Abstract
Objective: The aim of the present study was to identify psychosocial risk factors for the incidence of recurrent headache (HA) in children/adolescents (8–15 years).
Method: In 2003 (Wave 1) a representative, population-based sample of 8800 parents was mailed a questionnaire. Those who took part were asked to participate again one year later (Wave 2). Of the parents originally contacted, 47.3% participated in both surveys. Potential risk factors concerning the areas ‘school’ and ‘emotional and behavioural problems’ were collected in Wave 1. Binary logistic regression analyses were performed to assess their predictive value for HA in Wave 2.
Results: Univariable regression analyses showed that for boys and girls most of the predictor variables influenced the incidence of recurrent HA, but only to a very low extent. When all variables were assessed jointly in a multivariable model, these factors lost their predictive power for boys. For girls, ‘academic problems’ and ‘dysfunctional stress coping’ were shown to increase the chance for the incidence of recurrent HA.
Discussion: In contrast to previous findings, school-related factors and emotional and behavioural problems failed to predict HA in boys, and only two factors appeared relevant with regard to girls. This might be due to the strict unidirectional design, which focussed exclusively on the incidence of HA.
Keywords: children, headache, population-based longitudinal study, risk factors, incidence
Abstract
Zielsetzung: Es existieren eine Reihe von Querschnittstudien, die psychosoziale Faktoren mit Kopfschmerzen bei Kindern und Jugendlichen in Verbindung bringen. In diesen Studien bleibt aber offen, ob die psychosozialen Faktoren Ursache oder Folge der Kopfschmerzen sind. Ziel der vorliegenden Studie war es deshalb, in einem longitudinalen Design psychosoziale Risikofaktoren zu identifizieren, die das Neuauftreten (Inzidenz) von wiederkehrenden Kopfschmerzen bei Kindern und Jugendlichen im Alter von 8–15 Jahren ein Jahr nach der Ersterhebung vorhersagen können.
Methodik: Im Jahr 2003 (Welle 1) wurde einer repräsentativen Bevölkerungsstichprobe von 8800 Eltern ein Fragebogen zugesandt. Diejenigen, die den Fragebogen beantwortet hatten, wurden ein Jahr später erneut angeschrieben (Welle 2). Von den ursprünglich kontaktierten Eltern nahmen 47,3% an beiden Befragungen teil. Potentielle Risikofaktoren aus den Bereichen ‚Schule‘ und ‚emotionale Probleme‘ und ‚Verhaltensauffälligkeiten‘ wurden in Welle 1 erhoben und binäre logistische Regressionen durchgeführt, um ihre Vorhersagekraft für Kopfschmerzen in Welle 2 zu prüfen.
Ergebnisse: Univariate Regressionsanalysen zeigten, dass für Mädchen und Jungen die meisten untersuchten Variablen einen Einfluss auf die Inzidenz von wiederkehrenden Kopfschmerzen hatten. Dieser Einfluss war jedoch gering. Im multivariaten Modell verloren die Variablen ihre Vorhersagekraft bei den Jungen. Bei den Mädchen erhöhten ‚Schulprobleme‘ und ‚dysfunktionales Stress Coping‘ das Risiko für die Inzidenz von wiederkehrenden Kopfschmerzen.
Diskussion und Fazit: Entgegen bisherigen Befunden wurden Kopfschmerzen bei Jungen nicht durch Schulfaktoren und emotionale Probleme und Verhaltensauffälligkeiten vorhergesagt und nur zwei Faktoren erwiesen sich als relevant bei der Vorhersage von Kopfschmerzen bei Mädchen. Dieses Ergebnis ist vermutlich auf das strikte unidirektionale Design zurückzuführen, das sich ausschließlich auf die Inzidenz von Kopfschmerzen konzentriert.
Introduction
Longitudinal studies show that around 50% of children with HA continue to suffer from HA as adults [1], [2]. This discouraging long term prognosis illustrates the need for early and focused prevention or intervention. Therefore, the development of aetiological models is of great importance [3], [4].
As recurrent HA is generally assumed to be influenced by psychosocial factors [5], [6] as well as pathophysiological mechanisms (e.g., [7]), the relevance of an investigation of potential psychosocial risk factors for the incidence of paediatric HA is undeniable. Research to date has investigated many different constructs that could be seen as potential stressors that can lead to HA, but with often conflicting results. Numerous studies provided evidence for an association of certain factors, whereas others did not. From a range of variables tested in the ‘KiJuKo-’project, the current study selected those which could be subsumed under the two domains ‘school factors’ and ‘psychological factors’ (see Attachment 1), as these factors were frequently associated with HA in the pertinent literature.
In children and adolescents, especially stresses and strains in the school context were identified as influential factors in connection with HA [8], [9], [10], [11] and named as a trigger for HA [12]. Data from the World Health Organization (WHO) working group on the Health Behaviour in School-aged Children (HSBC) showed that the probability of weekly HA in adolescents with a high level of school-related stress is approximately four times higher than for adolescents without school-related stress [13]. The data also shows that children with HA tended to spend more time on their homework than children from a headache-free control group [14]. Gordon et al. [10] showed in their analyses that children with weekly HA were much more likely to experience negative feelings regarding school, feel unfairly treated by teachers, complain of ‘feeling left out’ and tended to report poor achievement. Various other studies found that there was a close correlation between ‘bullying’ or problems with school mates and HA [4], [15], [16]. Although the majority of publications agree that those factors exert an influence on HA, there are a number of researchers who failed to find connections between these factors and the occurrence of HA (e.g., [10], [17]).
On balance, research so far supports correlative relationships between school-related factors and HA despite contrary findings by some studies. However, the cause and effect relationship remains unclear [17], [18], as HA itself may be experienced as a stressor [10], [19], which may lead to psychosocial consequences such as poor school performance.
It is now widely agreed that dysfunctional stress coping is an important link between stress and pain experiences [9], [19], [20]. Saile [21] showed in a postal survey that children with HA twice per week or more used more dysfunctional coping strategies in stressful situations such as passive avoidance, rumination, resignation and irritable behaviour than children without HA.
Further research efforts have focused on the association between paediatric HA and psychiatric symptoms such as anxiety or depression. School children with recurrent weekly HA reported higher levels of anxiety and depression-related symptoms compared to children who seldomly or never had HA [22], [23]. In a population-based study, Egger and colleagues [24] described that conduct disorders were associated with the occurrence of weekly HA in boys, whereas for girls depression and anxiety disorders appeared relevant.
Longitudinal observations supported the link between anxiety/depression and HA [10], [25], [26]. Higher depression levels could predict HA frequency at a one-year follow-up [27]. In Rhee's [28] one-year longitudinal study, depression and low self-esteem in the first wave predicted HA in girls (but not in boys) a year later. Martin [29], however, assumed in his ‘functional model of chronic headache’ a reversed cause and effect direction. He postulated that HA can lead to social withdrawal because HA sufferers begin to avoid social activities. This, in turn, could result in negative emotions, such as sadness, anxiety or anger. Furthermore, children with frequent or severe HA tended to be more frequently affected by attention deficit disorder [30]. Virtanen and co-authors showed that externalising behaviour problems at the age of 11 could predict the incidence of monthly HA at the age of 14 (as judged by the parents) [31]. There are also authors, however, who failed to find a relationship between HA and anxiety/depression [3], [31] or externalizing symptoms [27].
Previous studies have found sex differences in HA in children and adolescents [28], [32], [33]. The female preponderance among children and adolescents with HA and other syndromes was linked to biological, social or psychological differences. Different factors have been discussed such as hormonal influences [34], [35], [36], biological differences in processing noxious stimuli [37], psychological factors, e.g., self-esteem [28], depression [24], [28], anxiety [24], behavioural and environmental factors, e.g., social-learning processes through modelling, gender role, pain coping strategies, parents’ dealing with children’s HA [9] or parents’ health [32], [38]. A combination of these and other factors may cause the sex differences found.
To sum up: Whereas there is some support for the correlation between school-related and psychological variables and HA, the causal relationships are far from clear. Psychosocial stressors and psychological impairments can be seen as risk factors for HA, as consequences of HA or as both cause and effect in the form of a vicious circle [29], [39]. Empirical findings to date do not permit a decision between these possibilities [19], [25]. Therefore, the objective of the present study is to use unidirectional analyses to identify those factors that precede the incidence of recurrent HA and are therefore candidates for causal factors in the development of recurrent HA. The risk factors as well as headache were assessed retrospectively for a specified time, mostly 6 month, prior to the filling in of the questionnaire (for the exact time windows covered please see Attachment 1). Therefore, in order to establish temporal precedence, we used risk factors from Wave 1 to predict the incidence of headache at Wave 2, rather than those from the same wave.
The following hypotheses will be tested:
First, it is hypothesized that stressful experiences (as reported in Wave 1) in the school context can increase the risk of developing recurrent HA (in Wave 2). Stressful school-related experiences were operationalised as ‘time spent on homework’, ‘academic problems’, ‘deteriorating grades’, ‘danger of grade repeat’, which in themselves could provide a hint to problems at school, as well as ‘school stress’ such as bullying, isolation and school-related fears (see Attachment 1).
Second, it is hypothesized that a high extent of ‘dysfunctional stress coping’ and the other psychological variables (as reported in Wave 1) increase the chance of developing paediatric HA (in Wave 2). Psychological variables were operationalised as ‘dysfunctional stress coping strategies’, ‘reaction to failure’, ‘anger expression’, ‘anxiousness/depressiveness’, ‘hyperactivity’ and ‘aggressive behaviour’ (see Attachment 1).
Since previous findings confirm the relevance of sex-specific effects [27], [28], the present study investigated whether potential risk factors have differing effects on HA in boys and girls.
Methods
Sample and procedure
This investigation is part of a large-scale, longitudinal epidemiological study (Children, Adolescents & Headache Study, ‘KiJuKo’) based on four annual surveys (2003–2006). Results presented here stem from the first two waves.
In the first assessment period (Wave 1, W1, 2003), 8800 families with a child aged 7 to 14 years received one questionnaire for the parents and one for the child (if the child was aged 9 years or older). The results reported here are based on the parents’ responses in order to provide information also for younger children (7 to 8 years of age). Furthermore the parents’ questionnaire contained a total of 111 questions (in W1) whereas the childrens’ questionnaire included only 43 questions, as in a pilot study it became apparent that a more comprehensive questionnaire would be too long for the younger children. Parents’ reports have also been utilised in a number of other studies [32], [40], [41], [42], [43]. The parents were asked to answer a total of 111 questions (in W1) regarding socio-demographic variables and variables relating to their child’s health, family, school, free time/friends and life events as well as emotional and behavioural problems. Extensive measures were implemented to optimize responses and reduce bias [44], [45]. For more detailed information regarding the KiJuKo Study, questionnaire development and results from W1, see Kröner-Herwig et al. [46], [47].
Of the 5586 parents who responded in W1, 5580 consented to be contacted again one year later. In Wave 2 (W2: 2004), 4159 of these parents participated. Of the returned questionnaires, 113 had to be excluded because the identity of the child could not be verified (e.g. a child entered as a “boy” in W1 was now reported as a “girl”). A further 8 questionnaires were omitted because the respondents had answered less than 50% of the items and 54 questionnaires because the item regarding headache frequency had not been answered. Ultimately, 3984 questionnaires were included in our analyses (71.3% of the valid parent questionnaires from W1 respondents). In W2, the children and adolescents had a mean age of 11.3 years (SD ± 2.3 years; range 8–15 years), 49.5% were boys.
Design
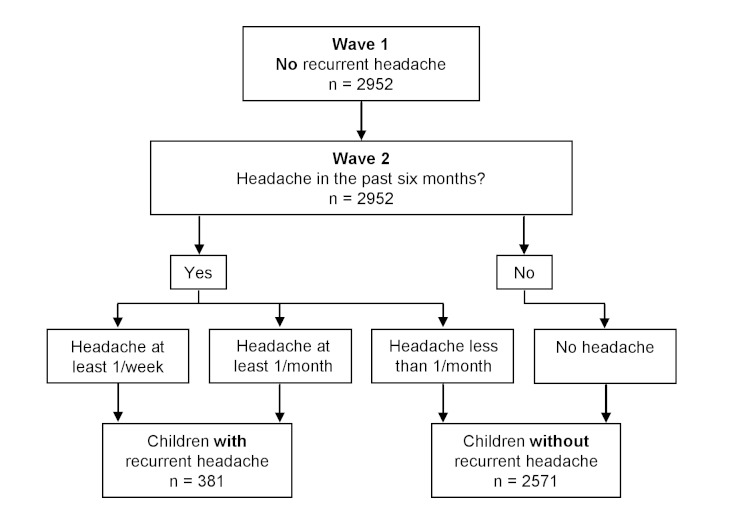
For both waves, W1 and W2, the children’s HA frequency as judged by their parents was grouped into four categories (no HA, <1/month, 1/month <1/week, ≥1/week). Only children who had no recurrent HA in W1 (i.e., HA either never or less than once per month in the preceding six months), but developed recurrent HA in W2 were included in the analyses (incidence sample). As can be seen in Figure 1 (Fig. 1), the criterion variable in W2 was defined as belonging to the group ‘recurrent HA’ (HA at least once per month in W2) as opposed to ‘no recurrent HA’ (HA less than once per month in W2). This categorisation was chosen because of its clinical relevance and because it is in line with categorisations utilised in other studies [48], [49], [50].
Figure 1. Longitudinal design and categorisation of the dependent variable (children with and without recurrent headache).
The predictor variables were assessed by several items of the parents’ questionnaire in W1 (see Attachment 1 for exact specifications of item content, number of items, internal consistency, and item sources). The predictors were grouped into the domains ‘school variables’ and ‘emotional and behavioural problems’. Since, due to their length, complete psychometric tests (for example Stressverarbeitungsfragebogen [51] for dysfunctional stress coping strategies) could not be adopted in the epidemiological study, it was necessary to select the most useful items to be included. This item selection was based on the criterion ‘largest item-scale correlation coefficient’ or ‘largest factor loadings’ in the original test analysis. In order to validate the scales thus shortened, a separate study was conducted on a sample of 250 children and the concordance with the original scales calculated. The validity of the selected items was demonstrated by the large correlations (.74≤r≤.96).
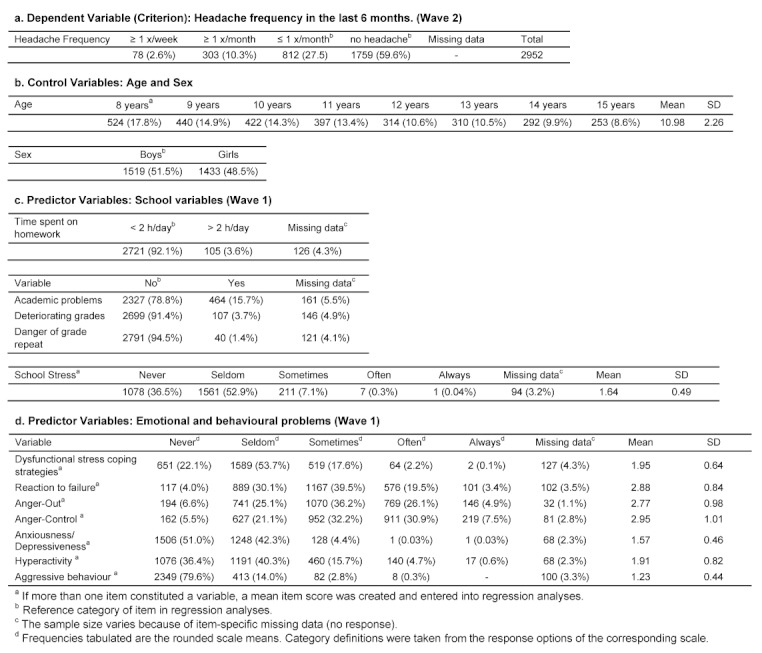
Descriptive statistics for all variables are listed in Table 1 (Tab. 1). Due to the satisfactory internal consistency (see Attachment 1; Cronbach’s Alpha, α≥0.6 [52]), the multi-item variables, which were assessed on 5-point rating scales, were combined into a mean scale score (see Table 1c-d (Tab. 1)). Higher values in the scale can be interpreted as unfavourable and lower values as favourable. The variable ‘time for homework’ was dichotomized (Table 1c (Tab. 1)) in order to distinguish between ‘spending much time’ and ‘spending little time’ on homework. The cut-off was arbitrarily set at ‘more/less than two hours per day’.
Table 1. Descriptive statistics for dependent, control and independent variables: Absolute frequencies (percentages provided in brackets). In this table only those children are included who had no HA in W1 but reported HA in W2 (incidence sample).
Statistical analyses
Before the data were analysed, an extensive data consolidation was undertaken. Data were crosschecked for correct data entry and examined for inconsistent answer patterns. From each wave to the next it was ascertained that the questionnaires referred to the same child (age/sex). Cases in which this could not be verified were excluded from further analyses. A binary logistic regression analysis with the criterion ‘no/recurrent HA’ and the predictor variables of the domains ‘school variables’ and ‘emotional and behavioural problems’ was carried out (method: Enter [53]). Cases with missing data were excluded from the analyses. Multicollinearity between the predictor variables could be excluded through appropriate diagnostics [54]; all variance inflation factor (VIF) values lay within the range 1–2.
First, age and sex were assessed with regard to their influence on the incidence of recurrent HA. Since sex appeared to be a meaningful predictor (see below), further analyses were conducted separately for boys and for girls. Age seemed to have only a very limited predictive power (see below) and was used as a control variable in the later analyses.
As the next step in the binary logistic regression analyses, every possible risk factor was analysed individually (age-adjusted single variable model) for its power to predict the incidence of recurrent HA [55]. After the univariable analyses, all variables with a p-value <.25 in the univariable analyses were entered into the multivariable regression model [55].
All statistical analyses were performed using SPSS software, version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
In W2, according to parents' responses, 49.5% (n=1908) of the children experienced no HA, 26.6% (n=1029) experienced HA <1/month, 17.1% (n=659) a minimum of 1/month and 6.8% (n=261) ≥1/week.
Univariable logistic regression analyses
Sex and age
In order to determine the impact of sex and age on the incidence of recurrent HA, both variables were initially examined for their influence in one model.
Girls were more likely to experience recurrent HA than boys (p<.001; OR=1.54; 95% confidence interval [CI]=1.24–1.92) and as age increased, children were more likely to report recurrent HA (p<.01; OR=1.07; 95% CI=1.02–1.12). Nagelkerke’s R2 amounted to 1.5%, indicating a poor fit of the model.
Sex-specific regression models (univariable analyses)
Boys
Univariable binary logistic regression analyses revealed that there were several significant factors that increased the risk for the incidence of HA for boys, namely: ‘academic problems’ (p<.05; OR=1.53; 95% CI=1.03–2.28), ‘school stress’ (p<.05; OR=1.34; 95% CI=1.02–1.75), ‘reaction to failure’ (p<.05; OR=1.35; 95% CI=1.12–1.62), ‘dysfunctional stress coping’ (p<.05; OR=1.53; 95% CI=1.2–1.92), ‘anxiousness/depressiveness’ (p<.05; OR=1.55; 95% CI=1.18–2.03) and ‘aggressive behaviour’ (p<.05; OR=1.42; 95% CI=1.10–1.83). The influence of age was controlled in each of the univariable models and shown to be irrelevant (all p’s>.05).
Girls
In the univariable model, all variables named above as relevant in boys were also relevant in girls, with the exception of ‘aggressive behaviour’ (p>.1; OR=0.91; 95% CI=0.60–1.39), namely: ‘academic problems’ (p<.05; OR=2.12; 95% CI=1.47–3.05), ‘school stress’ (p<.05; OR=1.44; 95% CI=1.13–1.82), ‘reaction to failure’ (p<.05; OR=1.29; 95% CI=1.09–1.52), ‘dysfunctional stress coping’ (p<.05; OR=1.72; 95% CI=1.41–2.09) and ‘anxiousness/depressiveness’ (p<.05; OR=1.75; 95% CI=1.38–2.23). Further predictive factors for girls were the variables ‘time spent on homework’ (p<.05; OR=0.35; 95% CI=0.13–0.99) and ‘deteriorating grades’ (p<.05; OR=2.15; 95% CI=1.11–4.18). In contrast to boys, age was shown to be a significant predictor for the incidence of HA in girls. However, the ORs for the influence of age ranged from 1.08 to 1.10, which is very low. As such, age appeared to have only a very limited effect on the incidence of recurrent HA.
Multivariable logistic regression analyses
Boys
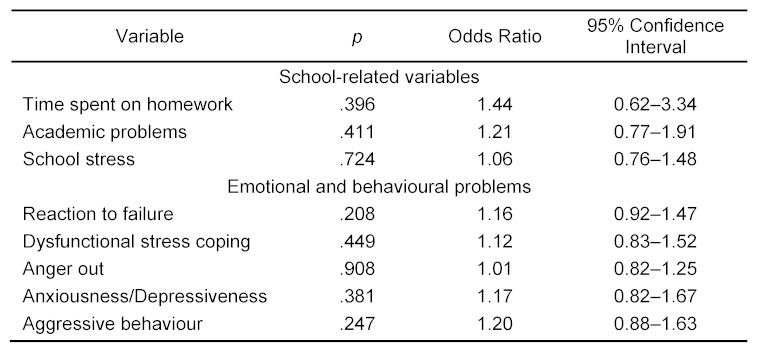
In the multivariable regression model, none of the variables contributed to the prediction of recurrent HA in boys (Table 2 (Tab. 2)).
Table 2. Summary of multivariable logistic regression analysis predicting the incidence of HA in boys .
(n=1310, 209 cases were excluded due to missing data), Nagelkerke R2=2.9%
Age also remained no longer significant in the multivariable model (p>.1; OR=1.07; 95% CI=0.99–1.16). The explained variance (Nagelkerke’s R2) was very low (2.9%).
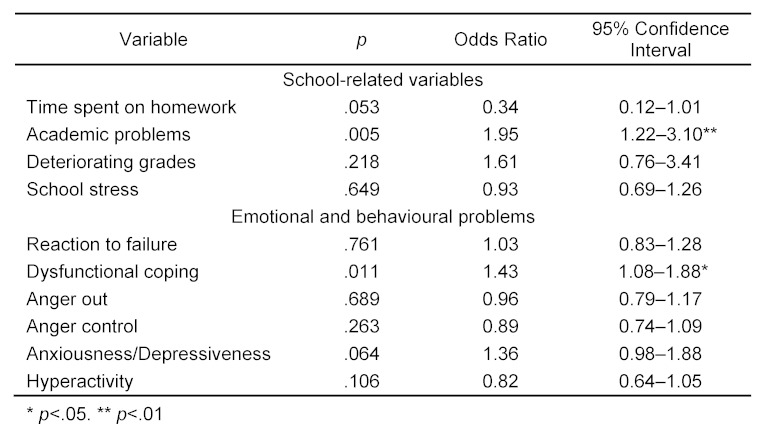
Girls
In a multivariable model, only ‘academic problems’ and ‘dysfunctional stress coping’ had an influence on the incidence of recurrent HA in girls after one year. The most powerful predictor was the variable ‘academic problems’: girls whose parents reported that their daughters suffered from academic problems had a 1.9 times increased chance of reporting recurrent HA (Table 3 (Tab. 3)).
Table 3. Summary of multivariable logistic regression analysis predicting the incidence of HA in girls .
(n=1216; 217 cases were excluded due to missing data). Nagelkerke R2=6.8%
Girls whose parents reported ‘dysfunctional stress coping’ for their daughters had a 1.4 times increased chance of reporting recurrent HA (Table 3 (Tab. 3)) compared to girls for whom the parents did not affirm dysfunctional coping. The multivariable model also revealed that age was not an explanatory factor (p>.1; OR=1.06; 95% CI=0.98–1.14). The two variables identified (‘academic problems’ and ‘dysfunctional stress coping’) accounted for only 6.8% (Nagelkerke’s R2) of the occurrence of recurrent HA, leaving 93.2% of the variability still to be accounted for by other factors.
Discussion
The present study set out to investigate whether psychosocial factors contribute to the prediction of the incidence of recurrent HA one year after the first assessment. Different risk profiles were found for boys and girls when the data were analysed separately. This result technically confirmed the hypothesis of sex-specific effects, but the variance explained by the model was very low. We found only a very slight effect of age on HA frequency in girls. It is an often reported finding, that from the age of 12 years onwards, girls experience HA more often than boys (e.g. [12]). These reports gave rise to the speculation that the increase of headache in girls might be the consequence of their pubertal development after the onset of menarche. Kröner-Herwig und Vath investigated this directly [56] and found only a relatively small impact (2.2% explained variance) of menarche on headache; this is in line with other authors (e.g. [12]).
In accordance with our hypotheses and the results of other publications [4], [10], the variables ‘academic problems’ and ‘dysfunctional stress coping’ were shown to be relevant to the incidence of paediatric HA in girls in a multivariable model. The data presented here show girls with ‘academic problems’ to be more likely to develop recurrent HA than those without such problems. The more often girls apply ‘dysfunctional stress coping strategies’, the higher the risk that they develop recurrent HA. Against our expectations based on the literature (see Introduction), none of the school-related factors or emotional and behavioural problems investigated were found to have an effect on the incidence of HA in boys when assessed in a multivariable model. Although the predictor variables examined had an influence on the outcome variable when investigated in isolation, this influence disappeared once further factors were taken into account, indicating that the variables shared some of the information with regard to the prediction of HA.
The majority of possible relationships described in the literature could not be substantiated through our analyses. In the present study, no evidence was found that factors such as the time required for homework, deteriorating grades, fear of being forced to repeat a year at school, stress at school or the examined emotional and behavioural problems represent risk factors for the incidence of paediatric HA. This result has to be seen in the context of the fact that the present sample is a general population sample, which by its nature is not very burdened regarding HA or the predictor variables (see Table 1 (Tab. 1), descriptive statistics). It is possible that some factors gain influence only once a certain level of intensity is reached. Many associations reported in the literature were studied in clinical populations that, naturally, were more severely affected (e.g. [57], [58]).
Moreover, there are some indications that parents may underestimate the HA frequency of their children [59], [60]. However, Kröner-Herwig et al. [61] showed that parents‘ reports are a more valid source for externally observable behaviour, whereas for internal cognitive-emotional processes the children’s reports are the most adequate source. The parents-children interrater reliability was lowest for depressive symptoms (r=.27), whereas the correlations between parents' reports and children’s reports regarding HA frequency were high (r=.65). In general, children’s self-reports mentioned more HA and other pain as well as somatic and depressive symptoms than their parents’ reports [61].
Although the majority of publications agree that those factors exert an influence on HA, there are a number of researchers who – in line with our results – failed to find connections between these factors and the occurrence of HA. Similar to the present study, Laurell et al. [3], did not find any connection between HA and the time spent on homework. Observations reported by Gordon et al. [10] and Santienello and co-authors [17] also show that bullying at school was not associated with frequent HA. The results presented here are also consistent with those of an Austrian group [62], who found no difference between children with migraine or TTH and healthy controls regarding school/workload stress. The authors concluded that migraine is not associated with family, home or school related factors [62], whereas TTH is associated with a higher rate of divorced parents and fewer peer relations.
The same situation obtains with regard to emotional and behavioural problems (for example anxiousness/depressiveness). Various authors found no relationship between HA and anxiety/depression [3], [31] or externalizing symptoms [27]. These results were corroborated by the data presented in this study. Aggression, conduct disorder and hyperactivity/inattention appeared not to be associated with weekly HA [10].
In the authors' opinion, the differences between some previous studies and the present findings result from the different methodological approaches, for example the study sample recruited (clinical vs. population sample, sample size), information sources (parental vs. children's responses), the criterion variable (incidence vs. occurrence) and its operationalisation (headache diagnosis vs. frequency), follow-up time and cross-sectional vs. longitudinal analyses.
Strengths and limitations
The large, population-based sample allows for the drawing of conclusions about the general population and avoids a bias resulting from the observation of samples from clinical subgroups of patients, who already use the healthcare system. Children who already sought medical help for their condition may suffer from stronger HA and may reasonably be expected to have patterns of experiences and behaviour distinct from children with moderate or less impairing HA [3].
Longitudinal studies, which are ideal for analysing factors that predict HA, rather than merely accompany HA, are only seldom carried out. The unidirectional design regarding the incidence of symptoms has, to the best of our knowledge, been used only in a few studies to date (e.g., [63]). Other longitudinal studies concentrate on changes in the HA diagnosis or relate to symptoms and risk factors that are not the focus of the present study (e.g., [30], [64], [65]).
The present study focused exclusively on the incidence of HA, by concentrating on children who had no recurrent HA in W1 and developed HA over the following year. This constitutes a very strict criterion. It was chosen in order to disengage the psychosocial factors that might be causative factors for the development of HA from those factors that are simply correlated with HA, since temporal precedence is a necessary, albeit not sufficient condition, for such a causal role. The conclusion that most of the psychosocial factors investigated do not appear to precede the development of HA has to be drawn with great caution, since a number of possible limitations has to be taken into consideration.
Firstly, this article reports data from a one-year follow-up. It is possible that the effects of some factors will only become apparent after a longer follow-up interval.
Secondly, in the present study, the focus lay on the frequency of HA rather than the different types of HA (migraine, TTH). The reason for this approach was that diagnoses based on conclusions drawn from questionnaire data have been criticised, and the use of interviews has instead been advocated [66]. In addition, there is evidence to suggest that parents and children generally find it difficult to differentiate between some symptoms, leading to around 20%–30% of HA that have to remain unclassified in epidemiological studies [45], [67].
Thirdly, we explored parents’ reports because they formed a more extensive data base and also permitted to make statements about younger children (<9 years). It is possible that we would have reached different conclusions if we had used the children’s reports. Moreover, as in most epidemiological studies, it was not feasible to use HA diaries/protocols or other means designed to minimize recall biases routinely used in clinical studies.
Fourthly, although the response rate of 47.3% related to the original sample in Wave 1 is comparable to response rates achieved in other studies that did not rely on school-based surveys [1], [25], one might argue that it is nevertheless rather low, which may limit the representativeness of the results.
Finally, a selection bias due to non-response of a specific group in Wave 2 cannot be ruled out. Parents whose child had HA, or parents who had HA themselves, may have been more likely to respond than parents who were HA-free or whose children were HA-free. This bias should result in an overestimation of the prevalence of paediatric HA. Such an overestimation was not confirmed, however, as most of our figures regarding prevalence tended to be lower than in other studies.
Conclusion
Our analyses show that the majority of the selected psychosocial variables do not signal an increased risk for the incidence of recurrent HA. With the exception of dysfunctional stress coping and academic problems, which seemed to have a small influence in girls, rigorous testing in an incidence sample rejected a causal role for school-related and psychological factors in the development of HA in children and adolescents.
Notes
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
This research project is a component project of the Research Association of the German Headache Konsortium under the direction of Professor Dr. med. H.C. Diener, Essen, and is supported by the German Federal Ministry of Education and Research (BMBF), grant number 01EM0521.
Erratum
Fig. 1 has been replaced by a corrected version.
Supplementary Material
References
- 1.Camarda R, Monastero R, Santangelo G, Raimondo D, Puma D, Pipia C, Camarda LK, Camarda C, Raieli V. Migraine headaches in adolescents: a five-year follow-up study. Headache. 2002 Nov-Dec;42(10):1000–1005. doi: 10.1046/j.1526-4610.2002.02229.x. Available from: http://dx.doi.org/10.1046/j.1526-4610.2002.02229.x. [DOI] [PubMed] [Google Scholar]
- 2.Laurell K, Larsson B, Mattsson P, Eeg-Olofsson O. A 3-year follow-up of headache diagnoses and symptoms in Swedish schoolchildren. Cephalalgia. 2006 Jul;26(7):809–815. doi: 10.1111/j.1468-2982.2006.01113.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.2006.01113.x. [DOI] [PubMed] [Google Scholar]
- 3.Laurell K, Larsson B, Eeg-Olofsson O. Headache in schoolchildren: association with other pain, family history and psychosocial factors. Pain. 2005 Dec;119(1-3):150–158. doi: 10.1016/j.pain.2005.09.030. Available from: http://dx.doi.org/10.1016/j.pain.2005.09.030. [DOI] [PubMed] [Google Scholar]
- 4.Metsähonkala L, Sillanpää M, Tuominen J. Social environment and headache in 8- to 9-year-old children: a follow-up study. Headache. 1998 Mar;38(3):222–228. doi: 10.1046/j.1526-4610.1998.3803222.x. Available from: http://dx.doi.org/10.1046/j.1526-4610.1998.3803222.x. [DOI] [PubMed] [Google Scholar]
- 5.Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain. 2004 Jun;8(3):187–199. doi: 10.1016/j.ejpain.2003.08.001. Available from: http://dx.doi.org/10.1016/j.ejpain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Connelly M. Recurrent pediatric headache: A comprehensive review. Child Health Care. 2003;32(3):153–189. doi: 10.1207/S15326888CHC3203_1. Available from: http://dx.doi.org/10.1207/S15326888CHC3203_1. [DOI] [Google Scholar]
- 7.Cevoli S, Sancisi E, Pierangeli G, Grimaldi D, Zanigni S, Nicodemo M, Cortelli P, Montagna P. Chronic daily headache: risk factors and pathogenetic considerations. Neurol Sci. 2006 May;27 Suppl 2:S168–S173. doi: 10.1007/s10072-006-0595-x. Available from: http://dx.doi.org/10.1007/s10072-006-0595-x. [DOI] [PubMed] [Google Scholar]
- 8.Anttila P, Metsähonkala L, Sillanpää M. School start and occurrence of headache. Pediatrics. 1999 Jun;103(6):e80. doi: 10.1542/peds.103.6.e80. Available from: http://dx.doi.org/10.1542/peds.103.6.e80. [DOI] [PubMed] [Google Scholar]
- 9.Bandell-Hoekstra I, Abu-Saad HH, Passchier J, Knipschild P. Recurrent headache, coping, and quality of life in children: a review. Headache. 2000 May;40(5):357–370. doi: 10.1046/j.1526-4610.2000.00054.x. Available from: http://dx.doi.org/10.1046/j.1526-4610.2000.00054.x. [DOI] [PubMed] [Google Scholar]
- 10.Gordon KE, Dooley JM, Wood EP. Self-reported headache frequency and features associated with frequent headaches in Canadian young adolescents. Headache. 2004 Jun;44(6):555–561. doi: 10.1111/j.1526-4610.2004.446003.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2004.446003.x. [DOI] [PubMed] [Google Scholar]
- 11.Rhee H. Risk factors for and sequelae of headaches in schoolchildren with clinical implications from a psychosocial perspective. J Pediatr Nurs. 2001 Dec;16(6):392–401. doi: 10.1053/jpdn.2001.27879. Available from: http://dx.doi.org/10.1053/jpdn.2001.27879. [DOI] [PubMed] [Google Scholar]
- 12.Passchier J, Orlebeke JF. Headaches and stress in schoolchildren: an epidemiological study. Cephalalgia. 1985 Sep;5(3):167–176. doi: 10.1046/j.1468-2982.1985.0503167.x. Available from: http://dx.doi.org/10.1046/j.1468-2982.1985.0503167.x. [DOI] [PubMed] [Google Scholar]
- 13.Torsheim T, Wold B. School-related stress, school support, and somatic complaints: A general population study. J Adolesc Res. 2001;16(3):293–303. doi: 10.1177/0743558401163003. Available from: http://dx.doi.org/10.1177/0743558401163003. [DOI] [Google Scholar]
- 14.Larsson B, Melin L. The psychological treatment of recurrent headache in adolescents--short-term outcome and its prediction. Headache. 1988 Apr;28(3):187–195. doi: 10.1111/j.1526-4610.1988.hed2803187.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.1988.hed2803187.x. [DOI] [PubMed] [Google Scholar]
- 15.Brattberg G. The incidence of back pain and headache among Swedish school children. Qual Life Res. 1994 Dec;3 Suppl 1:S27–S31. doi: 10.1007/BF00433372. Available from: http://dx.doi.org/10.1007/BF00433372. [DOI] [PubMed] [Google Scholar]
- 16.Fekkes M, Pijpers FI, Verloove-Vanhorick SP. Bullying behavior and associations with psychosomatic complaints and depression in victims. J Pediatr. 2004 Jan;144(1):17–22. doi: 10.1016/j.jpeds.2003.09.025. Available from: http://dx.doi.org/10.1016/j.jpeds.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 17.Santinello M, Vieno A, De Vogli R. Primary headache in Italian early adolescents: the role of perceived teacher unfairness. Headache. 2009 Mar;49(3):366–374. doi: 10.1111/j.1526-4610.2008.01208.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2008.01208.x. [DOI] [PubMed] [Google Scholar]
- 18.Bandell-Hoekstra IE, Abu-Saad HH, Passchier J, Frederiks CM, Feron FJ, Knipschild P. Coping and Quality of Life in relation to headache in Dutch schoolchildren. Eur J Pain. 2002;6(4):315–321. doi: 10.1053/eujp.2002.0343. Available from: http://dx.doi.org/10.1053/eujp.2002.0343. [DOI] [PubMed] [Google Scholar]
- 19.Björling EA. The momentary relationship between stress and headaches in adolescent girls. Headache. 2009 Sep;49(8):1186–1197. doi: 10.1111/j.1526-4610.2009.01406.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2009.01406.x. [DOI] [PubMed] [Google Scholar]
- 20.Houle T, Nash JM. Stress and headache chronification. Headache. 2008;48(1):40–44. doi: 10.1111/j.1526-4610.2007.00973.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2007.00973.x. [DOI] [PubMed] [Google Scholar]
- 21.Saile H, Scalla P. Chronische Kopfschmerzen und Stress bei Kindern. Z Klin Psychol Psychother. 2006;35:188–195. doi: 10.1026/1616-3443.35.3.188. Available from: http://dx.doi.org/10.1026/1616-3443.35.3.188. [DOI] [Google Scholar]
- 22.Fichtel A, Larsson B. Psychosocial impact of headache and comorbidity with other pains among Swedish school adolescents. Headache. 2002 Sep;42(8):766–775. doi: 10.1046/j.1526-4610.2002.02178.x. Available from: http://dx.doi.org/10.1046/j.1526-4610.2002.02178.x. [DOI] [PubMed] [Google Scholar]
- 23.Martin-Herz SP, Smith MS, McMahon RJ. Psychosocial factors associated with headache in Junior High School students. J Pediatr Psychol. 1999;24(1):13–23. doi: 10.1093/jpepsy/24.1.13. Available from: http://dx.doi.org/10.1093/jpepsy/24.1.13. [DOI] [Google Scholar]
- 24.Egger HL, Angold A, Costello EJ. Headaches and psychopathology in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1998 Sep;37(9):951–958. doi: 10.1097/00004583-199809000-00015. Available from: http://dx.doi.org/10.1097/00004583-199809000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Fearon P, Hotopf M. Relation between headache in childhood and physical and psychiatric symptoms in adulthood: national birth cohort study. BMJ. 2001 May;322(7295):1145. doi: 10.1136/bmj.322.7295.1145. Available from: http://dx.doi.org/10.1136/bmj.322.7295.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pine DS, Cohen P, Brook J. The association between major depression and headache: results of a longitudinal epidemiologic study in youth. J Child Adolesc Psychopharmacol. 1996;6(3):153–164. doi: 10.1089/cap.1996.6.153. Available from: http://dx.doi.org/10.1089/cap.1996.6.153. [DOI] [PubMed] [Google Scholar]
- 27.Larsson B, Sund AM. One-year incidence, course, and outcome predictors of frequent headaches among early adolescents. Headache. 2005 Jun;45(6):684–691. doi: 10.1111/j.1526-4610.2005.05137a.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2005.05137a.x. [DOI] [PubMed] [Google Scholar]
- 28.Rhee H. Prevalence and predictors of headaches in US adolescents. Headache. 2000 Jul-Aug;40(7):528–538. doi: 10.1046/j.1526-4610.2000.00084.x. Available from: http://dx.doi.org/10.1046/j.1526-4610.2000.00084.x. [DOI] [PubMed] [Google Scholar]
- 29.Martin PR. Psychological Management of Chronic Headaches. New York: Guilford Press; 1993. [Google Scholar]
- 30.Lateef TM, Merikangas KR, He J, Kalaydjian A, Khoromi S, Knight E, Nelson KB. Headache in a national sample of American children: prevalence and comorbidity. J Child Neurol. 2009 May;24(5):536–543. doi: 10.1177/0883073808327831. Available from: http://dx.doi.org/10.1177/0883073808327831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Virtanen R, Aromaa M, Koskenvuo M, Sillanpää M, Pulkkinen L, Metsähonkala L, Suominen S, Rose RJ, Helenius H, Kaprio J. Externalizing problem behaviors and headache: a follow-up study of adolescent Finnish twins. Pediatrics. 2004 Oct;114(4):981–987. doi: 10.1542/peds.2003-1103-L. Available from: http://dx.doi.org/10.1542/peds.2003-1103-L. [DOI] [PubMed] [Google Scholar]
- 32.Virtanen R, Aromaa M, Rautava P, Metsähonkala L, Anttila P, Helenius H, Sillanpää M. Changes in headache prevalence between pre-school and pre-pubertal ages. Cephalalgia. 2002 Apr;22(3):179–185. doi: 10.1046/j.1468-2982.2002.00337.x. Available from: http://dx.doi.org/10.1046/j.1468-2982.2002.00337.x. [DOI] [PubMed] [Google Scholar]
- 33.White KS, Farrell AD. Anxiety and psychosocial stress as predictors of headache and abdominal pain in urban early adolescents. J Pediatr Psychol. 2006 Jul;31(6):582–596. doi: 10.1093/jpepsy/jsj050. Available from: http://dx.doi.org/10.1093/jpepsy/jsj050. [DOI] [PubMed] [Google Scholar]
- 34.Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, Bohnen AM, van Suijlekom-Smit LW, Passchier J, van der Wouden JC. Pain in children and adolescents: a common experience. Pain. 2000 Jul;87(1):51–58. doi: 10.1016/S0304-3959(00)00269-4. Available from: http://dx.doi.org/10.1016/S0304-3959(00)00269-4. [DOI] [PubMed] [Google Scholar]
- 35.Rasmussen BK, Jensen R, Schroll M, Olesen J. Interrelations between migraine and tension-type headache in the general population. Arch. Neurol. 1992 Sep;49(9):914–918. doi: 10.1001/archneur.1992.00530330036012. Available from: http://dx.doi.org/10.1001/archneur.1992.00530330036012. [DOI] [PubMed] [Google Scholar]
- 36.Sillanpää M, Aro H. Headache in teenagers: comorbidity and prognosis. Funct. Neurol. 2000;15 Suppl 3:116–121. [PubMed] [Google Scholar]
- 37.Siniatchkin M, Gerber WD. Die Rolle der Familie in der Entstehung neurophysiologischer Auffälligkeiten bei Kindern mit Migräne. [Role of family in development of neurophysiological manifestations in children with migraine]. Prax Kinderpsychol Kinderpsychiatr. 2002 Mar;51(3):194–208. (Ger). [PubMed] [Google Scholar]
- 38.Aromaa M, Rautava P, Sillanpää M, Helenius H, Ojanlatva A. Familial occurrence of headache. Cephalalgia. 1999 Dec;19 Suppl 25:49–52. doi: 10.1177/0333102499019s2513. [DOI] [PubMed] [Google Scholar]
- 39.McGrath PA, Hillier LM. Recurrent headache: Triggers, causes, and contributing factors. In: McGrath PA, Hillier LM, editors. The child with headache: Diagnosis and treatment. Seattle, WA: IASP Press; 2001. pp. 77–107. [Google Scholar]
- 40.Bille BS. Migraine in school children. A study of the incidence and short-term prognosis, and a clinical, psychological and electroencephalographic comparison between children with migraine and matched controls. Acta Paediatr Suppl. 1962 May;136:1–151. [PubMed] [Google Scholar]
- 41.Linna SL, Moilanen I, Keistinen H, Ernvall ML, Karppinen MM. Prevalence of psychosomatic symptoms in children. Psychother Psychosom. 1991;56(1-2):85–87. doi: 10.1159/000288535. Available from: http://dx.doi.org/10.1159/000288535. [DOI] [PubMed] [Google Scholar]
- 42.Shivpuri D, Rajesh MS, Jain D. Prevalence and characteristics of migraine among adolescents: a questionnaire survey. Indian Pediatr. 2003 Jul;40(7):665–669. [PubMed] [Google Scholar]
- 43.Waldie KE. Childhood headache, stress in adolescence, and primary headache in young adulthood: a longitudinal cohort study. Headache. 2001 Jan;41(1):1–10. doi: 10.1046/j.1526-4610.2001.111006001.x. Available from: http://dx.doi.org/10.1046/j.1526-4610.2001.111006001.x. [DOI] [PubMed] [Google Scholar]
- 44.Gassmann J, Morris L, Heinrich M, Kröner-Herwig B. One-year course of paediatric headache in children and adolescents aged 8-15 years. Cephalalgia. 2008 Nov;28(11):1154–1162. doi: 10.1111/j.1468-2982.2008.01657.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.2008.01657.x. [DOI] [PubMed] [Google Scholar]
- 45.Heinrich M, Morris L, Kröner-Herwig B. Self-report of headache in children and adolescents in Germany: possibilities and confines of questionnaire data for headache classification. Cephalalgia. 2009 Aug;29(8):864–872. doi: 10.1111/j.1468-2982.2008.01812.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.2008.01812.x. [DOI] [PubMed] [Google Scholar]
- 46.Kröner-Herwig B, Heinrich M, Morris L. Headache in German children and adolescents: a population-based epidemiological study. Cephalalgia. 2007 Jun;27(6):519–527. doi: 10.1111/j.1468-2982.2007.01319.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.2007.01319.x. [DOI] [PubMed] [Google Scholar]
- 47.Kröner-Herwig B, Morris L, Heinrich M. Biopsychosocial correlates of headache: what predicts pediatric headache occurrence? Headache. 2008 Apr;48(4):529–544. doi: 10.1111/j.1526-4610.2007.00945.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2007.00945.x. [DOI] [PubMed] [Google Scholar]
- 48.Carlsson J. Prevalence of headache in schoolchildren: relation to family and school factors. Acta Paediatr. 1996 Jun;85(6):692–696. doi: 10.1111/j.1651-2227.1996.tb14128.x. Available from: http://dx.doi.org/10.1111/j.1651-2227.1996.tb14128.x. [DOI] [PubMed] [Google Scholar]
- 49.King NJ, Sharpley CF. Headache activity in children and adolescents. J Paediatr Child Health. 1990 Feb;26(1):50–54. doi: 10.1111/j.1440-1754.1990.tb02379.x. Available from: http://dx.doi.org/10.1111/j.1440-1754.1990.tb02379.x. [DOI] [PubMed] [Google Scholar]
- 50.Kristjánsdóttir G, Wahlberg V. Sociodemographic differences in the prevalence of self-reported headache in Icelandic school-children. Headache. 1993 Jul-Aug;33(7):376–380. doi: 10.1111/j.1526-4610.1993.hed3307376.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.1993.hed3307376.x. [DOI] [PubMed] [Google Scholar]
- 51.Hampel P, Petermann F, Dickow B. Stressverarbeitungsfragebogen von Janke und Erdmann angepasst für Kinder und Jugendliche (SVF-KJ) Göttingen, Germany: Hogrefe; 2001. [Google Scholar]
- 52.Kline P. The Handbook of Psychological Testing. London, New York: Routledge; 1999. [Google Scholar]
- 53.Field A. Discovering Statistics Using SPSS. Third ed. London: Sage; 2009. p. Third ed. [Google Scholar]
- 54.Tabachnick B, Fidell LS. Using Multivariate Statistics. 4 ed. Boston: Allyn and Bacon; 2001. pp. 88–91. [Google Scholar]
- 55.Hosmer DW, Lemeshow S. Applied Logistic Regression. Second ed. New York: John Wiley & Sons, Inc.; 2000. Available from: http://dx.doi.org/10.1002/0471722146. [DOI] [Google Scholar]
- 56.Kröner-Herwig B, Vath N. Menarche in girls and headache--a longitudinal analysis. Headache. 2009 Jun;49(6):860–867. doi: 10.1111/j.1526-4610.2009.01397.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2009.01397.x. [DOI] [PubMed] [Google Scholar]
- 57.Just U, Oelkers R, Bender S, Parzer P, Ebinger F, Weisbrod M, Resch F. Emotional and behavioural problems in children and adolescents with primary headache. Cephalalgia. 2003 Apr;23(3):206–213. doi: 10.1046/j.1468-2982.2003.00486.x. Available from: http://dx.doi.org/10.1046/j.1468-2982.2003.00486.x. [DOI] [PubMed] [Google Scholar]
- 58.Radat F, Mekies C, Géraud G, Valade D, Vivès E, Lucas C, Joubert JM, Lantéri-Minet M. Anxiety, stress and coping behaviours in primary care migraine patients: results of the SMILE study. Cephalalgia. 2008 Nov;28(11):1115–1125. doi: 10.1111/j.1468-2982.2008.01644.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.2008.01644.x. [DOI] [PubMed] [Google Scholar]
- 59.Lundqvist C, Clench-Aas J, Hofoss D, Bartonova A. Self-reported headache in schoolchildren: parents underestimate their children's headaches. Acta Paediatr. 2006 Aug;95(8):940–946. doi: 10.1080/08035250600678810. Available from: http://dx.doi.org/10.1080/08035250600678810. [DOI] [PubMed] [Google Scholar]
- 60.Nakamura EF, Cui L, Lateef T, Nelson KB, Merikangas KR. Parent-child agreement in the reporting of headaches in a national sample of adolescents. J Child Neurol. 2012 Jan;27(1):61–67. doi: 10.1177/0883073811413580. Available from: http://dx.doi.org/10.1177/0883073811413580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kröner-Herwig B, Morris L, Heinrich M, Gassmann J, Vath N. Agreement of parents and children on characteristics of pediatric headache, other pains, somatic symptoms, and depressive symptoms in an epidemiologic study. Clin J Pain. 2009 Jan;25(1):58–64. doi: 10.1097/AJP.0b013e31817fc62d. Available from: http://dx.doi.org/10.1097/AJP.0b013e31817fc62d. [DOI] [PubMed] [Google Scholar]
- 62.Karwautz A, Wöber C, Lang T, Böck A, Wagner-Ennsgraber C, Vesely C, Kienbacher C, Wöber-Bingöl C. Psychosocial factors in children and adolescents with migraine and tension-type headache: a controlled study and review of the literature. Cephalalgia. 1999 Jan;19(1):32–43. doi: 10.1111/j.1468-2982.1999.1901032.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.1999.1901032.x. [DOI] [PubMed] [Google Scholar]
- 63.Boardman HF, Thomas E, Millson DS, Croft PR. The natural history of headache: predictors of onset and recovery. Cephalalgia. 2006 Sep;26(9):1080–1088. doi: 10.1111/j.1468-2982.2006.01166.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.2006.01166.x. [DOI] [PubMed] [Google Scholar]
- 64.Laimi K, Vahlberg T, Salminen J, Metsähonkala L, Mikkelsson M, Anttila P, Aromaa M, Sillanpää M. Does neck pain determine the outcome of adolescent headache? Cephalalgia. 2007 Mar;27(3):244–253. doi: 10.1111/j.1468-2982.2006.01266.x. Available from: http://dx.doi.org/10.1111/j.1468-2982.2006.01266.x. [DOI] [PubMed] [Google Scholar]
- 65.Von Korff M, Le Resche L, Dworkin SF. First onset of common pain symptoms: a prospective study of depression as a risk factor. Pain. 1993 Nov;55(2):251–258. doi: 10.1016/0304-3959(93)90154-H. Available from: http://dx.doi.org/10.1016/0304-3959(93)90154-H. [DOI] [PubMed] [Google Scholar]
- 66.Rasmussen BK, Jensen R, Olesen J. Questionnaire versus clinical interview in the diagnosis of headache. Headache. 1991 May;31(5):290–295. doi: 10.1111/j.1526-4610.1991.hed3105290.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.1991.hed3105290.x. [DOI] [PubMed] [Google Scholar]
- 67.Wiendels NJ, van der Geest MC, Neven AK, Ferrari MD, Laan LA. Chronic daily headache in children and adolescents. Headache. 2005 Jun;45(6):678–683. doi: 10.1111/j.1526-4610.2005.05137.x. Available from: http://dx.doi.org/10.1111/j.1526-4610.2005.05137.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.