clustering analysis using generalized estimating equations controlling for clinical site of care showed similar results, with a significant increase in likelihood of receiving a Pap test instead of colposcopy following guideline change (OR, 6.09; CI 2.72–13.65). No patient characteristics were found to have an effect on receiving a Pap test before or after guideline change in the analysis using generalized estimating equations.
Table 2.
Multivariable Logistic Regression on the Association of Receiving a Repeat Pap Test Compared With Colposcopy Among Women Ages 18–20 With Minimally Abnormal Pap Tests (Low-Grade Squamous Intraepithelial Lesion and Atypical Squamous Cells of Undetermined Significance Human Papillomavirus +) (n=206*
| Characteristic | Preguideline | Postguideline |
Univariable, Unadjusted |
Multivariable, Adjusted† |
Multivariable, Adjusted |
||
|---|---|---|---|---|---|---|---|
| n=131 | n=75 | OR (95% CI) |
OR (95% CI) |
Wald Χ2P- value |
|||
|
Total n |
Percent Receiving Repeat Pap |
Total n |
Percent Receiving Repeat Pap |
||||
|
Date of Abnormal Pap Finding (LSIL/ ASC- US HPV+) |
|||||||
| Preguideline Date (ref) |
131 | 22% | 0 | 0% | - | - | - |
| Postguideline Date |
0 | 0% | 75 | 55% |
4.24 (2.30 -- 7.84) |
10.22 (4.37 -- 23.88) |
[lt].0001 |
| Site of care | |||||||
| A | 26 | 0% | 18 | 17% |
0.08 (0.02 -- 0.27) |
0.07 (0.01 -- 0.37) |
0.002 |
| B (ref) | 44 | 30% | 21 | 90% | - | - | - |
| C | 12 | 33% | 6 | 100% |
1.29 (0.45 -- 3.68) |
1.77 (0.48-- 6.50) |
0.39 |
| D | 13 | 8% | 10 | 20% |
0.16 (0.04 -- 0.57) |
0.07 (0.01 -- 0.33) |
[lt]0.01 |
| E | 13 | 23% | 10 | 60% |
0.66 (0.25 -- 1.75) |
0.77 (0.17 -- 3.56) |
0.74 |
| F | 23 | 35% | 10 | 50% |
0.67 (0.29 -- 1.57) |
1.02 (0.34 -- 3.11) |
0.97 |
|
Insurance status |
|||||||
| Uninsured | 40 | 23% | 19 | 53% |
0.80 (0.41 -- 1.58) |
1.54 (0.66 -- 3.60) |
0.32 |
| Public (ref) | 62 | 23% | 40 | 60% | - | - | - |
| Private | 29 | 21% | 16 | 44% |
0.68 (0.32 -- 1.46) |
0.57 (0.21 -- 1.56) |
0.28 |
| Language | |||||||
| English (ref) | 110 | 26% | 62 | 55% | - | - | - |
| Spanish Other | 14 | 7% | 7 | 14% |
0.18 (0.04 -- 0.80) |
0.60 (0.08 -- 4.58) |
0.63 |
| 7 | 0% | 6 | 100% |
0.98 (0.28 -- 3.49) |
0.97 (0.24 -- 4.01) |
0.97 | |
| Race or ethnicity | |||||||
| Hispanic | 32 | 13% | 18 | 28% |
0.28 (0.12 -- 0.63) |
0.34 (0.09 -- 1.25) |
0.10 |
| Black (ref) | 66 | 30% | 29 | 76% | - | - | - |
| White | 26 | 19% | 24 | 42% |
0.54 (0.26 -- 1.12) |
0.64 (0.18 -- 2.27) |
0.49 |
| Other | 7 | 0% | 4 | 100% |
0.72 (0.20 -- 2.63) |
1.36 (0.23 -- 7.93) |
0.73 |
LSIL, low-grade squamous intraepithelial lesions; ASC-US, atypical squamous cells of undetermined significance; HPV, human papillomavirus.
44 patients were excluded from analysis due to missing diagnostic data (eg, lost to follow-up), and 14 were excluded because their index Pap test was HSIL.
All variables are included in multivariable analysis: date of abnormal finding, site of care, insurance status, language and race or ethnicity.
We performed analyses of women ages 21-25 (n=532) and 26 and over (n=702) with the goal of estimating whether guidelines had unintended effects among adult women, and found no difference in the management of minimally abnormal Pap tests (ASC-US HPV+ and LSIL) prior to and after guideline changes. Among 21–25 year-olds, rates of colposcopy were 96% and 93% (p=0.22) prior to and after guidelines; rates for women aged 26 and older were 95% and 95%, respectively (p=0.88). Consistent with these stable, high rates of colposcopy, no demographic or clinical factors significantly predicted management with respect to date of guideline publication in multivariable analyses of these age groups.
To determine the effects of guideline changes on the management of moderate dysplasia (CIN2) in young women, we examined the management of all cases of moderate dysplasia (CIN2) in our dataset (n=128). Among 18–20 year olds, 6 of 16 (38%) underwent excisional procedures (LEEP) when the initial abnormal Pap test occurred prior to guideline changes, compared with 0 of 3 after guideline changes (p=0.52). Among 21–23 year olds, 17 of 26 (65%) underwent excisional procedures (LEEP) when the initial abnormal Pap test occurred prior to guideline change, compared with 2 of 8 (25%), after guideline changes (p=0.10). No change was seen in women ages 24 and over: 31 of 44 (70%) underwent excisional diagnostic procedure (LEEP) prior to guideline changes compared with 23 of 31 (74%) after guideline changes (p=0.72). Because women aged 18–20 and 21–23 were managed similarly, we combined these age groups in our analysis of excisional procedures (LEEP) completion. Fisher exact analysis of women aged 18–23 revealed a significant decrease in the number of excisional procedures (LEEP)s performed, from 55% prior to guideline changes to 18% after guideline changes (p=0.04) (Figure 1).
Figure 1.
The rate of loop electrosurgical excision procedures (LEEP) among women ages 18–23 years with moderate dysplasia (cervical intraepithelial neoplasia [CIN]2) decreased after guideline changes; no decrease was seen among older women. *P=.04.
Discussion
We used data from six community health centers serving over 50,000 low-income and minority women to determine health care provider adherence to the 2006 American Society for Colposcopy and Cervical Pathology guidelines for conservative management of minimally abnormal Pap tests (ASC-US HPV+ and LSIL) and moderate dysplasia (CIN2) in young women. We observed an overall decrease in the performance of colposcopies in 18–20 year old women with minimally abnormal Pap tests and reduced numbers of excisional procedures in 18–23 year old women with moderate dysplasia after publication of the guidelines. These findings show that the new guidelines were sufficient to change clinical practices among this cohort of health care providers serving an urban population of low-income and minority women.
Existing literature highlights reasons why these guidelines may have been rapidly adopted. First, clinical practice guidelines that are based on clear scientific evidence are more adhered to by health care providers (19, 20), and a robust literature accumulating over more than a decade indicated both high rates of regression of HPV infection and moderate dysplasia (CIN2) in young women (5–7), as well as clear obstetric harms from treatment of cervical dysplasia with excisional procedures(9, 21). These findings were highlighted in medical journals and at national meetings including the American Society of Colposcopy and Cervical Pathology and the American Congress of Obstetricians and Gynecologists prior to publication of the final consensus guidelines, thus health care providers may have been aware of the science underlying the guideline changes. In fact, our data indicated that some adolescents received repeat Pap tests for minimally abnormal Pap tests (ASC-US HPV+ and LSIL) and colposcopy for moderate dysplasia (CIN2) prior to publication of guidelines. Another reason for rapid adoption of guidelines may reflect the medical mantra “first, do no harm.” To avoid harming patients, many health care providers rapidly stop practices that are associated with negative outcomes, a prominent example being the dramatic decrease in use of post-menopausal hormone therapy after publication of the results of the Women’s Health Initiative (22, 23). Therefore, clinicians aware of the obstetric complications associated with excisional procedures (LEEP and cold knife cone) may have been eager to adopt guidelines published with the intent of avoiding these potentially harmful procedures in young women.
Multivariable analysis revealed that site of care impacted the management of minimally abnormal Pap tests (ASC-US HPV+ and LSIL), with women attending Health Centers A and D being more likely to receive colposcopy instead of repeat Pap testing than women at Health Center B. Differences in practice have been noted at the regional, local, and individual health care provider level (24–26), and a combination of individual and clinical systems factors may have played a role in guideline adoption in this case. While the design of this study did not specifically examine system factors within health centers or individual health care provider factors that may have contributed to early or late adoption of guidelines, individual health care provider factors seem to be most prominent based on the workflow related to abnormal Pap test management in these clinical sites. The six clinical sites encompassed 17 separate practices (pediatrics, family medicine, and internal medicine) in which 108 health care providers provided primary care including Pap testing during the study period. In 16 of these practices, abnormal Pap test results were routed directly back to the health care provider who ordered the Pap test, and that individual made the recommendation for colposcopy or repeat Pap test. Only one practice had a referral clinician who triaged all abnormal results. When patients with abnormal Pap tests were diagnosed with moderate dysplasia (CIN2) via colposcopic biopsy, the decision to perform a repeat colposcopy or an excisional procedure (LEEP) was made on an individual basis by the health care provider who had taken the biopsy.
This study has several limitations related to the use of retrospective data from electronic medical records. We accessed data related to the health care providers’ documentation in the patient’s medical chart and procedures ordered, but we do not know the extent of health care provider-patient discussion around management options, nor the degree to which patient preference influenced therapeutic choices. We also did not collect data on patient characteristics that may have influenced the decision to perform an invasive procedure, such as a prior history of abnormal Pap tests, HIV infection, or prior non-compliance with recommended follow-up. In addition, the influence of clinical site on the management of abnormal Pap tests could have reflected health center policy, health care provider education, or provider or patient attitudes, factors that could be explored in future research.
New guidelines for conservative management of minimally abnormal Pap tests and moderate cervical dysplasia in adolescents were quickly adopted among this group of community health centers serving low-income, urban populations. If this trend is observed nationwide, the resulting decrease in excisional procedures (LEEP) may reduce racial disparities in preterm deliveries in the future.
Acknowledgments
Funded by an American Cancer Society Mentored Research Scholar Grant (MRSG-09-151-01) and the Boston Patient Navigation Research Program (NIH grant U01CA116892).
The authors thank Drs. Richard Kalish, James Taylor, Stephen Tringale, Patrick Egan, Nisha Thakrar, and Ms. Barbara Lottero for their involvement in study design, recruitment and implementation at their respective clinical sites, Dr. Rebecca Silliman for her review of manuscript drafts, and Dr. Timothy Heeren for his help with statistical analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors did not report any potential conflicts of interest.
Presented at the Annual Clinical Meeting of the American College of Obstetricians and Gynecologists, May 5–9, 2012, San Diego, California.
Contributor Information
Rebecca B. Perkins, Boston University School of Medicine
Jennifer R. Jorgensen, Boston University School of Public Health
Molly E. McCoy, Boston University School of Medicine
Sharon M. Bak, Boston University School of Medicine
Tracy A. Battaglia, Boston University School of Medicine
Karen M. Freund, Boston University School of Medicine
REFERENCES
- 1.Kahn JA, Lan D, Kahn RS. Sociodemographic factors associated with high-risk human papillomavirus infection. Obstet Gynecol. 2007;110:87–95. doi: 10.1097/01.AOG.0000266984.23445.9c. [DOI] [PubMed] [Google Scholar]
- 2.Dunne EF, Unger ER, Sternberg M, McQuillan G, Swan DC, Patel SS, Markowitz LE. Prevalence of HPV infection among females in the United States. Jama. 2007;297:813–819. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 3. [Accessed 10/7/11];SEER. 2001 http://seer.cancer.gov/statfacts/html/cervix.html#incidence-mortality.
- 4.Clifford G, Franceschi S, Diaz M, Munoz N, Villa LL. Chapter 3: HPV type-distribution in women with and without cervical neoplastic diseases. Vaccine. 2006;24(Suppl 3):S26–S34. doi: 10.1016/j.vaccine.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 5.Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med. 1998;338:423–428. doi: 10.1056/NEJM199802123380703. [DOI] [PubMed] [Google Scholar]
- 6.McAllum B, Sykes PH, Sadler L, Macnab H, Simcock BJ, Mekhail AK. Is the treatment of CIN 2 always necessary in women under 25 years old? Am J Obstet Gynecol. 2011;205 doi: 10.1016/j.ajog.2011.06.069. 478 e1-7. [DOI] [PubMed] [Google Scholar]
- 7.Trimble CL, Piantadosi S, Gravitt P, Ronnett B, Pizer E, Elko A, Wilgus B, Yutzy W, Daniel R, Shah K, Peng S, Hung C, Roden R, Wu TC, Pardoll D. Spontaneous regression of high-grade cervical dysplasia: effects of human papillomavirus type and HLA phenotype. Clin Cancer Res. 2005;11:4717–4723. doi: 10.1158/1078-0432.CCR-04-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright TC, Jr, Cox JT, Massad LS, Carlson J, Twiggs LB, Wilkinson EJ. 2001 Consensus Guidelines for the Management of Women with Cervical Intraepithelial Neoplasia. J Low Genit Tract Dis. 2003;7:154–167. doi: 10.1097/00128360-200307000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Jakobsson M, Gissler M, Paavonen J, Tapper AM. Loop electrosurgical excision procedure and the risk for preterm birth. Obstet Gynecol. 2009;114:504–510. doi: 10.1097/AOG.0b013e3181b052de. [DOI] [PubMed] [Google Scholar]
- 10.Sadler L, Saftlas A. Cervical surgery and preterm birth. J Perinat Med. 2007;35:5–9. doi: 10.1515/JPM.2007.001. [DOI] [PubMed] [Google Scholar]
- 11.Janevic T, Stein CR, Savitz DA, Kaufman JS, Mason SM, Herring AH. Neighborhood deprivation and adverse birth outcomes among diverse ethnic groups. Ann Epidemiol. 2011;20:445–451. doi: 10.1016/j.annepidem.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahern J, Pickett KE, Selvin S, Abrams B. Preterm birth among African American and white women: a multilevel analysis of socioeconomic characteristics and cigarette smoking. J Epidemiol Community Health. 2003;57:606–611. doi: 10.1136/jech.57.8.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright TC, Jr, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D. 2006 consensus guidelines for the management of women with abnormal cervical cancer screening tests. Am J Obstet Gynecol. 2007;197:346–355. doi: 10.1016/j.ajog.2007.07.047. [DOI] [PubMed] [Google Scholar]
- 14.Wright TC, Jr, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D. 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. J Low Genit Tract Dis. 2007;11:223–239. doi: 10.1097/LGT.0b013e318159408b. [DOI] [PubMed] [Google Scholar]
- 15.Meissner HI, Tiro JA, Yabroff KR, Haggstrom DA, Coughlin SS. Too much of a good thing? Physician practices and patient willingness for less frequent pap test screening intervals. Med Care. 2010;48:249–259. doi: 10.1097/MLR.0b013e3181ca4015. [DOI] [PubMed] [Google Scholar]
- 16.Saraiya M, Berkowitz Z, Yabroff KR, Wideroff L, Kobrin S, Benard V. Cervical cancer screening with both human papillomavirus and Papanicolaou testing vs Papanicolaou testing alone: what screening intervals are physicians recommending? Arch Intern Med. 2010;170:977–985. doi: 10.1001/archinternmed.2010.134. [DOI] [PubMed] [Google Scholar]
- 17.Freund KM, Battaglia TA, Calhoun E, Dudley DJ, Fiscella K, Paskett E, Raich PC, Roetzheim RG. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113:3391–3399. doi: 10.1002/cncr.23960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Battaglia TA, Santana MC, Bak S, Gokhale M, Lash TL, Ash AS, Kalish R, Tringale S, Taylor JO, Freund KM. Predictors of timely follow-up after abnormal cancer screening among women seeking care at urban community health centers. Cancer. 2010;116:913–921. doi: 10.1002/cncr.24851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grol R, Dalhuijsen J, Thomas S, Veld C, Rutten G, Mokkink H. Attributes of clinical guidelines that influence use of guidelines in general practice: observational study. Bmj. 1998;317:858–861. doi: 10.1136/bmj.317.7162.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don't physicians follow clinical practice guidelines? A framework for improvement. Jama. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 21.Sadler L, Saftlas A, Wang W, Exeter M, Whittaker J, McCowan L. Treatment for cervical intraepithelial neoplasia and risk of preterm delivery. Jama. 2004;291:2100–2106. doi: 10.1001/jama.291.17.2100. [DOI] [PubMed] [Google Scholar]
- 22.Haas JS, Kaplan CP, Gerstenberger EP, Kerlikowske K. Changes in the use of postmenopausal hormone therapy after the publication of clinical trial results. Ann Intern Med. 2004;140:184–188. doi: 10.7326/0003-4819-140-3-200402030-00009. [DOI] [PubMed] [Google Scholar]
- 23.Hersh AL, Stefanick ML, Stafford RS. National use of postmenopausal hormone therapy: annual trends and response to recent evidence. Jama. 2004;291:47–53. doi: 10.1001/jama.291.1.47. [DOI] [PubMed] [Google Scholar]
- 24.Stafford RS, Blumenthal D, Pasternak RC. Variations in cholesterol management practices of U.S. physicians. J Am Coll Cardiol. 1997;29:139–146. doi: 10.1016/s0735-1097(96)00441-x. [DOI] [PubMed] [Google Scholar]
- 25.Goyert GL, Bottoms SF, Treadwell MC, Nehra PC. The physician factor in cesarean birth rates. N Engl J Med. 1989;320:706–709. doi: 10.1056/NEJM198903163201106. [DOI] [PubMed] [Google Scholar]
- 26.Strasser DC, Smits SJ, Falconer JA, Herrin JS, Bowen SE. The influence of hospital culture on rehabilitation team functioning in VA hospitals. J Rehabil Res Dev. 2002;39:115–125. [PubMed] [Google Scholar]