Abstract
Objectives:
The purpose of the study was to evaluate the effectiveness of the HemCon Dental Dressing (HDD) in controlling post extraction bleeding and to ascertain its role in healing of extraction wounds, as compared to control.
Methods:
The 40 participants in the study were all receiving oral antiplatelet therapy (OAT). A total of 80 extractions were conducted without altering the patients’ drug therapy. The extraction sites were divided into 2 groups: one group received a HDD, and the control group where the conventional method of pressure pack with sterile gauze under biting pressure (followed by suturing if required) was used to achieve haemostasis.
Results:
All HemCon treated sites achieved haemostasis sooner (mean = 53 seconds) than the control sites (mean = 918 seconds) which was statistically significant (P <0.001). Postoperative pain in the HDD group (1.74) was also significantly lower than in the control group (5.26) (P <0.001). Approximately 72.5% of HDD-treated sites showed significantly better postoperative healing when compared to the control site (P <0.001).
Conclusion:
HDD proved to be an excellent haemostatic agent that significantly shortened the bleeding time following dental extraction in patients on OAT. Additionally, HDD offered significantly improved post-operative healing of the extraction socket and less postoperative pain.
Keywords: Platelet aggregation inhibitors, Chitosan, Hemorrhage, Wound healing
Advances in Knowledge
- For patients undergoing simple extractions, the study outcome supports no change in patient’s oral antiplatelet drug regimen.
- Expected results regarding the effectiveness of chitosan were observed.
- This clinical study supports the use of advances in technology (chitosan) to improve patient care.
Application to Patient Care
- Health professionals still prefer to alter drug regimens for patients receiving oral antiplatelet therapy (OAT) prior to minor surgical procedures. This places patients at risk of developing thromboembolism.
- The study results showed earlier haemostasis, less discomfort, and better healing without changing a patient’s OAT regimen when undergoing minor surgical procedures using HDD.
- The study results also support early treatment without repeated evaluations of international normalised ratios in patients receiving OAT regimens.
Medical problems are one of the roadblocks for oral and maxillofacial surgeons; they are expected to manage patients with such ailments with utmost care.1 Excessive bleeding in patients on oral antiplatelet therapy (OAT) is currently one of the most commonly encountered complications in dentistry, making OAT patients some of the most challenging patients to treat.2
Although the prevalence of bleeding disorders in patients being treated by dentists and oral surgeons appears to be small, a study in 1994 showed that 2.3% of 1500 adults seeking dental treatment were on OAT and, indeed, bleeding disorders were more prevalent than cancer, renal disease, or joint replacement.3
When encountering such a patient, a dental surgeon has the choice of either altering or stopping the OAT, which presents a risk of thromboembolism, or continuing the OAT and risking uncontrolled bleeding.4–9 A common approach to managing such patients is suspension of the OAT for 3 to 4 days before surgery, which exposes the patients to a higher risk of thromboembolism, myocardial infarction, and cardiovascular accidents.10,11 Intraoperative or postoperative bleeding is not significantly reduced by this regimen. Other authors have suggested the use of local haemostatic measures to control intra- and postoperative bleeding without altering a patient’s OAT regimen.12–14 Many styptics such as the gelatin sponge, fibrin glue, and tranexamic acid have been used in the past to control intra- and postoperative haemorrhage.
The HemCon Dental Dressing (HDD) (HemCon Medical Technologies, Portland, Oregon, USA) is an USA Food and Drug Administration (FDA) approved material which has been used extensively under the name HemCon Bandage to stop bleeding in combat wounds and other severe trauma.15,16 The HDD is a new generation medical device which offers self-adhesion and provides a protective layer that can be custom cut according to a patient’s need. Although haemostasis proceeds rapidly, there is no heat generated that might cause thermal injury to the wound site.17 HDD is chitin, which is manufactured from freeze dried shrimp shells. Chitin is an insoluble polysaccharide polymer of glucosamine that is purified and partially deacetylated to form soluble chitosan aqueous gel.18,19 Chitosan gel is then freeze dried in moulds to make a highly electropositive sponge-like material that is haemostatic and adapts well to oral surgical wounds. Chitosan is a food grade material which can be safely ingested, and its accidental inhalation risk is almost zero as it undergoes dissolution.
Chitosan has a positive charge and attracts red blood cells (RBC) and platelets, which are negatively charged through ionic interaction; thus, a strong seal is formed at the wound site.16 This supportive, primary seal allows the body to activate its coagulation pathway effectively, initially forming organised platelets. HDDs are designed to maintain this seal and serve as a frontline support structure as the platelets and RBC continue to aggregate until haemostasis is achieved. HDDs do not rely solely on the clotting cascade to maintain haemostasis.20 The strong sealing action allows the body to form a clot naturally. HDD can also be used in haemophiliac patients as clot formation is based on electrostatic charge attraction instead of the normal quantities and functioning of clotting factors. In addition to providing haemostasis, HDD also offers an antibacterial barrier.
The purpose of this study was to evaluate the effectiveness of HDD in controlling post- extraction bleeding and its role in the healing of extraction wounds as compared to more conventional methods such as pressure gauze, followed by suturing if required. For our study, we hypothesised that, in OAT patients, HDD would yield better outcomes as compared to more conventional measures used after tooth extractions.
Methods
A total of 40 adult OAT patients undergoing extractions were chosen randomly for this study after institutional review board approval was obtained. All patients underwent extractions without any alteration to their antiplatelet medication regimens. Included in the study were OAT patients undergoing multiple tooth extractions who were between the ages of 35 and 75 years, and had international normalised ratio (INR) values ≤3 (1–3). Diabetic patients with well-controlled sugar levels were also included. Patients undergoing a single tooth extraction or multiple extractions limited to one quadrant; those with an allergy to seafood; those indicating that they were smokers, and those with genetic bleeding disorders were excluded from the study.
All patients underwent various investigations preoperatively such as haemoglobin estimation (Hb), bleeding time (BT), clotting time (CT), INR, and platelet count (PC). BT measures the primary phase of haemostasis—the interaction of the blood vessel wall and the formation of a haemostatic plug. CT indicates the time interval from the formation of a platelet plug to the completion of vasoconstriction and clot formation. Similar and identical extraction sites were selected within each patient (for example, extraction of the first molars in the right and left quadrants of the lower jaw). A split-mouth study design was used. By this method, a patient would receive HDD on one side of the mouth (study site). On the other side (control side), the conventional method of pressure packing with a sterile piece of gauze under biting pressure, followed by suturing, if required, was used to achieve haemostasis after extraction. To reduce study variability, similar contralateral or counterpart teeth were extracted wherever possible (32 patients). In the other 8 patients, similar sized teeth were selected (i.e. single rooted tooth for single rooted tooth and molar for molar). Neither the surgeon nor the patients could be blinded to the use of HDD versus the control method; however, every second patient’s left side/upper arch was used as a study site. After obtaining consent, each patient underwent atraumatic simple extractions under local anaesthesia using lignocaine with adrenaline (1:80,000). The procedure was completed on a single visit by a single surgeon. Surgical sites were randomly selected for treatment either by a complete or custom-cut HDD in one quadrant and a control consisting of biting pressure on a sterile cotton gauze dressing followed by suturing if required in the other quadrant in each patient. Custom-cut HDDs were used to fit loosely into extraction sockets that were smaller than the size of a complete HDD (10 mm × 12 mm × 5.5 mm). A HDD was placed into the extraction socket at the height of the crestal bone wherever possible. Direct finger pressure was placed over the extraction site for 40–60 seconds after placement of the HDD. Sutures were placed whenever haemostasis was not achieved under biting pressure over the sterile gauze piece after 900 seconds (15 minutes). Timing to haemostasis was noted for both the HDD and control surgical sites using a stopwatch. All patients were prescribed a diclomol tablet (diclofenac sodium 50 mg + paracetamol 500 mg) every 8 hours for 3 days. All patients were reviewed by another surgeon on the 7th postoperative day for assessment of pain and healing. Relative pain scores were assessed 1 week postoperatively. Self-reported pain scores on a scale of 0–10 were taken into account to estimate postoperative pain. Healing was assessed on the basis of epithelization using the visual analogue scale, the presence of liver clots, pus discharge, dry socket, and the extent of the sinus opening. Healing was compared between the study and control sites and was assessed on a scale of 1–3 with 1 representing the healing of the study site being significantly worse than the control; 2 representing the healing of the study site being the same as the control, and 3 meaning the healing of the study site was significantly better than the control.
Secondary bleeding was assessed through patients’ self-reporting and/or by the presence or absence of liver clots. Secondary bleeding/venous haemorrhage is usually characterised by the slow oozing of dark red blood and can manifest as liver clots. Liver clots, which are also known as currant jelly clots, are defined as red, jelly-like clots that are rich in haemoglobin from erythrocytes within the clot. Statistical analysis through a paired t-test and the Wilcoxon signed-rank test was applied for testing statistical significance.
Results
Out of the 40 patients, there were 33 males and 7 females. The mean BT was 192 seconds and the mean PC was 246,000/cc [Table 1].
Table 1:
Details of patient age and various investigations (N = 40)
| Variables | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Age (years) | 56.2 | 9.61 | 38 | 74 |
| Hb (gm %) | 13.2 | 0.92 | 11.6 | 15.8 |
| PC (mm3) | 2,46,900 | 48,113 | 1,14,000 | 3,28,000 |
| BT (seconds) | 192 | 24 | 150 | 240 |
| CT (seconds) | 324 | 30 | 240 | 390 |
Legend: SD = standard deviation; Hb = haemoglobin estimation; PC = platelet count; BT = bleeding time; CT = clotting time.
HDDs that had adhered to the soft/hard tissue adjacent to the extraction site were easily removed after wetting with sterile normal saline, and there was no adherence to the sterile gauze piece used on the control site postoperatively. Time to haemostasis was noted for both the HDD and control surgical sites using a stopwatch. The study site achieved haemostasis at 53 seconds, which was a considerably shorter time than the control site at 918 seconds [Table 2]. There was statistically improved haemostasis with the use of HDD.
Table 2:
Comparison of bleeding time, pain score and quality of healing
| Study site | Control site | P value | |
|---|---|---|---|
| Bleeding time | 53 ± 13 seconds | 918 ± 769 seconds | <0.0001 |
| Pain score | 1.74 ± 0.65 | 5.26 ± 1.33 | <0.0001 |
| Healing | 29 | 0 | <0.0001 |
The postoperative pain experienced by patients throughout the week while performing day-to-day activities such as eating, tooth brushing, etc. were recorded as 0 being no pain and 10 being the worst pain the patient had ever experienced. The average pain score at the study site (1.74) was considerably less than the control site (5.26) [Table 2].
Although we did not experience any cases of liver clots, sinus opening, pus discharge, or dry socket, there was comparatively better epithelialization with the use of HDD. The 29 study sites showed significantly better healing as compared to the control sites [Table 2].
Discussion
Clopidogrel and ticlopidine inhibit adenosine diphosphate (ADP)-induced platelet fibrinogen binding whereas aspirin inhibits the activity of cyclooxygenase. Platelets are affected for the life of the cell, and complete reversal of antiplatelet activity does not occur for approximately 2 weeks. In this study, the HDD was used to control bleeding in extraction wounds in patients receiving OAT. The results show that in every patient the time to haemostasis was shorter when using HDD than when using the control.
Shen et al. showed a release of growth factor from human platelets stimulated by chitosan exposure, which may help explain our positive findings.21 Cunha-Reis et al. showed cell adhesion consistent with the nature of the HDD material used in this study.22 In our study, sites receiving the HDD had improved postoperative healing with minimal complications when compared to the control site. This may be attributed to the antibacterial properties of chitosan, which have been investigated in vitro studies.23,24 Results demonstrated that chitosan increased permeability of the inner and outer membranes and ultimately disrupted the bacterial cell membranes, releasing their contents. Thus HDD provides an antibacterial barrier against a wide range of Gram positive and Gram negative organisms, including methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococcus (VRE), and Acinetobacter baumannii.23,24 In an animal study, Azargoon et al. found HDD to be as efficacious ferric sulfate in haemostasis and wound healing.25
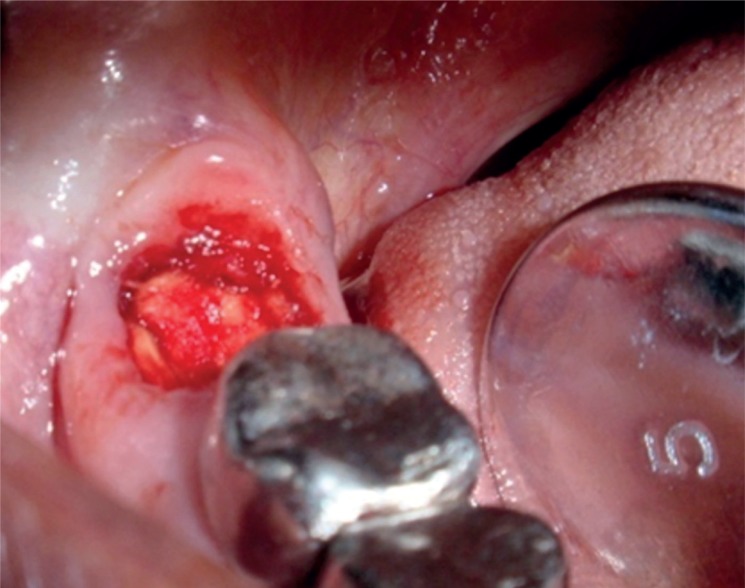
The self-adhesive nature of HDD is caused by the electrostatic attraction of RBC to the HemCon material. As the RBCs bind to the HDD surface, it forms a dense viscous mass that provides adhesion, and also adapts to the alveolar bone’s irregularities under digital pressure, thereby providing frictional locking with the bony socket. Considering the competency of HDD in forming a barrier that seals the wound from exposure to the environment, we can state that only a small amount of HDD (i.e. about ½ of a 10 mm × 12 mm piece) is required to attain complete haemostasis [Figure 1]. There was no clinical indication of the necessity to pack the extraction socket fully, and the excess was easily trimmed chair side, according to the patients’ needs.
Figure 1:
Intraoperative photograph of study site with HemCon Dental Dressing in situ (loosely placed).
Additionally, we observed initial slightly raised pain scores in sites with HDD, which subsided once the acetic acid was fully dissolved in oral fluids. To work, HDD material requires active bleeding; thus, the more bleeding takes place, the better the HDD material performs which is quite useful during surgical procedures.
Conclusion
The results of this study fully support our hypothesis regarding the effectiveness of HDD in patients receiving OAT. They show that HemCon is a new generation haemostatic agent which facilitates early haemostasis of extraction wounds, along with improved healing and reduces postoperative pain.25 The use of HDD eliminates or minimises the risk of thromboembolism by allowing the patient to continue his/her antiplatelet medication regimens; however, the haemostatic properties of the HDD do not obviate the need for thorough pre- and postoperative evaluation and management of a patient’s INR status.
Footnotes
CONFLICT OF INTEREST
The authors declared no conflict of interest
FUNDING
This research was funded by HemCon Inc., USA.
References
- 1.Henderson JM, Bergman S, Salama A, Koterwas G. Management of the oral and maxillofacial surgery patient with thrombocytopenia. J Oral Maxillofac Surg. 2001;59:421–7. doi: 10.1053/joms.2001.21881. [DOI] [PubMed] [Google Scholar]
- 2.Yacabucci JE, Kramer HS., Jr Platelet defects of importance in oral surgery. J Oral Surg. 1972;30:478–85. [PubMed] [Google Scholar]
- 3.Patton LL, Ship JA. Treatment of patients with bleeding disorders. Dent Clin North Am. 1994;38:465–82. [PubMed] [Google Scholar]
- 4.Anavi Y, Sharon A, Gutman D, Laufer D. Dental extractions during anticoagulant therapy. Refuat Hapeh Vehashinayim. 1981;28:9–12. [PubMed] [Google Scholar]
- 5.Blinder D, Martinowitz U, Ardekian L, Peleg M, Taicher S. Oral surgical procedures during anticoagulant therapy. Harefuah. 1996;130:681–3. [PubMed] [Google Scholar]
- 6.Campbell JH, Alvarado F, Murray RA. Anticoagulation and minor oral surgery: should the anticoagulation regimen be altered? J Oral Maxillofac Surg. 2000;58:131–5. doi: 10.1016/s0278-2391(00)90324-0. [DOI] [PubMed] [Google Scholar]
- 7.Blinder D, Manor Y, Martinowitz U, Taicher S. Dental extractions in patients maintained on oral anticoagulant therapy: Comparison of INR value with occurrence of postoperative bleeding. Int J Oral Maxillofac Surg. 2001;30:518–21. doi: 10.1054/ijom.2001.0172. [DOI] [PubMed] [Google Scholar]
- 8.Conti CR. Aspirin and elective surgical procedures. Clin Cardiol. 1992;15:709–10. doi: 10.1002/clc.4960151026. [DOI] [PubMed] [Google Scholar]
- 9.Handin RI. Disorders of the Platelet and Vessel Wall. In: Harrison I, Randolph T, Isselbacher K, editors. Harrison’s Principle of Internal Medicine. 13th ed. New York: McGraw-Hill; 1994. pp. 1798–803. [Google Scholar]
- 10.Beirne OR. Evidence to continue oral anticoagulant therapy for ambulatory oral surgery. J Oral Maxillofac Surg. 2005;63:540–5. doi: 10.1016/j.joms.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 11.US Army Medical Department High-Tech Bandages. From: www.armymedicine.army.mil/about/tl/factsbandages.html. Accessed: May 2012.
- 12.Blinder D, Manor Y, Martinowitz U, Taicher S, Hashomer T. Dental extractions in patients maintained on continued oral anticoagulant: Comparison of local hemostatic modalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:137–40. doi: 10.1016/s1079-2104(99)70106-x. [DOI] [PubMed] [Google Scholar]
- 13.Cannon PD, Dharmar VT. Minor oral surgical procedures in patients on oral anticoagulants--a controlled study. Aust Dent J. 2003;48:115–8. doi: 10.1111/j.1834-7819.2003.tb00019.x. [DOI] [PubMed] [Google Scholar]
- 14.Madan GA, Madan SG, Madan G, Madan AD. Minor oral surgery without stopping daily low-dose aspirin therapy: A study of 51 patients. J Oral Maxillofac Surg. 2005;63:1262–5. doi: 10.1016/j.joms.2005.05.164. [DOI] [PubMed] [Google Scholar]
- 15.Della Valle A, Sammartino G, Marenzi G, Tia M, Espedito di Lauro A, Ferrari F, et al. Prevention of postoperative bleeding in anticoagulated patients undergoing oral surgery: Use of platelet-rich plasma gel. J Oral Maxillofac Surg. 2003;61:1275–8. doi: 10.1016/s0278-2391(03)00727-4. [DOI] [PubMed] [Google Scholar]
- 16.Wedmore I, McManus JG, Pusateri AE, Holcomb JB. A special report on the chitosan-based hemostatic dressing: experience in current combat operations. J Trauma. 2006;60:655–8. doi: 10.1097/01.ta.0000199392.91772.44. [DOI] [PubMed] [Google Scholar]
- 17.Chou TC, Fu E, Wu CJ, Yeh JH. Chitosan enhances platelet adhesion and aggregation. Biochem Biophys Res Commun. 2003;302:480–3. doi: 10.1016/s0006-291x(03)00173-6. [DOI] [PubMed] [Google Scholar]
- 18.Kumar MN, Muzzarelli RA, Muzzarelli C, Sashiwa H, Domb AJ. Chitosan chemistry and pharmaceutical perspectives. Chem Rev. 2004;104:6017–84. doi: 10.1021/cr030441b. [DOI] [PubMed] [Google Scholar]
- 19.Yang J, Tian F, Wang Z, Wang Q, Zeng YJ, Chen SQ. Effect of chitosan molecular weight and deacetylation degree on hemostasis. J Biomed Mater Res B Appl Biomater. 2008;84:131–7. doi: 10.1002/jbm.b.30853. [DOI] [PubMed] [Google Scholar]
- 20.Malmquist JP, Clemens SC, Oien HJ, Wilson SL. Hemostasis of oral surgery wounds with the HemCon Dental Dressing. J Oral Maxillofac Surg. 2008;66:1177–83. doi: 10.1016/j.joms.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 21.Shen EC, Chou TC, Gau CH, Tu HP, Chen YT, Fu E. Releasing growth factors from activated human platelets after chitosan stimulation: a possible bio-material for platelet-rich plasma preparation. Clin Oral Implants Res. 2006;17:572–8. doi: 10.1111/j.1600-0501.2004.01241.x. [DOI] [PubMed] [Google Scholar]
- 22.Cunha-Reis C, TuzlaKoglu K, Baas E, Yang Y, El Haj A, Reis RL. Influence of porosity and fibre diameter on the degradation of chitosan fibre-mesh scaffolds and cell adhesion. J Mater Sci Mater Med. 2007;18:195–200. doi: 10.1007/s10856-006-0681-x. [DOI] [PubMed] [Google Scholar]
- 23.Burkatovskaya M, Tegos GP, Swietlik E, Demidova TN, P Castano A, Hamblin MR. Use of chitosan bandage to prevent fatal infections developing from highly contaminated wounds in mice. Biomaterials. 2006;27:4157–64. doi: 10.1016/j.biomaterials.2006.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Speechley JA, Rugman FP. Some problems with anticoagulants in dental surgery. Dent Update. 1992;19:204–6. [PubMed] [Google Scholar]
- 25.Azargoon H, Williams BJ, Solomon ES, Kessler HP, He J, Spears R. Assessment of hemostatic efficacy and osseous wound healing using HemCon dental dressing. J Endod. 2011;37:807–11. doi: 10.1016/j.joen.2011.02.023. [DOI] [PubMed] [Google Scholar]