Abstract
Objectives:
Although team-based learning (TBL) is widely used in medical education, its evaluation from the perspectives of the students exposed to it has been limited. This paper reports on a quantitative and qualitative evaluation of perceptions of first year medical students towards TBL.
Methods:
Lectures in an anatomy course were transformed into a series of TBL sessions for two cohorts of first-year medical students. Each session consisted of pre-class reading, in-class readiness assurance tests, and problem-solving of clinical cases by student teams. At the end of each course, students were surveyed using qualitative and quantitative instruments to assess their perceptions of the strategy. Internal consistency of questionnaire items was determined by a reliability analysis (Cronbach’s alpha). Principal component factor analysis and correspondence analysis were conducted on the quantitative data. Open-ended questions were explored by thematic analysis.
Results:
Students’ evaluations indicated that TBL is a welcome alternative to lecture-based teaching; as implemented in this study, it encouraged clinical problem solving and fruitful in-class discussion. Principal component factor analysis identified five factors (Cronbach’s alpha 0.602–0.875). However, the majority of students disapproved of mixed gender TBL teams. Most students agreed that the strategy facilitated consistency in their study, generated an increased awareness about self-directed learning, and had a positive impact on their learning attitudes.
Conclusion:
TBL is a welcome instructional strategy as reported by our first-year medical students. It was perceived to be a better approach compared to content-based lectures. The effect on actual student performance is currently being investigated.
Keywords: Active learning, Problem solving, Attitudes, Cooperative behavior, Oman
Advances in knowledge
- The implementation of TBL is feasible in the early years of undergraduate training, especially in a setting similar to that of Sultan Qaboos University’s College of Medicine & Health Sciences.
- Team-based learning is a refreshing alternative to lectures as a method of teaching large groups.
Application to patient care
- Although this strategy was implemented in the basic sciences, there are implications for patient care. Through TBL, students begin to learn about teamwork, peer assessment, and clinical reasoning, which have positive implications for their ability to provide quality patient care in the future.
“I wish all our lectures will be like this TBL.”
First year medical student.
One of the global trends in teaching in medical schools has been a move towards more student-centered, integrated, clinical application models.1–3 In addition, teaching strategies that promote active learning and problem-solving are increasingly being advocated.4–7 An example of such a strategy that combines features of student-centeredness and problem-solving attributes is team-based learning (TBL).8 In its classical format, TBL employs a structured three-phase sequence during which learners study an advanced assignment defined by faculty, demonstrate knowledge through individual and group readiness assurance tests (IRATs, GRATs), and apply course concepts to problem-solving exercises designed by faculty and analysed by teams.9 The method employs strategies that incorporate the effectiveness of small group learning methods like problem-based learning (PBL) into large-group, lecture-oriented sessions.10,11
Adequate knowledge of basic sciences such as anatomy, with a strong emphasis on ‘clinical application’, logical learning, and developing effective problem solving skills is considered crucial for effective and safe clinical practice.12,13 Although numerous strategies have been employed to develop these skills, implementing them early in the curriculum can be a great challenge. This is especially so in cases where the students have had little or no previous exposure to active learning and teamwork.14–16
In many medical curricula, the teaching methodology in basic sciences is largely characterised by content-based, tutor-centered lectures with hardly any problem-based or student-centered activities.17 This is despite the increasing recognition of the importance of early student introduction to clinical application, active learning, and group problem solving.15,16,18,19 One of the newer methods to develop these skills is the TBL method, first introduced by Michaelsen et al. for teaching large classes in business schools.10 Other significant motivators for implementing TBL were to introduce peer teaching and learning, keep students more engaged during in-class activities, and encourage students to take responsibility for their own learning. However, unlike other well-established teaching strategies, such as PBL, TBL has only recently been employed as an active learning strategy in medical education.20–23
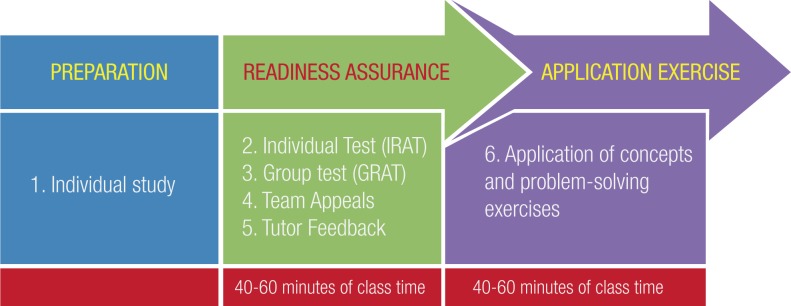
In its classical format [Figure 1], TBL employs a structured three-phase sequence: preparation, during which learners study an advance assignment defined by faculty; readiness assurance, where learners demonstrate knowledge through individual and group readiness assurance tests (IRATs and GRATs), and application, where learners apply course concepts to problem-solving exercises designed by faculty and analysed by teams.9
Figure 1:
The sequence of activities in a classical team-based learning (TBL) strategy
In this study, we evaluated the implementation of the TBL strategy over two semesters in the first year of a medical curriculum by using a survey that elicited student perceptions of both the process and its facilitation of their learning.
Methods
The College of Medicine & Health Sciences (COM&HS) at Sultan Qaboos University (SQU) has recently adopted an integrated, presentation-based, outcome-based and student-centered curriculum. The six-year curriculum is organised into three phases: foundation of medical sciences (one year), integrated organ-system phase (2.5 years), and clerkship phase (2.5 years). Teaching methods during the first two phases include didactic lectures, laboratory sessions (including clinical skills) and tutor-led seminars. The majority of students have had 12 years of secondary education which is an entry qualification to SQU. Although the implementation of the TBL strategy is part of the ongoing innovation in teaching within the medical school, this study was conducted as part of a teaching scholarship in medicine. As such, ethical approval was sought and granted by the COM&HS Medical Ethics & Research Committee. Before photographs were taken of students engaged in the TBL activity, they were informed of the intention to publish some of the images as part of a journal article. Therefore, consent was sought and permission given by the students.
In place of lectures in the Introduction to Anatomy course during the foundation phase, a modified TBL strategy was employed during two semesters of the academic year.24 The remaining contact time was utilised for laboratory practical sessions in the dissecting room.
Teams of six to seven students were formed by random sorting at the beginning of the semester and the students remained on the same teams throughout the course.25 In view of cultural sensitivities regarding mixing of genders, each group consisted of members of the same gender. The students remained in the same group throughout each semester.
Reading materials, multiple choice questions (MCQs) for readiness assurance (IRAT and GRAT) were prepared well before the semester started.26 Such reading materials were uploaded onto the Moodle™ learning management software accessible to all students. Additional study materials included readings from recommended textbooks, prosected specimens in the anatomy laboratory, as well as an image bank created on the learning management platform. The contents of all the reading materials were linked to a list of learning objectives for each of the eleven TBL sessions.
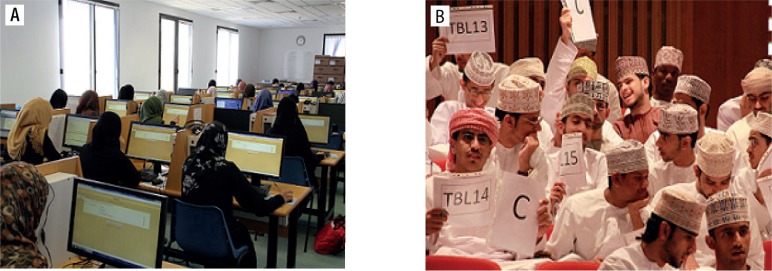
Each of the modified TBL sessions consisted of 3 phases: pre-class preparation, readiness assurance testing (including application of concepts to patient cases) and tutor wrap-up [Figure 1]. A trial TBL session was held to familiarise students with the entire concept. The first phase occurred prior to the TBL session and was completed by each student individually. The second and third phases occurred during the two-hour TBL session and involved individual students, their TBL teams, and the entire class [Figures 2A to 2D]. A final post-TBL reflection occurred at the end of the course consisting of peer evaluation where students within each team assessed one another with respect to teamwork and interpersonal skills. The whole TBL activity accounted for 20% of the overall course grade. This was distributed as 16%, 3% and 1% for individual quizzes (IRAT), group quizzes (GRAT), and peer evaluation, respectively.
Figure 2:
After individual study, the second and third phases were conducted in the computer laboratory and lecture theatre. (A) The individual readiness assurance test (IRAT) was administered in the computer laboratory. (B) The group readiness assurance test (GRAT).
The whole process strategy was evaluated both qualitatively and quantitatively. Students were asked about their perceptions through a six-point Likert-type questionnaire consisting of 22 items. Their responses were rated on a scale of 1–6 (1 = strongly disagree, 2 = disagree, 5 = agree, and 6 = strongly agree). The neutral (undecided) scale was split into two (3 = undecided but leaning towards disagree, and 4 = undecided but leaning towards agree) to increase the chance of obtaining either a positive or negative perception of the activity. In addition, the students were also asked a number of open-ended questions to solicit comments on the positive and negative aspects of TBL, and to garner suggestions as to where improvements could be made.
To aid in the identification of items to be included in the questionnaire, the course faculty conducted focus group meetings with students to explore aspects of the strategy they valued and appreciated. Themes from the focus groups were used to create a formal questionnaire to elicit student feedback about their experiences with TBL. To ensure face and content validity, the questionnaire was initially pilot-tested on 10 students before being administered to the whole class. The questions were directed at probing students’ level of preparation for RATs, the usefulness of learning issues for acquiring knowledge, the perceived importance of group discussion for deeper understanding, and students’ attitudes about the facilitation of the strategy.
Quantitative data analysis was carried out with Statistical Package for the Social Sciences (SPSS, Version 16.0, Polar Engineering and Consulting, Chicago, Illinois, USA, 2007). A principal components factor analysis with varimax rotation (Kaiser normalisation) was conducted on the complete quantitative data set. The internal consistency of questionnaire items was determined by reliability analysis (Cronbach’s alpha). Correspondence analysis based on gender was carried out on items with the highest mean score. All open-ended responses were categorised into common themes.
Results
A total of 125 out of 170 students completed the online questionnaire (response rate = 73.5%). A principal components factor analysis with varimax rotation (Kaiser normalisation) yielded five factors (subscales) with Eigen values greater than 1.0. The five factors, comprising 22 items, accounted for 66.7% of the overall variance and were determined to represent motivation (43.6%), teamwork (4.8%), learning objectives (6.9%), knowledge application (6.1%), and facilitation (5.1%), each with 3–5 items [Table 1].
Table 1:
Mean score and percentage of students responding 1–6 (strongly disagree–strongly agree) to items in the quantitative questionnaire (N = 125)
| Item | Percent Responding* | ||||||
|---|---|---|---|---|---|---|---|
| Strongly Disagree | Strongly Agree | Mean Score | |||||
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Motivation | 5.2 | ||||||
| I prefer TBL to normal lectures | 0.8 | 3.2 | 2.4 | 15.2 | 28.0 | 50.4 | 5.1 |
| TBL strategy motivated me to study hard | 1.9 | 2.8 | 2.8 | 17.6 | 40.7 | 34.3 | 5.4 |
| I look forward to learn again in a TBL course. | 2.4 | 0 | 5.6 | 14.4 | 26.4 | 51.2 | 5.1 |
| TBL challenged me to give my best. | 2.4 | 2.4 | 6.4 | 9.6 | 23.2 | 56.0 | 5.3 |
| I felt sad when I missed a TBL session. | 4.0 | 0 | 4.0 | 1.6 | 32.8 | 57.6 | 4.9 |
| TBL had a positive impact on my learning. | 1.6 | 0.8 | 2.4 | 8.0 | 42.4 | 44.8 | 5.1 |
| Teamwork | 4.1 | ||||||
| TBL helped me learn how to study in a group. | 12.0 | 16.0 | 11.2 | 13.6 | 23.2 | 24.0 | 4.5 |
| I would prefer to be in a mixed gender TBL team. | 16.8 | 18.4 | 8.8 | 4.8 | 7.6 | 3.6 | 3.1 |
| I frequently studied with my colleagues. | 5.6 | 2.4 | 2.4 | 14.4 | 34.4 | 40.8 | 3.5 |
| Discussion during GRATs helped me comprehend better. | 4.0 | 4.8 | 9.6 | 18.4 | 28.0 | 35.2 | 4.9 |
| TBL required more hard work by the students. | 4.0 | 1.6 | 9.6 | 12.0 | 41.6 | 31.2 | 4.7 |
| Learning Objectives | 5.1 | ||||||
| The IRAT was a good test of my knowledge. | 0.8 | 3.2 | 2.4 | 9.6 | 34.4 | 49.6 | 5.0 |
| The course materials were essential for the TBL. | 0.8 | 3.2 | 2.4 | 9.6 | 34.4 | 49.6 | 5.2 |
| I understood the learning objectives of the TBL. | 2.4 | 0.8 | 0.8 | 12.8 | 39.2 | 44.0 | 5.2 |
| I was able to achieve the learning objectives set. | 5.6 | 4.8 | 12.0 | 20.8 | 26.4 | 30.4 | 5.2 |
| Knowledge application | 5.1 | ||||||
| The GRAT was useful for applying knowledge. | 2.4 | 0.8 | 0.8 | 11.2 | 42.4 | 42.4 | 5.1 |
| TBL promoted understanding rather than memorisation. | 3.2 | 0 | 0 | 18.4 | 33.6 | 44.8 | 5.1 |
| TBL made me apply what I learned. | 3.2 | 0.8 | 8.8 | 20.0 | 35.2 | 32.0 | 5.0 |
| Facilitation | 5.0 | ||||||
| The TBL course is well-organised. | 2.4 | 1.6 | 6.4 | 17.6 | 35.2 | 36.8 | 4.9 |
| I was satisfied with this TBL approach. | 0.8 | 3.2 | 2.4 | 14.4 | 44.8 | 34.4 | 5.0 |
| The venue of the TBL was comfortable. | 1.6 | 3.2 | 12.8 | 17.6 | 27.2 | 37.6 | 4.8 |
| The duration of the TBL was just right. | 1.6 | 1.6 | 0 | 13.6 | 18.4 | 64.8 | 5.4 |
Legend: TBL = team-based learning; GRAT = group readiness assurance test; IRAT = individual readiness assurance test
Internal consistency (Cronbach’s alpha) for the 22-item questionnaire response was 0.933. Within each subscale, internal consistency of items is shown in Table 2. The motivation subscale had the highest rating (0.833) whilst teamwork had the lowest (0.602).
Table 2:
Internal consistency analysis (Cronbach’s alpha) for component factors (subscales) identified in the questionnaire
| Factor | Cronbach’s Alpha |
|---|---|
| Motivation | 0.875 |
| Teamwork | 0.602 |
| Learning objectives | 0.861 |
| Knowledge application | 0.806 |
| Facilitation | 0.768 |
Correspondence analysis by gender on items with the highest mean score in each of the five subscales is shown in Table 2. The teamwork item had the lowest percentage of positive perception by both male and female students (58.6% and 67.1% respectively). Male students felt more motivated by the strategy than females (82.3% and 68.4% respectively). In contrast, more female students agreed that the strategy helped them achieve the set objectives of the sessions than males (88.1% and 79.3% respectively).
A total of 50 students (40%) responded to the open-ended questions. They provided 75 responses, out of which four themes emerged from content analysis [Table 4]. Most students agreed that the strategy promoted deeper learning and was an enjoyable experience. The strategy also helped nurture self-directed learning. Although the composition of each TBL group was of the same gender, interestingly, the majority of students (70%) was opposed to the possibility of having mixed gender TBL groups in the future.
Table 4:
Open-ended questionnaire responses categorised into common themes
| Theme | Percentage (n) of comments* | Sample comment |
|---|---|---|
| Deep learning | 88 (110) | “... it is a good way to remember information for long time” |
| Team formation | 70 (88) | “I do not agree to mixed gender TBL group” |
| Motivated learning | 82 (103) | “I really like TBL and hope to have it again and again” |
| Self-directed learning | 74 (93) | “I spend a lot of time for preparing for the TBL ..., it helped me a lot” |
Most students wrote comments that touched on multiple themes. Legend: TBL = team-based learning
Discussion
TBL was introduced early in the medical curriculum with a view to improving upon the teaching-learning experience and to create an active learning environment for our students. In addition, it was thought advantageous to introduce the concept of self-directed learning and team working very early in the curriculum. The combination of the quantitative and qualitative approaches in this evaluation helped to complement the findings of each approach. The five factors identified by factor analysis explained a good percentage (66.7%) of the variance. Qualitative analysis of students’ responses to open-ended questions supported the quantitative data and added valuable information to be considered in future improvements in using TBL. The main strengths of the strategy, as perceived by the students, were related to considering TBL an enjoyable learning experience, with the invaluable potential to enhance students’ learning attitudes.
TBL advocates self-directed learning of course content and student application of this new knowledge within small collaborative teams and full classroom discussions, thus promoting deeper learning. Being aware that the IRAT will be administered at the beginning of a TBL session motivated students to prepare well by attempting to master independently the knowledge contained in the advanced assignment.
Nieder et al. have used the TBL method for teaching gross anatomy and embryology. Their first experience with this method was positive. The students felt that working in teams was an effective way of learning content and applying this to practice clinical reasoning skills.27
Other studies have shown that student perception of knowledge acquisition with the TBL method compared favourably with more traditional methods such as lectures.24,28–30 For example, Parmelee et al. recently assessed the attitudes of medical students to TBL in the pre-clinical curriculum. They reported high rates of agreement in response to a questionnaire assessing overall satisfaction with the impact of TBL on learning quality.31
We made two interesting observations during this study: first, our students seem not to value team-work as much as the other aspects of TBL and, second, they were reluctant to accept mixed gender teams. This lack of enthusiasm for teamwork could be related to the competitive atmosphere in secondary school. During secondary education, ranking of students is widely used as a means of selection and reward. This competitive atmosphere usually results in students being reluctant to share information. With regards to their opposition to mixed groups, this could be related to the fact than many of the students have been nurtured in a fairly traditional society where secondary education is segregated and mixing with the opposite genders is generally frowned upon. As the university is the first setting where both genders share a common learning environment, it appears that they are not ready yet to accept this change. It will be interesting to find out how these attitudes develop as they mature in the university environment. In addition, the finding that significantly more male students felt motivated by the strategy than females might be related to gender differences in learning styles. Student learning style is based on the sensory preference of the individual. These sensory modalities are defined by the neural system that is preferred when receiving information: visual (V), aural (A), mixed read-write (R), and kinaesthetic (K), collectively known as VARK.32
Students with a V preference learn best by seeing or observing (drawings, pictures, diagrams, demonstrations, etc). Learners that prefer A are best suited to learn by listening to or recording lectures, discussing material, and talking through material with themselves or others. R-type learners learn through interactions with textual materials. K-style learners perform best by using physical experiences: touching, performing an activity, moving, doing things within a lesson, and manipulating objects. Student learners are capable of using all of these sensory modes of learning; however, each individual has a unique preference, or set of preferences, in which one mode is often dominant.33 The fact that we found females to be less motivated than males could possibly be because more of them dislike the A nature of TBL learning compared to males. Indeed, some studies have shown that majority of females prefer mixed R and K learning styles and dislike A styles.34
Admittedly, this study suffers from some limitations. First, because the study was cross-sectional, we could not determine the long-term effects of TBL in changing students’ attitudes towards self-directed learning and teamwork. Second, it remains to be seen how the experience will translate into improved learning as evidenced by better examination scores. Third, its impact on future collaborative medical practice remains to be evaluated. These issues will be the focus of our future studies on this teaching strategy.
Conclusion
In summary, our initial experience with a modified TBL process adopted for our first year medical students demonstrated that they perceived the strategy to be more rewarding and enjoyable than regular lecture-based teaching. Despite their initial misgivings regarding team work and the mixing of genders during group learning, we believe that with time and experience, TBL has the potential to be an effective and highly valued learning strategy in settings similar to SQU’s, thus providing an environment that promotes active learning and deeper understanding of the subject matter.
Table 3:
Correspondence analysis by gender of items with the highest mean score in each factor (subscale)
| (Factor) Item | *Percentage responding (n) | |
|---|---|---|
| Males n = 58 | Females n = 67 | |
| (Motivation) TBL strategy motivated me to study harder | 82.3 (48) | 68.4 (46) |
| (Teamwork) Discussion during GRATs helped me comprehend better | 58.6 (34) | 67.1 (45) |
| (Learning objectives) I was able to achieve the learning objectives set | 79.3 (46) | 88.1 (59) |
| (Knowledge Application) TBL promoted understanding rather than memorisation | 81.0 (47) | 76.1 (51) |
| (Facilitation) The duration of the TBL session was just right | 81.0 (47) | 85.0 (57) |
Percentage of students who responded ‘agree’ or ‘strongly agree’ Legend: TBL = team-based learning; GRAT =group readiness assurance test.
Footnotes
CONFLICT OF INTEREST
The author declared no conflict of interest.
References
- 1.Harden RM, Davis MH, Crosby JR. The new Dundee medical curriculum: a whole that is greater than the sum of the parts. Med Educ. 1997;31:264–71. doi: 10.1111/j.1365-2923.1997.tb02923.x. [DOI] [PubMed] [Google Scholar]
- 2.Hook KM, Pfeiffer CA. Impact of a new curriculum on medical students’ interpersonal and interviewing skills. Med Educ. 2007;41:154–9. doi: 10.1111/j.1365-2929.2006.02680.x. [DOI] [PubMed] [Google Scholar]
- 3.Wijnen-Meijer M, Ten Cate TJ, Van der Schaaf M, Borleffs JC. Vertical integration in medical school: Effect on the transition to postgraduate training. Med Educ. 2010;44:272–9. doi: 10.1111/j.1365-2923.2009.03571.x. [DOI] [PubMed] [Google Scholar]
- 4.Harden RM. Twelve tips to encourage better teaching. Med Teach. 1992;14:5–9. doi: 10.3109/01421599209044009. [DOI] [PubMed] [Google Scholar]
- 5.Harden RM, Sowden S, Dunn WR. Educational strategies in curriculum development: the SPICES model. Med Educ. 1984;18:284–97. doi: 10.1111/j.1365-2923.1984.tb01024.x. [DOI] [PubMed] [Google Scholar]
- 6.Hook KM, Pfeiffer CA. Impact of a new curriculum on medical students’ interpersonal and interviewing skills. Med Educ. 2007;41:154–9. doi: 10.1111/j.1365-2929.2006.02680.x. [DOI] [PubMed] [Google Scholar]
- 7.Wijnen-Meijer M, Ten Cate TJ, Van der Schaaf M, Borleffs JC. Vertical integration in medical school: Effect on the transition to postgraduate training. Med Educ. 2010;44:272–9. doi: 10.1111/j.1365-2923.2009.03571.x. [DOI] [PubMed] [Google Scholar]
- 8.Michaelsen L, Black R. Building learning teams: The key to harnessing the power of small groups in higher education. In: Kadel S, Keener J, editors. Collaborative Learning: A Sourcebook for Higher Education. Vol. 2. State College, Pensylvania: National Center for Teaching, Learning, and Assessment; 1994. pp. 65–81. [Google Scholar]
- 9.Michaelsen L, Knight A, Fink L. Team-Based Learning: A Transformative Use of Small Groups in College Teaching. Sterling (VA): Stylus Publishing; 2004. pp. 85–9. [Google Scholar]
- 10.Michaelsen L, Fink L, Knight A. Designing effective group activities: lessons for classroom teaching and faculty development. In: DeZure D, editor. To Improve the Academy: Lessons for Classroom Teaching and Faculty Development. Stillwater (OK): New Forums Press; 1997. pp. 1–19. [Google Scholar]
- 11.Michaelsen L. Getting started with team-based learning. In: Michaelsen L, Knight A, Fink L, editors. Team-Based Learning: A Transformative Use of Small Groups. Westpoint (CN): Praeger; 2002. pp. 27–51. [Google Scholar]
- 12.Boon JM, Meiring JH, Richards PA. Clinical anatomy as the basis for clinical examination: Development and evaluation of an introduction to clinical examination in a problem-oriented medical curriculum. Clin Anat. 2002;15:45–50. doi: 10.1002/ca.1091. [DOI] [PubMed] [Google Scholar]
- 13.Heylings DJ. Anatomy 1999–2000: The curriculum, who teaches it and how? Med Educ. 2002;36:702–10. doi: 10.1046/j.1365-2923.2002.01272.x. [DOI] [PubMed] [Google Scholar]
- 14.Geuna S, Giacobini-Robecchi MG. The use of brainstorming for teaching human anatomy. Anat Rec. 2002;269:214–6. doi: 10.1002/ar.10168. [DOI] [PubMed] [Google Scholar]
- 15.Miller SA, Perrotti W, Silverthorn DU, Dalley AF, Rarey KE. From college to clinic: Reasoning over memorization is key for understanding anatomy. Anat Rec. 2002;269:69–80. doi: 10.1002/ar.10071. [DOI] [PubMed] [Google Scholar]
- 16.Holla SJ, Selvaraj KG, Isaac B, Chandi G. Significance of the role of self-study and group discussion. Clin Anat. 1999;12:277–80. doi: 10.1002/(SICI)1098-2353(1999)12:4<277::AID-CA7>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz PL. Active, small group learning with a large group in a lecture theatre: A practical example. Med Teach. 1989;11:81–6. doi: 10.3109/01421598909146279. [DOI] [PubMed] [Google Scholar]
- 18.Scott TM. A case-based anatomy course. Med Educ. 1994;28:68–73. doi: 10.1111/j.1365-2923.1994.tb02688.x. [DOI] [PubMed] [Google Scholar]
- 19.Michael J. Where’s the evidence that active learning works? Adv Physiol Educ. 2006;30:159–67. doi: 10.1152/advan.00053.2006. [DOI] [PubMed] [Google Scholar]
- 20.Haidet P, O’Malley KJ, Richards B. An initial experience with “team learning” in medical education. Acad Med. 2002;77:40–4. doi: 10.1097/00001888-200201000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Seidel CL, Richards BF. Application of team learning in a medical physiology course. Acad Med. 2001;76:533–4. doi: 10.1097/00001888-200105000-00071. [DOI] [PubMed] [Google Scholar]
- 22.Nieder GL, Parmelee DX, Stolfi A, Hudes PD. Team-based learning in a medical gross anatomy and embryology course. Clin Anat. 2005;18:56–63. doi: 10.1002/ca.20040. [DOI] [PubMed] [Google Scholar]
- 23.Koles P, Nelson S, Stolfi A, Parmelee D, Destephen D. Active learning in a Year 2 pathology curriculum. Med Educ. 2005;39:1045–55. doi: 10.1111/j.1365-2929.2005.02248.x. [DOI] [PubMed] [Google Scholar]
- 24.Dunaway GA. Adaption of team learning to an introductory graduate pharmacology course. Teach Learn Med. 2005;17:56–62. doi: 10.1207/s15328015tlm1701_10. [DOI] [PubMed] [Google Scholar]
- 25.McMahon K. Team formation. In: Michaelsen L, Parmelee D, McMahon K, Levine R, editors. Team-Based Learning for Health Professions Education. Sterling (VA): Stylus Publishing; 2008. pp. 85–8. [Google Scholar]
- 26.Michaelsen L, Sweet M. Fundamental Principles and Practices of Team-based Learning. In: Michaelsen L, Parmelee D, McMahon K, Levine R, editors. Team-Based Learning for Health Professions Education. Sterling, Virginia: Stylus Publishing; 2008. pp. 9–34. [Google Scholar]
- 27.Nieder GL, Parmelee DX, Stolfi A, Hudes PD. Team-based learning in a medical gross anatomy and embryology course. Clin Anat. 2005;18:56–63. doi: 10.1002/ca.20040. [DOI] [PubMed] [Google Scholar]
- 28.Koles P, Nelson S, Stolfi A, Parmelee D, Destephen D. Active learning in a year 2 pathology curriculum. Med Educ. 2005;39:1045–55. doi: 10.1111/j.1365-2929.2005.02248.x. [DOI] [PubMed] [Google Scholar]
- 29.Hunt DP, Haidet P, Coverdale JH, Richards B. The effect of using team learning in an evidence-based medicine course for medical students. Teach Learn Med. 2003;15:131–9. doi: 10.1207/S15328015TLM1502_11. [DOI] [PubMed] [Google Scholar]
- 30.Levine RE, O’Boyle M, Haidet P, Lynn DJ, Stone MM, Wolf DV, et al. Transforming a clinical clerkship with team learning. Teach Learn Med. 2004;16:270–5. doi: 10.1207/s15328015tlm1603_9. [DOI] [PubMed] [Google Scholar]
- 31.Parmelee DX, DeStephen D, Borges NJ. Medical students attitudes about team-based learning in a pre-clinical curriculum. Med Educ Online. 2009;14:1–7. doi: 10.3885/meo.2009.Res00280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fleming N. I’m different; not dumb. Modes of presentation (VARK) in the tertiary classroom. In: Zelmar A, editor. Research and Development in Higher Education. Canterbury, New Zealand: Lincoln University; 1995. pp. 308–13. [Google Scholar]
- 33.Coffield F, Moseley D, Hall E, Ecclestone K. Learning styles and pedagogy in post-16-year old learning: A systematic and critical review. Learn Skills Res Centre. 2004:1–5. [Google Scholar]
- 34.Wehrwein E, Lujan H, DiCarlo S. Gender differences in learning preferences amongst undergraduate physiology students. Adv Physiol Educ. 2007;31:153–7. doi: 10.1152/advan.00060.2006. [DOI] [PubMed] [Google Scholar]