Abstract
The Canadian Digestive Health Foundation initiated a scientific program to assess the incidence, prevalence, mortality and economic impact of digestive disorders across Canada in 2009. The current article presents the updated findings from the study concerning pancreatitis.
Keywords: Canada health care, Burden of disease, Digestive disease, Epidemiology, Health economics, Pancreatitis
Abstract
En 2009, la Fondation canadienne pour la promotion de la santé digestive a lancé un programme scientifique pour évaluer l’incidence, la prévalence, la mortalité et les conséquences économiques des maladies digestives au Canada. Le présent article expose les observations mises à jour de l’étude sur la pancréatite.
In 2009, the Canadian Digestive Health Foundation (CDHF) launched a scientific project to define incidence, prevalence, mortality and economic impact of digestive disorders across Canada. Detailed information was compiled on 19 digestive disorders through systematic reviews, government documents and websites. This information was published as Establishing Digestive Health as a Priority for Canadians, The Canadian Digestive Health Foundation National Digestive Disorders Prevalence and Impact Study Report, and released to the press and government in November 2009 (www.CDHF.ca). The CDHF Public Impact Series presents a full compilation of the available statistics for the impact of digestive disorders in Canada.
According to the Atlanta definition, the diagnosis of acute pancreatitis is made if two of the following three criteria are met: abdominal pain strongly suggestive of pancreatitis; amylase and/or lipase levels at least three times higher than normal; and characteristic findings of pancreatic inflammation on either transabdominal ultrasound or contrast-enhanced computed tomography scan, of which the latter is preferred (1). The most common causes of acute or recurrent pancreatitis are gallstones and alcoholism. Chronic pancreatitis involves inflammatory changes that result in permanent structural damage, leading to progressive degradation of pancreatic function (2). Where possible, acute and chronic pancreatitis will be discussed separately in the following sections. If there is insufficient literature, both forms will be grouped together.
Previous studies have indicated that pancreatitis is a prevalent and costly disease representing a considerable burden to health care systems, the individual and, by extension, their families. Although data are available, this information has not been extrapolated to the Canadian context in an accessible format. Written to inform both medical professionals and patients, the present review will increase awareness of pancreatitis through a comprehensive overview of disease incidence and prevalence, and implications for the Canadian health care system and socioeconomics.
METHODS
A systematic literature review was conducted to retrieve peer-reviewed, scholarly literature published in English using the PubMed, MEDLINE, EMBASE and Scopus databases. The search term used was “pancreatitis”, with a specific focus on epidemiology and economic studies from developed countries. Additional information was retrieved from government sources and not-for-profit organizations.
INCIDENCE
The peak incidence of pancreatitis for both men and women is between 40 and 70 years of age, with a male predominance in all age groups (3). Several studies conducted between 1981 and 2001 found that the incidence of first attacks of acute pancreatitis ranged from 9.8 to 37.8 per 100,000 individuals (3). The most recent epidemiological study conducted in California in 2001 (4) found that the incidence was as high as 43.8 per 100,000, possibly due to increased clinical awareness of the disease and improved testing. Although less well studied, the available data from western countries regarding chronic pancreatitis suggest an incidence of six per 100,000 individuals (3). Using 2010 demographic data for Canada (population 34,482,779), approximately 15,100 and 2070 Canadians will be diagnosed with acute and chronic pancreatitis, respectively, in the coming year (5).
PREVALENCE
The proportion of patients with a first attack of pancreatitis who progress to chronic pancreatitis is estimated to be 6.5%, while 16.5% will experience recurrent acute pancreatitis (6). Based on a 2011 study conducted in Olmstead County, Minnesota (USA) (7), the prevalence of chronic pancreatitis, adjusted for age and sex, was determined to be 41.6 per 100,000 inhabitants. Extrapolating this figure to the Canadian population means that there are 14,400 individuals living with chronic pancreatitis in this country.
MORTALITY
While overall mortality from acute pancreatitis has seen steady improvements and is now at 5%, the mortality from necrotizing pancreatitis is much higher (17%), and some studies have found rates as high as 30% within the subgroup of patients with severe acute pancreatitis (8,9). For patients with chronic pancreatitis, a population-based epidemiological study conducted in Olmstead County with a 10-year follow-up period found an all-cause mortality rate of 44%, which was significantly higher (P<0.001) than the age- and sex-specific expected mortality rate in Minnesota (7). However, chronic pancreatitis was considered to be the primary or contributing cause in only 5% and 18% of deaths, respectively. In Canada, the annual number of deaths due to acute and chronic pancreatitis is 300 and 40 persons, respectively, (Figure 1) (10). For acute pancreatitis, nearly 10% of all deaths are attributable to alcohol-induced pancreatitis, while deaths due to alcohol-induced chronic pancreatitis represent approximately 50% of cases (10).
Figure 1).
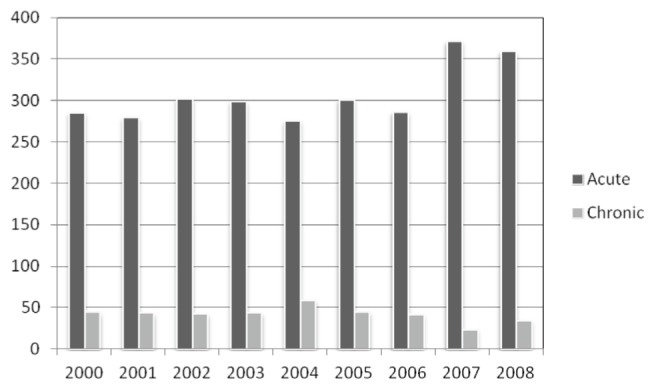
Number of Canadian mortalities due to pancreatitis (acute or chronic) according to year
ECONOMICS
Direct costs
The average length of hospital stay in Canada for patients with pancreatic conditions is 10 days. Between 1996 and 2005, this decreased to an average of eight days (11). In 2004/2005, the average cost per stay for pancreatic diseases was $8,896, which for 13,200 patients resulted in a total cost of $118 million (12). In comparison, $3.7 billion was spent in the United States in 2004, with an average cost per hospitalization of $11,402 (13,14). A German study noted that patients with chronic pancreatitis were prescribed daily analgesics (34%), enzyme supplements (57%), insulin (25%) and oral diabetic medications (4%), all of which contribute to considerable health care costs (15).
Indirect costs
Patients with acute and chronic pancreatitis report a decreased quality of life in many areas including physical restrictions and often suffer from long-term mental impairments (16). It is difficult to assess the actual indirect costs associated with pancreatitis due to the extensive comorbidities typical of this patient population (eg, diabetes, cardiovascular disease, smoking-related cancers and cirrhosis) and their cumulative effect on a person’s productivity within society. Nevertheless, a German study of chronic pancreatitis patients (17) found that only 41% worked full-time and, of these, 40% had pancreatitis-related absences from work in the previous year. Interestingly, 14% took early retirement due to impairments associated with pancreatitis. Another case series of chronic pancreatitis patients reported that 12.1% were unable to work due to their illness and, as the disease progressed, it became more difficult for other patients to remain employed full-time (17). Thus, although data are not available to extrapolate the indirect costs of pancreatitis, it is clear that the burden of the illness on patients and their families is substantial.
REFERENCES
- 1.Acute Pancreatitis Classification Working Group Revision of the Atlanta classification of acute pancreatitis (3rd revision) [Pancreas Club website] Apr 9, 2008. < www.pancreasclub.com/resources/AtlantaClassification.pdf> (Accessed November 9, 2011).
- 2.Steer ML, Waxman I, Freedman S. Chronic pancreatitis. New Engl J Med. 1995;332:1482–90. doi: 10.1056/NEJM199506013322206. [DOI] [PubMed] [Google Scholar]
- 3.Spanier BW, Dijkgraaf MG, Bruno MJ. Epidemiology, aetiology and outcome of acute and chronic pancreatitis: An update. Best Pract Res Clin Gastroenterol. 2008;22:45–63. doi: 10.1016/j.bpg.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Frey CF, Zhou H, Harvey DJ, et al. The incidence and case-fatality rates of acute biliary, alcoholic, and idiopathic pancreatitis in California, 1994–2001. Pancreas. 2006;33:336–44. doi: 10.1097/01.mpa.0000236727.16370.99. [DOI] [PubMed] [Google Scholar]
- 5.Statistics Canada Population estimates by sex and age group as of July 2011, Canada. < www.statcan.gc.ca/start-debut-eng.html> (Accessed November 1, 2011).
- 6.Lankisch PG, Breuer N, Bruns A, et al. Natural history of acute pancreatitis: A long-term population-based study. Am J Gastroenterol. 2009;104:2797–805. doi: 10.1038/ajg.2009.405. [DOI] [PubMed] [Google Scholar]
- 7.Yadav D, Timmons L, Benson JT, et al. Incidence, prevalence, and survival of chronic pancreatitis: A population-based study. Am J Gastroenterol. 2011;106:2192–9. doi: 10.1038/ajg.2011.328. (Erratum in 2011;106:2209). [DOI] [PubMed] [Google Scholar]
- 8.Banks PA, Freeman ML, Practice Parameters Committee of the American College of Gastroenterology Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379–400. doi: 10.1111/j.1572-0241.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 9.Sarles H. Revised classification of pancreatitis – Marseille 1984. Dig Dis Sci. 1985;30:573–4. doi: 10.1007/BF01320265. [DOI] [PubMed] [Google Scholar]
- 10.Statistics Canada Table 102-0531 – Deaths, by cause, Chapter XI: K00 to K93, age group and sex, Canada, 2000–2008, CANSIM. < http://cansim2.statcan.gc.ca> (Accessed November 1, 2011).
- 11.Organisation for Economic Co-operation and Development (OECD) OECD Health Data 2008. < www.oecd.org> (Accessed November 1, 2011).
- 12.Canadian Institute for Health Information . Ottawa: Canadian Institute for Health Information; 2008. The Cost of Acute Care Hospital Stays by Medical Condition in Canada: 2004–2005; pp. 1–155. [Google Scholar]
- 13.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part I: Overall and upper gastrointestinal diseases. Gastroenterology. 2009;136:376–86. doi: 10.1053/j.gastro.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 14.Fagenholz PJ, Fernandez-del Castillo C, Harris NS, et al. Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas. 2007;35:302–7. doi: 10.1097/MPA.0b013e3180cac24b. [DOI] [PubMed] [Google Scholar]
- 15.Wehler M, Nichterlein R, Fishcer B, et al. Factors associated with health-related quality of life in chronic pancreatitis. Am J Gastroenterol. 2004;99:138–46. doi: 10.1111/j.1572-0241.2004.04005.x. [DOI] [PubMed] [Google Scholar]
- 16.Wu BU, Conwell DL. Update in acute pancreatitis. Curr Gastroenterol Rep. 2010;12:83–90. doi: 10.1007/s11894-010-0091-6. [DOI] [PubMed] [Google Scholar]
- 17.Jupp J, Fine D, Johnson CD. The epidemiology and socioeconomic impact of chronic pancreatitis. Best Pract Res Clin Gastroenterol. 2010;24:219–31. doi: 10.1016/j.bpg.2010.03.005. [DOI] [PubMed] [Google Scholar]


