Abstract
A 25-year-old housewife presented with a burning sensation over both legs for the past 15 months, and fever with weight loss for the past six months. She had noticed a lump in her left breast one month ago. Examination revealed hyperaesthesia and allodynia over the lower limbs. Nerve conduction studies confirmed the presence of sensory neuropathy. Nerve biopsy was suggestive of a chronic axonopathy. Subsequently sputum as well as aspirate from the breast lump tested positive for acid fast bacilli. Treatment with anti-tubercular therapy resulted in full recovery. Peripheral neuropathy is a unique and unusual presentation of tuberculosis.
Keywords: peripheral neuropathy, disseminated tuberculosis, sensory polyneuropathy
Background
Peripheral neuropathy is a ubiquitous disorder that can arise from a variety of causes, most often non-infectious. While uncommon in the developed world, infectious causes of polyneuropathy are frequently encountered in developing countries, with leprosy constituting the leading one. Interestingly, peripheral neuropathy due to the closely related Mycobacterium tuberculosis is extremely rare even in developing countries. We describe a case of disseminated tuberculosis presenting with severe sensory peripheral neuropathy, which resolved completely with anti-tubercular therapy. As this case demonstrates, a high index of suspicion should be maintained for tuberculosis in patients presenting with otherwise unexplained peripheral neuropathy when associated with systemic symptoms of fever and weight loss. This is especially relevant in populations with a high prevalence of tuberculosis, such as the general population in developing countries and the immunocompromised population in the developed world.
Case details
A 25-year-old housewife presented with severe burning pain involving both legs for the past 15 months. The pain was insidious in onset and constant in nature with no diurnal variation. It was associated with tingling sensation over the same areas. The pain was aggravated by walking over rough surfaces and on exposure to cold air. The patient denied any symptoms of weakness or swaying while walking. The patient also complained of low grade fever with evening rise of temperature and mild chills since the past six months and weight loss of 17 kilograms over the same period of time. The patient had been previously prescribed gabapentin and tricyclic antidepressants with which she reported partial relief of the pain. Since the past month, the patient had also noticed a painless lump in her left breast.
At presentation, the patient had mild pallor; significant tachycardia was also noted. Neurological examination was unremarkable except for hyperaesthesia and allodynia over the soles of her feet. Respiratory examination revealed diminished breath sounds over the right lung base with dullness on percussion. Palpation of her left breast confirmed the presence of a firm, non-tender and mobile lump in the infero-lateral quadrant.
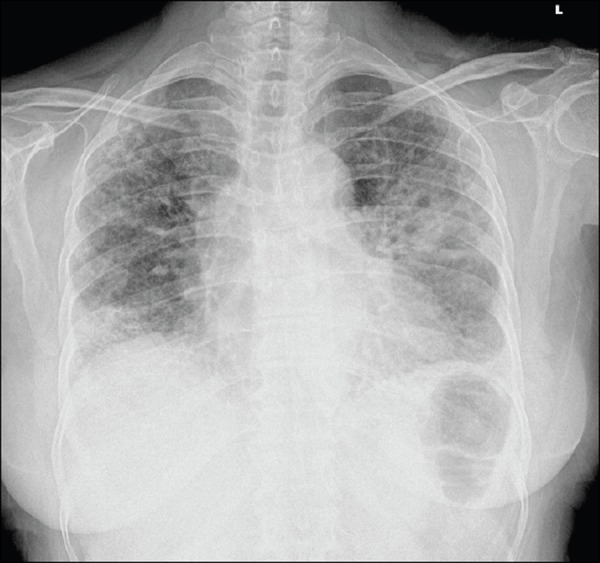
Laboratory parameters showed anaemia (haemoglobin: 10.6 g/dL) and elevated ESR (46 mm/hour). Significant hypoalbuminemia and hypergammaglobulinemia were also present (2.2 g/dL and 4.6 g/dL, respectively). Thoracic radiography revealed inhomogeneous fluffy shadows in the left mid- and lower zones and the right lower zone, with multiple cavities (Figure 1). Nerve conduction studies demonstrated a sensory neuropathy affecting both lower limbs. A nerve biopsy was performed which showed features of a chronic axonopathy of moderate severity.
Figure 1. Thoracic radiogram showing inhomogeneous fluffy shadows in the left mid- and lower zones and the right lower zone, with multiple cavities.
Simultaneously, ultrasonographic evaluation of the breast mass revealed a retro-mammary collection with internal echoes, extending from an erosion in the left fifth rib. Needle aspiration yielded pus which tested positive for acid fast bacilli (AFB). Subsequently, fluorescein staining of sputum smears was also reported positive for AFB. A diagnosis of disseminated tuberculosis was made, and the patient was started on anti-tubercular therapy (isoniazid 300 mg daily, rifampicin 450 mg daily, ethambutol 800 mg daily, and pyrazinamide 1 g daily) along with pyridoxine 40 mg daily. In the absence of an alternative explanation, the peripheral neuropathy was attributed to the infection itself. On follow up, the patient reported steady improvement in her symptoms including complete resolution of her fever, weight loss and the pain affecting her lower limbs.
Discussion
Neurological involvement in tuberculosis can occur due to the disease itself or as an adverse effect of therapy.1 Therapy-related neurotoxicity can arise either as a complication of isoniazid therapy or following over- supplementation of pyridoxine. Both these possibilities were invalidated in our patient, as she had never received any form of anti-tubercular therapy in the past.
Tuberculosis itself affects primarily the central nervous system in the form of tubercular meningitis, tuberculomas, and spinal arachnoiditis. Involvement of the peripheral nervous system is relatively unusual and most often due to compression by vertebral collapse or cold abscesses. Neuritis due to direct involvement by tuberculosis is extremely rare. Sporadic reports of such cases include a series of eight cases of isolated phrenic nerve palsy complicating tubercular mediastinal lymphadenopathy and a case of sciatica resulting from tubercular sacroiliitis. Presumably, nerve compression by inflammatory granulomatous tissue was responsible for these cases of neuropathy.
Polyneuropathy resulting from tuberculosis is even rarer. De la Torre2 described a patient with inflammatory bowel disease and tubercular lymphadenitis presenting with Guillain-Barre syndrome. The concomitant presence of two diseases in this patient, however, did not allow for a definitive diagnosis of tuberculosis-induced polyneuropathy, especially as inflammatory bowel disease is known to produce peripheral neuropathy3. Soehardy4 described a patient with pulmonary tuberculosis and Marfan’s syndrome with features of chronic inflammatory demyelinating polyneuropathy (CIDP). Chong5 also reported a case of ileo-caecal tuberculosis complicated by CIDP. Although the patient in question did not completely recover after anti-tubercular therapy, the temporal relationship of neurologic symptoms to repeated cessation and restarting of anti-tubercular drugs strongly supported a possibility of tuberculosis as the etiology of polyneuropathy.
The pathogenesis of tubercular polyneuropathy remains unknown, due to its extreme rarity. This is in sharp contrast to the closely related Mycobacterium leprae organism which is known to possess affinity for peripheral nerves. Neuropathic disease in leprosy results from direct invasion by M. leprae bacilli with destruction of axons, and granuloma formation. In our case, however, nerve biopsy was suggestive of a toxic neuropathy, raising the possibility of nerve damage secondary to neurotoxins elaborated by mycobacteria.
In summary, this is a rare case of disseminated tuberculosis presenting with peripheral sensory neuropathy. It highlights the need to maintain a high index of suspicion for tuberculosis especially in areas with high prevalence of the disease. Further studies are required to elucidate the mechanism of neurotoxicity in tuberculosis and identify putative mediators.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
FUNDING
No
PATIENT CONSENT
The authors declare that:
- They have obtained written, informed consent for the publication of the details relating to the patient in this report.
- All possible steps have been taken to safeguard the identity of the patient.
- This submission is compliant with the requirements of local research ethics committees.
Please cite this paper as: Naha K, Dasari S, Prabhu M. Tubercular neuritis: A new manifestation of an ancient disease. AMJ 2011, 4, 12, 674-676 http//dx.doi.org/10.4066/AMJ.2011.1029
References
- 1.The Neuropathy Association and Medical Advisory Committee. Guidelines for the diagnosis and treatment of chronic inflammatory demyelinating polyneuropathy. J Peripher Nerv Syst. 2003;8:282–4. [PubMed] [Google Scholar]
- 2.De la Torre RG, Morís G, Martínez DP, Montes IC. Guillain-Barre syndrome, tuberculosis and inflammatory bowel disease: a multiple association. Int Arch Med. 2010;3:15. doi: 10.1186/1755-7682-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gondim FA, Brannagan TH, Sander HW, Chin RL, Latov N. Peripheral neuropathy in patients with inflammatory bowel disease. Brain. 2005;128:867–79. doi: 10.1093/brain/awh429. [DOI] [PubMed] [Google Scholar]
- 4.Soehardy Z, Yuhanisa A, Thein SS, Rohana AG, Fauzi AR, Norlinah MI, Hamidon BB, Rozaidi SW. AMSAN variant of Guillain Barre syndrome progressing to chronic inflammatory demyelinating polyneuropathy in a patient with Marfan’s syndrome and pulmonary tuberculosis. Med J Malaysia. 2005;60:655–6. [PubMed] [Google Scholar]
- 5.Chong VH, Joseph TP, Telisinghe PU, Jalihal A. Chronic inflammatory demyelinating polyneuropathy associated with intestinal tuberculosis. J Microbiol Immunol Infect. 2007;40:377–80. [PubMed] [Google Scholar]


