Abstract
Introduction
Conjoined twins occur in approximately 0.2:10,000 births; the obstetrician and sonographer only rarely examine them. In Western countries, discovery of conjoined twins is often made by the end of the first trimester; however, in the third world, conjoined twins are often discovered only at birth.
Objective
To evaluate how ultrasound techniques, when possibly available, may improve management and counseling when conjoined twins are confirmed.
Material and Methods
The authors report two different cases of union of two equal twins with sole umbilical cord.
Results
The two cases presented with non contributive medical history and no prior teratogen exposure and an unfavorable prognosis.
Early discovery of viable conjoined twins permits assessment of the best route of delivery and a planning for serial sonography and fast MRI to plan eventual separation surgery or fetus after-birth surviving possibilities.
Keywords: conjoined twins, ultrasound
Introduction
Conjoined twins occur in approximately 0.2:10,000 pregnancies, but only 0.05:10,000 live births; there is a greater incidence of female conjoined twins, but the reason is unknown. A system of classification for conjoined twins, established by St-Hilaire in 1832 is used today (1). Monoamniotic twin pregnancies comprise 1% of monozygotic twin pregnancies (approximately 1:25,000 pregnancies) (2). Placentation in twin pregnancies depends on the stage of embryonic division; if cell differentiation takes place after the 14th day of embryonic development, development is incomplete, resulting in conjoined twins. The etiology of conjoined twins is not known. In general there are no karyotypic abnormalities, nor do race, heredity, birth order, or consanguinity appear to influence the process. Two prominent theories explain the appearance of conjoined twins, the theory of fusion and the theory of fission. In the fusion theory, authors propose that the twins join secondary to late embryonic division; in the fission theory, some authors feel there is instead an absence of complete embryonic division.
Pathogenesis of this entity is obscure. Common structures between conjoined twins vary; classification can be based on fused structures, as Dollander did using the classification system of St. Hilaire.
Only four cases of conjoined twins were seen before birth radiographically prior to the early sonographic era of the 1960s. In 1989, Grutter observed thoracopagus twins at 16 weeks (3). Sonography has demonstrated conjoined twins at the end of the first trimester since 1995 (1). In 1995, Maggio reported a diagnosis of conjoined twins (thoracopagus with a single heart) at 8 weeks, 5 days, confirmed at 13 weeks GA (4). In 1997, Hill diagnosed conjoined twins at 6 weeks, 6 days, confirmed at 10 weeks GA. Fast MRI is becoming an important tool for prognostic assessment, in the first trimester for anatomic evaluation, and later in pregnancy to plan the route of delivery and separation surgery when possible. Serial sonography at 12–13 weeks of gestational age confirms common anatomy and is recommended to prevent false-positive diagnosis. Early sonography shows continuity between the fetuses and fails to show independent movement. No amniotic membrane will be seen between the twins.
First-trimester endovaginal sonographic indications for possible conjoined twins include: 1) a sole extra-amniotic vitelline vesicle is correlated with incidence of conjoined twins, since the vesicle is usually enclosed between amnion and chorion; 2) a sole embryo with a bifid appearance seen before 10 weeks GA; 3) probe motion of the probe which moves both embryos at the same time; 4) visualization of two hearts or two stomachs.
The prognosis for conjoined twins is generally unfavorable, with approximately 40% of cases stillborn. The worst prognoses concern craniopagus twins and those with a sole cardiac mass. Structural anomalies are frequently found such as polyhydramnios (50%), cardiac malformations, common omphaloceles, and neural tube defects. Upon discovery of nonviable conjoined twins, interruption of pregnancy should therefore be recommended. When commonality of fetal organs is limited (5), surgical intervention often takes place around one year of age.
In the present report, the conjoined twins in Clinical Case 1 were: isodiploteratat and autosite (union of two equal twins); monomphalian (with sole umbilical cord); and Terata anacatadidyma (omphalopagus with midline fusion). In Clinical Case 2 were: isodiploterat and autosite (union of two equal twins); monomphalian, (with sole umbilical cord); and Terata anadidyma (omcraniopagus with proximal fusion).
Clinical cases
Case 1
A 30-year-old patient, G4P3, with noncontributive medical history and no prior teratogen exposure, was seen in our clinic. A monochorionic, monoamniotic abdominal conjoined twin pregnancy (thoraco-omphalopagus; Figs. 1–3) was discovered on sonography at 13 weeks GA. Four extremities were seen, as were two cardiac structures, two stomachs, and a liver (Fig. 4). Amniocentesis revealed 46, XY; the patient chose interruption of pregnancy.
Figure 1.
Sagittal section showing thoraco-omphalopagus twins; Case 1.
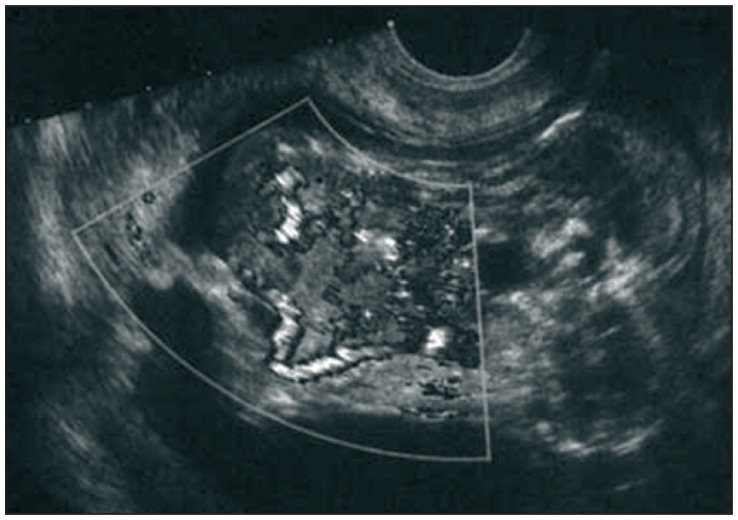
Figure 2.
Color Doppler sagittal image of thoraco-omphalopagus twins; Case 1.
Figure 3.
Transverse section through thoraces and pelves; Case 1.
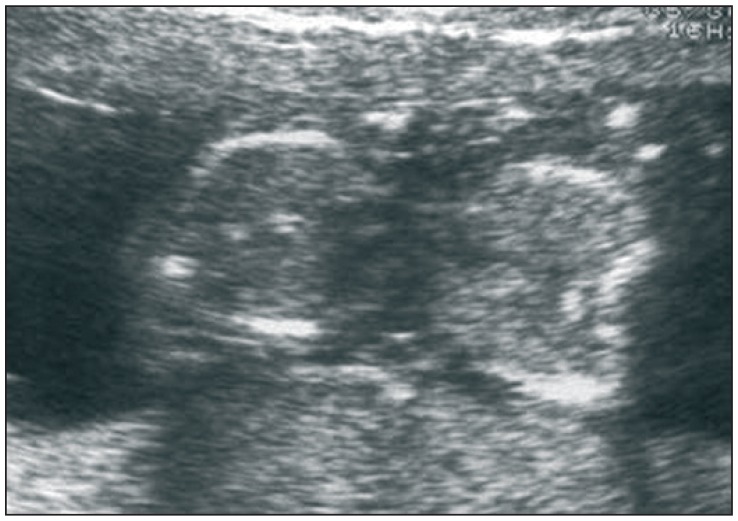
Figure 4.
Transverse section showing two stomachs and common liver; Case 1.
Postmortem analysis verified a common subumbilical abdominal wall with peritoneum and liver crossing in a bridgelike fashion behind it. The umbilical cord had four vessels on the fetal side of the placenta: a vein and an umbilical artery for each fetus in the shape of a “y” in the cord interior. One vein and one artery were seen on the maternal side of the placenta. Part of the common colon formed a median sac of 1 cm in diameter with meconium in the proximal and distal regions of the digestive tube of each fetus.
The rest of the viscera were unique to each twin; however, there was a defect of the superior sterno-abdominal wall in each, revealing ectopia cordis with truncus arteriosus type I in each fetus. The placenta was monochorionic and monoamniotic. We concluded that these were omphalopagus twins with a shared umbilical cord.
Case 2
While we served on a humanitarian mission to Gujarat, India, a patient came to the emergency department of Bharush Hospital at around 35 weeks GA. She presented with violent uterine contractions caused by polyhydramnios. Sonography performed with rudimentary equipment and poor resolution confirmed polyhydramnios and a fetus lodged in the posterior uterus, seeming to consist of a sole cephalic pole and four extremities (cephalothoracopagus). Unfortunately, images could not be preserved. The fetus was delivered vaginally without dystocia and proved to be conjoined twins with no cardiac activity (Fig. 5). Autopsy was declined by the mother.
Figure 5.
Cephalothoracopagus twins at birth of Case 2.
Discussion
In the case of potentially viable conjoined twins, after 24 weeks GA the choice between vaginal delivery or prophylactic caesarian section should be made based on maternal safety and neonatal criteria. Caesarian section avoids dystocia, uterine rupture, and fetal death in utero (5). Approximately six to ten cases of conjoined twins per annum worldwide are treated surgically. The surgery is most successful.
Diagnosis of conjoined twins is possible as early as 8 weeks GA, but accurate evaluation of common structures is not possible. The 12-week scan allows clinicians to assess viability, and, in the case of non viability, to propose early medical interruption of pregnancy, preventing hysterotomy in the case of a delayed termination.
Conclusion
Early discovery of viable conjoined twins permits assessment of the best route of delivery and a planning for serial sonography and fast MRI to plan separation surgery.
References
- 1.Vaughn TC, Powell LC. The obstetrical management of conjoined twins. Obstet Gynecol. 1979;53:67–72. [PubMed] [Google Scholar]
- 2.Blanc B, Guidicelli B, Boubli L, Bernard Y. Grossesses multiples. Encycl Med Chir (Paris-France), Obstetrique. 1988 Dec;5030(A10):12. [Google Scholar]
- 3.Moussaoui RD. Jumeaux conjoints: A propos d’une observation. Gynécologie Internationale. 1997;6:59–61. [Google Scholar]
- 4.Abossolo T, Dancoisne P, Tuaillon J, Orvain E, Sommer JC, Riviére JP. Diagnostic anténatal précoce de jumeaux céphalo-thoracopages asymétriques. J Gynecol Obstet Biol Reprod. 1994;23:79–84. [PubMed] [Google Scholar]
- 5.Usta IM, Awwad JT. A false positive diagnosis of conjoined twins in a triplet pregnancy: pitfalls of first trimester ultrasonographic prenatal diagnosis. Prenat Diagn. 2000;20:169–170. doi: 10.1002/(sici)1097-0223(200002)20:2<169::aid-pd768>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]