Abstract
Schizophrenia is a neurodevelopmental disorder whose clinical features include impairments in perception, cognition and motivation. These impairments reflect alterations in neuronal circuitry within and across multiple brain regions that are due, at least in part, to deficits in dendritic spines, the site of most excitatory synaptic connections. Dendritic spine alterations have been identified in multiple brain regions in schizophrenia, but are best characterized in layer 3 of the neocortex, where pyramidal cell spine density is lower. These spine deficits appear to arise during development, and thus are likely the result of disturbances in the molecular mechanisms that underlie spine formation, pruning, and/or maintenance. Each of these mechanisms may provide insight into novel therapeutic targets for preventing or repairing the alterations in neural circuitry that mediate the debilitating symptoms of schizophrenia.
Schizophrenia is a devastating and complex psychiatric disorder characterized by impairments in multiple domains, including perception, affect and cognition. This range of clinical features suggests that the pathophysiology of schizophrenia reflects altered connectivity within and between multiple brain regions. Many of these connections involve dendritic spines, small protrusions from dendritic shafts that are the synaptic targets of axon terminals. Dendritic spine number undergoes substantial changes during development, and abnormalities in these processes likely contribute to the pathology of a number of brain disorders, including schizophrenia. In this review, we consider 1) findings of dendritic spine abnormalities in schizophrenia, 2) evidence that these abnormalities reflect the disease process, 3) possible anatomical and molecular mechanisms underlying spine abnormalities in schizophrenia, 4) the potential role of altered developmental trajectories in these abnormalities, and 5) the implication of these findings for understanding the disease process of schizophrenia and for the development of novel therapeutic interventions.
Schizophrenia
Clinical Features
Schizophrenia affects approximately 0.5–1.0% of the world’s population, and the care and treatment of schizophrenia is associated with large economic, societal and family burdens (Wu et al., 2005; Awad and Voruganti, 2008). The clinical signs and symptoms of schizophrenia can be divided into three categories: positive, negative, and cognitive. Positive symptoms include hallucinations, delusions, and thought disorder. Negative symptoms include altered emotional expression (e.g., flat affect), inability to derive pleasure from activities that were previously enjoyable (i.e., anhedonia), poverty of speech (i.e., alogia), and inability to initiate and persist in goal-directed activities (i.e., avolition) (American Psychiatric Association, 1994). Cognitive symptoms include deficits in multiple domains such as executive functioning, attention, and working memory (Elvevag and Goldberg, 2000; Piskulic et al., 2007). The positive and negative diagnostic features generally appear in late adolescence or early adulthood (Lewis and Lieberman, 2000), while cognitive impairments are usually present years before the clinical diagnosis is made (Lesh et al., 2011).
The staple treatment for schizophrenia is antipsychotic drugs (APDs). Although these medications can suppress the positive symptoms experienced by patients (Kane, 1996; Lieberman and Stroup, 2011), they have little to no effect on negative and cognitive symptoms (Keefe et al., 2007; Harvey, 2007). Importantly, cognitive impairments are the best predictor of factors underlying recovery such as employment, social integration, and relapse (Green, 2006). Thus, while the discovery of antipsychotic drugs has improved the outcome and quality of life of many individuals diagnosed with schizophrenia, the limited efficacy of these drugs clearly indicates the need to identify new biological targets and therapeutics for schizophrenia patients (Insel and Scolnick, 2006).
Risk Factors
Schizophrenia is more commonly diagnosed in males (male:female ratio 1.4:1) (Aleman et al., 2003; McGrath et al., 2004); and males have more severe symptoms, including an earlier age of onset, poorer response to treatment, and worse outcomes (Grossman et al., 2008). People born in urban environments have twice the risk for developing schizophrenia as those born in rural environments (Marcelis et al., 1998; Mortensen et al., 1999; Pedersen and Mortensen, 2001), and some studies suggest an increased risk for those living in cities irrespective of their birthplace (McGrath et al., 2004; Saha et al., 2005). Migrant populations, especially those belonging to an ethnic minority in their new location, are at a significantly increased risk for schizophrenia (Fearon et al., 2006; Morgan et al., 2010). Finally, epidemiological data suggest a significantly increased risk for developing schizophrenia later in life in individuals who chronically use marijuana during early adolescence (Casadio et al., 2011).
Genetic factors also clearly contribute to the etiology of the illness as the relative risk of schizophrenia is 6 – 17 times greater among first degree relatives, and 40 – 50 times greater in the monozygotic twin of an affected individual than in the general population (Gottesman, 1991; Cardno et al., 1999). Both common allelic variants of small effect and rare copy number variants (i.e., large deletions or duplications of DNA) of apparently large effect have been associated with the illness, but identification of specific genetic causes remains an ongoing challenge (Kim et al., 2011).
Finally, schizophrenia has a clear developmental component; many symptoms appear or worsen during adolescence (Lewis and Lieberman, 2000), a time of great transition and refinements in brain structure and function (Casey et al., 2010; Chu-Shore et al., 2011). A proposed integrated conceptualization of schizophrenia as a disorder of neurodevelopment includes the interaction of genetic predisposition and environmental exposures, which lead to cascading effects of altered neurodevelopment, resulting in the behavioral syndrome (Lewis and Levitt, 2002).
Pathology
Structural imaging studies have shown smaller whole brain volumes in the prodromal stage, at the first episode of psychosis, and in chronically ill patients (Lawrie and Abukmeil, 1998; Steen et al., 2006; Levitt et al., 2010). For example, a recent eight year longitudinal magnetic resonance imaging (MRI) study demonstrated that people at high genetic risk for schizophrenia have greater reductions over time in whole brain, prefrontal cortex (PFC), and temporal lobe volumes than those with no genetic risk. Moreover, those who eventually converted to schizophrenia showed an even greater reduction in PFC volume (McIntosh et al., 2011). Smaller hippocampal volumes have also been identified at these early stages of the illness (Harrison, 2004; Tamminga et al., 2010), in agreement with the temporal lobe findings. Decreased volume in schizophrenia appears to be especially pronounced in cortical areas; in contrast, results from structural imaging studies of the basal ganglia (Bogerts et al., 1985; Brandt and Bonelli, 2008; Horga et al., 2011) and cerebellum (Supprian et al., 2000; Andersen and Pakkenberg, 2003; Kakeda and Korogi, 2010) have been mixed.
Reductions in grey matter may underlie the smaller cortical and hippocampal volumes in schizophrenia (Glahn et al., 2008). Although not conclusive, smaller grey matter volumes are frequently reported in individuals at high genetic risk (Cannon et al., 2002; Hulshoff Pol et al., 2004; Borgwardt et al., 2010; Mechelli et al., 2011), and in both first-episode and chronically ill subjects with schizophrenia relative to healthy comparison subjects (Honea et al., 2005; Takahashi et al., 2009; Levitt et al., 2010). Some longitudinal MRI studies have found that high risk subjects who convert to psychosis have larger deficits in grey matter volume than those who do not (Pantelis et al., 2003; Fornito et al., 2008; Sun et al., 2009); however, a recent large, multicenter study found that grey matter reductions in converters and non-converters were virtually indistinguishable (Mechelli et al., 2011). Finally, many studies indicate that deficits in grey matter may be progressive through the initial phases of the disease (Kasai et al., 2003b; Takahashi et al., 2009; Yoshida et al., 2009; Olabi et al., 2011).
Neuronal somal size is correlated with dendritic tree (Hayes and Lewis, 1996; Jacobs et al., 1997) and axonal arbor (Lund et al., 1975; Gilbert and Kelly, 1975) complexity, whose components (dendritic shafts, dendritic spines, axons, and axon terminals) contribute to the cortical neuropil. Studies using postmortem human tissue suggest that smaller pyramidal cell bodies and decreased neuropil, rather than neuron loss, may be the primary contributor to smaller cortical grey matter volumes in the dorsolateral prefrontal cortex (DLPFC) and auditory cortices in schizophrenia. On average, pyramidal cell somal volume is ~10% smaller in layer 3 of the DLPFC (Rajkowska et al., 1998; Glantz and Lewis, 2000; Pierri et al., 2001), and primary and association auditory cortices (Sweet et al., 2003; Sweet et al., 2004); and neuronal packing density is increased each of those regions in schizophrenia in some studies (Selemon et al., 1995; Selemon et al., 1998; Selemon et al., 2003; Dorph-Petersen et al., 2009). Together, these data suggest that schizophrenia is associated with diminished cortical neuropil (Selemon and Goldman-Rakic, 1999; Dorph-Petersen et al., 2009), and as summarized below, studies from multiple cortical areas indicate that lower dendritic spine density contributes to the reduced cortical neuropil in schizophrenia.
Spines are morphologically and biochemically discrete compartments that protrude from the dendritic shafts of cortical and hippocampal pyramidal cells, cortical spiny stellate cells, cerebellar Purkinje cells, and medium spiny neurons of the striatum (Gray, 1959; Harris and Kater, 1994). The vast majority (80 – 95%) of excitatory synapses in the central nervous system are formed onto dendritic spines (DeFelipe and Farinas, 1992; Wilson, 2007); and, as such, spines perform a significant role in regulating neuronal excitability. Each spine typically receives one glutamatergic synapse; thus spine density reflects the amount of excitatory drive a neuron receives (Yuste, 2011), though spines may also be innervated by other neurotransmitter and neuropeptide systems (Goldman-Rakic et al., 1989; Kung et al., 1998) (Figure 1). In experimental models, spine deficits are associated with impairments in working memory, attention, sensory-motor processing, and sociability (Liston et al., 2006; Cahill et al., 2009; Hains et al., 2009; Brennaman et al., 2011); such findings suggest that deficits in dendritic spines may contribute to the clinical features of schizophrenia. Indeed, the diverse symptomatology of schizophrenia suggests that a common alteration is present across many different brain regions and leads to impaired connectivity within and between regions; thus, alterations in dendritic spines could play a key role as a neural substrate for schizophrenia.
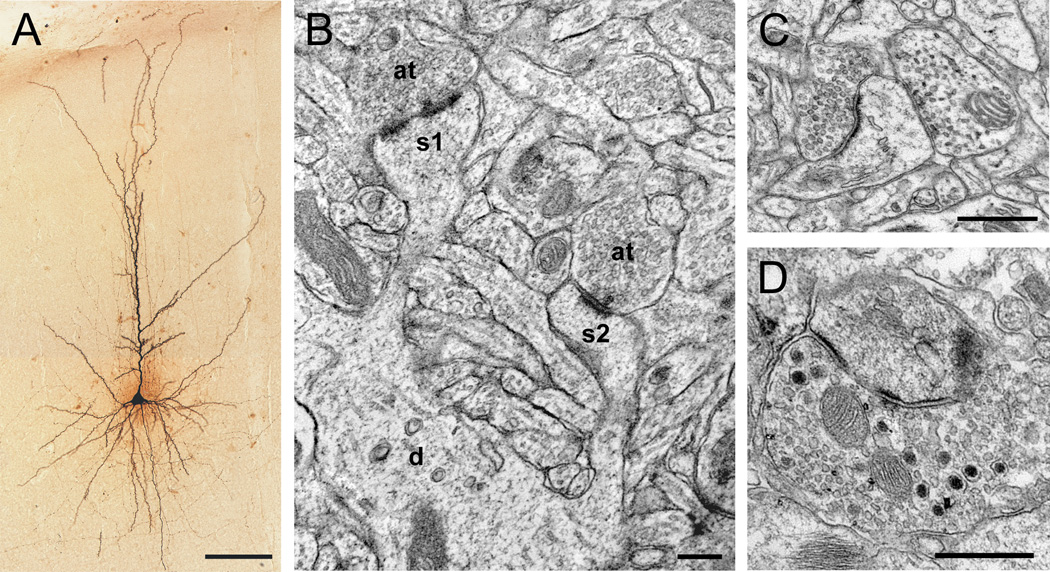
Figure 1.
Micrographs of pyramidal cell dendritic spines in the primate prefrontal cortex. A) Light micrograph of a biocytin-filled pyramidal cell showing the cell body, and basilar and apical dendritic shafts. B) Electron micrograph showing two spines (s1, s2) protruding from a dendritic shaft (d). Spine s1 is receiving a perforated asymmetric (presumably glutamatergic) synapse. C) Dendritic spine receiving an asymmetric (presumably glutamatergic) synapse and a symmetric (inhibitory or catecholaminergic) synapse. Note the difference in the appearance of the synaptic vesicles in each presynaptic axon terminal. D) Axon terminal containing small, round vesicles characteristic of glutamate, and large, dense-core vesicles characteristic of neuropeptides, forming an asymmetric synapse onto a spine. Scale bar is 100 µm in A, 200 nm in B, and 500 nm in C–D.
Spine Alterations in Schizophrenia
Neocortex
Direct quantification of neocortical dendritic spines in schizophrenia subjects has been performed in four studies using either Golgi impregnation of pyramidal cells or immunohistochemical labeling of spine markers (Table 1). All findings converge on the conclusions that spine density is lower in multiple neocortical areas in schizophrenia, and that these alterations might be most robust for pyramidal neurons located in layer 3, a major site for cortico-cortico and thalamo-cortical integration (Jones, 1984; Kritzer and Goldman-Rakic, 1995; Melchitzky et al., 1999). For example, layer 3 pyramidal cells receive both feed-forward and intrinsic excitatory cortical inputs, as well as excitatory inputs from the thalamus. Thus, lower spine density in layer 3 pyramidal cells may reflect, or contribute to, alterations in multiple types of excitatory connections in the cortex. The first Golgi study quantified spine density in pyramidal cells whose somata were located in layer 3 in various prefrontal and temporal cortical areas. In these multiple areas, spine density was significantly ~ 60% lower in the schizophrenia subjects (Garey et al., 1998).
Table 1.
Summary of reported dendritic spine alterations in schizophrenia
| Anatomical Regions |
Schizophrenia/Healthy Comparison Subjects |
Methods | Measures | Reported Significant Differences in Schizophrenia |
Reference |
|---|---|---|---|---|---|
| Frontal Cortex | 13/11 | Golgi | Spine density | 66% Decrease, Layer 3 | Garey et al 1998 |
| Temporal cortex | 13/11 | Golgi | Spine density | 59% Decrease, Layer 3 | Garey et al 1998 |
| BA46 | 15/15 | Golgi | Spine density | 23% Decrease, Layer deep 3 | Glantz and Lewis 2000 |
| BA46 | 15/15 | Golgi | Spine density | No difference, Layers 5–6 | Kolluri et al 2005 |
| BA17 | 15/15 | Golgi | Spine density | No difference, Layer 3 | Glantz and Lewis 2000 |
| BA41 | 15/15 | IHC | Spinophilin-IR puncta density | 27% Decrease, Layer deep 3 | Sweet et al 2009 |
| BA42 | 15/15 | IHC | Spinophilin-IR puncta density | 22% Decrease, Layer deep 3 | Sweet et al 2009 |
| Striatum | 6/6 | EM | Spine cross-sectional area | 30% Decrease | Roberts et al 1996 |
| Caudate | 17/10 | EM | Axospinous synapse density | 26% Increase | Roberts et al 2005b |
| Putamen | 17/10 | EM | Axospinous synapse density | No difference | Roberts et al 2005b |
| Caudate Patch & Matrix | 14/8 | EM | Axospinous synapse density | No difference | Roberts et al 2005a |
| Putamen Matrix | 14/8 | EM | Axospinous synapse density | No difference | Roberts et al 2005a |
| Putamen Patch | 14/8 | EM | Axospinous synapse density | 44% Increase | Roberts et al 2005a |
| Caudate Patch & Matrix | 16/10 | EM | Axospinous synapse density | No difference | Roberts et al 2008 |
| Putamen Matrix | 16/10 | EM | Axospinous synapse density | No difference | Roberts et al 2008 |
| Putamen Patch | 16/10 | EM | Axospinous synapse density | 44% Increase | Roberts et al 2008 |
| Subiculum | 13/8 | Golgi | Spine density | 35% Decrease, Apical dendrites | Rosoklija et al 2000 |
| CA3 | 9/10 | EM | Mossy fiber axospinous synapse density | No difference | Kolomeets et al 2005 |
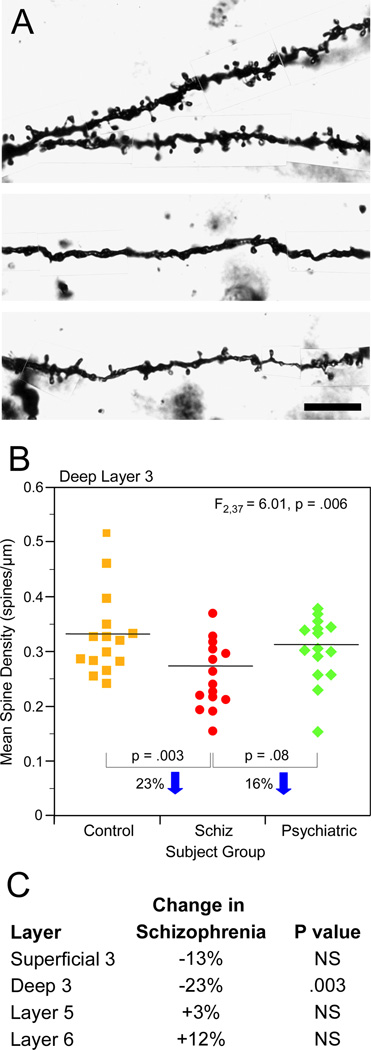
Subsequent work quantified spine density in triad cohorts of schizophrenia, healthy comparison, and psychiatric comparison subjects. Relative to both comparison subject groups, spine density in the subjects with schizophrenia was ~20% lower on the basilar dendrites of pyramidal neurons located in layer deep 3, but did not differ for pyramidal neurons in superficial layer 3, layer 5 or layer 6 of area 46, or in layer 3 of primary visual cortical area 17 (Glantz and Lewis, 2000; Kolluri et al., 2005) (Figure 2). Interestingly, within layer deep 3 of area 46, the total dendritic length (TDL) was also significantly lower in schizophrenia subjects, and analysis of spine density controlling for TDL increased the significance of the between group difference. Importantly, spine density in subjects in the psychiatric comparison group who had been treated with APD did not differ from healthy comparison subjects, suggesting that decreased DLPFC spine density in schizophrenia is not a consequence of APD treatment.
Figure 2.
Decreased layer 3 spine density in the dorsolateral prefrontal cortex (DLPFC) of schizophrenia subjects. A) Golgi-impregnated basilar dendrites and spines from a healthy comparison subject (top) and two schizophrenia subjects (bottom). Spine density is qualitatively decreased in the schizophrenia subjects relative to the healthy comparison subject. B) Scatter plot demonstrating lower layer deep 3 spine density in schizophrenia subjects relative to healthy comparison and psychiatrically ill subjects. C) Within the same subjects, lower DLPFC spine density is specific to layer deep 3. Scale bar is 10 µm in A. Adapted from Lewis and Gonzalez-Burgos (2008).
Finally, one study examined spine density in primary and association auditory cortices areas 41 and 42 by quantifying spinophilin-immunoreactive (SP-IR) puncta in matched pairs of schizophrenia and healthy comparison subjects (Sweet et al., 2009). The density of layer deep 3 SP-IR puncta was significantly 27% lower in area 41 and 22% lower in area 42 of schizophrenia subjects. Using the presence or absence of immunoreactivity to identify whether a neuronal structure is present or absent has some methodological limitations. For example, the spine may still be present, but no longer contains SP-immunoreactivity at detectable levels, resulting in an erroneous interpretation of decreased spine density. However, studies of cortical SP mRNA and protein expression have found either increased or unchanged levels in schizophrenia (Weickert et al., 2004; Baracskay et al., 2006), supporting the interpretation that lower SP-IR puncta density is reflective of decreased spine density, and not undetectable levels of SP-immunoreactivity per spine.
Non-cortical areas
Spine pathology has also been reported in the striatum and hippocampus of schizophrenia subjects (Table 1). In the striatum, spines on GABAergic medium spiny neurons (MSN) have been examined by electron microscopy in schizophrenia in several studies from the Roberts’ group. Overall, the studies indicate that axospinous synapse density may be increased in the dorsal striatum (Table 1). For example, a 3D reconstruction analysis of over 4,000 and 2,000 synapses in schizophrenia and healthy comparison subjects, respectively, found significantly higher densities of all types of synapses, including asymmetric axospinous, in the caudate of schizophrenia subjects. These findings were present in subjects receiving either typical or atypical APD, and they were especially pronounced in the two subjects off APD at the time of death, suggesting that medication effects were not driving the increase in synaptic density (Roberts et al., 2005b). To further examine which afferent sources may be contributing to increased axospinous synapse density, two subsequent studies quantified synaptic density in the patch and matrix compartments of the striatum (Roberts et al., 2005a; Roberts et al., 2008). A significant increase in total synaptic density in the putamen patch of subjects with schizophrenia was observed, and this difference was driven by a selective increase in the density of asymmetric axospinous synapses. Importantly, subjects on typical APD had normal levels of putamen patch axospinous synaptic density, those on atypical APDs had higher densities, and the two subjects not on APDs at the time of death had the highest density. Together, these results suggest that increased axospinous synaptic density in the putamen patch compartment may not be a consequence of APD treatment. Because patch compartments receive cortico-limbic inputs (Bolam et al., 2000), these findings may reflect increased glutamatergic inputs from corticolimbic regions onto MSNs in the putamen patch compartment in schizophrenia. Interestingly, putamen patch MSNs project to the substantia nigra pars compacta, where they inhibit dopaminergic neurons. Thus, enhanced excitation of inhibitory MSN may be a compensatory response to quell overactive nigral dopaminergic neurons in schizophrenia. However, whether increased axospinous synapse density, and presumably increased excitatory drive, reflects a cause of the illness, compensation to some other upstream pathology, or a consequence of treatment remains to be determined.
In the hippocampal formation, the major glutamatergic pathways consist of projections from the entorhinal cortex to the dentate gyrus via the perforant pathway, dentate gyrus to CA3 via the mossy fiber projections, CA3 to CA1 via the Schaffer collateral, and CA1 to the subiculum. Dendritic spine density in these pathways has only been reported in one study of schizophrenia. Apical spine density was significantly ~70% lower in schizophrenia subjects and significantly ~50% lower in mood disorder subjects relative to the healthy comparison group (Rosoklija et al., 2000). Importantly, because subjects in the mood disorder group, all of whom had all been treated with APD, also had significantly lower subicular spine density, an effect of APD treatment on spine density cannot be ruled out. Moreover, in contrast to many other postmortem studies of schizophrenia, all of the schizophrenia and mood disorder subjects were institutionalized in state hospitals for lengthy periods, and lack of environmental enrichment can decrease hippocampal spine density (Moser et al., 1994; Leuner and Gould, 2010).
Two studies using EM techniques have examined mossy fiber terminations (MFT) onto CA3 pyramidal cell spines in schizophrenia subjects. In the first study, subject groups did not differ in the volume fraction of spines, total number of invaginated spines, nor the number of spines receiving a synapse per MFT (Kolomeets et al., 2005). In a subsequent study, those authors found a significant 25% reduction in the mean number of synaptic contacts per MFT, though analysis was not restricted to axospinous synapses (Kolomeets et al., 2007). Whether these results differ from the previous study due to the inclusion of axodendritic synapses and/or the different characteristics of the subject cohorts is unclear. Thus, while imaging studies of the hippocampus have convincing data regarding smaller volume and altered activity during some memory tasks (Steen et al., 2006; Tamminga et al., 2010), studies on morphological changes of dendritic spines are mixed and preliminary.
Methodological & Medication Considerations
In interpreting the results of the studies that used Golgi impregnation methods to quantify spine density or dendritic length, it is important to keep in mind several potential limitations of this technique. First, only a small proportion of neurons are labeled using Golgi staining, and the number labeled can vary considerably across samples (Pasternak and Woolsey, 1975). However, the process by which cells are labeled is stochastic, and as such, labeled neurons are likely representative of the population. Second, because the reaction product of Golgi impregnation is opaque, labeled spines could be obscured behind dendritic shafts and not counted. Thus, differences in dendrite diameter between diagnostic groups could contribute to the findings (Horner and Arbuthnott, 1991), and this issue should be considered when interpreting Golgi studies which do not report dendritic diameter [ (Garey et al., 1998; Rosoklija et al., 2000; Kolluri et al., 2005)]. However, Glantz and Lewis (2000) reported no difference in mean dendrite diameter across schizophrenia and comparison subjects, suggesting that lower spine density in schizophrenia is not a consequence of hidden spines. Finally, although Golgi-labeled neurons that are fully impregnated can be identified following postmortem intervals (PMI) of up to 24 hours, longer PMIs can contribute to incomplete Golgi impregnation; indeed, even at 12 hour PMIs, spine density appears to be reduced, with superficial cortical layers reported to be preferentially affected (Williams et al., 1978; Buell, 1982). The longer PMIs in the schizophrenia relative to comparison subjects in the Garey et al (1998) and Rosoklija (2000) studies may have contributed to the larger between subject group differences in spine density identified in these two studies relative to those found in the shorter PMI study of Glantz and Lewis (2000).
Golgi studies of cortical spine density all demonstrate decreased number of spines per µm of dendrite in schizophrenia subjects relative to healthy comparison subjects, and this density measure is likely reflective of a decrease in the total number of spines. Total spine number can be altered by changes in the number of spines per dendritic length, and/or decreased dendritic length. By measuring the number of spines/µm, these studies confirm that spine deficits are not only due to shorter dendrites in schizophrenia. However, the decrease in schizophrenia may be reflective of both of these processes, given other reports of decreased dendritic complexity in the subiculum (Rosoklija et al., 2000) and PFC (Kalus et al., 2000; Broadbelt et al., 2002). Indeed, lower TDL was identified in the DLPFC (Glantz and Lewis, 2000) of schizophrenia subjects along with decreased spine density. Sweet et al (2009) found lower spine density in schizophrenia auditory cortex using the number of SP-IR puncta/µm3 of tissue. Given that structural imaging studies consistently report smaller gray matter volumes in schizophrenia, these density measures may actually underestimate the reduction in cortical dendritic spine number in schizophrenia.
Dendritic spines are dynamic structures, whose morphology and density can change in response to many factors, including circulating hormone levels, changes in environmental enrichment, drug use, learning, and synaptic activity (Yuste and Bonhoeffer, 2001; Fiala et al., 2002), and thus the potential impact of such factors on the findings of decreased spine density in schizophrenia must be kept in mind. Two studies which found lower spine density in schizophrenia statistically examined the effects of comorbid substance abuse diagnosis and duration of illness, and found no effect of these factors on spine density (Glantz and Lewis, 2000; Sweet et al., 2009). In addition, psychiatric comparison subjects, which may have similar hospitalization experiences as schizophrenia subjects, did not have altered cortical spine density (Glantz and Lewis, 2000; Kolluri et al., 2005). Moreover, experimental data demonstrate that the vast majority of spines in mouse cortex persist for over 13 months (Grutzendler et al., 2002), that persistent spines are more prevalent in adult animals (Holtmaat et al., 2005), and that dendritic spine density is relatively stable in adult monkey and human DLPFC (Anderson et al., 1995; Petanjek et al., 2011).
The possible effect of APD on spine measures is of potential concern in all the postmortem studies described above. In addition to statistically accounting for APD usage, animal studies have provided information about the effects of chronic APD treatment on spine measures. In rats chronically treated with haloperidol for six months, mean striatal spine density was decreased (Roberts et al., 1995; Kelley et al., 1997), whereas many of the striatal postmortem findings suggest increased striatal spine density in schizophrenia. Sweet et al (2009) included a control experiment comparing SP-IR puncta density across two groups of sex-, age- and weight-matched monkeys: one group was chronically administered haloperidol for 9 – 12 months at doses that produced serum levels comparable to those associated with therapeutic efficacy in humans, and the other group received vehicle. Quantification of SP-IR puncta density revealed no difference between the two groups. Finally, rats treated with clinically-relevant doses of haloperidol or olanzapine showed no changes in PFC pyramidal cell spine density (Wang and Deutch, 2008), and rats chronically treated with haloperidol for one year also did not show a change in cortical spine density (Vincent et al., 1991). Thus, while not conclusive, the available data suggest that the striatal and cortical spine findings are likely not an artifact of APD treatment.
Potential mechanisms underlying spine deficits in schizophrenia
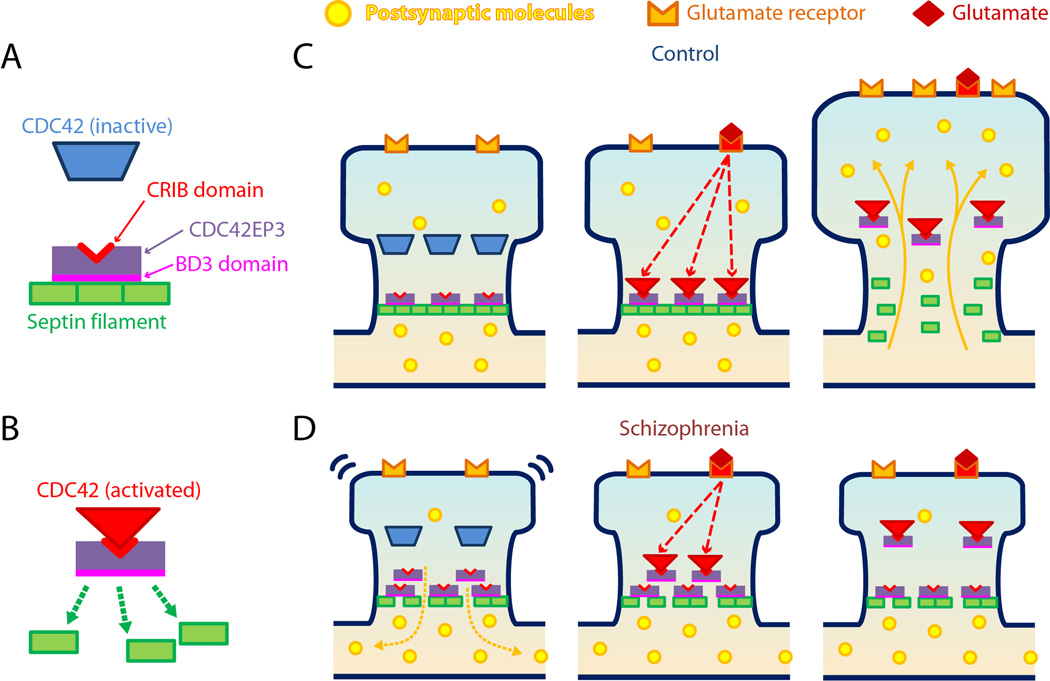
Markers of molecular mechanisms important for dendritic spine formation and maintenance are altered in schizophrenia. Stabilization of the actin cytoskeleton is essential for spine shape and density (Calabrese et al., 2006; Tada and Sheng, 2006; Bourne and Harris, 2008), and transcript and protein levels of molecules important for spine cytoskeletal stabilization are altered in multiple cortical areas in schizophrenia. Rho GTPases, small proteins that bind to GDP and GTP, are important for intracellular signaling and actin remodeling (Negishi and Katoh, 2005; Calabrese et al., 2006). Activity of the Rho GTPases Cdc42 (cell division cycle 42) and Rac1 (Ras-related C3 botulinum toxin substrate 1) increases spine formation in culture and in vivo (Nakayama et al., 2000; Irie and Yamaguchi, 2002; Scott et al., 2003; Kreis et al., 2007; Cerri et al., 2011; Bongmba et al., 2011). In schizophrenia, Cdc42 mRNA levels are lower, and the decrease is strongly correlated with DLPFC layer 3 spine deficits (Hill et al., 2006). Cdc42 has numerous effector proteins, and mRNA for Cdc42 effector protein 3 (Cdc42EP3), which is preferentially expressed in layer 3 of human DLPFC (Arion et al., 2007), is upregulated in schizophrenia (Ide and Lewis, 2010). Interestingly, current evidence suggests that activation of Cdc42 by glutamate stimulation inhibits Cdc42EP3 activity which in turn dissociates the complex of septin filaments in spine necks, enabling the movement from the parent dendrite of molecules (e.g., cytoskeletal proteins, second messengers, etc) required for synaptic potentiation (Ide and Lewis, 2010). The combination of lower levels of CDC42 and higher levels of Cdc42EP3 might lead to a reduced capacity for glutamatergic stimuli to open the septin filament barrier in the spine neck, impairing synaptic plasticity and contributing to spine loss (Figure 3).
Figure 3.
Schematic diagram of Cdc42-Cdc42EP3-septin interactions and their proposed roles in spine dysfunction in schizophrenia. A) Cdc42EP3 binds to septins via a BD3 domain, inducing the assembly of septin filaments. Inactive Cdc42 cannot bind to Cdc42EP3. B) Once activated, Cdc42 can bind to and inhibit Cdc42EP3 via its CRIB domain, disrupting septin filament formation. C) In the normal state, Cdc42EP3 consolidates septin filaments in the spine neck, effectively forming a barrier for molecular diffusion with the parent dendrite (left). Transient activation of Cdc42 by glutamate stimulation inhibits the Cdc42EP3-mediated assembly of the septin filament barrier (middle), enabling molecular diffusion with the parent dendrite (right). C) In schizophrenia, decreased expression of septin 7 mRNA contributes to impaired septin filament formation at the spine neck, limiting the retention of postsynaptic molecules that are critical for spine structure and function in the spine head (left). Furthermore, lower levels of Cdc42 and increased levels of Cdc42EP3 lead to a reduced capacity for glutamatergic signaling to open the septin barrier (middle), limiting synaptic plasticity and possibly contributing to spine loss (right). Cell division cycle 42 (Cdc42), Cdc42 effector protein 3(Cdc42EP3). Adapted from Ide and Lewis 2010.
Promotion of RhoGTPase interaction with effector proteins is mediated via guanine exchange factors (GEFs), including Kalirin, a Rac1 GEF that is concentrated in spine heads (Penzes et al., 2001) and regulates cortical spine density (Cahill et al., 2009). In schizophrenia, Kalirin mRNA expression (using a probe that identifies Kalirin-5 and Kalirin-7) is lower in DLPFC layer 3, and this decrease is correlated with DLPFC layer 3 spine deficits in the same subjects (Hill et al., 2006). Interestingly, a recent study demonstrated no change in the protein levels of Kalirin-5, -7, and -12 and a significant 11% increase in Kalirin-9 expression in total auditory cortex grey matter (Deo et al., 2011b). Kalirin-9 overexpression in mature cultured cortical neurons decreases dendritic length, without changing spine number (Deo et al., 2011a). Importantly, the KALRN locus has been associated with risk for schizophrenia (Ikeda et al., 2011); missense mutations in KALRN are reported in individuals with schizophrenia (Kushima et al., 2010); and the KALRN protein product interacts with those of other putative schizophrenia risk genes (e.g., DISC1, NRG, ERBB4) in regulating dendritic morphology and spine plasticity (Hayashi-Takagi et al., 2010; Cahill et al., 2012). While additional studies examining Kalirin mRNA and protein expression in a laminar-specific manner in DLPFC and auditory cortex are needed, these results suggest that alterations in Kalirin promotion of Rho GTPase activity, and subsequent spine formation and stabilization (Cahill et al., 2009; Xie et al., 2010), may contribute to the neocortical spine deficits in schizophrenia subjects.
Decreased presynaptic activity and/or fewer afferent inputs is another potential factor that could contribute to decreased cortical spine density in schizophrenia (Fiala et al., 2002). In mature neural systems, pharmacological blockade of AMPA receptors or surgical deafferentation of glutamatergic inputs results in decreased spine density (Hamori, 1973; Matthews et al., 1976; Cheng et al., 1997; McKinney et al., 1999; Smart and Halpain, 2000; Jacobs et al., 2003; Sa et al., 2010), and two recent studies showed that a constitutive reduction in NMDA receptor activity results in decreased spine density and cortical volume in PFC and sensory cortex (DeVito et al., 2011; Balu et al., 2011). Though the results of studies examining presynaptic transcript and protein levels in total cortical grey matter have been mixed (Bauer et al., 2008; Corradini et al., 2009; Fung et al., 2011), results from microscopy studies quantifying presynaptic protein levels suggest that cortical axon terminal density is likely to be decreased in schizophrenia. For example, synaptophysin immunoreactivity is decreased in all cortical layers of the DLPFC (Glantz and Lewis, 1997), and the density of synaptophysin-IR puncta is also decreased in auditory cortex (Sweet et al., 2007). Importantly, DLPFC spines receive glutamatergic inputs from local and long-range pyramidal cell projections, as well as projections from the mediodorsal (MD) nucleus of the thalamus (Melchitzky et al., 1999; Melchitzky et al., 2001; Negyessy and Goldman-Rakic, 2005). Determining whether spines postsynaptic to a specific afferent source are affected in schizophrenia will help to illuminate potential mechanisms for spine deficits in schizophrenia. Initial evidence suggested that the DLPFC received fewer inputs from the MD thalamus (Pakkenberg, 1990; Young et al., 2000; Popken et al., 2000; Byne et al., 2002), and since these axons preferentially innervate DLPFC deep layers 3 and 4, fewer inputs from the MD thalamus might explain the tendency for the deficit in spine density to be most marked on the basilar dendrites of deep layer 3 pyramidal cells. However, subsequent studies using unbiased stereological methods and larger samples of subjects failed to find evidence of fewer neurons in the MD thalamus in schizophrenia (Cullen et al., 2003; Dorph-Petersen et al., 2004; Young et al., 2004; Kreczmanski et al., 2007). Furthermore, thalamocortical inputs represent a small proportion of all glutamatergic synapses in the cortex (Ahmed et al., 1994; Peters, 2002), so even a complete loss of thalamic inputs would likely not result in the observed decrease in spine density. Thus, decreased density of spines is more likely to reflect a deficit in cortico-cortico projections.
DLPFC spines also receive inputs from dopaminergic axons projecting from the ventral tegmental area (VTA) (Goldman-Rakic et al., 1989). VTA lesions in adult rats result in decreased PFC pyramidal cell basilar spine density, with no change in motor cortex spine density, and this decrease may be mediated by both D1 and D2 dopamine receptors (Wang et al., 2009a). Interestingly, prefrontal dopaminergic signaling is also important for WM ability (Goldman-Rakic et al., 2000), and is thought to play a role in cognitive dysfunction in schizophrenia (Goldman-Rakic, 1994). For example, DLPFC dopamine D1-family receptors are more abundant in schizophrenia subjects (Abi-Dargham et al., 2002; Abi-Dargham et al., 2011), and this increase is thought to reflect a compensatory upregulation due to decreased DLPFC dopaminergic innervation. However, a postmortem examination of dopaminergic inputs to the DLPFC only found a deficit in layer 6, where spine density is reportedly unchanged (Akil et al., 1999). Further examination of dopaminergic afferents to the DLPFC in human postmortem tissue will be important to determine whether diminished dopamine signaling could contribute to altered spine density in schizophrenia.
Another potential mechanism underlying decreased spine density and presynaptic inputs in schizophrenia is impaired mitochondrial functioning or trafficking within neurons. Because the brain relies fully upon glycolysis and mitochondrial respiration for adenosine triphosphate generation, deficits in mitochondrial function would be expected to strongly affect neuronal systems. Indeed, maintenance of dendritic and axonal arborization requires targeted, sufficient energy production from mitochondria (Mattson et al., 2008; Cheng et al., 2010). For example, impairing mitochondrial transport to dendrites by inhibiting mitochondrial fission decreases neuronal spine density (Li et al., 2004; Ishihara et al., 2009; Wang et al., 2009b), as does altering the mitochondrial membrane potential and cytochrome c release (Tsai et al., 2009). Multiple sources of information point to mitochondrial dysfunction in schizophrenia (Clay et al., 2011), including altered lactate levels in cerebrospinal fluid (Regenold et al., 2009), genetic linkage studies (Washizuka et al., 2006), altered levels of transcripts and proteins crucial to mitochondrial functioning (Martins-de-Souza et al., 2011; Gigante et al., 2011; Rosenfeld et al., 2011; Regenold et al., 2012), and altered brain metabolics (Khaitovich et al., 2008; Shao et al., 2008). However, mitochondria dysfunction has also been implicated in other psychiatric illnesses, such as bipolar disorder (Clay et al., 2011), which have not as yet been shown to have lower spine density.
Other molecular mechanisms that could contribute to decreased spine density in schizophrenia are being investigated (Lin and Koleske, 2010; Penzes et al., 2011; Bennett, 2011). For example, a candidate susceptibility gene for schizophrenia, disrupted in schizophrenia 1 (DISC1) (Chubb et al., 2008), is involved with mitochondrial trafficking (Atkin et al., 2011), and regulates spine formation via Kalirin-7 and Rac1 (Hayashi-Takagi et al., 2010). Neuregulin-1 and ErbB4 are also candidate susceptibility genes for schizophrenia (Walsh et al., 2008; Mei and Xiong, 2008), and their activity is associated with changes in spine density (Penzes et al., 2011). Finally, astroglia can enhance spinogenesis, and deficits in markers of glial functioning are identified in schizophrenia (Allen and Barres, 2005; Bernstein et al., 2009). Thus, multiple molecular or anatomical mechanisms, many of which interact with each other, may contribute to decreased cortical spine density in schizophrenia. Understanding which of these mechanisms are most relevant for schizophrenia may be informed by knowledge of when during development the spine deficits in individuals with schizophrenia arise.
Developmental trajectory of cortical spine density
The density of cortical dendritic spines goes through a protracted developmental trajectory defined by excessive production early in life, followed by pruning and elimination, and finally stabilization (Huttenlocher, 1979; Bourgeois et al., 1994; Huttenlocher and Dabholkar, 1997; Zhang and Benson, 2000). For example, pyramidal cell spine density in human DLPFC increases rapidly after birth and peaks in childhood, at which point spine density begins to decline until stabilizing in the third decade of life (Petanjek et al., 2011). Spine morphology also changes across development, transitioning from filopodia-shaped thin spines early in development to larger spines with a defined head and neck (commonly referred to as mushroom spines) (Garcia-Lopez et al., 2010), one hallmark of a stable axospinous synapse. Cortical axospinous synapses which survive pruning are generally less dynamic than those present earlier in development, becoming relatively stable in both shape and density (Lin and Koleske, 2010). Thus, spine density and morphology reflect neuronal development, as well as plasticity and connectivity within a given region.
The developmental time point at which spine density deficits arise in schizophrenia is unclear. Experimental evidence suggests that adult spine density can be affected by manipulations that begin in utero (Mukai et al., 2008; DeVito et al., 2011), childhood or adolescence (Silva-Gomez et al., 2003; Rubino et al., 2009), and even adulthood (Wang and Deutch, 2008; Liston and Gan, 2011). However, the developmental trajectory of schizophrenia symptoms suggests that spine deficits may arise from impaired spinogenesis during early childhood and/or enhanced pruning during adolescence. For example, deficits in general knowledge, language skills, and verbal and visual reasoning are already emerging by age seven in individuals who later develop schizophrenia (Reichenberg et al., 2010). Furthermore, these individuals subsequently manifest deficits in processing speed and working memory by early adolescence. This longitudinal study indicates that cortical dysfunction is already present early in childhood in individuals who will later receive a schizophrenia diagnosis, perhaps reflecting abnormal spinogenesis, and that dysfunction of the affected cortical circuits might be exacerbated during adolescence when spines are pruned.
Further insight could come from longitudinal MRI studies of grey matter volume in individuals at genetic risk for schizophrenia, as cortical grey matter volume and spine density follow similar developmental trajectories (Bennett, 2011). MRI studies of 22q11 deletion syndrome (22q11 DS), a strong risk factor for developing schizophrenia (Drew et al., 2011), have been performed in children. While adults with 22q11 DS show smaller frontal lobe volumes (Tan et al., 2009), results from children have been mixed, showing increases or no difference (Eliez et al., 2000; Kates et al., 2001; Simon et al., 2005; Baker et al., 2011; Kates et al., 2011). Thus, studies from this patient population suggest spinogenesis may be unaffected in schizophrenia, though 22q11 DS-associated schizophrenia may not be generalizable to all forms of the illness. However, a recent MRI study found no difference in grey matter volume between infants of mothers with schizophrenia and those born to healthy comparison mothers (Gilmore et al., 2010). Thus, the available structural data suggests that spinogenesis may not be grossly impaired in individuals at high risk for developing schizophrenia. However, because the majority of these high risk individuals will not eventually develop schizophrenia, additional longitudinal structural MRI studies comparing converters and non-converters will help to clarify whether spinogenesis is impaired in schizophrenia.
Because cortical dendritic spine density decreases substantially throughout adolescence, enhanced spine pruning may contribute to decreased cortical spine density in schizophrenia. Feinberg first proposed abnormal synaptic pruning as a potential cause for schizophrenia (Feinberg, 1982), and seven years later Hoffman and Dobscha posited that over-pruning of PFC spines leads to schizophrenia (Hoffman and Dobscha, 1989). Excessive spine pruning is now considered a potential factor underlying reduced cortical grey matter volume in schizophrenia. This hypothesis is supported by 1) MRI studies showing that high-risk subjects who convert to schizophrenia may have greater reductions in grey matter volumes of the PFC and other cortical regions than non-converters (Pantelis et al., 2003; Borgwardt et al., 2007; Sun et al., 2009; McIntosh et al., 2011; Mechelli et al., 2011), and that grey matter loss may be progressive through the initial phases of the illness (Kasai et al., 2003b; Salisbury et al., 2007; Takahashi et al., 2009; Yoshida et al., 2009); 2) magnetic resonance spectroscopy studies suggesting an increased breakdown of plasma membrane phospholipids in the early stages of the illness (Keshavan et al., 2004); and 3) the observation that the emergence of schizophrenia symptoms generally occur during the period of spine pruning.
Over-elimination of cortical spines in schizophrenia may be due to pathologically enhanced pruning mechanisms, or an over-abundance of immature axospinous synapses that are normally pruned. The molecular mechanisms underlying pruning are not fully understood, though synaptic activity plays an important role (Trachtenberg et al., 2002; Lin and Koleske, 2010), and as such, many of the molecules and processes implicated in pruning are also implicated in spinogenesis and spine maintenance (Segal, 2005). Thus, alterations in one process are likely to affect the others, and decreased spine density in schizophrenia may represent a global problem in the formation, maturation, and maintenance of axospinous synapses, rather than a specific impairment in the generation, elimination or stabilization of spines.
Future Directions
The findings summarized above indicate that schizophrenia is associated with lower spine density that is best documented in the cerebral cortex, that this deficit may be most marked in layer 3, that a number of potential molecular mechanisms underlying this deficit exist, and that this deficit may reflect disturbances in the normal developmental trajectory of cortical spine number. Understanding the role of lower cortical spine density in the disease process of schizophrenia, and its treatment, requires answers to a number of important questions about 1) the circuits mediated by the affected spines, 2) the developmental timing of the deficit in the affected spines, and 3) the functional role of the affected spines.
The existing findings support the idea that dendritic spine density deficits in schizophrenia are layer specific, raising the possibility that certain cortical afferent circuits are affected. Layer 3 pyramidal cells receive afferents from four major sources: 1) local axon collaterals from neighboring pyramidal cells, 2) long-distance axon collaterals that travel through the grey matter from pyramidal cells in the same cortical region, 3) association and colossal projections from pyramidal neurons in other cortical regions, and 4) projections from the thalamus. Given that layer 3 pyramidal neurons are smaller in both the DLPFC and other regions that project to the DLPFC (Rajkowska et al., 1998; Glantz and Lewis, 2000; Pierri et al., 2001; Sweet et al., 2003; Sweet et al., 2004), any or all of the three cortical sources of inputs to layer 3 pyramidal cells could be affected. As discussed above, the number of neurons from the mediodorsal thalamus does not appear to be altered in schizophrenia, although fewer neurons have been reported in the pulvinar nucleus which also projects to the DLPFC (Dorph-Petersen and Lewis, 2011).
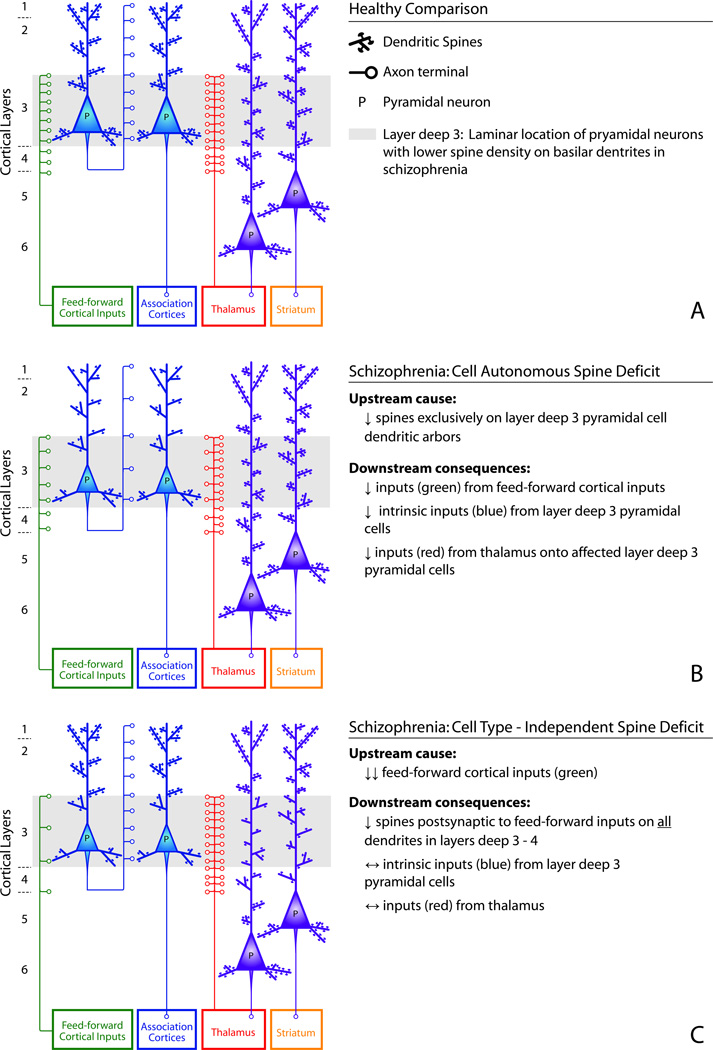
The distribution of spine deficits across the dendritic tree of the affected neurons could provide insight into both the affected afferents and whether the spine deficits are cell autonomous or independent of cell type. For example, lower spine density in all portions of the dendritic tree of a given class of cortical pyramidal neuron would suggest that the spine deficit is cell autonomous (Fig 4B), and thus possibly due to a cell type-specific, intrinsic deficit in the molecular machinery required for spine production/maintenance. A cell autonomous spine deficit restricted to deep layer 3 pyramidal cells would be predicted to result in the loss of targets for certain types of afferents, and thus would have the following downstream consequences for the affected pyramidal cells: fewer inputs from feed-forward cortical projections, fewer inputs from the intrinsic axon collaterals of layer 3 pyramidal cells, and fewer inputs from thalamic projections. In contrast, the connections furnished by these sources onto the dendritic spines of unaffected pyramidal cells, such as those with cell bodies are located in layers 5 and 6, would not be reduced (Fig 4B). Alternatively, a cell type-independent spine deficit in deep layer 3 would be associated with a different pattern of altered connectivity (Fig 4C). For example, an upstream deficit in feed-forward cortical projections would lead to a loss of spines on all dendrites in layers deep 3 and 4, but no change in the number of inputs from the intrinsic axon collaterals of layer 3 pyramidal cells or from thalamocortical projections (Fig 4C). Importantly, these two models provide testable hypotheses as to the upstream cause of spine deficits in schizophrenia.
Figure 4.
Two alternative models of potential cause and consequences of layer deep 3 spine deficits in schizophrenia.
Knowing when during the course of the illness cortical spine deficits arise in schizophrenia may have substantial implications for therapeutic interventions designed to restore or maintain normal spine density and plasticity. For example, if spine deficits arise in adolescence during the prodromal phase of the illness, when spine pruning predominates, then interventions that forestall or blunt this decline may be effective in delaying or preventing the cognitive symptoms of the illness. On the other hand, if spine deficits arise during birth or early childhood, when spinogenesis predominates, then early identification of individuals at high genetic risk and regular assessments of proxy markers of dendritic spine density (e.g., cortical grey matter thickness) becomes critical. A high genetic risk person with decreased cortical grey matter in early childhood may be a prime candidate for an intervention that bolsters spinogenesis. For example, the adrenergic α2 agonist guanfacine increases spine density in cultured cortical neurons (Hu et al., 2008; Ren et al., 2011), and local infusion of guanacine into the DLPFC of awake, behaving monkeys restores delay period pyramidal cell firing in aged monkeys (Wang et al., 2011). In addition, systemic administration of guanfacine improves working memory performance in young and aged monkeys (Arnsten et al., 1988; Rama et al., 1996; Franowicz and Arnsten, 1998; O'Neill et al., 2000). However, a double-bind, placebo-controlled clinical trial in chronically-ill schizophrenia subjects found no effect of adjunctive guanfacine treatment on performance in multiple cognitive domains (Friedman et al., 2001). Although discouraging, the results of this negative trial may highlight the importance of timing in the delivery of therapeutic interventions for schizophrenia, as early interventions to enhance spine number and function may be much more likely to be successful than when the deficit in circuitry function has been present for years.
Because spines have distinct morphologies that reflect different types of synaptic plasticity (Kasai et al., 2010), a preferential loss of one morphological class in schizophrenia would indicate which type of synaptic plasticity is altered. For example, small, thin spines have been described as “learning” spines (Kasai et al., 2003a), as they are transient and critical for rapid plasticity (Arnsten et al., 2010a). In contrast, large, mushroom spines are have been described as “memory” spines (Kasai et al., 2003a), as they are stable and engage in long-term synaptic plasticity (Bourne and Harris, 2007). Recently, thin spines have been proposed to be critical for “dynamic network connectivity,” an ongoing, rapid process by which PFC connections are strengthened or eliminated, providing the mental flexibility characteristic of the PFC (Arnsten et al., 2010b). Indeed, PFC thin spine density is positively correlated with working memory ability in monkeys (Dumitriu et al., 2010). These findings suggest the testable hypothesis that the impairments in working memory function that are common in schizophrenia reflect a preferential deficit in thin spines in the PFC.
If a lower density of thin spines in the PFC contributes to impaired cognitive ability in individuals with schizophrenia, then it may be possible to reverse this deficit through pharmacological means. For example, estrogen treatment increases thin spine density in the DLPFC of both younger and aged ovariectomized monkeys (Tang et al., 2004; Hao et al., 2006; Hao et al., 2007). Importantly, aged ovariectomized monkeys who received estrogen treatment did not display the normal age-related decline in DLPFC-dependent cognition (Rapp et al., 2003). Indeed, the findings that age of onset of diagnosis of schizophrenia is later in women (Riecher-Rossler and Kulkarni, 2011), and that women have a second period of increased rate of diagnosis after age 40 (Riecher-Rossler et al., 1997), have lead to the suggestion that estrogen has a protective effect in this illness. Interestingly, clinical trials of estrogen receptor modulators in postmenopausal women have shown improvements in schizophrenia symptoms (Kulkarni et al., 2010; Usall et al., 2011). Thus, these findings are consistent with the hypothesis that schizophrenia is associated with a deficit in thin spines and suggest that cyclical estrogen treatment might be a viable therapeutic intervention for the prevention of thin spine loss, and cognitive impairments, in schizophrenia.
Finally, identification of effective therapeutics also depends upon determining whether decreased dendritic spine density is a cause or consequence of the disease process of schizophrenia. Because spine density is not associated with the duration of psychotic illness, use of APDs, or presence of a psychiatric illness, spine deficits are not likely to be simply a consequence of the disease. On the other hand, excessive pruning of spines during late childhood/ adolescence could account for both the greater than normal decline in cortical grey matter during this time (Rapoport et al., 1999; Sporn et al., 2003) and the observation that cognitive impairments progress during this timeframe in individuals later diagnosed with schizophrenia (Reichenberg et al., 2010; Seidman et al., 2010). Moreover, spine deficits and associated reductions in network activity could drive the multiple changes identified in DLPFC GABA neurons in schizophrenia subjects (Lewis et al., 2012) that are thought to underlie the impaired cortical network oscillations and cognitive performance of the illness (Cho et al., 2006; Uhlhaas et al., 2008). Thus, while not conclusive, the existing evidence supports the idea that dendritic spine deficits are likely to represent the neural substrate for cognitive impairments in schizophrenia, and not to be a secondary consequence of the illness.
In summary, we have reviewed the evidence indicating that dendritic spine alterations are present in multiple brain regions in subjects with schizophrenia, but are best characterized in layer 3 of the neocortex, where pyramidal cell spine density is lower. These spine deficits appear to arise during development and thus are likely the result of disturbances in the molecular mechanisms that underlie spine formation, pruning, and/or maintenance. The conduct of definitive experiments that can reveal exactly where, how and when cortical spine deficits arise, and which schizophrenia symptoms can be attributed to these deficits, will provide a major step forward in the identification of novel therapeutic strategies for the prevention and treatment of schizophrenia.
Highlights.
Impaired perception, cognition and motivation are clinical features of schizophrenia
These symptoms reflect neural circuitry abnormalities, including spine deficits
Spine density is best characterized and lower in layer 3 of the neocortex
Altered spinogenesis or pruning during development likely underlies spine deficits
These processes represent possible novel therapeutic targets for schizophrenia
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- Abi-Dargham A, Mawlawi O, Lombardo I, Gill R, Martinez D, Huang Y, Hwang DR, Keilp J, Kochan L, van Heertum R, Gorman JM, Laruelle M. Prefrontal dopamine D1 receptors and working memory in schizophrenia. J Neurosci. 2002;22:3708–3719. doi: 10.1523/JNEUROSCI.22-09-03708.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abi-Dargham A, Xu X, Thompson JL, Gil R, Kegeles LS, Urban NB, Narendran R, Hwang DR, Laruelle M, Slifstein M. Increased prefrontal cortical D1 receptors in drug naive patients with schizophrenia: a PET study with [11C]NNC112. J Psychopharmacol. 2011 doi: 10.1177/0269881111409265. [epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Ahmed B, Anderson JC, Douglas RJ, Martin KAC, Nelson JC. Polyneuronal innervation of spiny stellate neurons in cat visual cortex. J Comp Neurol. 1994;341:39–49. doi: 10.1002/cne.903410105. [DOI] [PubMed] [Google Scholar]
- Akil M, Pierri JN, Whitehead RE, Edgar CL, Mohila C, Sampson AR, Lewis DA. Lamina-specific alterations in the dopamine innervation of the prefrontal cortex in schizophrenic subjects. Am J Psychiatry. 1999;156:1580–1589. doi: 10.1176/ajp.156.10.1580. [DOI] [PubMed] [Google Scholar]
- Aleman A, Kahn RS, Selten JP. Sex differences in the risk of schizophrenia: evidence from meta-analysis. Arch Gen Psychiatry. 2003;60:565–571. doi: 10.1001/archpsyc.60.6.565. [DOI] [PubMed] [Google Scholar]
- Allen NJ, Barres BA. Signaling between glia and neurons: focus on synaptic plasticity. Curr Opin Neurobiol. 2005;15:542–548. doi: 10.1016/j.conb.2005.08.006. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. DSM-IV. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, D.C.: American Psychiatric Association; 1994. [Google Scholar]
- Andersen BB, Pakkenberg B. Stereological quantitation in cerebella from people with schizophrenia. Br J Psychiatry. 2003;182:354–361. doi: 10.1192/bjp.182.4.354. [DOI] [PubMed] [Google Scholar]
- Anderson SA, Classey JD, Condé F, Lund JS, Lewis DA. Synchronous development of pyramidal neuron dendritic spines and parvalbumin-immunoreactive chandelier neuron axon terminals in layer III of monkey prefrontal cortex. Neuroscience. 1995;67:7–22. doi: 10.1016/0306-4522(95)00051-j. [DOI] [PubMed] [Google Scholar]
- Arion D, Unger T, Lewis DA, Mirnics K. Molecular markers distinguishing supragranular and infragranular layers in the human prefrontal cortex. Eur J Neurosci. 2007;25:1843–1854. doi: 10.1111/j.1460-9568.2007.05396.x. [DOI] [PubMed] [Google Scholar]
- Arnsten AF, Paspalas CD, Gamo NJ, Yang Y, Wang M. Dynamic Network Connectivity: A new form of neuroplasticity. Trends Cogn Sci. 2010a;14:365–375. doi: 10.1016/j.tics.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnsten AF, Paspalas CD, Gamo NJ, Yang Y, Wang M. Dynamic Network Connectivity: A new form of neuroplasticity. Trends Cogn Sci. 2010b;14:365–375. doi: 10.1016/j.tics.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnsten AFT, Cai JS, Goldman-Rakic PS. The alpha-2 adrenergic agonist guanfacine improves memory in aged monkeys without sedative or hypotensive side effects: evidence for alpha-2 receptor subtypes. J Neurosci. 1988;8:4287–4298. doi: 10.1523/JNEUROSCI.08-11-04287.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin TA, MacAskill AF, Brandon NJ, Kittler JT. Disrupted in Schizophrenia-1 regulates intracellular trafficking of mitochondria in neurons. Mol Psychiatry. 2011;16:122–124. 121. doi: 10.1038/mp.2010.110. [DOI] [PubMed] [Google Scholar]
- Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. Pharmacoeconomics. 2008;26:149–162. doi: 10.2165/00019053-200826020-00005. [DOI] [PubMed] [Google Scholar]
- Baker K, Chaddock CA, Baldeweg T, Skuse D. Neuroanatomy in adolescents and young adults with 22q11 deletion syndrome: comparison to an IQ-matched group. NeuroImage. 2011;55:491–499. doi: 10.1016/j.neuroimage.2010.12.041. [DOI] [PubMed] [Google Scholar]
- Balu DT, Basu AC, Corradi JP, Cacace AM, Coyle JT. The NMDA receptor co-agonists, d-serine and glycine, regulate neuronal dendritic architecture in the somatosensory cortex. Neurobiol Dis. 2011 doi: 10.1016/j.nbd.2011.10.006. [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baracskay KL, Haroutunian V, Meador-Woodruff JH. Dopamine receptor signaling molecules are altered in elderly schizophrenic cortex. Synapse. 2006;60:271–279. doi: 10.1002/syn.20292. [DOI] [PubMed] [Google Scholar]
- Bauer D, Gupta D, Harotunian V, Meador-Woodruff JH, McCullumsmith RE. Abnormal expression of glutamate transporter and transporter interacting molecules in prefrontal cortex in elderly patients with schizophrenia. Schizophr Res. 2008;104:108–120. doi: 10.1016/j.schres.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett MR. Schizophrenia: susceptibility genes, dendritic-spine pathology and gray matter loss. Prog Neurobiol. 2011;95:275–300. doi: 10.1016/j.pneurobio.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Bernstein HG, Steiner J, Bogerts B. Glial cells in schizophrenia: pathophysiological significance and possible consequences for therapy. Expert Rev Neurother. 2009;9:1059–1071. doi: 10.1586/ern.09.59. [DOI] [PubMed] [Google Scholar]
- Bogerts B, Meertz E, Schönfeldt-Bausch R. Basal ganglia and limbic system pathology in schizophrenia. A morphometric study of brain volume and shrinkage. Arch Gen Psychiatry. 1985;42:784–791. doi: 10.1001/archpsyc.1985.01790310046006. [DOI] [PubMed] [Google Scholar]
- Bolam JP, Hanley JJ, Booth PA, Bevan MD. Synaptic organisation of the basal ganglia. J Anat. 2000;196(Pt 4):527–542. doi: 10.1046/j.1469-7580.2000.19640527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongmba OY, Martinez LA, Elhardt ME, Butler K, Tejada-Simon MV. Modulation of dendritic spines and synaptic function by Rac1: a possible link to Fragile X syndrome pathology. Brain Res. 2011;1399:79–95. doi: 10.1016/j.brainres.2011.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgwardt SJ, Picchioni MM, Ettinger U, Toulopoulou T, Murray R, McGuire PK. Regional gray matter volume in monozygotic twins concordant and discordant for schizophrenia. Biol Psychiatry. 2010;67:956–964. doi: 10.1016/j.biopsych.2009.10.026. [DOI] [PubMed] [Google Scholar]
- Borgwardt SJ, Riecher-Rossler A, Dazzan P, Chitnis X, Aston J, Drewe M, Gschwandtner U, Haller S, Pfluger M, Rechsteiner E, D'Souza M, Stieglitz RD, Radu EW, McGuire PK. Regional gray matter volume abnormalities in the at risk mental state. Biol Psychiatry. 2007;61:1148–1156. doi: 10.1016/j.biopsych.2006.08.009. [DOI] [PubMed] [Google Scholar]
- Bourgeois J-P, Goldman-Rakic PS, Rakic P. Synaptogenesis in the prefrontal cortex of rhesus monkeys. Cereb Cortex. 1994;4:78–96. doi: 10.1093/cercor/4.1.78. [DOI] [PubMed] [Google Scholar]
- Bourne J, Harris KM. Do thin spines learn to be mushroom spines that remember? Curr Opin Neurobiol. 2007;17:381–386. doi: 10.1016/j.conb.2007.04.009. [DOI] [PubMed] [Google Scholar]
- Bourne JN, Harris KM. Balancing structure and function at hippocampal dendritic spines. Annu Rev Neurosci. 2008;31:47–67. doi: 10.1146/annurev.neuro.31.060407.125646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt GN, Bonelli RM. Structural neuroimaging of the basal ganglia in schizophrenic patients: a review. Wien Med Wochenschr. 2008;158:84–90. doi: 10.1007/s10354-007-0478-7. [DOI] [PubMed] [Google Scholar]
- Brennaman LH, Kochlamazashvili G, Stoenica L, Nonneman RJ, Moy SS, Schachner M, Dityatev A, Maness PF. Transgenic mice overexpressing the extracellular domain of NCAM are impaired in working memory and cortical plasticity. Neurobiol Dis. 2011;43:372–378. doi: 10.1016/j.nbd.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadbelt K, Byne W, Jones LB. Evidence for a decrease in basilar dendrites of pyramidal cells in schizophrenic medial prefrontal cortex. Schizophr Res. 2002;58:75–81. doi: 10.1016/s0920-9964(02)00201-3. [DOI] [PubMed] [Google Scholar]
- Buell SJ. Golgi-Cox and rapid golgi methods as applied to autopsied human brain tissue: widely disparate results. J Neuropathol Exp Neurol. 1982;41:500–507. doi: 10.1097/00005072-198209000-00003. [DOI] [PubMed] [Google Scholar]
- Byne W, Buchsbaum MS, Mattiace LA, Hazlett EA, Kemether E, Elhakem SL, Purohit DP, Haroutunian V, Jones L. Postmortem assessment of thalamic nuclear volumes in subjects with schizophrenia. Am J Psychiatry. 2002;159:59–65. doi: 10.1176/appi.ajp.159.1.59. [DOI] [PubMed] [Google Scholar]
- Cahill ME, Jones KA, Rafalovich I, Xie Z, Barros CS, Muller U, Penzes P. Control of interneuron dendritic growth through NRG1/erbB4-mediated kalirin-7 disinhibition. Mol Psychiatry. 2012;17:99–107. doi: 10.1038/mp.2011.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill ME, Xie Z, Day M, Photowala H, Barbolina MV, Miller CA, Weiss C, Radulovic J, Sweatt JD, Disterhoft JF, Surmeier DJ, Penzes P. Kalirin regulates cortical spine morphogenesis and disease-related behavioral phenotypes. Proc Natl Acad Sci U S A. 2009;106:13058–13063. doi: 10.1073/pnas.0904636106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese B, Wilson MS, Halpain S. Development and regulation of dendritic spine synapses. Physiology (Bethesda) 2006;21:38–47. doi: 10.1152/physiol.00042.2005. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Thompson PM, van Erp TGM, Toga AW, Poutanen V-P, Huttunen M, Lonnqvist J, Standertskjold-Nordenstam C-G, Narr KL, Khaledy M, Zoumalan CI, Dail R, Kaprio J. Cortex mapping reveals regionally specific patterns of genetic and disease-specific gray-matter deficits in twins discordant for schizophrenia. Proc Natl Acad Sci USA. 2002;99:3228–3223. doi: 10.1073/pnas.052023499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardno AG, Marshall EJ, Coid B, MacDonald AM, Ribchester TR, Davies NJ, Venturi P, Jones LA, Lewis SW, Sham PC, Gottesman II, Farmer AE, McGuffin P, Reveley AM, Murray RM. Heritability estimates for psychotic disorders: the Maudsley twin psychosis series. Arch Gen Psychiatry. 1999;56:162–168. doi: 10.1001/archpsyc.56.2.162. [DOI] [PubMed] [Google Scholar]
- Casadio P, Fernandes C, Murray RM, Di Forti M. Cannabis use in young people: the risk for schizophrenia. Neurosci Biobehav Rev. 2011;35:1779–1787. doi: 10.1016/j.neubiorev.2011.04.007. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, Levita L, Libby V, Pattwell SS, Ruberry EJ, Soliman F, Somerville LH. The storm and stress of adolescence: insights from human imaging and mouse genetics. Dev Psychobiol. 2010;52:225–235. doi: 10.1002/dev.20447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerri C, Fabbri A, Vannini E, Spolidoro M, Costa M, Maffei L, Fiorentini C, Caleo M. Activation of Rho GTPases triggers structural remodeling and functional plasticity in the adult rat visual cortex. J Neurosci. 2011;31:15163–15172. doi: 10.1523/JNEUROSCI.2617-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng A, Hou Y, Mattson MP. Mitochondria and neuroplasticity. ASN Neuro. 2010:2. doi: 10.1042/AN20100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng HW, Rafols JA, Goshgarian HG, Anavi Y, Tong J, McNeill TH. Differential spine loss and regrowth of striatal neurons following multiple forms of deafferentation: a Golgi study. Exp Neurol. 1997;147:287–298. doi: 10.1006/exnr.1997.6618. [DOI] [PubMed] [Google Scholar]
- Cho RY, Konecky RO, Carter CS. Impairments in frontal cortical gamma synchrony and cognitive control in schizophrenia. Proc Natl Acad Sci U S A. 2006;103:19878–19883. doi: 10.1073/pnas.0609440103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu-Shore CJ, Kramer MA, Bianchi MT, Caviness VS, Cash SS. Network analysis: applications for the developing brain. J Child Neurol. 2011;26:488–500. doi: 10.1177/0883073810385345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chubb JE, Bradshaw NJ, Soares DC, Porteous DJ, Millar JK. The DISC locus in psychiatric illness. Mol Psychiatry. 2008;13:36–64. doi: 10.1038/sj.mp.4002106. [DOI] [PubMed] [Google Scholar]
- Clay HB, Sillivan S, Konradi C. Mitochondrial dysfunction and pathology in bipolar disorder and schizophrenia. Int J Dev Neurosci. 2011;29:311–324. doi: 10.1016/j.ijdevneu.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corradini I, Verderio C, Sala M, Wilson MC, Matteoli M. SNAP-25 in neuropsychiatric disorders. Ann N Y Acad Sci. 2009;1152:93–99. doi: 10.1111/j.1749-6632.2008.03995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen TJ, Walker MA, Parkinson N, Craven R, Crow TJ, Esiri MM, Harrison PJ. A postmortem study of the mediodorsal nucleus of the thalamus in schizophrenia. Schizophr Res. 2003;60:157–166. doi: 10.1016/s0920-9964(02)00297-9. [DOI] [PubMed] [Google Scholar]
- DeFelipe J, Farinas I. The pyramidal neuron of the cerebral cortex: Morphological and chemical characteristics of the synaptic inputs. Prog Neurobiol. 1992;39:563–607. doi: 10.1016/0301-0082(92)90015-7. [DOI] [PubMed] [Google Scholar]
- Deo AJ, Cahill ME, Li S, Goldszer I, Henteleff R, VanLeeuwen JE, Rafalovich I, Gao R, Stachowski EK, Sampson AR, Lewis DA, Penzes P, Sweet RA. Increased expression of Kalirin-9 in the auditory cortex of schizophrenia subjects: Its role in dendritic pathology. Neurobiol Dis. 2011a doi: 10.1016/j.nbd.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deo AJ, Cahill ME, Li S, Goldszer I, Henteleff R, VanLeeuwen JE, Rafalovich I, Gao R, Stachowski EK, Sampson AR, Lewis DA, Penzes P, Sweet RA. Increased expression of Kalirin-9 in the auditory cortex of schizophrenia subjects: Its role in dendritic pathology. Neurobiol Dis. 2011b doi: 10.1016/j.nbd.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVito LM, Balu DT, Kanter BR, Lykken C, Basu AC, Coyle JT, Eichenbaum H. Serine racemase deletion disrupts memory for order and alters cortical dendritic morphology. Genes Brain Behav. 2011;10:210–222. doi: 10.1111/j.1601-183X.2010.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorph-Petersen KA, Lewis DA. Stereological approaches to identifying neuropathology in psychosis. Biol Psychiatry. 2011;69:113–126. doi: 10.1016/j.biopsych.2010.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorph-Petersen K-A, Delevich KM, Marcsisin MJ, Zhang W, Sampson AR, Gundersen HJG, Lewis DA, Sweet RA. Pyramidal neuron number in layer 3 of primary auditory cortex of subjects with schizophrenia. Brain Res. 2009;1285:42–57. doi: 10.1016/j.brainres.2009.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorph-Petersen K-A, Pierri JN, Sun Z, Sampson AR, Lewis DA. Stereological analysis of the mediodorsal thalamic nucleus in schizophrenia: Volume, neuron number, and cell types. J Comp Neurol. 2004;472:449–462. doi: 10.1002/cne.20055. [DOI] [PubMed] [Google Scholar]
- Drew LJ, Crabtree GW, Markx S, Stark KL, Chaverneff F, Xu B, Mukai J, Fenelon K, Hsu PK, Gogos JA, Karayiorgou M. The 22q11.2 microdeletion: fifteen years of insights into the genetic and neural complexity of psychiatric disorders. Int J Dev Neurosci. 2011;29:259–281. doi: 10.1016/j.ijdevneu.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumitriu D, Hao J, Hara Y, Kaufmann J, Janssen WG, Lou W, Rapp PR, Morrison JH. Selective changes in thin spine density and morphology in monkey prefrontal cortex correlate with aging-related cognitive impairment. J Neurosci. 2010;30:7507–7515. doi: 10.1523/JNEUROSCI.6410-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliez S, Schmitt JE, White CD, Reiss AL. Children and adolescents with velocardiofacial syndrome: a volumetric MRI study. Am J Psychiatry. 2000;157:409–415. doi: 10.1176/appi.ajp.157.3.409. [DOI] [PubMed] [Google Scholar]
- Elvevag B, Goldberg TE. Cognitive impairment in schizophrenia is the core of the disorder. Crit Rev Neurobiol. 2000;14:1–21. [PubMed] [Google Scholar]
- Fearon P, Kirkbride JB, Morgan C, Dazzan P, Morgan K, Lloyd T, Hutchinson G, Tarrant J, Fung WL, Holloway J, Mallett R, Harrison G, Leff J, Jones PB, Murray RM. Incidence of schizophrenia and other psychoses in ethnic minority groups: results from the MRC AESOP Study. Psychol Med. 2006;36:1541–1550. doi: 10.1017/S0033291706008774. [DOI] [PubMed] [Google Scholar]
- Feinberg I. Schizophrenia: Caused by a fault in programmed synaptic elimination during adolescence? J Psychiatry Res. 1982;17:319–334. doi: 10.1016/0022-3956(82)90038-3. [DOI] [PubMed] [Google Scholar]
- Fiala JC, Spacek J, Harris KM. Dendritic spine pathology: cause or consequence of neurological disorders? Brain Res Brain Res Rev. 2002;39:29–54. doi: 10.1016/s0165-0173(02)00158-3. [DOI] [PubMed] [Google Scholar]
- Fornito A, Yung AR, Wood SJ, Phillips LJ, Nelson B, Cotton S, Velakoulis D, McGorry PD, Pantelis C, Yucel M. Anatomic abnormalities of the anterior cingulate cortex before psychosis onset: an MRI study of ultra-high-risk individuals. Biol Psychiatry. 2008;64:758–765. doi: 10.1016/j.biopsych.2008.05.032. [DOI] [PubMed] [Google Scholar]
- Franowicz JS, Arnsten AF. The alpha-2a noradrenergic agonist, guanfacine, improves delayed response performance in young adult rhesus monkeys. Psychopharmacology (Berl) 1998;136:8–14. doi: 10.1007/s002130050533. [DOI] [PubMed] [Google Scholar]
- Friedman JI, Adler DN, Temporini HD, Kemether E, Harvey PD, White L, Parrella M, Davis KL. Guanfacine treatment of cognitive impairment in schizophrenia. Neuropsychopharm. 2001;25:402–409. doi: 10.1016/S0893-133X(01)00249-4. [DOI] [PubMed] [Google Scholar]
- Fung SJ, Sivagnanasundaram S, Weickert CS. Lack of change in markers of presynaptic terminal abundance alongside subtle reductions in markers of presynaptic terminal plasticity in prefrontal cortex of schizophrenia patients. Biol Psychiatry. 2011;69:71–79. doi: 10.1016/j.biopsych.2010.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Lopez P, Garcia-Marin V, Freire M. Dendritic spines and development: towards a unifying model of spinogenesis--a present day review of Cajal's histological slides and drawings. Neural Plast. 2010;2010 doi: 10.1155/2010/769207. 769207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garey LJ, Ong WY, Patel TS, Kanani M, Davis A, Mortimer AM, Barnes TRE, Hirsch SR. Reduced dendritic spine density on cerebral cortical pyramidal neurons in schizophrenia. J Neurol Neurosurg Psychiatry. 1998;65:446–453. doi: 10.1136/jnnp.65.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gigante AD, Andreazza AC, Lafer B, Yatham LN, Beasley CL, Young LT. Decreased mRNA expression of uncoupling protein 2, a mitochondrial proton transporter, in post-mortem prefrontal cortex from patients with bipolar disorder and schizophrenia. Neurosci Lett. 2011;505:47–51. doi: 10.1016/j.neulet.2011.09.064. [DOI] [PubMed] [Google Scholar]
- Gilbert CD, Kelly JP. The projections of cells in different layers of the cat's visual cortex. J Comp Neurol. 1975;63:81–106. doi: 10.1002/cne.901630106. [DOI] [PubMed] [Google Scholar]
- Gilmore JH, Kang C, Evans DD, Wolfe HM, Smith JK, Lieberman JA, Lin W, Hamer RM, Styner M, Gerig G. Prenatal and neonatal brain structure and white matter maturation in children at high risk for schizophrenia. Am J Psychiatry. 2010;167:1083–1091. doi: 10.1176/appi.ajp.2010.09101492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glahn DC, Laird AR, Ellison-Wright I, Thelen SM, Robinson JL, Lancaster JL, Bullmore E, Fox PT. Meta-analysis of gray matter anomalies in schizophrenia: application of anatomic likelihood estimation and network analysis. Biol Psychiatry. 2008;64:774–781. doi: 10.1016/j.biopsych.2008.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glantz LA, Lewis DA. Reduction of synaptophysin immunoreactivity in the prefrontal cortex of subjects with schizophrenia: Regional and diagnostic specificity. Arch Gen Psychiatry. 1997;54:943–952. doi: 10.1001/archpsyc.1997.01830220065010. [DOI] [PubMed] [Google Scholar]
- Glantz LA, Lewis DA. Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Arch Gen Psychiatry. 2000;57:65–73. doi: 10.1001/archpsyc.57.1.65. [DOI] [PubMed] [Google Scholar]
- Goldman-Rakic PS. Working memory dysfunction in schizophrenia. J Neuropsychiatry Clin Neurosci. 1994;6:348–357. doi: 10.1176/jnp.6.4.348. [DOI] [PubMed] [Google Scholar]
- Goldman-Rakic PS, Leranth C, Williams SM, Mons N, Geffard M. Dopamine synaptic complex with pyramidal neurons in primate cerebral cortex. Proc Natl Acad Sci USA. 1989;86:9015–9019. doi: 10.1073/pnas.86.22.9015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman-Rakic PS, Muly EC, III, Williams GV. D(1) receptors in prefrontal cells and circuits. Brain Res Brain Res Rev. 2000;31:295–301. doi: 10.1016/s0165-0173(99)00045-4. [DOI] [PubMed] [Google Scholar]
- Gottesman II. Schizophrenia Genesis: The Origins of Madness. New York: W.H. Freeman; 1991. [Google Scholar]
- Gray EG. Axo-somatic and axo-dendritic synapses of the cerebral cortex: An electron microscopic study. J Anat. 1959;93:420–433. [PMC free article] [PubMed] [Google Scholar]
- Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry. 2006;67(Suppl 9):3–8. [PubMed] [Google Scholar]
- Grossman LS, Harrow M, Rosen C, Faull R, Strauss GP. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49:523–529. doi: 10.1016/j.comppsych.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grutzendler J, Kasthuri N, Gan W-B. Long-term dendritic spine stability in the adult cortex. Nature. 2002;420:812–816. doi: 10.1038/nature01276. [DOI] [PubMed] [Google Scholar]
- Hains AB, Vu MA, Maciejewski PK, van Dyck CH, Gottron M, Arnsten AF. Inhibition of protein kinase C signaling protects prefrontal cortex dendritic spines and cognition from the effects of chronic stress. Proc Natl Acad Sci U S A. 2009;106:17957–17962. doi: 10.1073/pnas.0908563106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamori J. The inductive role of presynaptic axons in the development of postsynaptic spines. Brain Res. 1973;62:337–344. doi: 10.1016/0006-8993(73)90694-x. [DOI] [PubMed] [Google Scholar]
- Hao J, Rapp PR, Janssen WG, Lou W, Lasley BL, Hof PR, Morrison JH. Interactive effects of age and estrogen on cognition and pyramidal neurons in monkey prefrontal cortex. Proc Natl Acad Sci U S A. 2007;104:11465–11470. doi: 10.1073/pnas.0704757104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao J, Rapp PR, Leffler AE, Leffler SR, Janssen WG, Lou W, McKay H, Roberts JA, Wearne SL, Hof PR, Morrison JH. Estrogen alters spine number and morphology in prefrontal cortex of aged female rhesus monkeys. J Neurosci. 2006;26:2571–2578. doi: 10.1523/JNEUROSCI.3440-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Kater SB. Dendritic spines: Cellular specializations imparting both stability and flexibility to synaptic function. Annu Rev Neurosci. 1994;17:341–371. doi: 10.1146/annurev.ne.17.030194.002013. [DOI] [PubMed] [Google Scholar]
- Harrison PJ. The hippocampus in schizophrenia: a review of the neuropathological evidence and its pathophysiological implications. Psychopharmacology (Berl) 2004;174:151–162. doi: 10.1007/s00213-003-1761-y. [DOI] [PubMed] [Google Scholar]
- Harvey PD. Cognitive Outcomes in the CATIE Schizophrenia Trial: Why do they seem different from previous results? Psychiatry (Edgmont) 2007;4:20–23. [PMC free article] [PubMed] [Google Scholar]
- Hayashi-Takagi A, Takaki M, Graziane N, Seshadri S, Murdoch H, Dunlop AJ, Makino Y, Seshadri AJ, Ishizuka K, Srivastava DP, Xie Z, Baraban JM, Houslay MD, Tomoda T, Brandon NJ, Kamiya A, Yan Z, Penzes P, Sawa A. Disrupted-in-Schizophrenia 1 (DISC1) regulates spines of the glutamate synapse via Rac1. Nat Neurosci. 2010;13:327–332. doi: 10.1038/nn.2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes TL, Lewis DA. Magnopyramidal neurons in the anterior motor speech region: Dendritic features and interhemispheric comparisons. Arch Neurol. 1996;53:1277–1283. doi: 10.1001/archneur.1996.00550120089021. [DOI] [PubMed] [Google Scholar]
- Hill JJ, Hashimoto T, Lewis DA. Molecular mechanisms contributing to dendritic spine alterations in the prefrontal cortex of subjects with schizophrenia. Mol Psychiatry. 2006;11:557–566. doi: 10.1038/sj.mp.4001792. [DOI] [PubMed] [Google Scholar]
- Hoffman RE, Dobscha SK. Cortical pruning and the development of schizophrenia: A computer model. Schizophr Bull. 1989;15:477–490. doi: 10.1093/schbul/15.3.477. [DOI] [PubMed] [Google Scholar]
- Holtmaat AJ, Trachtenberg JT, Wilbrecht L, Shepherd GM, Zhang X, Knott GW, Svoboda K. Transient and persistent dendritic spines in the neocortex in vivo. Neuron. 2005;45:279–291. doi: 10.1016/j.neuron.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Honea R, Crow TJ, Passingham D, Mackay CE. Regional deficits in brain volume in schizophrenia: a meta-analysis of voxel-based morphometry studies. Am J Psychiatry. 2005;162:2233–2245. doi: 10.1176/appi.ajp.162.12.2233. [DOI] [PubMed] [Google Scholar]
- Horga G, Bernacer J, Dusi N, Entis J, Chu K, Hazlett EA, Mehmet HM, Kemether E, Byne W, Buchsbaum MS. Correlations between ventricular enlargement and gray and white matter volumes of cortex, thalamus, striatum, and internal capsule in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2011;261:467–476. doi: 10.1007/s00406-011-0202-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner CH, Arbuthnott E. Methods of estimation of spine density--are spines evenly distributed throughout the dendritic field? J Anat. 1991;177:179–184. [PMC free article] [PubMed] [Google Scholar]
- Hu J, Vidovic M, Chen MM, Lu QY, Song ZM. Activation of alpha 2A adrenoceptors alters dendritic spine development and the expression of spinophilin in cultured cortical neurones. Brain Res. 2008;1199:37–45. doi: 10.1016/j.brainres.2007.12.073. [DOI] [PubMed] [Google Scholar]
- Hulshoff Pol HE, Brans RG, van Haren NE, Schnack HG, Langen M, Baare WF, van Oel CJ, Kahn RS. Gray and white matter volume abnormalities in monozygotic and same-gender dizygotic twins discordant for schizophrenia. Biol Psychiatry. 2004;55:126–130. doi: 10.1016/s0006-3223(03)00728-5. [DOI] [PubMed] [Google Scholar]
- Huttenlocher PR. Synaptic density in human frontal cortex - Developmental changes and effects of aging. Brain Res. 1979;163:195–205. doi: 10.1016/0006-8993(79)90349-4. [DOI] [PubMed] [Google Scholar]
- Huttenlocher PR, Dabholkar AS. Regional differences in synaptogenesis in human cerebral cortex. J Comp Neurol. 1997;387:167–178. doi: 10.1002/(sici)1096-9861(19971020)387:2<167::aid-cne1>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Ide M, Lewis DA. Altered cortical CDC42 signaling pathways in schizophrenia: Implications for dendritic spine deficits. Biol Psychiatry. 2010;68:25–32. doi: 10.1016/j.biopsych.2010.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda M, Aleksic B, Kinoshita Y, Okochi T, Kawashima K, Kushima I, Ito Y, Nakamura Y, Kishi T, Okumura T, Fukuo Y, Williams HJ, Hamshere ML, Ivanov D, Inada T, Suzuki M, Hashimoto R, Ujike H, Takeda M, Craddock N, Kaibuchi K, Owen MJ, Ozaki N, O'Donovan MC, Iwata N. Genome-wide association study of schizophrenia in a Japanese population. Biol Psychiatry. 2011;69:472–478. doi: 10.1016/j.biopsych.2010.07.010. [DOI] [PubMed] [Google Scholar]
- Insel TR, Scolnick EM. Cure therapeutics and strategic prevention: raising the bar for mental health research. Mol Psychiatry. 2006;11:11–17. doi: 10.1038/sj.mp.4001777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irie F, Yamaguchi Y. EphB receptors regulate dendritic spine development via intersectin, Cdc42 and N-WASP. Nat Neurosci. 2002;5:1117–1118. doi: 10.1038/nn964. [DOI] [PubMed] [Google Scholar]
- Ishihara N, Nomura M, Jofuku A, Kato H, Suzuki SO, Masuda K, Otera H, Nakanishi Y, Nonaka I, Goto Y, Taguchi N, Morinaga H, Maeda M, Takayanagi R, Yokota S, Mihara K. Mitochondrial fission factor Drp1 is essential for embryonic development and synapse formation in mice. Nat Cell Biol. 2009;11:958–966. doi: 10.1038/ncb1907. [DOI] [PubMed] [Google Scholar]
- Jacobs B, Creswell J, Britt JP, Ford KL, Bogen JE, Zaidel E. Quantitative analysis of cortical pyramidal neurons after corpus callosotomy. Ann Neurol. 2003;54:126–130. doi: 10.1002/ana.10620. [DOI] [PubMed] [Google Scholar]
- Jacobs B, Driscoll L, Schall M. Life-span dendritic and spine changes in areas 10 and 18 of human cortex: A quantitative Golgi study. J Comp Neurol. 1997;386:661–680. [PubMed] [Google Scholar]
- Jones EG. Laminar distribution of cortical efferent cells. In: Peters A, Jones EG, editors. Cerebral Cortex. Vol. 1. New York: Plenum Press; 1984. pp. 521–553. [Google Scholar]
- Kakeda S, Korogi Y. The efficacy of a voxel-based morphometry on the analysis of imaging in schizophrenia, temporal lobe epilepsy, and Alzheimer's disease/mild cognitive impairment: a review. Neuroradiology. 2010;52:711–721. doi: 10.1007/s00234-010-0717-2. [DOI] [PubMed] [Google Scholar]
- Kalus P, Müller TJ, Zuschratter W, Senitz D. The dendritic architecture of prefrontal pyramidal neurons in schizophrenic patients. NeuroReport. 2000;11:3621–3625. doi: 10.1097/00001756-200011090-00044. [DOI] [PubMed] [Google Scholar]
- Kane JM. Schizophrenia. N Engl J Med. 1996;334:34–41. doi: 10.1056/NEJM199601043340109. [DOI] [PubMed] [Google Scholar]
- Kasai H, Fukuda M, Watanabe S, Hayashi-Takagi A, Noguchi J. Structural dynamics of dendritic spines in memory and cognition. Trends Neurosci. 2010;33:121–129. doi: 10.1016/j.tins.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Kasai H, Matsuzaki M, Noguchi J, Yasumatsu N, Nakahara H. Structure-stability-function relationships of dendritic spines. Trends Neurosci. 2003a;26:360–368. doi: 10.1016/S0166-2236(03)00162-0. [DOI] [PubMed] [Google Scholar]
- Kasai K, Shenton ME, Salisbury DF, Hirayasu Y, Onitsuka T, Spencer MH, Yurgelun-Todd DA, Kikinis R, Jolesz FA, McCarley RW. Progressive decrease of left Heschl gyrus and planum temporale gray matter volume in first-episode schizophrenia: a longitudinal magnetic resonance imaging study. Arch Gen Psychiatry. 2003b;60:766–775. doi: 10.1001/archpsyc.60.8.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kates WR, Antshel KM, Faraone SV, Fremont WP, Higgins AM, Shprintzen RJ, Botti JA, Kelchner L, McCarthy C. Neuroanatomic predictors to prodromal psychosis in velocardiofacial syndrome (22q11.2 deletion syndrome): a longitudinal study. Biol Psychiatry. 2011;69:945–952. doi: 10.1016/j.biopsych.2010.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kates WR, Burnette CP, Jabs EW, Rutberg J, Murphy AM, Grados M, Geraghty M, Kaufmann WE, Pearlson GD. Regional cortical white matter reductions in velocardiofacial syndrome: a volumetric MRI analysis. Biol Psychiatry. 2001;49:677–684. doi: 10.1016/s0006-3223(00)01002-7. [DOI] [PubMed] [Google Scholar]
- Keefe RS, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM, Meltzer HY, Green MF, Capuano G, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Davis CE, Hsiao JK, Lieberman JA. Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry. 2007;64:633–647. doi: 10.1001/archpsyc.64.6.633. [DOI] [PubMed] [Google Scholar]
- Kelley JJ, Gao XM, Tamminga CA, Roberts RC. The effect of chronic haloperidol treatment on dendritic spines in the rat striatum. Exp Neurol. 1997;146:471–478. doi: 10.1006/exnr.1997.6552. [DOI] [PubMed] [Google Scholar]
- Keshavan MS, Diwadkar VA, Montrose DM, Stanley JA, Pettegrew JW. Premorbid characterization in schizophrenia: the Pittsburgh High Risk Study. World Psychiatry. 2004;3:163–168. [PMC free article] [PubMed] [Google Scholar]
- Khaitovich P, Lockstone HE, Wayland MT, Tsang TM, Jayatilaka SD, Guo AJ, Zhou J, Somel M, Harris LW, Holmes E, Paabo S, Bahn S. Metabolic changes in schizophrenia and human brain evolution. Genome Biol. 2008;9:R124. doi: 10.1186/gb-2008-9-8-r124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Zerwas S, Trace SE, Sullivan PF. Schizophrenia genetics: where next? Schizophr Bull. 2011;37:456–463. doi: 10.1093/schbul/sbr031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolluri N, Sun Z, Sampson AR, Lewis DA. Lamina-specific reductions in dendritic spine density in the prefrontal cortex of subjects with schizophrenia. Am J Psychiatry. 2005;162:1200–1202. doi: 10.1176/appi.ajp.162.6.1200. [DOI] [PubMed] [Google Scholar]
- Kolomeets NS, Orlovskaya DD, Rachmanova VI, Uranova NA. Ultrastructural alterations in hippocampal mossy fiber synapses in schizophrenia: a postmortem morphometric study. Synapse. 2005;57:47–55. doi: 10.1002/syn.20153. [DOI] [PubMed] [Google Scholar]
- Kolomeets NS, Orlovskaya DD, Uranova NA. Decreased numerical density of CA3 hippocampal mossy fiber synapses in schizophrenia. Synapse. 2007;61:615–621. doi: 10.1002/syn.20405. [DOI] [PubMed] [Google Scholar]
- Kreczmanski P, Heinsen H, Mantua V, Woltersdorf F, Masson T, Ulfig N, Schmidt-Kastner R, Korr H, Steinbusch HWM, Hof PR, Schmitz C. Volume, neuron density and total neuron number in five subcortical regions in schizophrenia. Brain. 2007;130:678–692. doi: 10.1093/brain/awl386. [DOI] [PubMed] [Google Scholar]
- Kreis P, Thevenot E, Rousseau V, Boda B, Muller D, Barnier JV. The p21-activated kinase 3 implicated in mental retardation regulates spine morphogenesis through a Cdc42-dependent pathway. J Biol Chem. 2007;282:21497–21506. doi: 10.1074/jbc.M703298200. [DOI] [PubMed] [Google Scholar]
- Kritzer MF, Goldman-Rakic PS. Intrinsic circuit organization of the major layers and sublayers of the dorsolateral prefrontal cortex in the rhesus monkey. J Comp Neurol. 1995;359:131–143. doi: 10.1002/cne.903590109. [DOI] [PubMed] [Google Scholar]
- Kulkarni J, Gurvich C, Lee SJ, Gilbert H, Gavrilidis E, de Castella A, Berk M, Dodd S, Fitzgerald PB, Davis SR. Piloting the effective therapeutic dose of adjunctive selective estrogen receptor modulator treatment in postmenopausal women with schizophrenia. Psychoneuroendocrinology. 2010;35:1142–1147. doi: 10.1016/j.psyneuen.2010.01.014. [DOI] [PubMed] [Google Scholar]
- Kung L, Force M, Chute DJ, Roberts RC. Immunocytochemical localization of tyrosine hydroxylase in the human striatum: a postmortem ultrastructural study. J Comp Neurol. 1998;390:52–62. doi: 10.1002/(sici)1096-9861(19980105)390:1<52::aid-cne5>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Kushima I, Nakamura Y, Aleksic B, Ikeda M, Ito Y, Shiino T, Okochi T, Fukuo Y, Ujike H, Suzuki M, Inada T, Hashimoto R, Takeda M, Kaibuchi K, Iwata N, Ozaki N. Resequencing and association analysis of the KALRN and EPHB1 genes and their contribution to schizophrenia susceptibility. Schizophr Bull. 2010 doi: 10.1093/schbul/sbq118. [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrie SM, Abukmeil SS. Brain abnormality in schizophrenia: A systematic and quantitative review of volumetric magnetic resonance imaging studies. Br J Psychiatry. 1998;172:110–120. doi: 10.1192/bjp.172.2.110. [DOI] [PubMed] [Google Scholar]
- Lesh TA, Niendam TA, Minzenberg MJ, Carter CS. Cognitive control deficits in schizophrenia: mechanisms and meaning. Neuropsychopharm. 2011;36:316–338. doi: 10.1038/npp.2010.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leuner B, Gould E. Structural plasticity and hippocampal function. Annu Rev Psychol. 2010;61:111–113. doi: 10.1146/annurev.psych.093008.100359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt JJ, Bobrow L, Lucia D, Srinivasan P. A selective review of volumetric and morphometric imaging in schizophrenia. Curr Top Behav Neurosci. 2010;4:243–281. doi: 10.1007/7854_2010_53. [DOI] [PubMed] [Google Scholar]
- Lewis DA, Curley AA, Glausier JR, Volk DW. Cortical parvalbumin interneurons and cognitive dysfunction in schizophrenia. Trends Neurosci. 2012;35:57–67. doi: 10.1016/j.tins.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis DA, Levitt P. Schizophrenia as a disorder of neurodevelopment. Annu Rev Neurosci. 2002;25:409–432. doi: 10.1146/annurev.neuro.25.112701.142754. [DOI] [PubMed] [Google Scholar]
- Lewis DA, Lieberman JA. Catching up on schizophrenia: Natural history and neurobiology. Neuron. 2000;28:325–334. doi: 10.1016/s0896-6273(00)00111-2. [DOI] [PubMed] [Google Scholar]
- Li Z, Okamoto K, Hayashi Y, Sheng M. The importance of dendritic mitochondria in the morphogenesis and plasticity of spines and synapses. Cell. 2004;119:873–887. doi: 10.1016/j.cell.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Stroup TS. The NIMH-CATIE Schizophrenia Study: what did we learn? Am J Psychiatry. 2011;168:770–775. doi: 10.1176/appi.ajp.2011.11010039. [DOI] [PubMed] [Google Scholar]
- Lin YC, Koleske AJ. Mechanisms of synapse and dendrite maintenance and their disruption in psychiatric and neurodegenerative disorders. Annu Rev Neurosci. 2010;33:349–378. doi: 10.1146/annurev-neuro-060909-153204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liston C, Gan WB. Glucocorticoids are critical regulators of dendritic spine development and plasticity in vivo. Proc Natl Acad Sci U S A. 2011;108:16074–16079. doi: 10.1073/pnas.1110444108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liston C, Miller MM, Goldwater DS, Radley JJ, Rocher AB, Hof PR, Morrison JH, McEwen BS. Stress-induced alterations in prefrontal cortical dendritic morphology predict selective impairments in perceptual attentional set-shifting. J Neurosci. 2006;26:7870–7874. doi: 10.1523/JNEUROSCI.1184-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund JS, Lund RD, Hendrickson AE, Bunt AH, Fuchs AF. The origin of efferent pathways from the primary visual cortex, area 17, of the macaque monkey as shown by retrograde transport of horseradish peroxidase. J Comp Neurol. 1975;164:287–304. doi: 10.1002/cne.901640303. [DOI] [PubMed] [Google Scholar]
- Marcelis M, Navarro-Mateau F, Murray R, Selten J-P, van Os J. Urbanization and psychosis: A study of 1942–1978 birth cohorts in The Netherlands. Psychol Med. 1998;28:871–879. doi: 10.1017/s0033291798006898. [DOI] [PubMed] [Google Scholar]
- Martins-de-Souza D, Harris LW, Guest PC, Bahn S. The role of energy metabolism dysfunction and oxidative stress in schizophrenia revealed by proteomics. Antioxid Redox Signal. 2011;15:2067–2079. doi: 10.1089/ars.2010.3459. [DOI] [PubMed] [Google Scholar]
- Matthews DA, Cotman C, Lynch G. An electron microscopic study of lesion-induced synaptogenesis in the dentate gyrus of the adult rat. II. Reappearance of morphologically normal synaptic contacts. Brain Res. 1976;115:23–41. doi: 10.1016/0006-8993(76)90820-9. [DOI] [PubMed] [Google Scholar]
- Mattson MP, Gleichmann M, Cheng A. Mitochondria in neuroplasticity and neurological disorders. Neuron. 2008;60:748–766. doi: 10.1016/j.neuron.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath J, Saha S, Welham J, El Saadi O, MacCauley C, Chant D. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004;2:13. doi: 10.1186/1741-7015-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh AM, Owens DC, Moorhead WJ, Whalley HC, Stanfield AC, Hall J, Johnstone EC, Lawrie SM. Longitudinal volume reductions in people at high genetic risk of schizophrenia as they develop psychosis. Biol Psychiatry. 2011;69:953–958. doi: 10.1016/j.biopsych.2010.11.003. [DOI] [PubMed] [Google Scholar]
- McKinney RA, Capogna M, Durr R, Gahwiler BH, Thompson SM. Miniature synaptic events maintain dendritic spines via AMPA receptor activation. Nat Neurosci. 1999;2:44–49. doi: 10.1038/4548. [DOI] [PubMed] [Google Scholar]
- Mechelli A, Riecher-Rossler A, Meisenzahl EM, Tognin S, Wood SJ, Borgwardt SJ, Koutsouleris N, Yung AR, Stone JM, Phillips LJ, McGorry PD, Valli I, Velakoulis D, Woolley J, Pantelis C, McGuire P. Neuroanatomical abnormalities that predate the onset of psychosis: a multicenter study. Arch Gen Psychiatry. 2011;68:489–495. doi: 10.1001/archgenpsychiatry.2011.42. [DOI] [PubMed] [Google Scholar]
- Mei L, Xiong WC. Neuregulin 1 in neural development, synaptic plasticity and schizophrenia. Nat Rev Neurosci. 2008;9:437–452. doi: 10.1038/nrn2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchitzky DS, González-Burgos G, Barrionuevo G, Lewis DA. Synaptic targets of the intrinsic axon collaterals of supragranular pyramidal neurons in monkey prefrontal cortex. J Comp Neurol. 2001;430:209–221. doi: 10.1002/1096-9861(20010205)430:2<209::aid-cne1026>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Melchitzky DS, Sesack SR, Lewis DA. Parvalbumin-immunoreactive axon terminals in macaque monkey and human prefrontal cortex: Laminar, regional and target specificity of Type I and Type II synapses. J Comp Neurol. 1999;408:11–22. [PubMed] [Google Scholar]
- Morgan C, Charalambides M, Hutchinson G, Murray RM. Migration, ethnicity, and psychosis: toward a sociodevelopmental model. Schizophr Bull. 2010;36:655–664. doi: 10.1093/schbul/sbq051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen PB, Pedersen CB, Westegaard T, Wohlfahrt J, Ewald H, Mors O, Andersen PK, Melbye M. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340:603–608. doi: 10.1056/NEJM199902253400803. [DOI] [PubMed] [Google Scholar]
- Moser M-B, Trommald M, Andersen P. An increase in dendritic spine density on hippocampal CA1 pyramidal cells following spatial learning in adult rats suggests the formation of new synapses. Proc Natl Acad Sci USA. 1994;91:12673–12675. doi: 10.1073/pnas.91.26.12673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukai J, Dhilla A, Drew LJ, Stark KL, Cao L, MacDermott AB, Karayiorgou M, Gogos JA. Palmitoylation-dependent neurodevelopmental deficits in a mouse model of 22q11 microdeletion. Nat Neurosci. 2008;11:1302–1310. doi: 10.1038/nn.2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakayama AY, Harms MB, Luo L. Small GTPases Rac and Rho in the maintenance of dendritic spines and branches in hippocampal pyramidal neurons. J Neurosci. 2000;20:5329–5338. doi: 10.1523/JNEUROSCI.20-14-05329.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negishi M, Katoh H. Rho family GTPases and dendrite plasticity. Neuroscientist. 2005;11:187–191. doi: 10.1177/1073858404268768. [DOI] [PubMed] [Google Scholar]
- Negyessy L, Goldman-Rakic PS. Morphometric characterization of synapses in the primate prefrontal cortex formed by afferents from the mediodorsal thalamic nucleus. Exp Brain Res. 2005;164:148–154. doi: 10.1007/s00221-005-2237-6. [DOI] [PubMed] [Google Scholar]
- O'Neill J, Fitten LJ, Siembieda DW, Ortiz F, Halgren E. Effects of guanfacine on three forms of distraction in the aging macaque. Life Sci. 2000;67:877–885. doi: 10.1016/s0024-3205(00)00681-0. [DOI] [PubMed] [Google Scholar]
- Olabi B, Ellison-Wright I, McIntosh AM, Wood SJ, Bullmore E, Lawrie SM. Are there progressive brain changes in schizophrenia? A meta-analysis of structural magnetic resonance imaging studies. Biol Psychiatry. 2011;70:88–96. doi: 10.1016/j.biopsych.2011.01.032. [DOI] [PubMed] [Google Scholar]
- Pakkenberg B. Pronounced reduction of total neuron number in mediodorsal thalamic nucleus and nucleus accumbens in schizophrenics. Arch Gen Psychiatry. 1990;47:1023–1028. doi: 10.1001/archpsyc.1990.01810230039007. [DOI] [PubMed] [Google Scholar]
- Pantelis C, Velakoulis D, McGorry PD, Wood SJ, Suckling J, Phillips LJ, Yung AR, Bullmore ET, Brewer W, Soulsby B, Desmond P, McGuire PK. Neuroanatomical abnormalities before and after onset of psychosis: A cross-sectional and longitudinal MRI comparison. Lancet. 2003;361:281–288. doi: 10.1016/S0140-6736(03)12323-9. [DOI] [PubMed] [Google Scholar]
- Pasternak JF, Woolsey TA. On the selectivity of the Golgi-Cox method. J Comp Neurol. 1975;160:307–312. doi: 10.1002/cne.901600304. [DOI] [PubMed] [Google Scholar]
- Pedersen CB, Mortensen PB. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry. 2001;58:1039–1046. doi: 10.1001/archpsyc.58.11.1039. [DOI] [PubMed] [Google Scholar]
- Penzes P, Cahill ME, Jones KA, VanLeeuwen JE, Woolfrey KM. Dendritic spine pathology in neuropsychiatric disorders. Nat Neurosci. 2011;14:285–293. doi: 10.1038/nn.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penzes P, Johnson RC, Sattler R, Zhang X, Huganir RL, Kambampati V, Mains RE, Eipper BA. The neuronal Rho-GEF Kalirin-7 interacts with PDZ domain-containing proteins and regulates dendritic morphogenesis. Neuron. 2001;29:229–242. doi: 10.1016/s0896-6273(01)00193-3. [DOI] [PubMed] [Google Scholar]
- Petanjek Z, Judas M, Simic G, Rasin MR, Uylings HB, Rakic P, Kostovic I. Extraordinary neoteny of synaptic spines in the human prefrontal cortex. Proc Natl Acad Sci U S A. 2011;108:13281–13286. doi: 10.1073/pnas.1105108108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters A. Examining neocortical circuits: some background and facts. J Neurocytol. 2002;31:183–193. doi: 10.1023/a:1024157522651. [DOI] [PubMed] [Google Scholar]
- Pierri JN, Volk CLE, Auh S, Sampson A, Lewis DA. Decreased somal size of deep layer 3 pyramidal neurons in the prefrontal cortex of subjects with schizophrenia. Arch Gen Psychiatry. 2001;58:466–473. doi: 10.1001/archpsyc.58.5.466. [DOI] [PubMed] [Google Scholar]
- Piskulic D, Olver JS, Norman TR, Maruff P. Behavioural studies of spatial working memory dysfunction in schizophrenia: a quantitative literature review. Psychiatry Res. 2007;150:111–121. doi: 10.1016/j.psychres.2006.03.018. [DOI] [PubMed] [Google Scholar]
- Popken GJ, Bunney WE, Jr., Potkin SG, Jones EG. Subnucleus-specific loss of neurons in medial thalamus of schizophrenics. Proc Natl Acad Sci U S A. 2000;97:9276–9280. doi: 10.1073/pnas.150243397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkowska G, Selemon LD, Goldman-Rakic PS. Neuronal and glial somal size in the prefrontal cortex: A postmortem morphometric study of schizophrenia and Huntington disease. Arch Gen Psychiatry. 1998;55:215–224. doi: 10.1001/archpsyc.55.3.215. [DOI] [PubMed] [Google Scholar]
- Rama P, Linnankoski I, Tanila H, Pertovaara A, Carlson S. Medetomidine, atipamezole, and guanfacine in delayed response performance of aged monkeys. Pharmacol Biochem Behav. 1996;55:415–422. doi: 10.1016/s0091-3057(96)00111-6. [DOI] [PubMed] [Google Scholar]
- Rapoport JL, Giedd JN, Blumenthal J, Hamburger S, Jeffries N, Fernandez T, Nicolson R, Bedwell J, Lenane M, Zijdenbos A, Paus T, Evans A. Progressive cortical change during adolescence in childhood-onset schizophrenia: A longitudinal magnetic resonance imaging study. Arch Gen Psychiatry. 1999;56:649–654. doi: 10.1001/archpsyc.56.7.649. [DOI] [PubMed] [Google Scholar]
- Rapp PR, Morrison JH, Roberts JA. Cyclic estrogen replacement improves cognitive function in aged ovariectomized rhesus monkeys. J Neurosci. 2003;23:5708–5714. doi: 10.1523/JNEUROSCI.23-13-05708.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regenold WT, Phatak P, Marano CM, Sassan A, Conley RR, Kling MA. Elevated cerebrospinal fluid lactate concentrations in patients with bipolar disorder and schizophrenia: implications for the mitochondrial dysfunction hypothesis. Biol Psychiatry. 2009;65:489–494. doi: 10.1016/j.biopsych.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regenold WT, Pratt M, Nekkalapu S, Shapiro PS, Kristian T, Fiskum G. Mitochondrial detachment of hexokinase 1 in mood and psychotic disorders: Implications for brain energy metabolism and neurotrophic signaling. J Psychiatr Res. 2012;46:95–104. doi: 10.1016/j.jpsychires.2011.09.018. [DOI] [PubMed] [Google Scholar]
- Reichenberg A, Caspi A, Harrington H, Houts R, Keefe RS, Murray RM, Poulton R, Moffitt TE. Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study. Am J Psychiatry. 2010;167:160–169. doi: 10.1176/appi.ajp.2009.09040574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren WW, Liu Y, Li BM. Stimulation of alpha(2A)-adrenoceptors promotes the maturation of dendritic spines in cultured neurons of the medial prefrontal cortex. Mol Cell Neurosci. 2011;49:205–216. doi: 10.1016/j.mcn.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Riecher-Rossler A, Kulkarni J. Estrogens and gonadal function in schizophrenia and related psychoses. Curr Top Behav Neurosci. 2011;8:155–171. doi: 10.1007/7854_2010_100. [DOI] [PubMed] [Google Scholar]
- Riecher-Rossler A, Loffler W, Munk-Jorgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195–208. doi: 10.1007/BF02900216. [DOI] [PubMed] [Google Scholar]
- Roberts RC, Conley R, Kung L, Peretti FJ, Chute DJ. Reduced striatal spine size in schizophrenia: A postmortem ultrastructural study. NeuroReport. 1996;7:1214–1218. doi: 10.1097/00001756-199604260-00024. [DOI] [PubMed] [Google Scholar]
- Roberts RC, Gaither LA, Gao XM, Kashyap SM, Tamminga CA. Ultrastructural correlates of haloperidol-induced oral dyskinesias in rat striatum. Synapse. 1995;20:234–243. doi: 10.1002/syn.890200307. [DOI] [PubMed] [Google Scholar]
- Roberts RC, Roche JK, Conley RR. Synaptic differences in the patch matrix compartments of subjects with schizophrenia: a postmortem ultrastructural study of the striatum. Neurobiol Dis. 2005a;20:324–335. doi: 10.1016/j.nbd.2005.03.015. [DOI] [PubMed] [Google Scholar]
- Roberts RC, Roche JK, Conley RR. Synaptic differences in the postmortem striatum of subjects with schizophrenia: a stereological ultrastructural analysis. Synapse. 2005b;56:185–197. doi: 10.1002/syn.20144. [DOI] [PubMed] [Google Scholar]
- Roberts RC, Roche JK, Conley RR. Differential synaptic changes in the striatum of subjects with undifferentiated versus paranoid schizophrenia. Synapse. 2008;62:616–627. doi: 10.1002/syn.20534. [DOI] [PubMed] [Google Scholar]
- Rosenfeld M, Brenner-Lavie H, Ari SG, Kavushansky A, Ben Shachar D. Perturbation in mitochondrial network dynamics and in complex I dependent cellular respiration in schizophrenia. Biol Psychiatry. 2011;69:980–988. doi: 10.1016/j.biopsych.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Rosoklija G, Toomayan G, Ellis SP, Keilp J, Mann JJ, Latov N, Hays AP, Dwork AJ. Structural abnormalities of subicular dendrites in subjects with schizophrenia and mood disorders: Preliminary findings. Arch Gen Psychiatry. 2000;57:349–356. doi: 10.1001/archpsyc.57.4.349. [DOI] [PubMed] [Google Scholar]
- Rubino T, Realini N, Braida D, Guidi S, Capurro V, Vigano D, Guidali C, Pinter M, Sala M, Bartesaghi R, Parolaro D. Changes in hippocampal morphology and neuroplasticity induced by adolescent THC treatment are associated with cognitive impairment in adulthood. Hippocampus. 2009;19:763–772. doi: 10.1002/hipo.20554. [DOI] [PubMed] [Google Scholar]
- Sa SI, Pereira PA, Paula-Barbosa MM, Madeira MD. Role of neural afferents as mediators of estrogen effects on the hypothalamic ventromedial nucleus. Brain Res. 2010;1366:60–70. doi: 10.1016/j.brainres.2010.10.043. [DOI] [PubMed] [Google Scholar]
- Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salisbury DF, Kuroki N, Kasai K, Shenton ME, McCarley RW. Progressive and interrelated functional and structural evidence of post-onset brain reduction in schizophrenia. Arch Gen Psychiatry. 2007;64:521–529. doi: 10.1001/archpsyc.64.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott EK, Reuter JE, Luo L. Small GTPase Cdc42 is required for multiple aspects of dendritic morphogenesis. J Neurosci. 2003;23:3118–3123. doi: 10.1523/JNEUROSCI.23-08-03118.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal M. Dendritic spines and long-term plasticity. Nat Rev Neurosci. 2005;6:277–284. doi: 10.1038/nrn1649. [DOI] [PubMed] [Google Scholar]
- Seidman LJ, Giuliano AJ, Meyer EC, Addington J, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Tsuang MT, Walker EF, Woods SW, Bearden CE, Christensen BK, Hawkins K, Heaton R, Keefe RS, Heinssen R, Cornblatt BA. Neuropsychology of the prodrome to psychosis in the NAPLS consortium: relationship to family history and conversion to psychosis. Arch Gen Psychiatry. 2010;67:578–588. doi: 10.1001/archgenpsychiatry.2010.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selemon LD, Goldman-Rakic PS. The reduced neuropil hypothesis: A circuit based model of schizophrenia. Biol Psychiatry. 1999;45:17–25. doi: 10.1016/s0006-3223(98)00281-9. [DOI] [PubMed] [Google Scholar]
- Selemon LD, Mrzljak J, Kleinman JE, Herman MM, Goldman-Rakic PS. Regional specificity in the neuropathologic substrates of schizophrenia: a morphometric analysis of Broca's area 44 and area 9. Arch Gen Psychiatry. 2003;60:69–77. doi: 10.1001/archpsyc.60.1.69. [DOI] [PubMed] [Google Scholar]
- Selemon LD, Rajkowska G, Goldman-Rakic PS. Abnormally high neuronal density in the schizophrenic cortex: A morphometric analysis of prefrontal area 9 and occipital area 17. Arch Gen Psychiatry. 1995;52:805–818. doi: 10.1001/archpsyc.1995.03950220015005. [DOI] [PubMed] [Google Scholar]
- Selemon LD, Rajkowska G, Goldman-Rakic PS. Elevated neuronal density in prefrontal area 46 in brains from schizophrenic patients: Application of a three-dimensional, stereologic counting method. J Comp Neurol. 1998;392:402–412. [PubMed] [Google Scholar]
- Shao L, Martin MV, Watson SJ, Schatzberg A, Akil H, Myers RM, Jones EG, Bunney WE, Vawter MP. Mitochondrial involvement in psychiatric disorders. Ann Med. 2008;40:281–295. doi: 10.1080/07853890801923753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva-Gomez AB, Rojas D, Juarez I, Flores G. Decreased dendritic spine density on prefrontal cortical and hippocampal pyramidal neurons in postweaning social isolation rats. Brain Res. 2003;983:128–136. doi: 10.1016/s0006-8993(03)03042-7. [DOI] [PubMed] [Google Scholar]
- Simon TJ, Ding L, Bish JP, McDonald-McGinn DM, Zackai EH, Gee J. Volumetric, connective, and morphologic changes in the brains of children with chromosome 22q11.2 deletion syndrome: an integrative study. NeuroImage. 2005;25:169–180. doi: 10.1016/j.neuroimage.2004.11.018. [DOI] [PubMed] [Google Scholar]
- Smart FM, Halpain S. Regulation of dendritic spine stability. Hippocampus. 2000;10:542–554. doi: 10.1002/1098-1063(2000)10:5<542::AID-HIPO4>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Sporn AL, Greenstein DK, Gogtay N, Jeffries NO, Lenane M, Gochman P, Clasen LS, Blumenthal J, Giedd JN, Rapoport JL. Progressive brain volume loss during adolescence in childhood-onset schizophrenia. Am J Psychiatry. 2003;160:2181–2189. doi: 10.1176/appi.ajp.160.12.2181. [DOI] [PubMed] [Google Scholar]
- Steen RG, Mull C, McClure R, Hamer RM, Lieberman JA. Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies. Br J Psychiatry. 2006;188:510–518. doi: 10.1192/bjp.188.6.510. [DOI] [PubMed] [Google Scholar]
- Sun D, Phillips L, Velakoulis D, Yung A, McGorry PD, Wood SJ, Van Erp TG, Thompson PM, Toga AW, Cannon TD, Pantelis C. Progressive brain structural changes mapped as psychosis develops in 'at risk' individuals. Schizophr Res. 2009;108:85–92. doi: 10.1016/j.schres.2008.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Supprian T, Ulmar G, Bauer M, Schuler M, Puschel K, Retz-Junginger P, Schmitt HP, Heinsen H. Cerebellar vermis area in schizophrenic patients - a post-mortem study. Schizophr Res. 2000;42:19–28. doi: 10.1016/s0920-9964(99)00103-6. [DOI] [PubMed] [Google Scholar]
- Sweet RA, Bergen SE, Sun Z, Marcsisin MJ, Sampson AR, Lewis DA. Anatomical evidence of impaired feedforward auditory processing in schizophrenia. Biol Psychiatry. 2007;61:854–864. doi: 10.1016/j.biopsych.2006.07.033. [DOI] [PubMed] [Google Scholar]
- Sweet RA, Bergen SE, Sun Z, Sampson AR, Pierri JN, Lewis DA. Pyramidal cell size reduction in schizophrenia: Evidence for involvement of auditory feedforward circuits. Biol Psychiatry. 2004;55:1128–1137. doi: 10.1016/j.biopsych.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Sweet RA, Henteleff RA, Zhang W, Sampson AR, Lewis DA. Reduced dendritic spine density in auditory cortex of subjects with schizophrenia. Neuropsychopharm. 2009;34:374–389. doi: 10.1038/npp.2008.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet RA, Pierri JN, Auh S, Sampson AR, Lewis DA. Reduced pyramidal cell somal volume in auditory association cortex of subjects with schizophrenia. Neuropsychopharm. 2003;28:599–609. doi: 10.1038/sj.npp.1300120. [DOI] [PubMed] [Google Scholar]
- Tada T, Sheng M. Molecular mechanisms of dendritic spine morphogenesis. Curr Opin Neurobiol. 2006;16:95–101. doi: 10.1016/j.conb.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Takahashi T, Wood SJ, Yung AR, Soulsby B, McGorry PD, Suzuki M, Kawasaki Y, Phillips LJ, Velakoulis D, Pantelis C. Progressive gray matter reduction of the superior temporal gyrus during transition to psychosis. Arch Gen Psychiatry. 2009;66:366–376. doi: 10.1001/archgenpsychiatry.2009.12. [DOI] [PubMed] [Google Scholar]
- Tamminga CA, Stan AD, Wagner AD. The hippocampal formation in schizophrenia. Am J Psychiatry. 2010;167:1178–1193. doi: 10.1176/appi.ajp.2010.09081187. [DOI] [PubMed] [Google Scholar]
- Tan GM, Arnone D, McIntosh AM, Ebmeier KP. Meta-analysis of magnetic resonance imaging studies in chromosome 22q11.2 deletion syndrome (velocardiofacial syndrome) Schizophr Res. 2009;115:173–181. doi: 10.1016/j.schres.2009.09.010. [DOI] [PubMed] [Google Scholar]
- Tang Y, Janssen WG, Hao J, Roberts JA, McKay H, Lasley B, Allen PB, Greengard P, Rapp PR, Kordower JH, Hof PR, Morrison JH. Estrogen replacement increases spinophilin-immunoreactive spine number in the prefrontal cortex of female rhesus monkeys. Cereb Cortex. 2004;14:215–223. doi: 10.1093/cercor/bhg121. [DOI] [PubMed] [Google Scholar]
- Trachtenberg JT, Chen BE, Knott GW, Feng G, Sanes JR, Welker E, Svoboda K. Long-term in vivo imaging of experience-dependent synaptic plasticity in adult cortex. Nature. 2002;420:788–794. doi: 10.1038/nature01273. [DOI] [PubMed] [Google Scholar]
- Tsai SY, Hayashi T, Harvey BK, Wang Y, Wu WW, Shen RF, Zhang Y, Becker KG, Hoffer BJ, Su TP. Sigma-1 receptors regulate hippocampal dendritic spine formation via a free radical-sensitive mechanism involving Rac1xGTP pathway. Proc Natl Acad Sci U S A. 2009;106:22468–22473. doi: 10.1073/pnas.0909089106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlhaas PJ, Haenschel C, Nikolic D, Singer W. The role of oscillations and synchrony in cortical networks and their putative relevance for the pathophysiology of schizophrenia. Schizophr Bull. 2008;34:927–943. doi: 10.1093/schbul/sbn062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usall J, Huerta-Ramos E, Iniesta R, Cobo J, Araya S, Roca M, Serrano-Blanco A, Teba F, Ochoa S. Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. J Clin Psychiatry. 2011;72:1552–1557. doi: 10.4088/JCP.10m06610. [DOI] [PubMed] [Google Scholar]
- Vincent SL, McSparren J, Wang RY, Benes FM. Evidence for ultrastructural changes in cortical axodendritic synapses following long-term treatment with haloperidol or clozapine. Neuropsychopharm. 1991;5(3):147–155. [PubMed] [Google Scholar]
- Walsh T, McClellan JM, McCarthy SE, Addington AM, Pierce SB, Cooper GM, Nord AS, Kusenda M, Malhotra D, Bhandari A, Stray SM, Rippey CF, Roccanova P, Makarov V, Lakshmi B, Findling RL, Sikich L, Stromberg T, Merriman B, Gogtay N, Butler P, Eckstrand K, Noory L, Gochman P, Long R, Chen Z, Davis S, Baker C, Eichler EE, Meltzer PS, Nelson SF, Singleton AB, Lee MK, Rapoport JL, King MC, Sebat J. Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science. 2008;320:539–543. doi: 10.1126/science.1155174. [DOI] [PubMed] [Google Scholar]
- Wang HD, Deutch AY. Dopamine depletion of the prefrontal cortex induces dendritic spine loss: reversal by atypical antipsychotic drug treatment. Neuropsychopharm. 2008;33:1276–1286. doi: 10.1038/sj.npp.1301521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang HD, Stanwood GD, Grandy DK, Deutch AY. Dystrophic dendrites in prefrontal cortical pyramidal cells of dopamine D1 and D2 but not D4 receptor knockout mice. Brain Res. 2009a;1300:58–64. doi: 10.1016/j.brainres.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Gamo NJ, Yang Y, Jin LE, Wang XJ, Laubach M, Mazer JA, Lee D, Arnsten AF. Neuronal basis of age-related working memory decline. Nature. 2011;476:210–213. doi: 10.1038/nature10243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Su B, Lee HG, Li X, Perry G, Smith MA, Zhu X. Impaired balance of mitochondrial fission and fusion in Alzheimer's disease. J Neurosci. 2009b;29:9090–9103. doi: 10.1523/JNEUROSCI.1357-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washizuka S, Kametani M, Sasaki T, Tochigi M, Umekage T, Kohda K, Kato T. Association of mitochondrial complex I subunit gene NDUFV2 at 18p11 with schizophrenia in the Japanese population. Am J Med Genet B Neuropsychiatr Genet. 2006;141B:301–304. doi: 10.1002/ajmg.b.30285. [DOI] [PubMed] [Google Scholar]
- Weickert CS, Straub RE, McClintock BW, Matsumoto M, Hashimoto R, Hyde TM, Herman MM, Weinberger DR, Kleinman JE. Human dysbindin (DTNBP1) gene expression in normal brain and in schizophrenic prefrontal cortex and midbrain. Arch Gen Psychiatry. 2004;61:544–555. doi: 10.1001/archpsyc.61.6.544. [DOI] [PubMed] [Google Scholar]
- Williams RS, Ferrante RJ, Caviness VS., Jr. The Golgi rapid method in clinical neuropathology: The morphologic consequences of suboptimal fixation. J Neuropatho Exp Neurol. 1978;37:13–33. doi: 10.1097/00005072-197801000-00002. [DOI] [PubMed] [Google Scholar]
- Wilson CJ. GABAergic inhibition in the neostriatum. Prog Brain Res. 2007;160:91–110. doi: 10.1016/S0079-6123(06)60006-X. [DOI] [PubMed] [Google Scholar]
- Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66:1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]
- Xie Z, Cahill ME, Penzes P. Kalirin loss results in cortical morphological alterations. Mol Cell Neurosci. 2010;43:81–89. doi: 10.1016/j.mcn.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida T, McCarley RW, Nakamura M, Lee K, Koo MS, Bouix S, Salisbury DF, Morra L, Shenton ME, Niznikiewicz MA. A prospective longitudinal volumetric MRI study of superior temporal gyrus gray matter and amygdala-hippocampal complex in chronic schizophrenia. Schizophr Res. 2009;113:84–94. doi: 10.1016/j.schres.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young KA, Holcomb LA, Yazdani U, Hicks PB, German DC. Elevated neuron number in the limbic thalamus in major depression. Am J Psychiatry. 2004;161:1270–1277. doi: 10.1176/appi.ajp.161.7.1270. [DOI] [PubMed] [Google Scholar]
- Young KA, Manaye KF, Liang C-L, Hicks PB, German DC. Reduced number of mediodorsal and anterior thalamic neurons in schizophrenia. Biol Psychiatry. 2000;47:944–953. doi: 10.1016/s0006-3223(00)00826-x. [DOI] [PubMed] [Google Scholar]
- Yuste R. Dendritic spines and distributed circuits. Neuron. 2011;71:772–781. doi: 10.1016/j.neuron.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuste R, Bonhoeffer T. Morphological changes in dendritic spines associated with long-term synaptic plasticity. Annu Rev Neurosci. 2001;24:1071–1089. doi: 10.1146/annurev.neuro.24.1.1071. [DOI] [PubMed] [Google Scholar]
- Zhang W, Benson DL. Development and molecular organization of dendritic spines and their synapses. Hippocampus. 2000;10:512–526. doi: 10.1002/1098-1063(2000)10:5<512::AID-HIPO2>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]