Abstract
Computed tomography (CT) has been regarded as the method of choice for detecting the presence, site and cause of gastrointestinal tract perforation. In addition to determining the presence of perforation, CT can also localise the perforation size and demonstrate direct and indirect findings relative to the perforation. In this case study, we report the CT results in a patient with perforated duodenal ulcer associated with anterior abdominal abscess, and highlight the diagnostic value of CT imaging.
Keywords: Computed tomography, perforation, duodenal ulcer, diagnosis
Background
Gastrointestinal tract (GI) perforation is an emergent condition that requires immediate surgery. Diagnosis is mainly dependent on imaging examinations, and identification of the presence, level, and cause of perforation is essential for appropriate management and surgical planning.1 Extraluminal air is strongly suggested as a reliable sign for the presence of GI tract perforation and extraluminal air findings usually lead to surgical treatment. 2-4 Extraluminal air is only observed on 50–70% of conventional radiographs,5,6 however, it can be demonstrated by CT. Abdominal CT has been reported to be superior to conventional radiographs for the detection of extraluminal air and other signs, thus allowing for accurate diagnosis of GI tract perforations. 7-9
CT can display extraluminal, intraperitoneal, or retroperitoneal air with higher sensitivity than that of plain radiography. CT can also localise the perforation site. It has been reported that the overall accuracy of CT for predicting the site of GI tract perforation ranges from 82% to 90%.10,11 Moreover, diagnostic accuracy of CT for detecting the site of GI tract perforation has been significantly improved with the technological developments in CT imaging techniques, such as the wide availability of multislice CT. 8,10 In this case report, we present the CT findings of duodenal ulcer perforation in a patient with an abscess formed in the anterior abdominal wall, and highlight the importance of CT use in the detection and diagnosis of GI tract perforation.
Case details
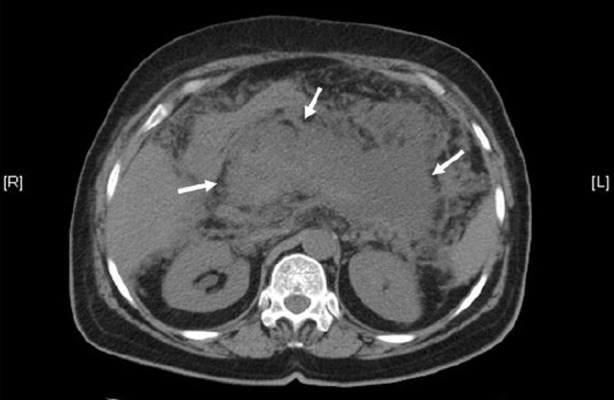
A 70-year-old woman presented to the emergency department with a history of severe epigastric pain. She was noted to be dehydrated and hypotensive. She had no history of chronic medical illness, except previous history of open cholecystectomy which was performed 10 years ago due to gallbladder stones. Laboratory tests on admission showed that white blood count was 17,000 per millimetre, serum amylase was 1450 units/litre. Abdominal ultrasound revealed normal appearance of intrahepatic ducts and common bile duct. Non-contrast enhanced CT scan was performed on a 32-slice scanner (GE Medical Systems, Lightspeed VCT, 32 x 1.25 mm) with a slice thickness of 5 mm. CT images showed that the pancreas was diffusely enlarged, with acute pancreatitis being diagnosed (Figure 1). The patient was admitted into the intensive care unit and received treatment to deal with the acute pancreatitis. Her condition improved and she was discharged 10 days later.
Figure 1. Non contrast-enhanced abdominal CT shows that the pancreas is diffusely enlarged (arrows), with loss of normal pancreatic appearance.
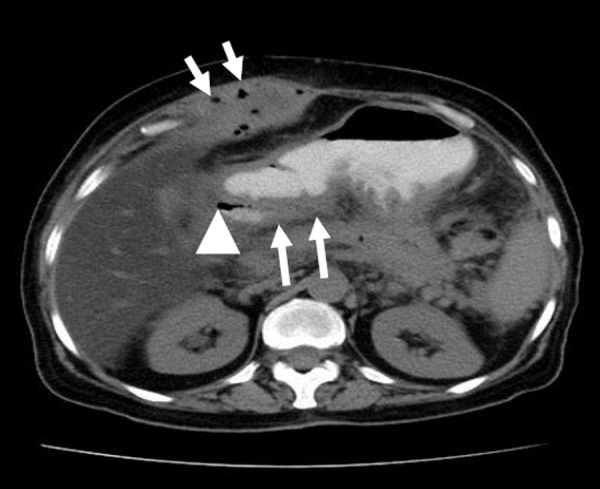
The patient was followed up in the outpatient department, but she refused to undergo endoscopic retrograde cholangiopancreatography (ERCP) examination. Three months later, a swelling appeared in the right upper abdomen. Non contrast-enhanced abdominal CT showed a soft tissue mass in the anterior abdominal wall at the right upper abdomen (Figure 2). Oral administration of contrast medium (gastrographin) was given to the patient, and air was injected into the GI tract through the nasogastric tube, followed by an abdominal CT scan. Air bubbles were found in the soft tissue mass, and the duodenal wall was thickened with free air present at the location of descending duodenum (Figure 3). This indicates a direct communication between the gastroduodenal tract and the soft tissue mass.
Figure 2. Non contrast-enhanced CT abdominal CT shows an abscess in the anterior abdominal wall (arrows).
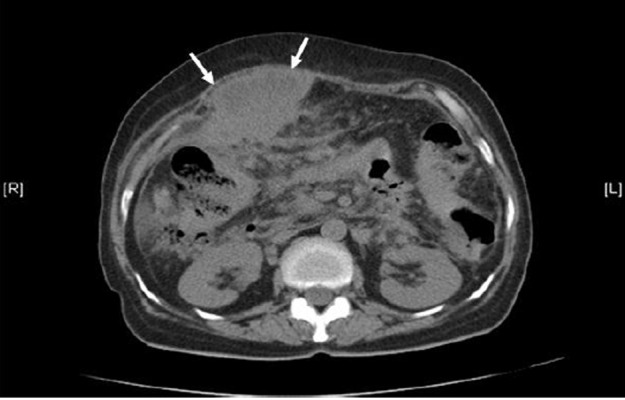
Figure 3. After administration of oral contrast medium in the gastrointestinal tract, multiple air bubbles are noticed in the abscess (short arrows). The duodenal wall is thickened (long arrows) and free air is present at the location of descending duodenum (arrowhead).
The patient was admitted to the surgical ward with preparation for open surgery. The abdomen was opened through the site of the previous incision, and an abscess was observed and drained. A hole was detected in the peritoneal fascia. The anterior duodenum was oedematous and thickened with coverage of fibrin. A small perforated duodenal ulcer was seen. Graham patch procedure was performed to repair the perforated duodenal ulcer with two drains put in place and then the abdomen was closed. The patient was managed with intravenous fluids, as well as analgesics and antibiotics. She was discharged on the eighth day after operation without developing any complications.
Discussion
CT is a convenient and sensitive imaging modality for the diagnosis of GI tract perforation. It can demonstrate intra- and extraperitoneal air that is too small to be displayed on plain radiography.11 In addition to the presence, site and cause of perforation and associated complications such as phlegmon, abscess and peritonitis can be demonstrated in most cases. Thus, CT allows for accurate assessment of the disease extent, which is valuable for patient management. As shown in this case report, CT shows the abscess in the anterior abdominal wall, with extraluminal air bubbles due to communication between the abscess and the duodenal perforation. Oral contrast administration is usually recommended prior to the examination with the aim of demonstrating the GI tract lumen and localising the site of perforation, although extraluminal leakage of contrast medium is not a frequent CT finding in patients with GI tract perforation. 12 This is confirmed in this case report, as the non contrast-enhanced CT scan only demonstrated the soft tissue mass in the anterior abdominal wall, however, confirmation of the diagnosis due to GI tract perforation was made based on the CT scan with orally administered contrast medium. This emphasises the importance of choosing appropriate CT scanning protocols.
Diagnosis of GI tract perforation is based on direct and indirect findings, which are detected on CT images. Direct findings include extraluminal air or luminal contrast material and discontinuity of the GI wall, while indirect findings consist of abscess and an inflammatory mass or phlegmon related to the bowel with or without an associated enterolith or foreign body.1,7,13,14 The site of perforation can be assessed by the following CT findings: (a) discontinuation of the GI wall, (b) the site of luminal contrast medium leakage, (c) the level of bowel obstruction, and (d) abrupt GI wall thickening with or without an associated phlegmon, inflammatory mass or abscess.11
In this case study, the discontinuity of GI wall was not observed due to the small perforated duodenal ulcer. However, an abscess was detected in the anterior abdominal wall while air bubbles were noticed in the abscess and free air at the location of descending duodenum following orally-administered contrast medium. The direction communication between the soft tissue mass and the GI tract is a reliable sign to confirm that the anterior abdominal abscess is caused by the GI tract perforation. This finding provides additional information to the above-mentioned common findings related to the GI tract perforation, thus, offering valuable advice to physicians dealing with patients who presented with abdominal pain. The amount and location of extraluminal air was assessed on CT images, indicating the perforation of GI tract.
Peptic ulcers are the main cause of gastroduodenal perforation, followed by necrotic or ulcerated malignancies. The most common and reliable CT findings of gastroduodenal perforation are extraluminal air and leakage of luminal contrast.1 Sites of perforation are usually assessed by CT findings of ulceration or focal interruption of the gastroduodenal wall and abrupt wall thickening associated with adjacent increased fat density. CT is also helpful in differentiating a duodenal haematoma from a perforation.15,16
In conclusion, CT has been established as the most valuable imaging technique for making an immediate and correct diagnosis of GI tract perforation. CT assists physicians not only to detect extraluminal air, but also to precisely determine the anatomic site of GI tract perforation and other direct and indirect findings which are useful for assessing the site of perforation. This case report highlights the importance of using CT in making accurate diagnosis in patients with abdominal pain due to suspected GI tract perforation. In particular, appropriate selection of CT scanning protocol, such as with oral contrast administration is necessary to ensure timely diagnosis and improve patient management.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
FUNDING
Not applicable.
PATIENT CONSENT
The authors, Sun Z, Al-naami A, Ali Khan A, declare that:
- They have obtained written, informed consent for the publication of the details relating to the patient(s) in this report.
- All possible steps have been taken to safeguard the identity of the patient(s).
- This submission is compliant with the requirements of local research ethics committees.
Please cite this paper as: Sun Z, Al-naami A, Ali Khan L, Perforated duodenal ulcer associated with anterior abdominal abscess: A case report. AMJ 2012, 5, 1, 14-17. http//dx.doi.org/10.4066/AMJ.2012.1006
References
- 1.Furukawa A, Sakoda M, Yamasaki M, Kono N, Tanaka T, Nitta N, Kanasaki S, Imoto K, Takahashi M, Murata K, Sakamoto T, Tani T. Gastrointestinal tract perforation: CT diagnosis of presence, site and cause. Abdom Imaging. 2005;30:524–534. doi: 10.1007/s00261-004-0289-x. [DOI] [PubMed] [Google Scholar]
- 2.Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, Tai YP, Li MK. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002;235:313–319. doi: 10.1097/00000658-200203000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJ, Chung SC, Li AK. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996;224:131–138. doi: 10.1097/00000658-199608000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lau JY, Lo SY, Ng EK, Lee DW, Lam YH, Chung SC. A randomized comparison of acute phase response and endotoxemia in patients with perforated peptic ulcers receiving laparoscopic or open patch repair. Am J Surg. 1998;175:325–327. doi: 10.1016/s0002-9610(98)00006-3. [DOI] [PubMed] [Google Scholar]
- 5.Cho KC, Baker SR, Cho KC, Baker SR. Extraluminal air: Diagnosis and significance. Radiol Clin North Am. 1994;32:829–844. [PubMed] [Google Scholar]
- 6.Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993;31:1219–1234. [PubMed] [Google Scholar]
- 7.Hainaux B, Agneessens E, Bertinotti R, De Maertelaer V, Rubesova E, Capelluto E, Moschopoulos C. Accuracy of MDCT in predicting site of gastrointestinal tract perforation. AJR Am J Roentgenol. 2006;187:1179–1183. doi: 10.2214/AJR.05.1179. [DOI] [PubMed] [Google Scholar]
- 8.Imuta M, Awai K, Nakayama Y, Murata Y, Asao C, Matsukawa T, Yamashita Y. Multidetector CT findings suggesting a perforation site in the gastrointestinal tract: analysis in surgically confirmed 155 patients. Radiat Med. 2007;25:113–118. doi: 10.1007/s11604-006-0112-4. [DOI] [PubMed] [Google Scholar]
- 9.Miki T, Ogata S, Uto M, Nakazono T, Urata M, Ishibe R, Shinyama S, Nakajo M. Multidetector-row CT findings of colonic perforation: direct visualization of ruptured colonic wall. Abdom Imaging. 2004;29:658–662. doi: 10.1007/s00261-003-0159-y. [DOI] [PubMed] [Google Scholar]
- 10.Kim HC, Shin HC, Park SJ, Park SI, Kim HH, Bae WK, Kim IY, Jeong DS. Traumatic bowel perforation: analysis of CT findings according to the perforation site and the elapsed time since accident. Clin Imaging. 2004;28:334–339. doi: 10.1016/S0899-7071(03)00244-4. [DOI] [PubMed] [Google Scholar]
- 11.Chen CH, Huang HS, Yang CC, Yeh YH. The features of perforated peptic ulcers in conventional computed tomography. Hepatogastroenterology. 2001;48:1393–1396. [PubMed] [Google Scholar]
- 12.Maniatis V, Chryssikopoulos H, Roussakis A, Kalamara C, Kavadias S, Papadopoulos A, Andreou J, Stringaris K. Perforation of the alimentary tract: evaluation with computed tomography. Abdom Imaging. 2000;25:373–379. doi: 10.1007/s002610000022. [DOI] [PubMed] [Google Scholar]
- 13.Oguro S, Funabiki T, Hosoda K, Inoue Y, Yamane T, Sato M, Kitano M, Jinzaki M. 64-slice multidetector computed tomography evaluation of gastrointestinal tract perforation site: detectability of direct findings in upper and lower GI tract. Eur Radiol. 2010;20:1396–1403. doi: 10.1007/s00330-009-1670-5. [DOI] [PubMed] [Google Scholar]
- 14.Kim SH, Shin SS, Jeong YY, Heo SH, Kim JW, Kang HK. Gastrointestinal tract perforation: MDCT findings according to the perforation sites. Korean J Radiol. 2009;10:63–70. doi: 10.3348/kjr.2009.10.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hofer GA, Cohen AJ. CT signs of duodenal perforation secondary to blunt abdominal trauma. J Comput Assist Tomogr. 1989;13:430–432. doi: 10.1097/00004728-198905000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Shilyansky J, Pearl RF, Kreller M, Sena LM, Babyn PS. Diagnosis and management of duodenal injury in children. J Pediatr Surg. 1997;32:880–886. doi: 10.1016/s0022-3468(97)90642-4. [DOI] [PubMed] [Google Scholar]


