Abstract
The cannabinoids comprise three major classes of substances, including compounds derived from the cannabis plant (e.g. Δ9-tetrahydrocannabinol and the chemically related substances CP55940 and HU210), endogenously formed (e.g. anandamide) and synthetic compounds (e.g. WIN55212-2). Beyond their psychotropic effects, cannabinoids have complex effects on blood pressure, including biphasic changes of Δ9-tetrahydrocannabinol and WIN55212-2 and an even triphasic effect of anandamide. The differing pattern of blood pressure changes displayed by the three types of compounds is not really surprising since, although they share an agonistic effect at cannabinoid CB1 and CB2 receptors, some compounds have additional effects. In particular, anandamide is known for its pleiotropic effects, and there is overwhelming evidence that anandamide influences blood pressure via (i) CB1 receptors, (ii) TRPV1 receptors, (iii) endothelial cannabinoid receptors and (iv) degradation products. This review is dedicated to the description of the effects of externally added cannabinoids on cardiovascular parameters in vivo. First, the cardiovascular effects of cannabinoids in anaesthetized animals will be highlighted since most data have been generated in experiments of that type. The text will follow the three phases of anandamide on blood pressure, and we will check to which extent cardiovascular changes elicited by other cannabinoids show overlap with those effects or differ. The second part will be dedicated to the cardiovascular effects of the cannabinoids in conscious animals. In the third part, cardiovascular effects in humans will be discussed, and similarities and differences with respect to the data from animals will be examined.
Keywords: blood pressure response, anandamide, Δ9-tetrahydrocannabinol, WIN55212-2, anaesthetized rodents, conscious rat, humans, cannabinoid CB1 receptor, vanilloid TRPV1 receptor, endothelial cannabinoid receptor
Introduction
Cannabis preparations have been used for recreational and therapeutic purposes for thousands of years, but details of the mechanisms of action have been disclosed during the recent 20 years only. Cannabis preparations or, stricto sensu, some of their constituents activate an endogenous system of the body, the so-called endocannabinoid system, which is activated also by endogenously formed compounds, the so-called endocannabinoids that chemically differ from the plant-derived cannabinoids. The endocannabinoid system plays a role under physiological and many pathophysiological conditions not only in the brain but also in peripheral tissues. Consequently, it has not only to do with psychotropic but also with many other effects including cardiovascular function. Thus, endocannabinoids are implicated in the pathogenesis of hypertension, hypotension associated with haemorrhagic, endotoxic and cardiogenic shock and with advanced liver cirrhosis or in the control of atherosclerosis (for review, see Pacher et al., 2005; Malinowska et al., 2008; Bátkai and Pacher, 2009). The possibility has even been considered that diseases of the cardiovascular system might be treated by targeting the endocannabinoid system (Pacher et al., 2006).
In the present review, the effects of several types of cannabinoids on cardiovascular parameters in vivo will be described. The review is dedicated to the description of haemodynamic effects of externally added cannabinoids, and so the involvement of the endocannabinoid system in the pathogenesis of many diseases of the cardiovascular system will not be touched here. However, the effects of cannabinoids in animals or humans with hypertension will be covered. First, the cardiovascular effects of cannabinoids in anaesthetized animals will be highlighted since most data have been generated in experiments of that type. The text will follow the three phases of the endocannabinoid arachidonoylethanolamide (anandamide, AEA; for chemical structure, see Figure 1) on blood pressure (BP) in anaesthetized rodents (e.g. Varga et al., 1995; Malinowska et al., 2001a; Pacher et al., 2004), and we will check to which extent cardiovascular effects elicited by other cannabinoids show overlap with those effects or differ. The second part will be dedicated to the cardiovascular effects of the cannabinoids in conscious animals. In the third part, cardiovascular effects in humans will be discussed, and similarities and differences with respect to the data from animals will be examined. The review will be preceded by a very brief overview about the cannabinoids and the major constituents of the endocannabinoid system. For detailed information related to the latter two topics, the reader is referred to excellent reviews; only some of them have been quoted in the subsequent two paragraphs. Drug/molecular target nomenclature conforms to the British Journal of Pharmacology's Guide to Receptors and Channels (Alexander et al., 2011).
Figure 1.
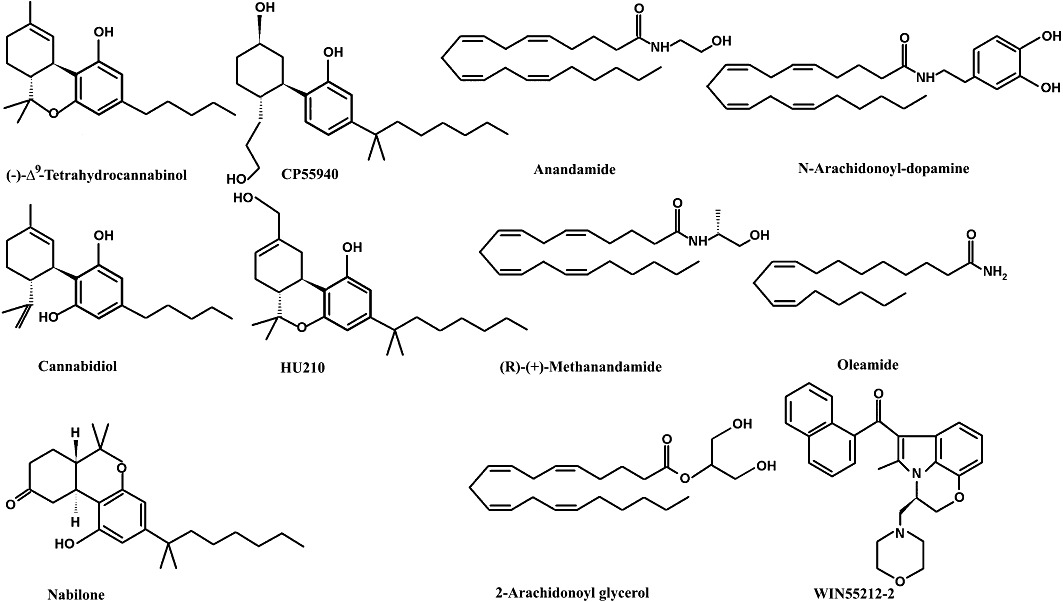
Chemical structures of cannabinoids.
The term ‘cannabinoids’, which originally referred to a series of chemically closely related compounds occurring in the cannabis plant Cannabis sativa, var. indica, is now used rather in a functional sense and comprises substances of different chemical structure activating the endocannabinoid system (Pertwee, 2005; Figure 1). In the class of compounds isolated from the cannabis plant, Δ9-tetrahydrocannabinol (Δ9-THC) is the most important one. HU210 and CP55940, chemically modified from Δ9-THC, may also be entered into this class; they do not play a role in humans but are frequently used for scientific purposes (Pertwee, 2005). Cannabidiol, which occurs in the cannabis plant in a similarly high concentration as Δ9-THC, is devoid of psychotropic effects (Russo and Guy, 2006; Izzo et al., 2009). The second class of cannabinoids are the endogenously formed endocannabinoids, that is derivatives from arachidonic acid synthetized by the cell membrane on demand. The aforementioned AEA and 2-arachidonoyl glycerol (2-AG) are the two compounds that have so far attracted most attention (Di Marzo et al., 2005; Howlett et al., 2011). WIN55212-2 belongs to a third class of cannabinoids, which are chemically unrelated to either of the aforementioned classes; the compound is potent and less lipophilic compared with the above compounds and is frequently used for scientific purposes (Pertwee, 2005).
The major molecular targets for the effect of the cannabinoids as far as they play a role for the cardiovascular system are (i) cannabinoid receptors (primarily CB1), (ii) the vanilloid transient receptor potential (TRP) channels of V1 type (TRPV1) receptor and (iii) the so-called endothelial cannabinoid receptor. Only AEA activates each of those entities, whereas the other cannabinoids activate only part of them (Pertwee et al., 2010). The CB1 receptor, which is Gi/o-protein-coupled and serves as a presynaptic inhibitory receptor, occurs in very high density in the brain and is the substrate of the psychotropic effects of cannabinoids; it is expressed in low density also in peripheral tissues (Pertwee, 2005; Pacher et al., 2006). Unlike the CB1 receptor, the TRPV1 receptor is a ligand-gated ion channel usually activated by extreme physical alterations (e.g. low pH value or high temperature) but also by high concentrations of AEA (Gunthorpe et al., 2002). The molecular properties of the endothelial cannabinoid receptor, sometimes and herein termed CBx receptor, have not yet been disclosed; its activation leads to dilatation of some vessels, e.g. of the mesenterial arterial bed (Offertáler et al., 2003; Kozłowska et al., 2007, 2008). Moreover, in some instances, the endocannabinoids act indirectly via their degradation products (Kozłowska et al., 2008 and references therein). AEA and 2-AG are degraded to arachidonic acid mainly by fatty acid amide hydrolase (FAAH) and monoacylglycerole lipase (MAGL), respectively, and new compounds (e.g. prostanoids) can be formed from arachidonic acid. Investigation of the effects mediated via the aforementioned receptors is facilitated by the availability of CB1 (Valverde et al., 2005) and TRPV1 receptor knockout mice (Caterina et al., 2000). Moreover, antagonists are available comprising rimonabant and AM251 for the CB1 (Pertwee, 2005), capsazepine for the TRPV1 (Gunthorpe et al., 2002) and O-1918 for the CBx receptor (Offertáler et al., 2003). The FAAH inhibitor URB597 has to be mentioned here as well (Kathuria et al., 2003).
Influence of cannabinoids on cardiovascular parameters in anaesthetized animals
In rats anaesthetized with urethane (Varga et al., 1995; Lake et al., 1997a,b; Malinowska et al., 2001a, 2010; Kwolek et al., 2005; Zakrzeska et al., 2010) or in mice anaesthetized with pentobarbitone (Pacher et al., 2004, 2005) rapid i.v. injection of AEA (1–57 µmol·kg−1) induces typical triphasic changes in cardiovascular parameters (Figure 2; Table 1). The initial phase I is characterized by a rapid and pronounced bradycardia and a transient drop in BP associated with a decrease in cardiac contractility and an increase in total peripheral resistance. The subsequent phase II consists of a brief pressor response (lasting for about 30–60 s) associated with an increase in cardiac contractility and blood flow in the mesenteric and renal vascular beds. In the final phase III, a more prolonged (lasting up to 10 min), marked decrease in BP accompanied by a fall in mesenteric and renal blood flow, a marked decrease in cardiac contractility and a slight decrease in heart rate (HR) and total peripheral resistance occurs.
Figure 2.
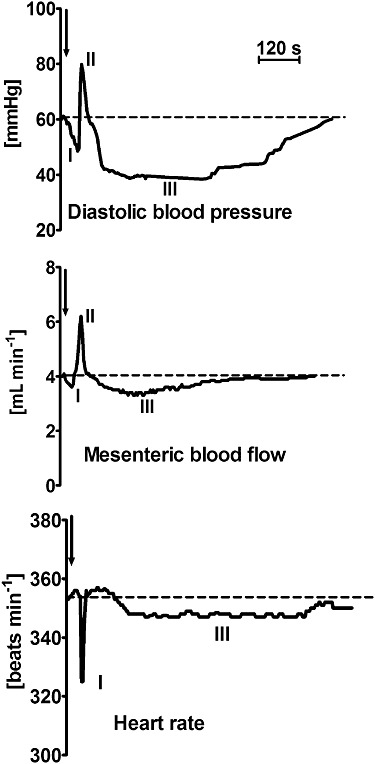
Typical traces showing the changes in diastolic blood pressure, mesenteric blood flow and heart rate induced by i.v. injection of anandamide (3 µmol·kg−1) in a rat anaesthetized with urethane. Arrows indicate drug application. From Zakrzeska et al. (2010) (modified).
Table 1.
Influence of cannabinoids on selected parameters of the animal cardiovascular system
| Species | Agonist | Doses (µmol·kg−1) | Route of administration | Anaesthesia | Effects | Examples of the literature |
|---|---|---|---|---|---|---|
| Rat | AEA | 0.9–58 | i.v. | urethane | I: ↓BP, ↓HR; II: ↑BP; III: ↓BP, ↓HR | Lake et al. (1997a); Malinowska et al. (2001a) |
| See Figure 1 | ||||||
| Mouse | AEA | 58 | i.v. | pentobarbital | I: ↓BP, ↓HR; ↓cardiac contractility; ↑TPR; | Pacher et al. (2004) |
| II: ↑BP; ↑cardiac contractility; | ||||||
| III: ↓BP, ↓HR, ↓cardiac contractility; ↓TPR | ||||||
| Rat | MethAEA | 0.03–3 | i.v. | urethane | I: ↓BP, ↓HR; II: ↑BP; III: ↓BP, ↓HR | Malinowska et al. (2001a) |
| Rat | THC | 0.03–32 | i.v. | urethane | II: ↑BP; III: ↓BP, ↓HR | Lake et al. (1997a) |
| Rat | WIN | 0.02–19 | i.v. | urethane | ↓BP, ↓HR, ↓[NAdr] | Lake et al. (1997a); Niederhoffer et al. (2003) |
| CP | 0.003–2.7 | ↓BP, ↓HR, ↓[NAdr] | ||||
| HU210 | 0.0008–0.8 | ↓BP, ↓HR, ↓[NAdr] | ||||
| Rat | HU210 | 0.03–2.6 | i.v. | pentobarbital | ↓BP, ↓HR | Vidrio et al. (1996) |
| Rat | 2-AG | 2.6; 7.9 | i.v. | urethane | ↓BP, ↑HR | Varga et al. (1998) |
| Mouse | 2-AG | 26 | i.v. | pentobarbital | ↓BP, ↑HR | Járai et al. (2000) |
| Rat | NADA | 2.3–23 | i.v. | conscious | I. ↓BP, II. ↑BP, III. ↓BP, ↑HR | Wang and Wang (2007) |
| Rat | AEA | 0.2–8.6 | i.v. | conscious | ↑BP, ↓HR, vasoconstriction in renal and mesenteric and vasodilatation in hindquarters vascular bed | Gardiner et al. (2002a, 2009) |
| MethAEA | 8.3 | |||||
| Rat | WIN | 0.3 | i.v. | conscious | ↑BP, ↓HR, vasoconstriction in renal and mesenteric and vasodilatation in hindquarters vascular bed | Gardiner et al. (2002b); O'Sullivan et al. (2007) |
| HU210 | 0.3 | |||||
| THC | 3.2 | |||||
| Monkey | THC | 1.6 | i.v. | conscious | ↑HR, ↓BP | Fredericks et al. (1981) |
| Rat | oleamide | 35 and 71 | i.p. | conscious | No changes in BP and HR | Huitrón-Reséndiz et al. (2001) |
| Rat | THC | 1–95 | i.a. | urethane | ↑perfusion pressure in the hindquarters | Adams et al. (1976) |
| Rat | AEA | 86–863* | i.a. | urethane | ↓BP, ↑ventilation | Smith and McQueen (2001) |
| Rat | AEA | 2900* | i.a. | decerebrate | ↑BP | Williams et al. (2008) |
| Rat | AEA | 50 and 100* | i.t. | urethane | ↓BP | García et al. (2003; 2009) |
| MethAEA | 50 and 100* | ↓BP | ||||
| WIN | 20* | ↓BP | ||||
| NADA | 50 and 100* | ↓BP | ||||
| Rat | AEA | 30–100* | i.c.v. | urethane | ↑BP but only in the presence of AM251 and ruthenium red | Malinowska et al. (2010) |
| Rat | WIN | 0.06* | i.c. | urethane | ↑BP, ↑[NAdr], ↓HR | Pfitzer et al. (2004) |
| Rabbit | WIN | 0.002 and 0.020* | i.c. | conscious | ↑RSNA, ↑[NAdr], ↑BP (only the highest doses) and ↓HR | Niederhoffer and Szabo (2000) |
| CP | 0.003 and 0.026* | |||||
| Rat | AEA | 0.0017* | PAG | pentobarbital | ↑BP, ↑RSNA | Dean (2011) |
| Rat | CBD | 60* | BNST | conscious | ↑baroreflex-induced bradycardia | Alves et al. (2010) |
| Rat | WIN | 1.9 and 9.6* | NTS | urethane | No changes in BP, HR and [NAdr] | Niederhoffer et al. (2003) |
| Dog | WIN | 0.00125–0.0015* | NTS | α-chloralose + urethane | No changes in BP and baroreflex sensitivity | Rademacher et al. (2003) |
| Rat | AEA | 0.0035* | NTS | pentobarbital | prolongation of baroreflex inhibition of RSNA | Brozoski et al. (2009) |
| Rat | AEA | 11.5 | i.v. | urethane | ↑activity of barosensitive neurons in the RVLM | Varga et al. (1996) |
| Rat | WIN | 1.9 and 9.6* | RVLM | urethane | ↓BP (slight), ↓HR (slight), no changes in [NAdr] | Niederhoffer et al. (2003) |
| Rat | WIN | 0.00005–0.0005* | RVLM | urethane | ↑RSNA, ↑BP; no changes in HR | Padley et al. (2003) |
| HU210 | 0.0005* | ↑RSNA, ↑BP; no changes in HR |
nmol per rat.
BNST, bed nucleus of the stria terminalis; CBD, cannabidiol; CP, CP55940; [NAdr], plasma noradrenaline concentration; TPR, total peripheral resistance; WIN, WIN55212-2; I–III, phases of cardiovascular changes. Since doses have been given in mg or µg rather than in µmol in many papers, we re-calculated them in µmol or nmol (molecular weights: AEA – 347.5; 2-AG – 378.6; CP – 376.6; HU210 – 386.6; MethAEA – 361.6; NADA – 439.6; oleamide – 281.5; THC – 314.4; WIN – 522.6).
Similar triphasic changes in cardiovascular parameters were also obtained after i.v. administration of methanandamide (MethAEA; a stable analogue of anandamide; for chemical structure, see Figure 1), arguing against the possibility that AEA acts indirectly via its arachidonic acid metabolites (Malinowska et al., 2001a). A triphasic response occurred also after administration of the endovanilloid N-arachidonoyl-dopamine (NADA; for chemical structure, see Figure 1) with the difference that in phase III the decrease in BP was associated with a pronounced increase in HR (Wang and Wang, 2007). Δ9-THC elicited biphasic (phases II and III only) and 2-AG, HU210, CP55940 and WIN55212-2 elicited monophasic cardiovascular responses (phase III only) (Vidrio et al., 1996; Lake et al., 1997a; Niederhoffer et al., 2003; Table 1). The decrease in BP obtained with 2-AG, unlike that obtained with the other three cannabinoids, was associated with an increase in HR (Table 1).
Phase I
The first phase of cardiovascular changes induced by AEA in anaesthetized rodents is mainly a short-lasting bradycardia and hypotension. The following observations clearly prove that this phase is mediated by vanilloid TRPV1 receptors: (i) It was absent in TRPV1−/− mice (Pacher et al., 2004); (ii) it was induced not only by rapid injection of AEA and MethAEA but also by the TRPV1 receptor agonist capsaicin with the following rank order of potencies: capsaicin > MethAEA > AEA (the apparent ED50 that decreased HR by 150 beats·min−1 were 0.013, 0.744 and 7.562 µmol·kg−1, respectively); and (iii) it was blocked by a selective (capsazepine) and non-selective (ruthenium red) TRPV1 receptor antagonist but (iv) not by the CB1 receptor antagonist rimonabant (Smith and McQueen, 2001; Malinowska et al., 2001a; Pacher et al., 2004). The profound drop in cardiac contractility that accompanied the reflex bradycardia and hypotension was also absent in TRPV1−/− mice (Pacher et al., 2004).
Phase I involves the so-called Bezold–Jarisch reflex, which leads to bradycardia plus hypotension (Campagna and Carter, 2003), and can also be induced by the activation of serotonin 5-HT3 receptors, which like the TRPV1 receptors are located on sensory vagal nerves in the heart (Figure 3). This reflex is blocked by atropine, bilateral vagotomy (Varga et al., 1995) and is absent in pithed rats; the latter model offers the opportunity to study drug effects on the peripheral cardiovascular system only (Kwolek et al., 2005; Zakrzeska et al., 2010). Phase I is the most homogeneous and the best explained change. However, it is detected relatively rarely, probably because of two reasons. First, this short-lasting phase is induced by relatively high doses of the agonist; for the apparent ED50 value see above. Such responses can be achieved only by rapid i.v. injection of the agonist (Pacher et al., 2005; also pers. obs.). Second, reflex responses are diminished by pentobarbitone anaesthesia (for literature, see Malinowska et al., 2001a). This explains why phase I occurred in rats anaesthetized with urethane but could be elicited not at all (Kwolek et al., 2005) or only at a high dose of 57 µmol·kg−1 in rats treated with pentobarbitone instead (Pacher et al., 2004, 2005). Phase I is not induced by most of the other cannabinoids including CP55940 and WIN55212-2 since they do not possess affinity towards TRPV1 receptors. The latter two compounds are even known to inhibit the afferent limb of the 5-HT3 receptor-mediated Bezold–Jarisch reflex (Godlewski et al., 2003).
Figure 3.
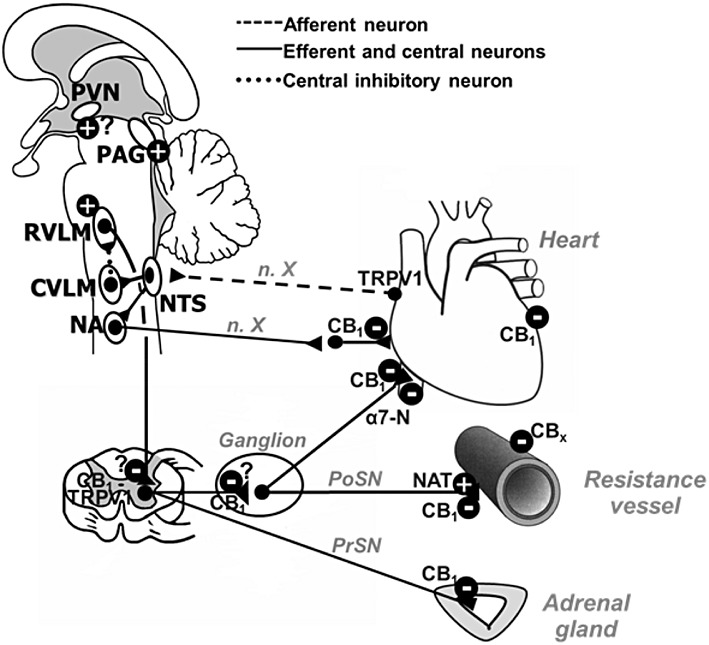
Potential central and peripheral mechanisms involved in the cardiovascular effects of cannabinoids. Plus and minus signs in the CNS mean stimulatory and inhibitory effects on cardiovascular parameters respectively. In the periphery, minus signs mean inhibition of transmitter release (where applicable) or decrease in the tone of heart or vascular muscle; the plus sign means stimulation of the carrier-mediated noradrenaline release. CVLM; caudal ventrolateral medulla; n. X, vagal nerve; NA, nucleus ambiguus; PoSN, postganglionic sympathetic nerve; PrSN, preganglionic sympathetic nerve. Receptors: α7-nicotinic acetylcholine receptor (α7-N), cannabinoid CB1, CB2 and CBx receptors and vanilloid TRPV1 receptor.
It has been postulated that TRPV1 receptors located on cardiac afferents may serve also as a molecular detector of myocardial ischemia to activate cardiac nociceptors (Pan and Chen, 2004) and a sympathoexcitatory reflex (Zahner et al., 2003). We found (Łupiński et al., 2011) that acute myocardial ischemia in rats increased by about 100% the reflex bradycardia elicited (i) by AEA (in a manner sensitive to the TRPV1 receptor antagonist capsazepine) and (ii) the 5-HT3 receptor agonist phenylbiguanide (in a manner sensitive to the 5-HT3 receptor antagonist ondansetron). Moreover, the blockade of TRPV1 receptors increased the ischemic area size and decreased the survival rate after acute myocardial ischaemia. A beneficial cardioprotective influence of these receptors against cardiac injury has been demonstrated in the isolated heart. Moreover, TRPV1 gene deletion increased the mortality of mice 3 days after myocardial infarction (Huang et al., 2009).
Phase II
Phase II of the AEA-induced changes in the cardiovascular parameters of anaesthetized rodents consists of a brief pressor effect. The highest doses of AEA under study (30 and 60 µmol·kg−1) in anaesthetized rats and mice increased BP by about 60% and even 120% of the basal values respectively. The lack of the ability of some CB1 receptor agonists (e.g. WIN55212-2 or CP55940) to induce this phase and the lack of effect of rimonabant on the AEA-stimulated pressor effect argue against the involvement of CB1 receptors (Varga et al., 1995; Lake et al., 1997a,b; Malinowska et al., 2001a; Pacher et al., 2004; Kwolek et al., 2005). Unfortunately, the pressor response to AEA has not been analysed in CB1-/- mice (Járai et al., 1999; Ledent et al., 1999).
The most trivial hypothesis, that is that the pressor effect of AEA can be the simple response to the preceding hypotension (phase I), was excluded because it was not modified by acute surgical transection of the cervical spinal cord, atropine pretreatment (Varga et al., 1995), bilateral vagotomy or pithing (Kwolek et al., 2005), that is measures that inhibit or abolish the reflex loop of the Bezold-Jarisch reflex. In pithed rats, the pressor effect of the highest dose of the endocannabinoid (30 µmol·kg−1) was even higher than in animals with intact spinal cord, suggesting the participation of peripheral mechanism(s). However, the possibility has to be considered that the particularly marked increase in BP is related to an inhibitory effect of pithing on the subsequent depressor phase III.
Phase II may be, at least partially, due to the activation of vanilloid TRPV1 receptors since it was reduced in TRPV1−/− pentobarbital-anaesthetized mice (Pacher et al., 2004; in this case, anandamide at a high dose of 57 µmol·kg−1 was used). Moreover, in urethane-anesthetized rats, it was induced not only by AEA and MethAEA but also by capsaicin, and it was inhibited by a non-selective antagonist of TRPV1 receptors, ruthenium red (Malinowska et al., 2001a; Pacher et al., 2004; Kwolek et al., 2005). Surprisingly, capsazepine, a selective antagonist of these receptors, failed to modify the AEA-stimulated increase in BP (Kwolek et al., 2005). This may result from species differences between mouse and rat or the involvement of another TRPV receptor subtype in the rat (Alexander et al., 2011). In this context, the obvious discrepancy has to be discussed that the TRPV1 (or a closely related) receptor is capable of inducing both phases I and II, which extremely differ with respect to their influence on cardiovascular parameters. A solution of this discrepancy may be that TRPV receptors do not only elicit the Bezold–Jarisch reflex (phase I) but also lead to a sympathoexcitatory response with a brief increase in BP. Such a sympathoexcitatory reflex response was induced by the activation of TRPV1 receptors located on afferent nerve fibres in the rat heart (Zahner et al., 2003).
There may be additional components contributing to phase II. Thus, we found that the L-type calcium channel blocker nifedipine reduced this phase both in intact urethane-anaesthetized and pithed rats. These data point to a calcium-dependent mode of action in the periphery (most probably in blood vessels) and the fact that ruthenium red and pentobarbitone behaved in a similar way as nifedipine are in harmony with this view (Kwolek et al., 2005). In an attempt to further delineate this site of action, we studied the interaction of anandamide with a variety of antagonists in urethane-anaesthetized rats. The results suggest that α1- and α2-adrenoceptors, P2X/P2Y, neuropeptide Y1, serotonin 5-HT2A, vasopressin V1a, endothelin and angiotensin AT1 receptors are not involved in the pressor response to AEA (Kwolek et al., 2005). There is some evidence to suggest that the vasoconstriction in the spleen vascular bed of urethane-anaesthetized rats, which is insensitive to CB1 receptor and sympathetic blockade (Wagner et al., 2001), has the same mechanism.
In the paper by Kwolek et al. (2005) and in a subsequent study (Malinowska et al., 2010), the AEA-stimulated pressor action in urethane-anaesthetized, as opposed to pithed, rats was counteracted by antagonists of NMDA receptors, β2-adrenoceptors and thromboxane A2 (TP) receptors – MK-801, ICI 118551 and sulotroban respectively. These data suggest that central NMDA receptors, β2-adrenoceptors and TP receptors may also play a role in the pressor effect of AEA. In order to further substantiate this hypothesis experiments were carried out in which AEA was administered i.c.v. Since i.c.v. AEA elicited two subsequent short-lived and small hypotensive effects only, the TRPV1 and CB1 receptors (major components of phase I and III) were blocked and under this condition indeed a marked pressor effect was obtained. The latter was counteracted by i.v. administration of an NMDA, β2 or TP receptor antagonist. For the thromboxane A2 system, we could show that AEA and MethAEA are devoid of an affinity at the TP receptor; they may rather lead to an increase in thromboxane A2 formation (Malinowska et al., 2010).
The mechanism of action, the interplay of the three receptors and the anatomical site(s) could not be proven by the study by Malinowska et al. (2010). Anandamide may act as a positive allosteric modulator at NMDA receptors (which in turn have a stimulatory effect on BP); evidence that AEA may act as a positive allosteric modulator is available from the literature (Hampson et al., 1998; Mukhtarov et al., 2005). The NMDA receptor may be the first step followed by TP and β2 receptors and the paraventricular nucleus of the hypothalamus (PVN; an important brain area for BP control) may be the primary site of action.
So far, the vasopressor response to AEA and its metabolically stable analogue has been considered only. However, Δ9-THC and Δ8-THC can also elicit a vasopressor response in urethane-anaesthetized rats (Adams et al., 1976; Lake et al., 1997a) in a manner insensitive to rimonabant (Δ9-THC; Lake et al., 1997a). In the study by Adams et al. (1976), an increase in the perfusion pressure of the hindquarters vascular bed was obtained after i.a. injection of Δ9-THC into the hind limb. This effect was counteracted by the α-adrenoceptor antagonist phentolamine and by pretreatment of the animals with reserpine, suggesting that the vasopressor effect in this case is based on the displacement of noradrenaline from the vascular sympathetic nerve endings by a carrier-mediated release (reverse direction of transport by the neuronal noradrenaline transporter, NAT; Figure 3).
Phase III
The prolonged hypotension induced by AEA (phase III) has been examined most extensively among the three phases so far. Like phase II, it is probably stimulated by complex mechanisms involving different receptors.
The main mechanism responsible is the activation of CB1 receptors since the hypotension was blocked by the CB1 receptor antagonists rimonabant or AM251 (Varga et al., 1995, 1996; Vidrio et al., 1996; Lake et al., 1997a; Malinowska et al., 2001a; Kwolek et al., 2005; Zakrzeska et al., 2010) and was absent in CB1−/− mice (Járai et al., 1999; Ledent et al., 1999). In addition, there is a positive correlation between the EC50 values of various cannabinoid receptor agonists in producing hypotensive and bradycardic responses and in their affinity constants for binding to CB1 receptors: HU210 > CP55940 > WIN55212-2 > Δ9-THC > AEA (Lake et al., 1997a).
Almost from the beginning on, the involvement of presynaptically located CB1 receptors in phase III was postulated (Figure 3). In a series on intact and barodenervated urethane-anaesthetized rats, Varga et al. (1996) could exclude a site within the CNS as the target area for AEA. Instead, these receptors are located in the sympathetic nervous system. This is also suggested by a broad body of experiments in pithed animals and in vitro. So CP55940 and WIN55212-2 failed to affect the isoprenaline- or noradrenaline-stimulated tachycardia and pressor response, respectively, excluding postsynaptic sites of action. On the other hand, they inhibited the electrically stimulated increase in BP, HR and/or plasma noradrenaline concentration in pithed rats (Malinowska et al., 1997, 2001b; Niederhoffer et al., 2003) and rabbits (Niederhoffer and Szabo, 1999, 2000; Szabo et al., 2001) in a manner sensitive to rimonabant. Moreover, Δ9-THC, AEA or WIN55212-2 decreased the release of [3H]-noradrenaline from isolated rat (Ishac et al., 1996), guinea pig (Kurz et al., 2008) and human (Molderings et al., 1999; Table 2) atria and from vessels of the guinea-pig (Schultheißet al., 2005). All the above effects were diminished by rimonabant.
Table 2.
Occurrence of components of the endocannabinoid system in human cardiovascular tissues1
| Component | Parameter | Function | Tissue | References |
|---|---|---|---|---|
| AEA | Compound | n.d. | V. saphena vascular endothelium | Bilfinger et al. (1998) |
| 2-AG | Compound | n.d. | Aortic smooth muscle and umbilical vein endothelial cells | Sugiura et al. (1998) |
| CB1 receptor | mRNA, protein | n.d. | Left ventricular myocardium | Weis et al. (2010) |
| Function | Inhibiton of NAdr release | Atrial appendages | Molderings et al. (1999) | |
| Protein | Decrease in contractility | Atrium | Bonz et al. (2003) | |
| Function | AEA- and 2-AG-stimulated NO release | Right atrium | Bilfinger et al. (1998); Stefano et al. (2000) | |
| Protein | AEA-stimulated NO release | Internal thoracic artery | Bilfinger et al. (1998) | |
| Function | 2-AG stimulated NO release | V. saphena vascular endothelium | Bilfinger et al. (1998); Stefano et al. (2000) | |
| mRNA | n.d. | Aortic smooth muscle and umbilical vein endothelial cells | Sugiura et al. (1998) | |
| mRNA | n.d. | Hepatic artery | Liu et al. (2000) | |
| Protein | n.d. | Coronary artery smooth muscle cells | Rajesh et al. (2007) | |
| mRNA, protein | n.d. | Cerebromicrovascular endothelial cells | Golech et al. (2004) | |
| CB2 receptor | mRNA, protein | n.d. | Left ventricular myocardium | Weis et al. (2010) |
| Protein | n.d. | Coronary artery smooth muscle cells | Rajesh et al. (2007) | |
| mRNA, protein | n.d. | Cerebromicrovascular endothelial cells | Golech et al. (2004) | |
| CBx receptor | Function | Relaxation | Pulmonary artery | Kozłowska et al. (2007, 2008) |
| TRPV1 receptor | mRNA, protein | n.d. | Cerebromicrovascular endothelial cells | Golech et al. (2004) |
Note that this table also comprises mechanisms of the endocannabinoid system not considered in the rest of this review that is focussing on haemodynamic aspects of cannabinoids. E.g., Rajesh et al. (2007) showed that CB2 receptors regulate vascular smooth muscle proliferation and migration. For some of the entries, a functional effect in vitro and/or in vivo has so far not been shown.
n.d., not determined; NAdr, noradrenaline.
With respect to the location of the presynaptic inhibitory CB1 receptors in the sympathetic nervous system in vivo, several possibilities have to be considered (Figure 3). These receptors are probably located on the postganglionic sympathetic nerve endings since the inhibitory effect mediated via these receptors was detected not only after electrical stimulation of the pre-ganglionic sympathetic nerve fibres in pithed rabbits or rats but also if the post-ganglionic fibres were stimulated electrically (Szabo et al., 2001) or by injection of nicotine (Malinowska et al., 2001b). However, an additional pre-ganglionic localization cannot been excluded. Moreover, presynaptic inhibitory CB1 receptors located on the pre-ganglionic sympathetic nerve fibres projecting to the adrenal medulla may contribute since CP55940 and WIN55212-2 decreased plasma adrenaline release in pithed rabbits and in their isolated adrenal glands in a manner sensitive to rimonabant (Niederhoffer et al., 2001). Presynaptic inhibitory CB1 receptors have also been demonstrated on heart vagal fibres in pithed rabbits (Figure 3; Szabo et al., 2001) but not in pithed rats (Malinowska et al., 2001b). When present, these receptors may limit the extent of bradycardia accompanying phase III since they should functionally counteract the bradycardia elicited by CB1 receptors located on sympathetic nerves and causing inhibition of noradrenaline and/or adrenaline.
In a study on urethane-anaesthetized pithed rats, we found that MethAEA inhibited the nicotine-stimulated tachycardia in a manner not sensitive to the CB1 receptor antagonist AM251 (Baranowska et al., 2008). The data of that study suggest that this inhibitory effect is related to a negative allosteric effect of MethAEA at α7-nicotinic acetylcholine receptors. Thus, a competitive antagonist at the latter receptors, methyllycaconitine, inhibited the nicotine-induced tachycardia to the same extent as MethAEA and the effects of both compounds were not additive. Moreover, it is known from studies in Xenopus oocytes that MethAEA (like anandamide but unlike Δ9-THC, CP55940 and WIN55212-2) allosterically inhibits α7-nicotinic acetylcholine receptors (Oz et al., 2003, 2004). Taken together, both CB1 receptors and an allosteric binding site at α7-nicotinic acetylcholine receptors can be implicated in the presynaptic inhibition of the neurogenic tachycardia of the heart (Figure 3).
Postsynaptic myocardial CB1 receptors (Figure 3) which cause negative inotropy in rats are suggested to be also involved in phase III under certain circumstances (e.g. hypertension or septic shock; for review, see Bátkai and Pacher, 2009). Thus, it has been found in experiments in which a sophisticated pressure-volume analysis system was applied to anaesthetized rodents that the hypotensive effect of AEA could be attributed to a CB1 receptor-mediated decrease in cardiac contractility rather than to a decrease in vascular resistance (Bátkai et al., 2004; Pacher et al., 2005; Bátkai and Pacher, 2009). CB1 receptors leading to a decrease in contractile performance have also been detected in human atrial tissue (Bonz et al., 2003; Table 2).
Importantly, AEA caused a stronger hypotension in anaesthetized spontaneously hypertensive rats (SHR) compared with normotensive animals (Lake et al., 1997a; Bátkai et al., 2004). In addition, the CB1 receptor antagonists rimonabant and AM251 increased BP and cardiac contractility not in normotensive anaesthetized rats but in three models of hypertensive anaesthetized animals (SHR, Dahl salt-sensitive rats, rats with angiotensin II-induced hypertension; Bátkai et al., 2004). Similarly, the FAAH inhibitor AM3506 normalized the elevated BP and cardiac contractility of SHR without affecting those parameters in normotensive rats (Godlewski et al., 2010).
The prolonged hypotension might also be elicited by the activation of cannabinoid CB1 and/or vanilloid TRPV1 receptors in the spinal cord since intrathecal (i.t.) administration (at the level of T12-L1) of WIN55212-2, AEA, MethAEA, NADA and capsaicin to urethane-anaesthetized rats produced hypotensive effects (García et al., 2003; 2009). The above responses were abolished/reduced by nicotinic ganglion blockade with hexamethonium and by the CB1 receptor antagonist rimonabant (against WIN55212-2) and the TRPV1 receptor antagonist capsazepine (against capsaicin). Authors concluded that the fall in BP elicited by AEA (i.t.) is related to the release of calcitonin-gene-related-peptide (CGRP) followed by the release of GABA in the spinal cord since it was mimicked by CGRP and prevented by GABAA as well as GABAB receptor antagonists.
A direct vasodilator effect may also contribute to the prolonged fall in BP elicited by AEA (Zakrzeska et al., 2010). In urethane-anaesthetized rats, the decrease in BP elicited by AEA and MethAEA was counteracted by the antagonists of CBx receptors, cannabidiol and O-1918, suggesting that these receptors contribute to the effect of AEA (Figure 3). The effect of the two antagonists was retained in pithed rats, excluding an interaction in the central nervous system. The possibility that the effect of the two antagonists to some extent involves CB1 receptors can be discarded since cannabidiol and O-1918 at the doses used were ineffective in a CB1 receptor paradigm in pithed rats in the same study. Importantly, vasodilatory CBx receptors have also been demonstrated in human pulmonary arteries (Kozłowska et al., 2007, 2008; Table 2). The possibility that other vasodilator mechanisms activated by cannabinoids and identified in vitro (for review, see Randall et al., 2004; Mendizábal and Adler-Graschinsky, 2007) may come into play has also to be considered (for human vessels, see Table 2). However, so far, in vivo data are not available.
A special comment to 2-AG is necessary here. In contrast to AEA, its cardiovascular effects have been less examined although its level in the brain and in the periphery is higher than that of AEA (e.g. Di Marzo et al., 2005). In addition, the blood level of 2-AG increases more dramatically under various pathological states than that of AEA (e.g. Kase et al., 2008; Weis et al., 2010). Bolus i.v. injection of 2-AG in rats anaesthetized with urethane (Varga et al., 1998) or in mice anaesthetized with pentobarbitone (Járai et al., 2000) induced monophasic changes in cardiovascular parameters, that is, hypotension connected with moderate tachycardia (Table 1). They lasted for about 10 min. Their mechanisms have been examined in detail in mice only (Járai et al., 2000). Thus, the hypotension induced by 2-AG was insensitive to the CB1 receptor antagonist rimonabant and was retained in CB1−/− mice but was significantly diminished by the cyclooxygenase inhibitor indomethacin. On the other hand, the 2-AG-stimulated tachycardia was not modified by indomethacin but reduced by rimonabant (probably related to the rimonabant-elicited increase in basal HR), although it still occurred in CB1−/− mice. Authors concluded that the hypotension is related to rapid degradation of 2-AG to a hypotensive arachidonic acid metabolite, whereas the mechanism of the tachycardia remains unclear (Járai et al., 2000). Interestingly, a metabolically stable ether analogue of 2-AG decreased BP and HR via CB1 receptors; that is, the changes were blocked by rimonabant and absent in CB1−/− mice (Járai et al., 2000). In rats, rimonabant diminished the 2-AG-induced hypotension without affecting the tachycardia (Varga et al., 1998).
In summary, in anaesthetized rodents, the short-lived decrease in HR and BP obtained only with AEA, and its stable analogue MethAEA (phase I) is related to the activation of TRPV1 receptors (Bezold–Jarisch reflex). A short-lived increase in BP (phase II) was obtained with AEA, MethAEA and Δ9-THC only. The mechanism is poorly understood so far, but the involvement of CB1 receptors was excluded. There is good evidence to suggest that there are peripheral and central components. It is even unclear whether AEA (and MethAEA) on the one hand and Δ9-THC on the other share the same mechanism(s). The prolonged hypotension (phase III) obtained with each of the cannabinoids AEA, MethAEA, Δ9-THC, CP55940, HU210 and WIN55212-2 is related to the activation of peripheral CB1 receptors including presynaptic CB1 receptors on the sympathetic nerves innervating the resistance vessels and the heart. CB1 receptors leading to a direct negative inotropic effect and other mechanisms may contribute.
Influence of cannabinoids on cardiovascular parameters in conscious animals
The reason why the cardiovascular effects in anaesthetized and conscious animals are described in separate sections is that there are very marked differences. The most prominent effect in anaesthetized rodents is a prolonged hypotension, whereas in conscious rodents, a pressor response prevails. How can we explain this discrepancy? The most obvious reason is the direct influence of anaesthetic agents on components of the endocannabinoid system. Thus, urethane, but not pentobarbitone, attenuates presynaptic CB1 receptor function (Kurz et al., 2009), which is important for phase III. On the other hand, pentobarbitone, but not urethane, inhibits the pressor effect of AEA (Kwolek et al., 2005), which is important for phase II. In addition, anaesthesia per se affects the resting sympathetic tone, which is higher under the influence of urethane than in unstressed conscious rats (Carruba et al., 1987). It has already been mentioned that phase III is related to the inhibition of the sympathetic tone. Moreover, the complex haemodynamic effects of AEA, that is two hypotensive responses separated by a hypertensive one, causes that a factor that reduces the fall in BP (e.g. the blockade of CB1 receptors) may automatically enhance the preceding pressor effect and vice versa.
As shown in Table 1, in conscious rats AEA, MethAEA, Δ9-THC, WIN55212-2 and HU210 elicited a brief pressor response connected with renal and mesenteric vasoconstriction and hindquarters vasodilatation (Lake et al., 1997b; Gardiner et al., 2001, 2002a,b, 2009; O'Sullivan et al., 2007) (phase II). An initial bradycardia, hypotension and hindquarters vasoconstriction were also observed in response to AEA, especially its higher doses (phase I); however, unlike in anaesthetized rats, none of the five cannabinoids led to a prolonged hypotension (phase III). Mesenteric vasoconstriction and hindquarters vasodilatation of AEA were augmented by the inhibition of FAAH with URB597 but not by COX-2 inhibition with parecoxib (Gardiner et al., 2009); these data suggest that AEA is degraded to a marked extent by FAAH under the experimental conditions chosen, but that formation of prostanoids from the degradation product arachidonic acid does not occur. Surprisingly, the TRPV1 receptor antagonist capsazepine failed to modify the cardiovascular effects of AEA (including phase I) (Gardiner et al., 2009). The authors concluded that either there is no TRPV1 receptor involvement in the cardiovascular actions of AEA, or that the dose of capsazepine was inadequate under the conditions of their experiment.
Rimonabant slightly increased and prolonged the pressor effect of AEA (Lake et al., 1997b), suggesting that this pressor effect is partially masked by peripheral CB1 receptors leading to an inhibition of noradrenaline release. Another CB1 receptor antagonist, AM251, failed to affect the increase in BP and all vasoconstrictor responses induced by i.v. AEA injection (Gardiner et al., 2002a) but diminished all cardiovascular effects of Δ9-THC (O'Sullivan et al., 2007), WIN55212-2 and HU210 (Gardiner et al., 2002b) and, interestingly, also those elicited by MethAEA (Gardiner et al., 2009). The actions of WIN55212-2 were also abolished by the ganglion blocking agent pentolinium pointing to sympathoexcitation as the underlying mechanism (Gardiner et al., 2001). The hindquarters vasodilatation induced by all cannabinoids under study involves β2-adrenoceptors. It has been also demonstrated that none of the cardiovascular effects of AEA was modified by the serotonin 5-HT3 receptor antagonist azasetron (Gardiner et al., 2002a). In contrast to the i.v. injection of AEA, its local i.a. administration in the decerebrate rat model (in the absence of anaesthesia) elicited an increase in BP that involves predominantly CB1 and partially TRPV1 receptors located on group IV primary afferent fibres (Williams et al., 2008; Table 1).
Unlike in conscious normotensive animals, prolonged hypotension and bradycardia (phase III) were elicited in rats made acutely hypertensive by infusion of angiotensin II plus vasopressin by AEA and WIN55212-2 (Ho and Gardiner, 2009) and in SHR by AEA (Lake et al., 1997b) and the new FAAH inhibitor AM3506 (Godlewski et al., 2010). The depressor effects were connected with vasodilatation in the renal, mesenteric and hindquarters vascular beds (Ho and Gardiner, 2009). Rimonabant or AM251 blocked the above cardiovascular responses to AEA (only in SHR; Lake et al., 1997b), WIN55212-2 (Lake et al., 1997b; Ho and Gardiner, 2009) and AM3506 (Godlewski et al., 2010) without affecting those elicited by AEA in acutely hypertensive rats (Ho and Gardiner, 2009). The bradycardic response to Δ9-THC was enhanced by AM251 (O'Sullivan et al., 2007), suggesting that CB1 receptors may be coupled to a positive chronotropic activity, either centrally or directly. Taken together, the data suggest that in conscious rodents phase I involves TRPV1 receptors (although final proof is missing), phase II central CB1 receptors (this mechanism is agonist-specific and is not valid for AEA) and phase III (occurring in animals with an elevated blood pressure only) peripheral CB1 receptors. In addition, non-CB1 receptor-mediated mechanisms may be involved in the cardiovascular effects of AEA both in normotensive and in acutely hypertensive rats since CB1 receptor antagonists failed to block cardiovascular effects of this agonist (see above, Gardiner et al., 2002a; Ho and Gardiner, 2009). Locations of the central CB1 receptors leading to an increase in blood pressure have been examined in a series of studies in which cannabinoids have been administered topically to sites within the brain; these results will be discussed in the next few paragraphs.
Almost all experiments in which cannabinoids were applied centrally support the hypothesis that central mechanisms contribute to phase II (Figure 3, Table 1). In the study by Niederhoffer and Szabo (2000), cannabinoids have been administered into the cisterna magna (i.c.) of conscious rabbits; this procedure allows to examine their effects on cardiovascular centres in the medulla oblongata. I.c. injection of CP55940 and WIN55212-2 elicited a CB1 receptor-dependent sympathoactivation manifested by increases in mean BP, plasma noradrenaline concentration and renal sympathetic nerve activity (RSNA) and by a vagally mediated bradycardia. Since the same pattern of changes has also been found in response to WIN55212-2 in urethane-anaesthetized rats (Pfitzer et al., 2004; for details see Table 1), one can probably exclude the possibility that the sympathoexcitation is related to the state of consciousness rather than to a central site of cannabinoid actions. However, the above effects were accompanied by decreases in the respiratory rate and minute volume and all changes were sensitive to CB1 receptor blockade. Thus, Pfitzer et al. (2004) concluded that the pressor effect of the cannabinoid may result from the activation of cardiovascular centres in the brain stem, but it can also be the response to the respiratory depression.
A key centre in the CNS responsible for the tonical pressor activity of the sympathetic nerve fibres is the rostral ventrolateral medulla (RVLM) (Figure 3). The brief pressor response to AEA i.v. was preceded by a transient rise in the activity of the RVLM and a brief rise in splanchnic sympathetic nerve discharge in urethane-anaesthetized rats (Varga et al., 1996). In addition, the direct microinjection of WIN55212-2 and HU210 into the RVLM increased BP and renal sympathetic nerve activity in a CB1 receptor-dependent manner; CB1 receptor gene expression in the RVLM has also been shown (Padley et al., 2003).
Sympathoexcitation can also result from the activation of the periaqueductal gray (PAG) (Figure 3), a mesencephalic region that has been proposed to play a role in specific cardiovascular changes associated with different emotional behaviours observed during the defense reaction. It has been demonstrated in a recent paper (Dean, 2011) that microinjection of AEA into the defense pathway of the dorsal PAG (dPAG) resulted in an increase in BP and RSNA in a manner sensitive to the CB1 receptor antagonist AM281. In addition, AM281 injected into the dPAG attenuated the increase in BP and RSNA induced by electrical stimulation of the dPAG (Dean, 2011).
CB1 receptors have also been found in the nucleus tractus solitarii (NTS; Brozoski et al., 2009), that is a medullary area where various cardiac sensory afferents terminate including those of the baroreceptor, chemoreceptor and Bezold–Jarisch reflex (Figure 3). In anaesthetized rats (Niederhoffer et al., 2003; Brozoski et al., 2009) and dogs (Rademacher et al., 2003) microinjection of AEA, AM404 (an inhibitor of endocannabinoid transport and probably also of FAAH) or WIN55212-2 into the NTS elicited no effects. However, AEA and AM404 injected into the NTS prolonged the reflex inhibition of the RSNA in a manner sensitive to rimonabant (Brozoski et al., 2009). It is suggested that an acute increase in BP leads to the activation of presynaptic CB1 receptors that alter the release of GABA and hence prolong the baroreflex-related sympathoinhibition (for detailed discussion, see Brozoski et al., 2009).
At the end of this section, two cannabinoids that have so far not been mentioned in this review will be discussed (for their chemical structure, see Figure 1). Oleamide, which possesses affinity both for TRPV1 and CB1 receptors, failed to affect BP and HR in conscious rats at 35 and 71 µmol·kg−1 administered i.p. although it elicited a series of centrally mediated effects, for example locomotor activity (Huitrón-Reséndiz et al., 2001). By contrast, NADA i.v. elicited a triphasic BP response in conscious rats; the BP pattern closely resembles that obtained with AEA in anaesthetized rats, but the prolonged hypotension is accompanied by a tachycardia (Wang and Wang, 2007). The mechanisms involved in the three phases have been disclosed only partially. Interesting enough, on the basis of experiments with capsazepine TRPV1 receptors do not appear to be involved in phase I and II but play a role in phase III. On the other hand, the involvement of CB1 receptors in the hypotension in phase III (and also in the BP responses in phase I and II) was excluded by experiments with rimonabant. The lack of contribution of CB1 receptors to the hypotension in phase III is not so surprising since NADA activates CB1 receptors in higher concentrations only. The TRPV1 receptors involved in phase III act via the release of CGRP, which in turn leads to vasodilatation. This conclusion is based on experiments in which a CGRP receptor antagonist was used and an increase in the plasma level of CGRP was determined. No information is available with respect to the mechanism underlying the tachycardia in phase III. Note that the TRPV1 receptors involved in phase III here act via a local antidromic reflex, whereas those leading to phase I and II in anaesthetized animals involve the CNS.
In summary, when comparing the data obtained on anaesthetized and conscious animals, phase I does not differ markedly. Extreme differences, however, appear with respect to phases II and III. Phase II becomes more prominent for AEA, MethAEA and Δ9-THC and is also obtained with other cannabinoids (HU210, WIN55212-2); this stimulatory phase may be (with the exception of AEA) related to activation of CB1 receptors in the brain. The reason why these receptors do not come into play in anaesthetized rats is so far unclear. Phase III is no longer detectable in conscious rats but re-appears when BP is increased. There is good evidence that this phase is unmasked only when the sympathetic tone is high; anaesthesia is a situation under which a high sympathetic tone occurs.
Influence of cannabinoids on cardiovascular parameters in humans
Cannabinoids exhibit cardiovascular effects also in humans. In this context, one has to take into consideration that the cannabinoids are restricted to cannabis preparations, Δ9-THC and nabilone used for recreational and/or therapeutic purposes and that smoking is the most frequent route of administration. Compounds like AEA, MethAEA, CP55940, HU210 and WIN55212-2 do not play a role. Many components of the endocannabinoid system have also been shown in human tissues but only in few cases their function under in vitro conditions has been demonstrated (Table 2).
One of the well-known acute effects of cannabis preparations including their major psychotropic constituent Δ9-THC (whether delivered orally, i.v. or through smoking) is a rapid and substantial dose-dependent increase in HR. It may be accompanied by a modest increase in BP (particularly when supine) and an increase in cardiac output. Tachycardia was also noticed after oral administration of the synthetic cannabinoid nabilone (Cesamet®; Lile et al., 2011) or by the oromucosal spray Sativex® (containing Δ9-THC: cannabidiol ≍ 1:1; Karschner et al., 2011). A review of almost 200 articles describing almost 400 different tests demonstrated that an increase in HR was the most consistent result, and almost all studies with the measurement of this parameter proved statistically significant. Thus, an increase in HR is even believed to be a useful cannabinoid biomarker (Zuurman et al., 2009). Although there is much inter-individual variability, typical increases in HR associated with a single marijuana cigarette range from 20% to 100%, with the peak in HR occurring 10 to 30 min after the onset of smoking. Tolerance to the acute cardiovascular effects of marijuana smoking develops over several days to a few weeks, but it is rapidly lost when cannabinoid administration is stopped (Benowitz and Jones, 1981).
In a study on male cannabis users, the tachycardia was markedly attenuated by orally administered rimonabant (Huestis et al., 2007). Additional studies suggest that the tachycardia may be related to an increased sympathetic activity connected with catecholamine release and decreased parasympathetic autonomic activity. For example, the peak HR rise after Δ9-THC was attenuated by atropine and by propranolol and nearly abolished by atropine-propranolol pretreatment (Benowitz et al., 1979). However, the immediate tachycardia was not accompanied by an increase in noradrenaline levels, which increased 30 min after marijuana exposure only and remained elevated for at least 2 h (Gash et al., 1978). In addition, it has recently been demonstrated in 16 volunteers that Δ9-THC increased HR independent of sympathetic activity since catecholamine levels were not changed (Dumont et al., 2009). Under such conditions, the tachycardia might be related to the CB1 receptor-mediated inhibition of acetylcholine release from the parasympathetic nerves innervating the heart (Figure 3). Pacher et al. (2005) suppose that this mechanism may play a role particularly in healthy young adults whose heart is under a dominant vagal tone. The typical tachycardia obtained with Δ9-THC or cannabis preparations cannot be related to a Δ9-THC-triggered increase in carrier-mediated noradrenaline release (studied in rats; Figure 3); in this case, one would rather expect an increase in BP associated with a baroreceptor reflex-related decrease in HR. Finally, it is remarkable that combined administration of Δ9-THC plus cannabidiol had the same effect as administration of Δ9-THC alone. Cannabidiol is known to counteract many Δ9-THC-induced effects in general (Russo and Guy, 2006) and to increase the baroreflex-induced bradycardia by the activation of 5-HT1A receptors in rats (Alves et al., 2010) (Table 1).
A second cardiovascular effect associated with marijuana smoking is orthostatic hypotension. The hypotension was greater and longer lasting in hypertensive compared with normotensive volunteers (Crawford and Merritt, 1979). It may occur as a result of decreased vascular resistance (e.g. Jones, 2002; Sidney, 2002; Mathew et al., 2003). The Δ9-THC-induced decrease in BP (Gorelick et al., 2006) could be blocked by the CB1 receptor antagonist rimonabant, again indicating the involvement of these receptors. Chronic use of cannabis may elicit a long-lasting decrease in HR and BP. Interestingly, both major alterations obtained with Δ9-THC in humans, namely an increase in HR and a decrease in BP, have also been detected in conscious rhesus monkeys (Fredericks et al., 1981; Table 1). However, unlike in humans, both phenomena occurred in combination. A rapid tolerance developed to the tachycardia, whereas the hypotension did not change upon repeated administration of Δ9-THC (Fredericks et al., 1981).
Severe acute cardiovascular events may be associated with marijuana as described by some clinical reports. Thus, a decrease in the exercise time to angina, cardiac arrhythmias, ventricular tachycardia, palpitations or atrial fibrillation have been noticed (Caldicott et al., 2005; Aryana and Williams, 2007). Moreover, it caused a 4.8-fold increase in the risk of myocardial infarction within 1 h after marijuana smoking (Mittleman et al., 2001). Marijuana use was also associated with a threefold greater mortality after myocardial infarction (Mukamal et al., 2008) and ischemic stroke (Singh et al., 2011). However, the exact aetiopathology of these changes still remains to be established. The following mechanisms are proposed: cardiac ischaemia due to an increase in HR, postural hypotension, proarrhythmic effect of catecholamines, delay in seeking medical care for acute coronary events due to the analgesic properties of cannabinoids, impaired oxygen supply to the heart secondary to increases in blood carboxyhaemoglobin levels and cellular stress elicited by oxidant gases produced by marijuana. Transient vasospasm is suggested as a cause for stroke (Caldicott et al., 2005; Aryana and Williams, 2007). The well-known reduction in cerebral blood flow may contribute as well.
In summary, in humans the cannabinoids Δ9-THC (alone or in combination with cannabidiol) or nabilone are used only. They frequently lead to a tachycardia sometimes associated with a modest increase in blood pressure. Rarely, they lead to decrease in blood pressure. There are two major differences with respect to animals. First, the two alterations do not occur in combination. Second, the stimulation of the cardiovascular system primarily involves an increase in heart rate rather than in blood pressure. There are, however, also remarkable similarities to the situation in conscious animals. Thus, like in conscious animals, ‘phases II’ and ‘III’ may be related to the activation of CB1 receptors. ‘Phase II’ in humans is frequently related to an excitation of the sympathetic and depression of the parasympathetic nervous system. In some instances, presynaptic inhibitory CB1 receptors on the parasympathetic nerve fibres supplying the heart (decelerator nerves) may be involved. ‘Phase III’ may be related to the activation of inhibitory presynaptic CB1 receptors on the sympathetic nerve fibres innervating resistance vessels and heart. Like in animals, this phase is more marked under hypertension.
Acknowledgments
The authors would like to thank the Deutsche Forschungsgemeinschaft (DFG) and the Fundacja na rzecz Nauki Polskiej (FNP) (Copernicus Award jointly to BM and ES), the Medical University of Bialystok (F-13954F to BM) and the DFG (Forschergruppe 926, Schl 266/7-1 to ES) for the financial support they received for their research quoted in this review article.
Glossary
- 2-AG
2-arachidonoyl glycerol
- AEA
anandamide
- AM251
(N-(piperidin-1-yl)-5-(4-iodophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide)
- AM404
N-(4-hydroxyphenyl)-5Z,8Z, 11Z,14Z-eicosatetraenamide
- AM3506
(5-[4-hydroxyphenyl] pentanesulphonyl fluoride)
- BP
blood pressure
- CGRP
calcitonin-gene-related-peptide
- CP55940
(−)-cis-3-[2-hydroxy-4-(1,1-dimethylheptyl)phenyl]-trans-4-(3-hydroxypropyl)-cyclohexanol
- dPAG
dorsal periaqueductal gray
- FAAH
fatty acid amide hydrolase
- HR
heart rate
- HU210
(6aR)-trans-3-(1,1-dimethylheptyl)-6a,7,10,10a-tetrahydro-1-hydroxy-6, 6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol
- i.c
into the cisterna magna
- ICI
118551, (erythro-(+/−)-1-(7-methylindan-4-yloxy)-3-isopropylaminobutan-2-ol)
- i.t
intrathecal
- MAGL
monoacylglycerole lipase
- MethAEA
R-(+)-methanandamide
- MK-801
((5R,10S)-(+)-5-methyl-10,11-dihydro-5H-dibenzo(a,d)-cyclohepten-5,10-imine hydrogen maleate)
- NADA
N-arachidonoyl-dopamine
- NAT
neuronal noradrenaline transporter
- NTS
nucleus tractus solitarii
- O-1918
(1,3-dimethoxy-5-methyl-2-[(1R,6R)-3-methyl-6-(1-methylethenyl)-2-cyclohexen-1-yl]-benzene)
- PAG
periaqueductal gray
- PVN
paraventricular nucleus of the hypothalamus
- RSNA
renal sympathetic nerve activity
- RVLM
rostral ventrolateral medulla
- SHR
spontaneously hypertensive rats
- Δ9-THC
Δ9-tetrahydrocannabinol
- TRPV1
transient receptor potential channels of V1 type
- URB597
(3′-(aminocarbonyl)[1,1′-biphenyl]-3-yl)-cyclohexylcarbamate)
- WIN55212-2
(R(+) [2,3-dihydro-5-methyl-3-[(morpholinyl)methyl]pyrrolo[1,2,3-de]-1,4-benzoxazinyl]-(1-naphthalenyl)-methanone mesylate)
Conflicts of interest
None.
References
- Adams MD, Earnhardt JT, Dewey WL, Harris LS. Vasoconstriction action of Δ8- and Δ9-tetrahydrocannabinol in the rat. J Pharmacol Exp Ther. 1976;196:649–656. [PubMed] [Google Scholar]
- Alexander SPH, Mathie A, Peters JA. Guide to Receptors and Channels (GRAC), 5th Edition. Br J Pharmacol. 2011;164(Suppl. 1):S1–S324. doi: 10.1111/j.1476-5381.2011.01649_1.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves FHF, Crestani CC, Gomes FV, Guimarães FS, Correa FMA, Resstel LBM, et al. Cannabidiol injected into the bed nucleus of the stria terminalis modulates baroreflex activity through 5-HT1A receptors. Pharmacol Res. 2010;62:228–236. doi: 10.1016/j.phrs.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Aryana A, Williams M. Marijuana as a trigger of cardiovascular events: speculation or scientific certainty? Int J Cardiol. 2007;118:141–144. doi: 10.1016/j.ijcard.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Baranowska U, Göthert M, Rudz R, Malinowska B. Methanandamide allosterically inhibits in vivo the function of peripheral nicotinic acetylcholine receptors containing the α7-subunit. J Pharmacol Exp Ther. 2008;326:912–919. doi: 10.1124/jpet.108.140863. [DOI] [PubMed] [Google Scholar]
- Bátkai S, Pacher P. Endocannabinoids and cardiac contractile function: pathophysiological implications. Pharmacol Res. 2009;60:99–106. doi: 10.1016/j.phrs.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bátkai S, Pacher P, Osei-Hyiaman D, Radaeva S, Liu J, Harvey-White J, et al. Endocannabinoids acting at cannabinoid-1 receptors regulate cardiovascular function in hypertension. Circulation. 2004;110:1996–2002. doi: 10.1161/01.CIR.0000143230.23252.D2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL, Jones RT. Cardiovascular and metabolic considerations in prolonged cannabinoid administration in man. J Clin Pharmacol. 1981;21(8–9 Suppl.):214S–223S. doi: 10.1002/j.1552-4604.1981.tb02598.x. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Rosenberg J, Rogers W, Bachman J, Jones RT. Cardiovascular effects of intravenous Δ9-tetrahydrocannabinol: autonomic nervous mechanisms. Clin Pharmacol Ther. 1979;25:440–446. doi: 10.1002/cpt1979254440. [DOI] [PubMed] [Google Scholar]
- Bilfinger TV, Salzet M, Fimiani C, Deutsch DG, Tramu G, Stefano GB. Pharmacological evidence for anandamide amidase in human cardiac and vascular tissues. Int J Cardiol. 1998;64(Suppl. 1):S15–S22. doi: 10.1016/s0167-5273(98)00031-x. [DOI] [PubMed] [Google Scholar]
- Bonz A, Laser M, Küllmer S, Kniesch S, Babin-Ebell J, Popp V, et al. Cannabinoids acting on CB1 receptors decrease contractile performance in human atrial muscle. J Cardiovasc Pharmacol. 2003;41:657–664. doi: 10.1097/00005344-200304000-00020. [DOI] [PubMed] [Google Scholar]
- Brozoski DT, Dean C, Hopp FA, Hillard CJ, Segard JL. Differential endocannabinoid regulation of baroreflex-evked sympathoinhibition in normotensive versus hypertensive rats. Autonom Neurosci. 2009;150:82–93. doi: 10.1016/j.autneu.2009.05.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldicott DGE, Holmes J, Roberts-Thomson KC, Mahar L. Keep off the grass: marijuana use and acute cardiovascular events. Eur J Emerg Med. 2005;12:236–244. doi: 10.1097/00063110-200510000-00008. [DOI] [PubMed] [Google Scholar]
- Campagna JA, Carter C. Clinical relevance of the Bezold-Jarisch reflex. Anesthesiology. 2003;98:1250–1260. doi: 10.1097/00000542-200305000-00030. [DOI] [PubMed] [Google Scholar]
- Carruba MO, Bondiolotti G, Picotti GB, Catteruccia N, Da Prada M. Effects of diethyl ether, halothane, ketamine and urethane on sympathetic activity in the rat. Eur J Pharmacol. 1987;134:15–24. doi: 10.1016/0014-2999(87)90126-9. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Leffler A, Malmberg AB, Martin WJ, Trafton J, Petersen-Zeitz KR, et al. Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science. 2000;288:306–313. doi: 10.1126/science.288.5464.306. [DOI] [PubMed] [Google Scholar]
- Crawford WJ, Merritt JC. Effects of tetrahydrocannabinol on arterial and intraocular hypertension. Int J Clin Pharmacol Biopharm. 1979;17:191–196. [PubMed] [Google Scholar]
- Dean C. Endocannabinoid modulation of sympathetic and cardiovascular responses to acute stress in the periaqueductal gray of the rat. Am J Physiol Regul Integr Comp Physiol. 2011;300:R771–R779. doi: 10.1152/ajpregu.00391.2010. [DOI] [PubMed] [Google Scholar]
- Di Marzo V, De Petrocellis L, Bisogno T. The biosynthesis, fate and pharmacological properties of endocannabinoids. Handb Exp Pharmacol. 2005;168:147–185. doi: 10.1007/3-540-26573-2_5. [DOI] [PubMed] [Google Scholar]
- Dumont GJ, Kramers C, Sweep FC, Touw DJ, vanHasselt JG, de Kam M, et al. Cannabis coadministration potentiates the effects of ‘ecstasy’ on heart rate and temperature in humans. Clin Pharmacol Ther. 2009;86:160–166. doi: 10.1038/clpt.2009.62. [DOI] [PubMed] [Google Scholar]
- Fredericks AB, Benowitz NL, Savanapridi CY. The cardiovascular and autonomic effects of repeated administration of Δ9-tetrahydrocannabinol to rhesus monkeys. J Pharmacol Exp Ther. 1981;216:247–253. [PubMed] [Google Scholar]
- García MC, Adler-Graschinsky E, Celuch SM. Hypotensive effect of anandamide through the activation of CB1 and VR1 spinal receptors in urethane-anaesthetized rats. Naunyn Schmiedebergs Arch Pharmacol. 2003;368:270–276. doi: 10.1007/s00210-003-0800-x. [DOI] [PubMed] [Google Scholar]
- García MC, Adler-Graschinsky E, Celuch SM. Enhancement of the hypotensive effects of intrathecally injected endocannabinoids by the entourage compound palmitoylethanolamide. Eur J Pharmacol. 2009;610:75–80. doi: 10.1016/j.ejphar.2009.03.021. [DOI] [PubMed] [Google Scholar]
- Gardiner SM, March JE, Kemp PA, Bennett T. Regional haemodynamic responses to the cannabinoid agonist, WIN 55212-2, in conscious, normotensive rats, and in hypertensive, transgenic rats. Br J Pharmacol. 2001;33:445–453. doi: 10.1038/sj.bjp.0704100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner SM, March JE, Kemp PA, Bennett T. Complex regional haemodynamic effects of anandamide in conscious rats. Br J Pharmacol. 2002a;135:1889–1896. doi: 10.1038/sj.bjp.0704649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner SM, March JE, Kemp PA, Bennett T. Influence of the CB1 receptor antagonist, AM 251, on the regional haemodynamic effects of WIN-55212-2 or HU 210 in conscious rats. Br J Pharmacol. 2002b;136:581–587. doi: 10.1038/sj.bjp.0704750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner SM, March JE, Kemp PA, Bennett T. Factors influencing the regional haemodynamic responses to methanandamide and anandamide in conscious rats. Br J Pharmacol. 2009;158:1143–1152. doi: 10.1111/j.1476-5381.2009.00363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gash A, Karliner JS, Janowsky D, Lake CR. Effects of smoking marihuana on left ventricular performance and plasma norepinephrine: studies in normal men. Ann Intern Med. 1978;89:448–452. doi: 10.7326/0003-4819-89-4-448. [DOI] [PubMed] [Google Scholar]
- Godlewski G, Göthert M, Malinowska B. Cannabinoid receptor-independent inhibition by cannabinoid agonists of the peripheral 5-HT3 receptor-mediated von Bezold-Jarisch reflex. Br J Pharmacol. 2003;138:767–774. doi: 10.1038/sj.bjp.0705114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godlewski G, Alapafuja SO, Bátkai S, Nikas SP, Cinar R, Offertáler L, et al. Inhibitor of fatty acid amide hydrolase normalizes cardiovascular function in hypertension without adverse metabolic effects. Chem Biol. 2010;17:1256–1266. doi: 10.1016/j.chembiol.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golech SA, McCarron RM, Chen Y, Bembry J, Lenz F, Mechoulam R, et al. Human brain endothelium: coexpression and function of vanilloid and endocannabinoid receptors. Brain Res Mol Brain Res. 2004;132:87–92. doi: 10.1016/j.molbrainres.2004.08.025. [DOI] [PubMed] [Google Scholar]
- Gorelick DA, Heishman SJ, Preston KL, Nelson RA, Moolchan ET, Huestis MA. The cannabinoid CB1 receptor antagonist rimonabant attenuates the hypotensive effect of smoked marijuana in male smokers. Am Heart J. 2006;151:754.e1–754.e5. doi: 10.1016/j.ahj.2005.11.006. [DOI] [PubMed] [Google Scholar]
- Gunthorpe MJ, Benham CD, Randall A, Davis JB. The diversity in the vanilloid (TRPV) receptor family of ion channels. Trends Pharmacol Sci. 2002;23:183–191. doi: 10.1016/s0165-6147(02)01999-5. [DOI] [PubMed] [Google Scholar]
- Hampson AJ, Bornheim LM, Scanziani M, Yost CS, Gray AT, Hansen BM, et al. Dual effects of anandamide on NMDA receptor-mediated responses and neurotransmission. J Neurochem. 1998;70:671–676. doi: 10.1046/j.1471-4159.1998.70020671.x. [DOI] [PubMed] [Google Scholar]
- Ho WS, Gardiner SM. Acute hypertension reveals depressor and vasodilator effects of cannabinoids in conscious rats. Br J Pharmacol. 2009;156:94–104. doi: 10.1111/j.1476-5381.2008.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlett AC, Reggio PH, Childers SR, Hampson RE, Ulloa NM, Deutsch DG. Endocannabinoid tone versus constitutive activity of cannabinoid receptors. Br J Pharmacol. 2011;163:1329–1343. doi: 10.1111/j.1476-5381.2011.01364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W, Rubinstein J, Prieto AR, Thang LV, Wang DH. Transient receptor potential vanilloid gene deletion exacerbates inflammation and atypical cardiac remodeling after myocardial infarction. Hypertension. 2009;53:243–250. doi: 10.1161/HYPERTENSIONAHA.108.118349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huestis MA, Boyd SJ, Heishman SJ, Preston KL, Bonnet D, Le Fur G, et al. Single and multiple doses of rimonabant antagonize acute effects of smoked cannabis in male cannabis users. Psychopharmacology (Berl) 2007;194:505–515. doi: 10.1007/s00213-007-0861-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huitrón-Reséndiz S, Gombart L, Cravatt BF, Henriksen SJ. Effect of oleamide on sleep and its relationship to blood pressure, body temperature, and locomotor activity. Exp Neurol. 2001;172:235–243. doi: 10.1006/exnr.2001.7792. [DOI] [PubMed] [Google Scholar]
- Ishac EJ, Jiang L, Lake KD, Varga K, Abood ME, Kunos G. Inhibition of exocytotic noradrenaline release by presynaptic cannabinoid CB1 receptors on peripheral sympathetic nerves. Br J Pharmacol. 1996;118:2023–2028. doi: 10.1111/j.1476-5381.1996.tb15639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izzo AA, Borrelli F, Capasso R, Di Marzo V, Mechoulam R. Non-psychotropic plant cannabinoids: new therapeutic opportunities from an ancient herb. Trends Pharmacol Sci. 2009;30:515–527. doi: 10.1016/j.tips.2009.07.006. [DOI] [PubMed] [Google Scholar]
- Járai Z, Wagner JA, Varga K, Lake KD, Compton DR, Martin BR, et al. Cannabinoid-induced medenteric vasodilatation through an endothelial site distinct from CB1 or CB2 receptors. Proc Natl Acad Sci U S A. 1999;96:14136–14141. doi: 10.1073/pnas.96.24.14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Járai Z, Wagner JA, Goparaju SK, Wang L, Razdan RK, Sugiura T, et al. Cardiovascular effects of 2-arachidonoyl glycerol in anesthetized mice. Hypertension. 2000;35:679–684. doi: 10.1161/01.hyp.35.2.679. [DOI] [PubMed] [Google Scholar]
- Jones RT. Cardiovascular system effects of marijuana. J Clin Pharmacol. 2002;42:58–63. doi: 10.1002/j.1552-4604.2002.tb06004.x. [DOI] [PubMed] [Google Scholar]
- Karschner EL, Darwin WD, McMahon RP, Liu F, Wright S, Goodwin RS, et al. Subjective and physiological effects after controlled Sativex and oral THC administration. Clin Pharmacol Ther. 2011;89:400–407. doi: 10.1038/clpt.2010.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kase Y, Obata T, Okamoto Y, Iwai K, Saito K, Yokoyama K, et al. Removal of 2-arachidonylglycerol by direct hemoperfusion therapy with polymyxin B immobilized fibers benefits patients with septic shock. Ther Apher Dial. 2008;12:374–380. doi: 10.1111/j.1744-9987.2008.00612.x. [DOI] [PubMed] [Google Scholar]
- Kathuria S, Gaetani S, Fegley D, Valino F, Duranti A, Tontini A, et al. Modulation of anxiety through blockade of anandamide hydrolysis. Nat Med. 2003;9:76–81. doi: 10.1038/nm803. [DOI] [PubMed] [Google Scholar]
- Kozłowska H, Baranowska M, Schlicker E, Kozłowski M, Laudański J, Malinowska B. Identification of the vasodilatory endothelial cannabinoid receptor in the human pulmonary artery. J Hypertens. 2007;25:2240–2248. doi: 10.1097/HJH.0b013e3282ef7a0a. [DOI] [PubMed] [Google Scholar]
- Kozłowska H, Baranowska M, Schlicker E, Kozłowski M, Laudański J, Malinowska B. Virodhamine relaxes the human pulmonary artery through the endothelial cannabinoid receptor and indirectly through a COX product. Br J Pharmacol. 2008;155:1034–1042. doi: 10.1038/bjp.2008.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurz C, Baranowska U, Lupiński S, Göthert M, Malinowska B, Schlicker E. Urethane, but not pentobarbitone, attenuates presynaptic receptor function in rats: a contribution to the choice of anaesthetic. Br J Pharmacol. 2009;157:1474–1482. doi: 10.1111/j.1476-5381.2009.00315.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurz CM, Gottschalk C, Schlicker E, Kathmann M. Identification of a presynaptic cannabinoid CB1 receptor in the guinea-pig atrium and sequencing of the guinea-pig CB1 receptor. J Physiol Pharmacol. 2008;59:3–15. [PubMed] [Google Scholar]
- Kwolek G, Zakrzeska A, Schlicker E, Göthert M, Godlewski G, Malinowska B. Central and peripheral components of the pressor effect of anandamide in urethane-anaesthetized rats. Br J Pharmacol. 2005;145:567–675. doi: 10.1038/sj.bjp.0706195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake KD, Campton DR, Varga K, Martin BR, Kunos G. Cannabinoid-induced hypotension and bradycardia in rats is mediated by CB1-like cannabinoid receptors. J Pharmacol Exp Ther. 1997a;281:1030–1037. [PubMed] [Google Scholar]
- Lake KD, Martin BR, Kunos G, Varga K. Cardiovascular effects of anandamide in anesthetized and conscious normotensive and hypertensive rats. Hypertension. 1997b;29:1204–1210. doi: 10.1161/01.hyp.29.5.1204. [DOI] [PubMed] [Google Scholar]
- Ledent C, Valverde O, Cossu G, Petitet F, Aubert JF, Beslot F, et al. Unresponsiveness to cannabinoids and reduced addictive effects of opiates in CB1 receptor knockout mice. Science. 1999;283:401–404. doi: 10.1126/science.283.5400.401. [DOI] [PubMed] [Google Scholar]
- Lile JA, Kelly TH, Hays LR. Separate and combined effects of the cannabinoid agonists nabilone and Δ9-THC in humans discriminating Δ9-THC. Drug Alcohol Depend. 2011;116:86–92. doi: 10.1016/j.drugalcdep.2010.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Gao B, Mirshahi F, Sanyal AJ, Khanolkar AD, Makriyannis A, et al. Functional CB1 cannabinoid receptors in human vascular endothelial cells. Biochem J. 2000;346:835–840. [PMC free article] [PubMed] [Google Scholar]
- Łupiński SŁ, Schlicker E, Pędzińska-Betiuk A, Malinowska B. Acute myocardial ischemia enhances the vanilloid TRPV1 and serotonin 5-HT3 receptor-mediated Bezold-Jarisch reflex in rats. Pharmacol Rep. 2011 doi: 10.1016/s1734-1140(11)70709-5. (in press) [DOI] [PubMed] [Google Scholar]
- Malinowska B, Godlewski G, Bucher B, Schlicker E. Cannabinoid CB1 receptor-mediated inhibition of the neurogenic vasopressor response in the pithed rat. Naunyn Schmiedebergs Arch Pharmacol. 1997;356:197–202. doi: 10.1007/pl00005041. [DOI] [PubMed] [Google Scholar]
- Malinowska B, Kwolek G, Göthert M. Anandamide and methanandamide induce both vanilloid VR1- and cannabinoid CB1 receptor-mediated changes in heart rate and blood pressure in anaesthetized rats. Naunyn Schmiedebergs Arch Pharmacol. 2001a;364:562–569. doi: 10.1007/s00210-001-0498-6. [DOI] [PubMed] [Google Scholar]
- Malinowska B, Piszcz J, Koneczny B, Hryniewicz A, Schlicker E. Modulation of the cardiac autonomic transmission of pithed rats by presynaptic opioid OP4 and cannabinoid CB1 receptors. Naunyn Schmiedebergs Arch Pharmacol. 2001b;364:233–241. doi: 10.1007/s002100100450. [DOI] [PubMed] [Google Scholar]
- Malinowska B, Łupiński S, Godlewski G, Baranowska U, Schlicker E. Role of endocannabinoids in cardiovascular shock. J Physiol Pharmacol. 2008;59(Suppl. 8):91–107. [PubMed] [Google Scholar]
- Malinowska B, Zakrzeska A, Kurz CM, Göthert M, Kwolek G, Wielgat P, et al. Involvement of central β2-adrenergic, NMDA and thromboxane A2 receptors in the pressor effect of anandamide in rats. Naunyn Schmiedebergs Arch Pharmacol. 2010;381:349–360. doi: 10.1007/s00210-010-0497-6. [DOI] [PubMed] [Google Scholar]
- Mathew RJ, Wilson WH, Davir R. Postural syncope after marijuana: a transcranial Doppler study of the hemodynamics. Pharmacol Biochem Behav. 2003;75:309–318. doi: 10.1016/s0091-3057(03)00086-8. [DOI] [PubMed] [Google Scholar]
- Mendizábal VE, Adler-Graschinsky E. Cannabinoids as therapeutic agents in cardiovascular disease: a tale of passions and illusions. Br J Pharmacol. 2007;151:427–440. doi: 10.1038/sj.bjp.0707261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittleman MA, Rebecca AL, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805–2809. doi: 10.1161/01.cir.103.23.2805. [DOI] [PubMed] [Google Scholar]
- Molderings GJ, Likungu J, Göthert M. Presynaptic cannabinoid and imidazoline receptors in the human heart and their potential relationship. Naunyn Schmiedebergs Arch Pharmacol. 1999;360:157–164. doi: 10.1007/s002109900043. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Maclure M, Muller JE, Mittleman MA. An exploratory prospective study of marijuana use and mortality following acute myocardial infarction. Am Heart J. 2008;155:465–470. doi: 10.1016/j.ahj.2007.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukhtarov M, Ragozzino D, Bregestovski P. Dual Ca2+ modulation of glycinergic synaptic currents in rodent hypoglossal motoneurones. J Physiol. 2005;569:817–831. doi: 10.1113/jphysiol.2005.094862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederhoffer N, Szabo B. Effect of the cannabinoid receptor agonist WIN55212-2 on sympathetic cardiovascular regulation. Br J Pharmacol. 1999;126:457–466. doi: 10.1038/sj.bjp.0702337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederhoffer N, Szabo B. Cannabinoid cause central sympathoexcitation and bradycardia in rabbits. J Pharmacol Exp Ther. 2000;294:707–713. [PubMed] [Google Scholar]
- Niederhoffer N, Hansen HH, Fernandez-Ruiz JJ, Szabo B. Effects of cannabinoids on adrenaline release from adrenal medullary cells. Br J Pharmacol. 2001;134:1319–1327. doi: 10.1038/sj.bjp.0704359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederhoffer N, Schmid K, Szabo B. The peripheral sympathetic nervous system is the major target of cannabinoids in eliciting cardiovascular depression. Naunyn Schmiedebergs Arch Pharmacol. 2003;367:434–443. doi: 10.1007/s00210-003-0755-y. [DOI] [PubMed] [Google Scholar]
- O'Sullivan SE, Randall MD, Gardiner SM. The in vitro and in vivo cardiovascular effects of Δ9-tetrahydrocannabinol in rats made hypertensive by chronic inhibition of nitric-oxide synthase. J Pharmacol Exp Ther. 2007;321:663–672. doi: 10.1124/jpet.106.116566. [DOI] [PubMed] [Google Scholar]
- Offertáler L, Mo FM, Bátkai S, Liu J, Begg M, Razdan RK, et al. Selective ligands and cellular effectors of a G protein-coupled endothelial cannabinoid receptor. Mol Pharmacol. 2003;63:699–705. doi: 10.1124/mol.63.3.699. [DOI] [PubMed] [Google Scholar]
- Oz M, Ravindran A, Diaz-Ruiz O, Zhang L, Morales M. The endogenous cannabinoid anandamide inhibits α7 nicotinic acetylcholine receptor-mediated responses in Xenopus oocytes. J Pharmacol Exp Ther. 2003;306:1003–1010. doi: 10.1124/jpet.103.049981. [DOI] [PubMed] [Google Scholar]
- Oz M, Zhang L, Ravindran A, Morales M, Lupica C. Differential effects of endogenous and synthetic cannabinoids on α7-nicotinic acetylcholine receptor-mediated responses in Xenopus oocytes. J Pharmacol Exp Ther. 2004;310:1152–1160. doi: 10.1124/jpet.104.067751. [DOI] [PubMed] [Google Scholar]
- Pacher P, Bátkai S, Kunos G. Haemodynamic profile and responsiveness to anandamide of TRPV1 receptor knock-out mice. J Physiol. 2004;558:647–657. doi: 10.1113/jphysiol.2004.064824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacher P, Bátkai S, Kunos G. Cardiovascular pharmacology of cannabinoids. Handb Exp Pharmacol. 2005;168:599–625. doi: 10.1007/3-540-26573-2_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacher P, Bátkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58:389–462. doi: 10.1124/pr.58.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padley JR, Li Q, Pilowsky PM, Goodchild AK. Cannabinoid receptor activation in the rostral ventrolateral medulla oblongata evokes cardiorespiratory effects in anaesthetized rats. Br J Pharmacol. 2003;140:384–394. doi: 10.1038/sj.bjp.0705422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan HL, Chen SR. Sensing tissue ischemia. Another new function for capsaicin receptors? Circulation. 2004;110:1826–1831. doi: 10.1161/01.CIR.0000142618.20278.7A. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. Pharmacological actions of cannabinoids. Handb Exp Pharmacol. 2005;168:1–51. doi: 10.1007/3-540-26573-2_1. [DOI] [PubMed] [Google Scholar]
- Pertwee RG, Howlett AC, Abood ME, Alexander SP, Di Marzo V, Elphick MR, et al. International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2. Pharmacol Rev. 2010;62:588–631. doi: 10.1124/pr.110.003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfitzer T, Niederhoffer N, Szabo B. Central effects oft he cannabinoid receptor agonist WIN55212-2 on respiratory and cardiovascular regulation in anaesthetized rats. Br J Pharmacol. 2004;142:943–952. doi: 10.1038/sj.bjp.0705874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rademacher DJ, Patel S, Hopp S, Dean C, Hillard CJ, Seagard JL. Microinjection of a cannabinoid antagonist into the NTS increases baroreflex duration in dogs. Am J Physiol Heart Circ Physiol. 2003;284:H1570–H1576. doi: 10.1152/ajpheart.00772.2002. [DOI] [PubMed] [Google Scholar]
- Rajesh M, Mukhopadhyay P, Haskó G, Huffman JW, Mackie K, Pacher P. CB2 cannabinoid receptor agonists attenuate TNF-alpha-induced human vascular smooth muscle cell proliferation and migration. Br J Pharmacol. 2007;153:347–357. doi: 10.1038/sj.bjp.0707569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall MD, Kendall DA, O'Sullivan S. The complexities of the cardiovascular actions of cannabinoids. Br J Pharmacol. 2004;142:20–26. doi: 10.1038/sj.bjp.0705725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo E, Guy GW. A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. Med Hypotheses. 2006;66:234–246. doi: 10.1016/j.mehy.2005.08.026. [DOI] [PubMed] [Google Scholar]
- Schultheiβ T, Flau K, Kathmann M, Göthert M, Schlicker E. Cannabinoid CB1 receptor-mediated inhibition of noradrenaline release in guinea-pig vessels, but not in rat and mouse aorta. Naunyn Schmiedebergs Arch Pharmacol. 2005;372:139–146. doi: 10.1007/s00210-005-0007-4. [DOI] [PubMed] [Google Scholar]
- Sidney Y. Cardiovascular consequences of marijuana use. J Clin Pharmacol. 2002;42(11 Suppl.):64S–70S. doi: 10.1002/j.1552-4604.2002.tb06005.x. [DOI] [PubMed] [Google Scholar]
- Singh NN, Pan Y, Muengtaweeponsa S, Geller TJ, Cruz-Flores S. Cannabis-related stroke: case series and review of literature. J Stroke Cerebrovasc Dis. 2011 doi: 10.1016/j.jstrokecerebrovasdis.2010.12.010. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Smith PJ, McQueen DS. Anandamide induces cardiovascular and respiratory reflexes via vasosensory nerves in the anaesthetized rat. Br J Pharmacol. 2001;134:655–663. doi: 10.1038/sj.bjp.0704296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefano GB, Bilfinger TV, Rialas CM, Deutsch DG. 2-arachidonyl-glycerol stimulates nitric oxide release from human immune and vascular tissues and invertebrate immunocytes by cannabinoid receptor 1. Pharmacol Res. 2000;42:317–322. doi: 10.1006/phrs.2000.0702. [DOI] [PubMed] [Google Scholar]
- Sugiura T, Kodaka T, Nakane S, Kishimoto S, Kondo S, Waku K. Detection of an endogenous cannabimimetic molecule, 2-arachidonoylglycerol, and cannabinoid CB1 receptor mRNA in human vascular cells: is 2-arachidonoylglycerol a possible vasomodulator? Biochem Biophys Res Commun. 1998;243:838–843. doi: 10.1006/bbrc.1998.8187. [DOI] [PubMed] [Google Scholar]
- Szabo B, Nordheim U, Niederhoffer N. Effects of cannabinoids on sympathetic and parasympathetic neuroeffector transmission in the rabbit heart. J Pharmacol Exp Ther. 2001;297:819–826. [PubMed] [Google Scholar]
- Valverde O, Karsak M, Zimmer A. Analysis of the endocannabinoid system by using CB1 cannabinoid receptor knockout mice. Handb Exp Pharmacol. 2005;168:117–145. doi: 10.1007/3-540-26573-2_4. [DOI] [PubMed] [Google Scholar]
- Varga K, Lake K, Martin BR, Kunos G. Novel antagonist implicates the CB1 cannabinoid receptor in the hypotensive action of anandamide. Eur J Pharmacol. 1995;278:279–283. doi: 10.1016/0014-2999(95)00181-j. [DOI] [PubMed] [Google Scholar]
- Varga K, Lake K, Huangfu D, Guyenet PG, Kunos G. Mechanism of hypotensive actio of anandamide in anesthetized rats. Hypertension. 1996;28:682–686. doi: 10.1161/01.hyp.28.4.682. [DOI] [PubMed] [Google Scholar]
- Varga K, Wagner JA, Bridgen DT, Kunos G. Platelet- and macrophage-derived endogenous cannabinoids are involved in endotoxin-induced hypotension. FASEB J. 1998;12:1035–1044. doi: 10.1096/fasebj.12.11.1035. [DOI] [PubMed] [Google Scholar]
- Vidrio H, Sánches-Salvatori MA, Medina M. Cardiovascular effects of (-)-11-Δ8-tetrahydrocannabinol-dimethylheptyl in rats. J Cardiovasc Pharmacol. 1996;28:332–336. doi: 10.1097/00005344-199608000-00022. [DOI] [PubMed] [Google Scholar]
- Wagner JA, Járai Z, Bátkai S, Kunos G. Hemodynamic effects of cannabinoids: coronary and cerebral vasodilation mediated by cannabinoid CB1 receptors. Eur J Pharmacol. 2001;423:203–210. doi: 10.1016/s0014-2999(01)01112-8. [DOI] [PubMed] [Google Scholar]
- Wang Y, Wang DH. Increased depressor response to N-arachidonoyl-dopamine during high salt intake: role of the TRPV1 receptor. J Hypertens. 2007;25:2426–2433. doi: 10.1097/HJH.0b013e3282efd1bf. [DOI] [PubMed] [Google Scholar]
- Weis F, Beiras-Fernandez A, Kaczmarek I, Reichart B, Beiras A, Schelling G, et al. Substantially altered expression of cannabinoid receptor 2 and activated endocannabinoid system in patients with severe heart failure. J Mol Cell Cardiol. 2010;48:1187–1193. doi: 10.1016/j.yjmcc.2009.10.025. [DOI] [PubMed] [Google Scholar]
- Williams MA, Smith SS, O'Brien DE, Mitchel JH, Garry MG. The group IV afferent neuron express multiple receptor alternation in cardiomyopathyic rats: evidence at the cannabinoid CB1 receptor. J Physiol. 2008;586:835–845. doi: 10.1113/jphysiol.2007.140392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahner MR, Li DP, Chen SR, Pan HL. Cardiac vanilloid receptor 1-expressing afferent nerves and their role in the cardiogenic sympathetic reflex in rats. J Physiol. 2003;551:515–523. doi: 10.1113/jphysiol.2003.048207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakrzeska A, Schlicker E, Baranowska M, Kozłowska H, Kwolek G, Malinowska B. A cannabinoid receptor, sensitive to O-1918, is involved in the delayed hypotension induced by anandamide in anaesthetized rats. Br J Pharmacol. 2010;160:574–584. doi: 10.1111/j.1476-5381.2009.00579.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuurman L, Ippel AE, Moin E, van Gerven JM. Biomarkers for the effects of cannabis and THC in healthy volunteers. Br J Clin Pharmacol. 2009;67:5–21. doi: 10.1111/j.1365-2125.2008.03329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


