Abstract
Objectives
To analyse costs and consequences of changing physical activity behaviour due to the “Physical Activity on Prescription” (PAP) programme.
Design
A randomized controlled trial with a four-month intervention, with comparison between intervention and control group.
Intervention
The PAP programme, with exercise twice a week, education, and motivational counselling.
Subjects
525 sedentary individuals, 20–80 years (intervention group n = 268, control group n = 257), with lifestyle-related health problems. A total of 245 returned for the four-month assessment.
Main outcome measure
Programme costs based on intention-to-treat estimations, direct and indirect costs of inactivity, and physical activity behaviour analysed with IPAQ (International Physical Activity Questionnaire), self-reported physical activity, and measures of functional capacity.
Results
The intention-to-treat programme costs for the four-month programme period was SEK (Swedish Kronor) 6475 (€ [Euro] 684) for the intervention group and SEK 3038 (€ 321) for the control group. Of this, healthcare providers’ costs were 24% in the intervention group, and 31% in the control group. The physical activity behaviour was significantly improved in both groups, but no differences were found between the groups.
Implications
The largest share of the PAP programme costs was the participants’ costs. Significant improvements were shown in physical activity behaviour in both groups, but no differences were found between the intervention and control groups. Due to many non-completers, the potential for improvements of the motivating assignment with sedentary individuals in primary healthcare is obvious. Long-term follow-up can determine the sustainability of the results, and can be used in a future cost-effectiveness analysis.
Keywords: Costs, primary healthcare, Physical Activity on Prescription, RCT study
Almost 40% of the Swedish population was in 2006 insufficiently physically active, implying a substantial individual and societal health burden [1–7]. The estimated costs of inactivity were SEK 6000 million in 2002 in Sweden, including costs for production loss and healthcare [8]. Scientific evidence supports physical activity as a preventive and therapeutic measure of inactivity-related chronic conditions [1,2,9–12]. The “Physical Activity on Prescription” (PAP) programme aims to increase the physical activity level among sedentary adults, and has not been evaluated from a health-economic perspective looking at costs and consequences [11,13–16]. Several studies have estimated the cost-effectiveness of physical activity interventions, but the evidence for this is limited [17–20].
The aim of this paper was to analyse the costs and consequences of changing physical activity behaviour through the four-month PAP programme by comparing a high-intensity group (intervention) and low-intensity group (control).
Material and methods
The study was a randomized controlled trial with a four-month intervention with comparison between an intervention and a control group. Participant outcomes were evaluated before intervention and after four months. Written consent was obtained from all participants. The study protocol was approved by the Ethical Committee of Research at the University of Lund.
Costs and consequences of changing physical activity through the “Physical activity on Prescription” programme were studied in this RCT.
Healthcare providers were responsible for 28% of the costs. Participants’ contribution – leisure time and travelling – was the largest share.
The cost offset due to decreased inactivity is for both groups SEK 241 200 (€ 25 497) every year.
Both intervention and control group showed significantly improved physical activity behaviour, but no differences were found between the groups.
Sample
Participants were recruited in primary healthcare from five municipalities in the South-East Healthcare District of Skåne Region, Sweden. Starting in February 2006 participants were recruited continuously until December 2007 as all those who received a prescription for physical activity from a physician, nurse, physiotherapist, occupational therapist, welfare officer, or nutritionist. Criteria for having a prescription were: being at least 18 years old, having a sedentary lifestyle and one or more of the following diseases: cardiovascular disease, type 2 diabetes, obesity, musculoskeletal pain and disorders, mental illness, or respiratory problems.
Intervention
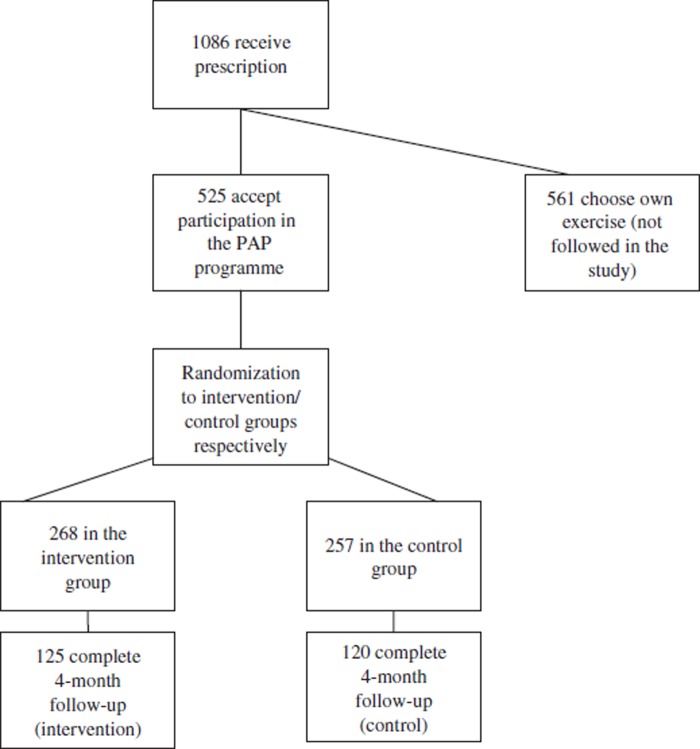
The randomization process, using closed envelopes, was performed by the physiotherapists before the functional testing of the participants. Of the 525 participants randomised to either intervention or control group, 245 returned for the four-month assessment (Figure 1). The share of dropouts was for both groups 53%. Participants randomized to the intervention group had two supervised exercise sessions (45 to 60 minutes) in local sport clubs twice a week, two hours’ education in physical activity and individual motivational counselling performed by physiotherapists [21]. They were also instructed to exercise additionally once a week on their own with an activity lasting at least 30 minutes and at least on a moderate level. The control group obtained written information about the possibility to participate in supervised exercise once a week on a moderately intense level. Results were reported from a societal perspective [22].
Figure 1.
Flow chart showing the prescription, randomization, and participation rates of the participants.
Direct and indirect costs of physical inactivity
The estimated total costs of inactivity in Sweden on at the 2002 price level were between SEK 5820 and 6902 million [23]. In 2002 the Swedish population comprised 8 940 788 persons, and 6 999 878 were aged 18 years and older [24]. A prevalence of inactivity of 40% is equal to 2 799 951 persons, and means a cost of ∼SEK 2265 per inactive person in the year of 2002. Transferred to the 2007 price level with the Swedish consumer price index, the cost is SEK 2412 per inactive person, and is a cost to society which a sufficient physically active person does not carry. Based on this calculation, we can estimate the indirect and direct costs of the inactive and active individuals respectively before and after participation in the PAP programme.
Main outcome measures
Three different methods were used to classify inactive vs active physical activity behaviour: self-rated physical activity with the IPAQ (International Physical Activity Questionnaire) short form, self-reported physical activity level, and a functional test with the Six-Minute Walk Test [25–27]. The IPAQ short form protocol assesses MET values of walking, moderate-intensity activities, and vigorous activities, and the average MET minutes was used in the analysis [28,29]. The second method, a single question of present extent of physical activity level, is based on the Transtheoretical Model, and the five levels were dichotomized into “active” and “inactive” for the further analysis [30]. The third method was the Six-Minute Walk Test; the participant walked as fast as possible during six minutes, and the distance (metres) covered was measured [31]. The outcomes also included an exercise diary to measure compliance.
Self-reported costs of the individual associated with the programme included exercise equipment purchased, travelling and travel time costs to and from exercise, and injuries due to the programme. Participants’ exercise and travel time cost is a mean value, calculated on the basis of the self-reported monthly gross salary and working hours. The exercise was performed in participants’ leisure time. The costs of the exercise in the different sport clubs in the area include staff time for exercise instructors and rent of facilities. Each participant visited the physiotherapist twice (for the intervention group an additional 20 minutes’ time for the motivational counselling), at baseline and at four months. For the non-completers the costs were based on the assumption that the majority of them dropped out within the first month, implying that the first month's costs were same for both completers and non-completers.
Statistical analyses
Means and standard deviations as well as relative frequencies (%) were used to describe the sample. Differences at baseline between intervention and control groups were tested with t-tests with regard to age, BMI, and income, and with chi-squared tests with regard to sex, education, and health. Due to skew distributions the Mann–Whitney U-test was used for comparisons between intervention and control groups with regard to MET minutes and the Six-Minute Walk Test, while Wilcoxon's signed rank test was used for comparisons between baseline and the four-month follow-up. Chi-squared tests were used for comparisons between intervention and control groups with regard to physical inactivity. McNemar's test was used to test change in inacti vity between baseline and four-month follow up. Statistical significance was set at p < 0.05.
Resource utilization and costs
In the following estimation of the costs within the PAP programme, we designated the value of resources used rather than expenses. All costs are reported in Swedish Kronor (SEK).
Programme costs and quantities
Baseline analyses showed no significant differences between the groups in age, BMI, income, education level, or self-perceived health (Table I). The programme costs for the four-month intervention period were based on intention-to-treat estimations and are presented in Table II.
Table I.
Baseline characteristics of the completers and non-completers (baseline only): Differences between intervention and control groups are tested.
| Completers (n = 245) |
Non-completers (n = 280) |
|||||
| Intervention n = 1251 | Control n = 1202 | p-value | Intervention n = 1433 | Control n = 1374 | p-value | |
| Sex (%) | 0.3945 | 0.1235 | ||||
| Women | 70.4 | 66.7 | 63.6 | 72.3 | ||
| Men | 29.6 | 33.3 | 36.4 | 27.7 | ||
| Age (years) | 0.5916 | 0.6796 | ||||
| Mean (SD) | 55.2 (12.5) | 54.4 (13.2) | 49.7 (13.9) | 49.0 (13.5) | ||
| Range | 20–80 | 22–79 | 19–81 | 18–84 | ||
| BMI (kg/m2) | 0.6356 | 0.2736 | ||||
| Mean (SD) | 31.5 (5.8) | 31.8 (6.7) | 32.4 (6.2) | 33.3 (7.0) | ||
| Range | 18.0–50.0 | 19.8–55.0 | 19.4–60.7 | 19.7–55.6 | ||
| Income (SKr) | 0.5386 | |||||
| Mean (SD) | 15 440 (7 027)1 | 14 805 (6 811)2 | n.a.7 | n.a.7 | ||
| Range | 0–40 300 | 0–37 500 | ||||
| Education level (%) | 0.8525 | 0.7205 | ||||
| Nine-year compulsory school | 36.8 | 33.3 | 30.5 | 34.1 | ||
| 2 years upper secondary school | 20.0 | 25.0 | 21.3 | 18.5 | ||
| 3 years upper secondary school | 24.8 | 22.5 | 27.0 | 26.7 | ||
| University or college | 18.4 | 19.2 | 21.3 | 20.7 | ||
| Health (%) | 0.8585 | 0.2995 | ||||
| Poor | 8.9 | 9.2 | 18.3 | 19.7 | ||
| Somewhat poor | 50.0 | 50.8 | 51.4 | 51.8 | ||
| Good | 31.5 | 30.0 | 21.8 | 25.5 | ||
| Very good | 8.1 | 9.2 | 7.0 | 2.9 | ||
| Excellent | 1.6 | 0.8 | 1.4 | 0 | ||
Notes: 1Due to missing values n varies between 90 and 125; 2due to missing values n varies between 91 and 120; 3due to missing values n varies between 139 and 143; 4due to missing values n varies between 134 and 137; 5chi-squared test, linear-by-linear association; 6t-test 1: n = 84, 2: n = 86; 7not available.
Table II.
Intention-to-treat programme average costs (SKr) per patient for the four-month programme period for intervention group and control group.
| Type of cost | Intervention n = 268 | Control n = 257 | |
| Medical staff time | SEK | SEK | |
| Physiotherapist | 586 | 506 | |
| Health educator | 73 | 0 | |
| Exercise | |||
| Activity instructor | 560 | 288 | |
| Rent | 80 | 41 | |
| Introduction | 8 | 0 | |
| Group leader | 168 | 86 | |
| Participants’ costs | |||
| Exercise time | 1722 | 652 | |
| Travel time costs | 1310 | 449 | |
| Exercise equipment | 483 | 426 | |
| Travel costs | 1420 | 571 | |
| Costs of programme due to participants’ injuries | |||
| Visits to hospital | 0 | 0 | |
| Visits to primary healthcare | 7 | 7 | |
| Costs of absence from work due to injury | 58 | 12 | |
| Total costs | 6475 | 3038 |
Note: The table shows the value of each cost component.
Among the participants, 82% used a car to travel to the exercise class, 18% walked or cycled, and 0 % used public transport. The average travel time of the participants was 22 minutes.
Three minor injuries due to participation in the programme were reported in the intervention group and four in the control group, respectively, and comprised knee or ankle sprains. They resulted in one visit to primary healthcare and absence from work for 10 and two days respectively. Due to the exercise diary, the mean number of exercise sessions for individuals who completed the four-month intervention was 31 (SD = 14, range = 2–48) for the intervention group (n = 91), and 12 (SD = 4, range = 2–23) for the control group (n = 79).
Costs of the PAP programme
The results show intention-to-treat programme costs for the four-month programme period of SEK 6475 for the intervention group and SEK 3038 for the control group (see Table II). The largest share of the costs was the participant's cost, which included time spent on exercise, travel, and travel time to and from exercise. An on-treatment analysis shows programme costs for the intervention group of SEK 10 721 per patient and for the control group SEK 4822, which is an expected result considering the adherence rate and time of participation of the non-completers.
Table III shows the average change in physical activity of completers in intervention and control group. All three measures of physical activity were significantly improved in both groups at the four-month follow-up. After four months, 65% of the intervention group reported an active level of self-perceived physical activity, among the controls this was 53%. For both groups together, 12% of the already active individuals became inactive. The self-rated estimation of MET minutes per week showed more than twice as many MET minutes at the four-month follow-up compared with baseline in both groups. The Six-Minute Walk Test showed significant improvements for both groups. The improvements from baseline to four-month follow-up showed no significant differences between the two groups.
Table III.
Physical activity behaviour for intervention and control group at baseline and at four-month follow-up for participants who have completed the four-month programme: Differences between intervention and control group.
| Baseline | Four-month follow-up | p-values1 | ||
| Intervention n = 125 | ||||
| MET minutes per week2 median (q1 − q3) | 480 (6-1737) | 1020 (264–2493) | 0.0033 | |
| Inactivity (%) | 76 | 28.8 | < 0.0014 | |
| Six-Minute Walk Test2 (metres) median (q1 − q3) | 510 (457–550) | 525 (489–580) | < 0.0013 | |
| Control n = 120 | ||||
| MET minutes per week2 median (q1 − q3) | 524 (7–1382) | 1200 (268–2940) | 0.0013 | |
| Inactivity (%) | 71.8 | 37.4 | < 0.0014 | |
| Six-Minute Walk Test2 (metres) median (q1 − q3) | 500 (442-552) | 521 (468-573) | < 0.0013 | |
| p-values5 | Differences between the groups regarding changes from baseline to four-month follow up (p-values6) | |||
| MET minutes | 0.7336 | 0.9366 | 0.681 | |
| Inactivity | 0.2317 | 0.2497 | 0.053 | |
| Six-Minute Walk Test | 0.4446 | 0.3446 | 0.180 |
Notes: 1Comparisons between baseline and four-month follow-up; 2due to missing values n varies between 183 and 225; 3Wilcoxon's test; 4McNemar's test; 5comparisons between intervention and control group; 6Mann–Whitney U-test; 7chi-squared test.
Table IV shows the costs for the share of inactive individuals, and as a consequence of the programme the cost offset every year due to reduced inactivity.
Table IV.
Costs of inactivity for intervention and control group at baseline and at four-month follow-up.
| Intervention n = 1251 |
Control n = 1202 |
Total n = 2453 |
||||
| Baseline | Four-month Follow-up | Baseline | Four-month follow-up | Baseline | Four-month follow-up | |
| Inactivity, n (%) | 95 (76) | 36 (28.8) | 84 (71.8) | 43 (37.4) | 179 (80.5) | 79 (33.8) |
| Costs of inactivity every year (SEK) | 229 140 | 86 832 | 202 608 | 103 716 | 431 748 | 190 548 |
| Estimated cost offset every year (SEK) | 142 308 | 98 892 | 241 200 | |||
Notes: Inactivity was assessed using the self-reported question about present extent of physical activity. Estimated cost offset every year with a retained activity level.1Due to missing values n varies between 119 and 125;2 due to missing values n varies between 115 and 120;3due to missing values n varies between 234 and 245.
Discussion
The cost offset due to decreased inactivity as a consequence of participation in the PAP programme was for both groups SEK 241 200 (€ 25 497) every year, and is a cost offset of SEK 984 (€ 104) for healthcare costs and value of lost production per individual and year based on the assumption that the individual maintains the physical activity level during a period of one year.
The healthcare provider was responsible for only a minor part of the total programme costs: 24% (intervention group) and 31% (control group), respectively. The main part of the programme costs was the participants’ own costs – leisure time and travelling, together 76% for the intervention group and 69% for the control group. However, the programme costs do not cover the intangible benefits, i.e. consequences that are difficult to value such as the value of improved health.
The individuals’ own cost should be considered when planning physical activity interventions for sedentary individuals with lifestyle-related diseases and the question of a subsidy from society must be raised. The individual's own contribution may also influence the motivation for participation, and be a reason for the number of non-completers.
The main strength of the present study is that it is a randomized controlled trial. We chose three different ways of measuring physical activity. The IPAQ short form has relevant questions and acceptable criterion validity and specificity to correctly classify people achieving current physical activity guidelines, and has measurement properties as good as other self-reports [25,26]. A low physical activity level is defined as less than 600 MET minutes, a moderate level at least 600 MET minutes, and a high level at least 1500 MET minutes [29]. The participants in the present study show baseline values of around 500 MET minutes and at four months 1000–1200 MET minutes. Research shows different suggestions for significant improvements in the Six-Minute Walk Test: depending on intervention, gender, and patient category, reported mean changes of improvements in different studies have been between 33 and 170 metres [27,32]. In our results, the median increase was 15 and 21 metres respectively (both p-values < 0.001). The changes in physical activity are in agreement with earlier studies, showing improvements but no differences between intervention group and controls [33–35]. Our study showed that exercise twice a week, motivational counselling, and education compared with exercise only once a week does not make any difference in improving physical activity, and may be of note when designing programmes in primary healthcare. The completers may have stronger motivation for physical activity and exercise, and could have influenced the results of physical activity. The number of non-completers shows substantial potential for improvements in the implementation of the PAP programme with special regard to recruitment, motivational tasks, and environmental background.
A follow-up study should analyse the net resource utilization and costs vs net benefits of quality of life per se and cost per QALY respectively. Long-term follow-up of the results can be transformed into cost-effectiveness analyses, and should contain analyses of the cost offset in a long-term perspective and the sustainability of the improved physical activity level, and should consider quality of life.
The cost offset due to decreased inactivity is SEK 984 (€ 104) per individual and year, assuming a maintained physical activity level during one year. Both intervention and control group showed significantly improved physical activity behaviour, but no differences between the groups, a result that is of interest when planning health-promotion interventions in primary healthcare and for a future cost-effectiveness study.
Acknowledgements
This work was supported by Region Skåne, Sweden and the Skåne District Sport Federation. The authors would also like to thank the physiotherapists in primary healthcare in the South East Health Care District for their helpful participation. Opinions expressed in the article are the responsibility of the authors and do not reflect the views of the funding bodies.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.US Department of Health and Human Services. A report of the Surgeon General. Washington, DC:: US Department of Health and Human Services; 1996. Physical activity and health. [Google Scholar]
- 2.UK Department of Health. A report from Chief Medical Officer. London:: Department of Health; 2004. At least five a week: Evidence on the impact of physical activity and its relationship to health. [Google Scholar]
- 3.National Institute of Public Health in Sweden. Hälsa på lika villkor [Health under equal conditions; in Swedish] Stockholm:: >Author;; 2006. [Google Scholar]
- 4.Leon AS, Conett J. Physical activity and 10.5 year mortality in the Multiple Risk Factor Intervention Trial (MRFIT). Int J Epidemiol. 1991;20:690–7. doi: 10.1093/ije/20.3.690. [DOI] [PubMed] [Google Scholar]
- 5.Allender S, Foster C, Scarborough P, Rayner M. The burden of physical activity-related ill health in the UK. J Epidemiol Community Health. 2007;61:344–8. doi: 10.1136/jech.2006.050807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joubert J, Norman R, Lambert EV, Groenewald P, Schneider M, Bull F, et al. South African Comparative Risk Assessment Collaborating Group. Estimating the burden of disease attributable to physical inactivity in South Africa in 2000. S Afr Med J. 2007;97:725–31. [PubMed] [Google Scholar]
- 7.Johannesson M, Borgquist L, Jönsson B. The costs of treating hypertension in Sweden: An empirical investigation in primary health care. Scand J Prim Health Care. 1991;9:155–60. doi: 10.3109/02813439109018511. [DOI] [PubMed] [Google Scholar]
- 8.Bolin K, Lindgren B. FRISAM:: Stockholm; 2006. Fysisk inaktivitet – produktionsbortfall och sjukdomskostnader [Physical inactivity – production loss and health care costs; in Swedish]. [Google Scholar]
- 9.Blair SN, Kohl III HW, Paffenberger RS, Gibbons LW, Macera CA. Physical fitness and all-cause mortality. JAMA. 1989;262:2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 10.Pedersen BK, Saltin B. Evidence for describing exercise as therapy in chronic disease. Review. Scand J Med Sci Sports. 2006;16:3–63. doi: 10.1111/j.1600-0838.2006.00520.x. [DOI] [PubMed] [Google Scholar]
- 11.Yrkesföreningar för fysisk aktivitet. FYSS; Fysisk aktivitet i sjukdomsprevention och sjukdomsbehandling [Physical activity in disease prevention and disease treatment; in Swedish], ed A. Ståhle. Stockholm:: National Institute of Public Health; 2003. [Google Scholar]
- 12.International Conference on Health Promotion. Ottawa: 1986. Ottawa Charter for Health Promotion: The move towards a new public health. November. [Google Scholar]
- 13.Folland S, Goodman AC, Stano M. New Jersey:: Pearson Higher Education; 2004. The economics of health and health care. 4th; pp. 1–618. [Google Scholar]
- 14.Sturm R. Economics and physical activity: A research agenda. Am J Prev Med. 2005;28:141–9. doi: 10.1016/j.amepre.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Drummond MF, Sculpher MJ, Torrance GW, O’Brian BJ, Stoddart GL. Oxford:: Oxford University Press; 2005. Methods for the economic evaluation of health care programmes. 3rd; pp. 1–378. [Google Scholar]
- 16.Soerensen JB, Skovgaard T, Puggaard L. Exercise on prescription in general practice: A systematic review. Scand J Prim Health Care. 2006;24:69–74. doi: 10.1080/02813430600700027. [DOI] [PubMed] [Google Scholar]
- 17.Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost-effectiveness of a primary care based physical activity intervention in 45–74 year old men and women: A randomised controlled trial. Br J Sports Med. 1998;32:236–41. doi: 10.1136/bjsm.32.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elley R, Kerse N, Arroll B, Swinburn B, Ashton T, Robinson E. Cost-effectiveness of physical activity counselling in general practice. N Z Med J. 2004;117:U1216. [PubMed] [Google Scholar]
- 19.Sevick MA, Dunn AL, Morrow MS, Marcus BH, Chen GJ, Blair SN. Cost-effectiveness of lifestyle and structured exercise interventions in sedentary adults. Results of Project Active. Am J Prev Med. 2000;19:1–8. doi: 10.1016/s0749-3797(00)00154-9. [DOI] [PubMed] [Google Scholar]
- 20.Swedish Council on Technology Assessment in Health Care. Stockholm:: Swedish Council on Technology Assessment in Health Care; 2006. Metoder för att främja fysisk aktivitet [Methods of promoting physical activity; in Swedish]. [Google Scholar]
- 21.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 22.Brouwer W, Rutte F, Koopmanschap M. Oxford:: Oxford University Press; 2001. Economic evaluation in health care: Merging theory with practice. pp. 69–93. [Google Scholar]
- 23.Moutakis M, Persson U. Lund:: Institutionen för teknik och samhälle, Lunds tekniska högskola, Lunds Universitet (forthcoming); 2007. Inaktivitet, sjukdomskostnader och resvanor [Inactivity, cost of illness and travel habits; in Swedish]. [Google Scholar]
- 24.Central Bureau of Statistics. Sweden:: Population statistics; 2008. . Available at: http://www.scb.se/statistik/BE/BE0101/2007K03/be0101tab8samdrag.xls (accessed 18 March 2008). [Google Scholar]
- 25.Ekelund U, Sepp H, Brage S, Becker W, Jakes R, Hennings M, et al. Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish Adults. Public Health Nutr. 2006;2:258–65. doi: 10.1079/phn2005840. [DOI] [PubMed] [Google Scholar]
- 26.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 27.American Thoracic Society. ATS Statement: Guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med. 2002;166:111–17. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 28.McArdle WD, Katch FI, VL K. Baltimore, MD:: Lippincott Williams & Wilkins; 2006. Exercise physiology: Energy nutrition and human performance. [Google Scholar]
- 29.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: An update of activity codes and MET intensities. Med Sci Sport Exerc. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 30.Prochaska JO, Norcross JC, DiClemente CC. New York:: Quill; 2002. Changing for good: A revolutionary six-stage program for overcoming bad habits and moving your life positively forward. [Google Scholar]
- 31.Region of Skåne. Sweden:: Prices in health care; 2008. . Available at: http://www.skane.se/upload/Webbplatser/Sodra%20regionvardsnamnden/prislista/hela_prislistan.pdf (accessed 24 April 2008). [Google Scholar]
- 32.Enright PL, Sherrill DL. Reference equations for the Six-Minute Walk in healthy adults. Am J Respir Crit Care Med. 1998;158:1384–7. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [PubMed] [Google Scholar]
- 33.The Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care. The Activity Counseling Trial: A randomized controlled trial. JAMA. 2001;286:677–87. doi: 10.1001/jama.286.6.677. [DOI] [PubMed] [Google Scholar]
- 34.Soerensen JB, Kragstrup J, Skovgaard T, Puggaard L. Exercise on prescription: A randomized study on the effect of counselling vs counselling and supervised exercise. Scand J Med Sci Sports. 2008;18:288–97. doi: 10.1111/j.1600-0838.2008.00811.x. [DOI] [PubMed] [Google Scholar]
- 35.Van Sluijs EM, van Poppel MN, Twisk JW, Chin A, Paw MJ, Calfas KJ, van Mechelen W. Effect of a tailored physical activity intervention delivered in general practice settings: Results of a randomized controlled trial. Am J Public Health. 2005;95:1825–31. doi: 10.2105/AJPH.2004.044537. [DOI] [PMC free article] [PubMed] [Google Scholar]