Abstract
We use quantitative and qualitative data to explore the psychological impact of weight change among American adults. Using data from the Midlife Development in the United States (MIDUS) study, a survey of more than 3,000 adults ages 25 to 74 in 1995, we contrast underweight, normal weight, overweight, obese I, and obese II/III persons along five psychosocial outcomes: positive mood, negative mood, perceived interpersonal discrimination, self-acceptance, and self-satisfaction. We further assess whether these relationships are contingent upon one's body mass index (BMI) at age 21. We find a strong inverse association between adult BMI and each of the five outcomes, reflecting the stigma associated with high body weight. However, overweight adults who were also overweight at age 21 are more likely than persons who were previously slender to say they were “very satisfied” with themselves. Results from 40 in-depth semi-structured interviews reveal similarly that persons who were persistently overweight or obese accept their weight as part of their identity, whereas those who experienced substantial weight increases (or decreases) struggle between two identities: the weight they actually are, and the weight that they believe exemplifies who they are. We discuss implications for stigma theory, and the ways that stigma exits and entries affect psychological well-being.
Keywords: body mass index (BMI), psychological well-being, self-concept, stigma, temporal comparison theory, weight change
1. Introduction
The physical health consequences of obesity are well-documented, with most studies showing that the risks of chronic illness and mortality increase as one's body mass index (BMI) increases (Koch, 2011; Yan et al., 2006). However, studies investigating the psychological consequences of obesity yield equivocal findings (Faith et al., 2004). Most studies reveal an inverse association between body weight and psychological well-being (Heo et al., 2005; Wadden et al., 2006), yet others detect either a positive (Carr et al., 2007; Jorm et al., 2003) or nonsignificant association (Faith et al., 2001; Istvan et al., 1992).
These equivocal findings may reflect the fact that persons classified as overweight or obese in cross-sectional epidemiological studies are a heterogeneous population, including both persons who have been overweight since childhood or adolescence, and persons who became overweight or obese in adulthood. Likewise, the “normal” weight category may comprise both persons who have always enjoyed a slender physique, and those who struggled with obesity earlier in life, yet subsequently lost weight. Stigma theories suggest that the psychological consequences of a personal attribute, such as obesity, may be contingent upon when one acquired (or shed) that attribute (Goffman, 1963; Link et al., 1989). Stigmatizing treatment from significant others, especially one's family origin, may be particularly distressing when it occurs during one's childhood or adolescent years – critical stages of identity development (Puhl and Latner, 2007). Temporal comparison theory also suggests that the psychological costs (or benefits) associated with a particular attribute are contingent upon whether that attribute reflects perceived improvement or decline over time (Albert, 1977).
Thus, we examine the extent to which the effects of adult BMI on five psychological outcomes (positive and negative mood, perceived discrimination, self-acceptance, and self-satisfaction) are contingent upon one's weight during late adolescence (age 21). Adult BMI is classified according to the widely used National Heart, Lung, and Blood Institute (NHLBI, 1998) categories of underweight, normal weight, overweight, and obese. Youthful weight is classified as whether one was at a body weight deemed “at risk for overweight” by the Centers for Disease Control (CDC, 2000). Data are from the Midlife Development in the United States (MIDUS) survey, a random sample of more than 3,000 men and women ages 25 to 74 in 1995. We also analyze data from open-ended interviews with 40 currently or formerly overweight persons, to reveal the processes through which weight change may affect self-concept. Understanding the psychological consequences of body weight is an important public health goal, given that two-thirds of U.S. adults are now overweight or obese (Flegal et al., 2010).
2. Psychosocial consequences of obesity
Obesity is considered one of the most enduring social stigmas (Puhl and Heuer, 2009). Participants in experimental studies describe obese persons as less physically attractive and desirable than thinner persons, and as responsible for their weight due to a moral flaw such as laziness or gluttony (Puhl and Heur, 2009). Epidemiologic studies also document that obese persons garner lower wages and accumulate less wealth than their thinner counterparts (Han, Norton and Powell, 2011; Zagorsky, 2005). This social devaluation may trigger self-devaluation (Goffman, 1963) or “self-stigmatization” (Corrigan and Calabrese, 2005). Obese persons are more likely than their slimmer peers to report institutional and interpersonal discrimination, teasing, and strained relationships with family (Carr and Friedman, 2005, 2006).
Given the compelling evidence documenting prejudice and discrimination toward persons who are overweight or obese, one might conclude that they also experience compromised psychological well-being, including depressed mood and poor self-esteem. Reflected appraisals theory suggests that individuals will develop critical self-views if they believe others view them negatively (Cooley, 1956). However, empirical research on the psychological consequences of obesity is equivocal (Faith et al., 2004). We propose that these equivocal findings may reflect the fact that most studies do not consider an important source of heterogeneity among adults who are currently obese: some have been obese throughout their lives, whereas others became overweight or obese in adulthood after enjoying a slim physique during their formative years. Thus, we investigate the extent to which psychological consequences of adult body weight are contingent upon one's weight during one's adolescence.
Social psychological theories generate two distinctive sets of hypotheses about weight change and psychological well-being. Temporal comparison theories suggest that persons who were slender or “normal” weight as adolescents yet became overweight or obese in adulthood will fare worse than those who have been persistently overweight or obese, as the former experience a socially devalued change (Albert, 1977; Wilson and Ross, 2001). Stigma theories suggest, conversely, that the psychological costs of being overweight or obese are more severe for those who have been persistently overweight since early life (e.g., Goffman, 1963; Link et al., 1989), although some individuals may develop strategies to deflect the psychological threats of stigma (e.g., Crocker and Major, 1989; Thoits, 2011).
2.1 Temporal comparison theory
Temporal comparison theory proposes that an important source of self-evaluation is one's assessment of how one is doing in the present compared to the past (Albert, 1977). Just as individuals may compare themselves to significant others when they engage in social comparisons (Festinger, 1954), they use their earlier self as an evaluative standard when engaging in temporal comparisons. Empirical studies reveal that individuals enjoy heightened psychological well-being and self-esteem when they perceive that they have improved over time, relative to declining or remaining constant (Wilson and Ross, 2001). Given the high value placed on a slender physique in contemporary U.S. society and the well-documented difficulty of losing weight (Brownell and Rodin, 1994), weight loss may be perceived as an improvement and weight gain a decrement in one's status, competence, and social value. Thus, temporal comparison theory generates the straightforward prediction that individuals who gain weight may suffer from compromised emotional well-being, whereas those who lose weight may enjoy enhanced psychological well-being, relative to those whose weight remains stable over time.
2.1 Stigma theory
Stigma theory proposes that the psychological consequences of belonging to a socially devalued group may vary based on whether one has possessed the stigmatizing attribute throughout life (i.e., an “inborn stigma”) or whether one acquired the attribute later in life (Goffman, 1963: 34). Modified labeling theory (MLT) suggests further that persons who possess a stigmatized identity early in life may be particularly susceptible to the harmful consequences of that identity (Link, 1989). MLT proposes that people learn and internalize a set of beliefs about members of some stigmatized group. The more strongly individuals believe that they will be devalued because of their stigmatized identity, the more they will suffer psychologically and interpersonally. Those who internalize negative self-beliefs early in life are presumed to hold these views most strongly and thus experience particularly severe emotional consequences.
Consistent with stigma perspectives, some studies suggest that persons who were overweight early in life but who later lose weight do not ultimately enjoy the same body image, confidence, or social ease as persons who were thin adolescents. The “phantom fat” of formerly overweight persons continues to affect their self-image even after the weight has disappeared (Cash et al., 1990). This effect may operate directly, or indirectly, via compromised relationships with others. Overweight and obese adolescents experience more strained relationships with their parents and siblings, compared to normal weight teens (Rhee, 2008). They also are more socially isolated and have fewer friends than their slender peers (Strauss and Pollack, 2003). Early experiences of isolation and family strain among overweight young people may impede their psychosocial well-being in the longer term, even among those who eventually lose weight.
Conversely, a person who enjoyed “normal” weight early in life but who later became obese may not necessarily re-identify as a member of a stigmatized group and thus maintains a positive self-concept (Goffman, 1963: 34). Researchers have outlined strategies stigmatized individuals use to protect themselves from the self-concept threats that typically accompany their devalued social status (Crocker and Major, 1989). We propose that several of these strategies may be particularly common among persons who transition into a stigmatized group in adulthood. Some obese persons may view the negative stereotypes associated with their stigmatized identity as “not me” (Thoits, 2011). They may view their stigmatizing attribute as a “temporary” aspect of self, that can be attributed to a particular life circumstance (e.g., childbirth, stress) rather than an enduring aspect of one's identity. In sum, stigma theories suggest that the psychosocial strains associated with early life overweight may persist even in the face of adult weight loss, whereas persons who become obese in adulthood may be less susceptible to such strains.
2.3 Study aims
We know of no large scale, nationally representative studies that investigate systematically the links between weight change and psychological well-being. The large MIDUS sample enables us to address four important methodological concerns. First, we move beyond the dichotomy of “obese” versus “non-obese,” and consider the distinctive consequences of being underweight, normal weight, overweight, and two categories of obese: BMI between 30 and 35 (obese I) and 35 or higher (obese II/III). Obese individuals are a heterogeneous population, yet few studies examine whether the psychological consequences of weight vary at different points on the BMI continuum (Puhl and Brownell, 2003). Second, we examine whether the association between BMI trajectory and psychological well-being persists when demographic and socioeconomic characteristics are controlled. These characteristics may confound the relationship between BMI and well-being. Demographic characteristics such as being female, black, middle-aged, and less highly educated increase one's risk of being overweight or obese (Flegal et al., 2010). Each of these characteristics also is a significant predictor of psychological outcomes including mood (Mroczek, 2004) and perceived discrimination (Kessler et al., 1999).
Third, we assess whether the effects of body weight change on psychological well-being persist when early parent-child relationships are controlled. Family problems in early life, including parental neglect or criticism, maternal depression, and family disorganization increase the likelihood of becoming obese in childhood and in the longer term (Christoffel and Forsyth, 1989; Lissau and Sorenson, 1994). Youthful obesity, in turn, is associated with problematic interpersonal interactions (Banis et al., 1988) and behavioral problems in adolescence (Lumeng et al., 2003), and poorer socioeconomic outcomes (Viner and Cole, 2005) -- each of which gives rise to compromised psychological well-being in adulthood.
Fourth, MIDUS obtains multiple measures of psychological well-being including mood, self-acceptance, and perceived discrimination. It is important to consider multiple outcomes to fully understand how BMI shapes daily life. Some researchers have found that persons with a very high BMI may enjoy self-esteem or positive mood levels that are equal to or better than members of non-stigmatized groups because they can externalize or deflect the negative treatment by others (Crocker and Major, 1989). However, studies that focus on mood or self-evaluations only may fail to identify those outcomes for which obese persons are disadvantaged, such as interpersonal discrimination and mistreatment (Carr and Friedman, 2005).
We supplement our analysis of MIDUS data with qualitative data obtained from 40 open-ended semi-structured interviews with adults in the greater New York area who are currently or formerly overweight, and who believe that their weight history has a powerful influence on their identity. Our analysis of qualitative data provides an important first step toward understanding the ways that weight change shapes psychological well-being and self-concept.
3. Data
3.1 Quantitative data
The National Survey of Midlife Development in the United States (MIDUS) is a national multistage probability sample of noninstitutionalized English speaking adults ages 25 to 74, selected from working telephone banks in the continental United States. In the first stage, households were selected via random digit dialing. Disproportionate stratified sampling was used at the second stage to select respondents. The sample was stratified by age and gender; men and persons age 65 to 74 were oversampled. A telephone interview and mail questionnaire were administered in 1995–1996. The analyses presented here are based on the unweighted data; results were virtually identical when we adjusted for unequal probabilities of household selection and respondent selection within households.
The total MIDUS sample includes 4,242 adults (2,155 men and 2,087 women). We focus on the 3,511 persons who completed the mail questionnaire and telephone interview in 19951. The response rate for the self-administered mail questionnaire is 87 percent, thus caution should be taken in extrapolating our results to the total population (Brim et al., 2004).
3.1.1 Dependent variables
We consider five outcomes that may be affected by one's weight trajectory: positive and negative mood; perceived daily discrimination; self-acceptance, and self-satisfaction. Positive mood (α = .87) is evaluated with the question: “during the past 30 days, how much of the time did you feel: (a) cheerful; (b) in good spirits; (c) extremely happy; (d) calm and peaceful; (e) satisfied; and (f) full of life.” Negative mood (α = .87) is assessed with the question: “during the past 30 days, how much of the time did you feel: (a) so sad nothing could cheer you up; (b) nervous; (c) restless or fidgety; (d) hopeless; (e) that everything was an effort; and (f) worthless.” Response categories are none of the time, a little of the time, some of the time, most of the time, and all of the time. We constructed scale scores by averaging responses across each set of items; higher scores reflect more frequent positive or negative mood (Mroczek, 2004). Scales are standardized for ease of interpretation and comparability of coefficients.
Interpersonal discrimination (α= .98) describes recent experiences that involve character assaults and mistreatment. Respondents are asked: “How often on a day-to-day basis do you experience each of the following types of discrimination: (a) you are treated with less courtesy than other people; (b) you are treated with less respect than other people; (c) you receive poorer service than other people at restaurants or stores; (d) people act as if they think you are not smart; (e) people act as if they are afraid of you; (f) people act as if they think you are dishonest; (g) people act as if they think you are not as good as they are; (h) you are called names or insulted; and (i) you are threatened or harassed. Response categories range from 1 (“never”) to 4 (“often”). Responses are averaged. Items were developed for the MIDUS and produce more accurate estimates of perceived discrimination than single-item questions (Kessler et al., 1999).
We consider two measures of self-evaluations: self-acceptance and self-satisfaction. Self-acceptance (α=.62) is one of six dimensions of the Ryff (1989) psychological well-being scale, and is conceptually similar to widely used self-esteem scales (Rosenberg and Pearlin, 1978). Scores are based on three questions: (1) I like most parts of my personality; (2) When I look at the story of my life, I am pleased with how things have turned out so far; and (3) In many ways I feel disappointed about my achievements in life (reverse coded). Respondents indicate their level of agreement using a seven-point Likert scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”). Responses are summed and scale scores range from 3 to 21. Self-satisfaction is assessed with one item: “overall, how satisfied are you with yourself? A lot, somewhat, a little, or not at all.” Only five percent of respondents reported the latter two responses, so we constructed a dichotomous variable contrasting “a lot” with “somewhat” or less satisfied.
3.1.2. Independent variables
Adult body mass index (BMI) is the key independent variable. Respondents reported their current height and weight; BMI is calculated based on the formula where BMI equals weight in kilograms/height in meters squared. BMI scores were recoded into six categories, based on cutpoints defined by the NHLBI Guidelines (1998): underweight (BMI < 18.5), normal (BMI between 18.5 and 24.9), overweight (BMI between 25 and 29.9), obese I (BMI between 30 and 34.9), obese II (BMI between 35 and 39.9), and obese III (BMI > 40). We combine the latter two, due to the small number of cases in the Obese III category (2.6 percent of sample). Persons classified as “normal” are the reference category; the label “normal” is not a qualitative assessment, but rather, the descriptive label used by NHLBI. Self-reported weights are highly correlated with scale weights (Palta et al., 1982; Spencer et al., 2002). Very overweight persons tend to underestimate their weight, but the bias introduced is considered “inconsequential” (Palta et al., 1982: 230), especially when classifying persons into the broad NHLBI categories.
Demographic and socioeconomic status characteristics
Demographic characteristics included age (continuous measure, ranging from 25 to 74), sex (1= female; 0 = male), race (1 = Black; 0 = all other races), and marital status (categorical variables indicated persons who were never married, and formerly married. Currently married was the reference group). We use a dichotomous indicator of race, indicating African Americans versus all others because the MIDUS sample included very small numbers of Asians and Hispanics; preliminary analyses reveal that neither category differs significantly from Whites in terms of BMI.
Socioeconomic characteristics include education and employment status. Years of completed education are recoded into the categories: less than 12 years, 12 years (reference category), 13–15 years, and 16 or more years of education. Employment status is a dichotomous variable indicating that a person was employed at the time of interview.
Early life influences
We evaluate early body weight with the question “About how much did you weigh when you were 21 years old.” BMI at age 21 was recoded into a dichotomous variable indicating those who were “normal” or “underweight” versus overweight or above (reference category). We used a BMI of 25 as the cutpoint because the CDC (2000) has determined that children and adolescents with a BMI of roughly 25 are “at risk for overweight.”
To address the possibility that statistical associations among youthful body weight, adult body weight, and adult psychosocial outcomes may be a function of early family relationships, we adjust for the quality of parental relationships in early life. Early family relationships are evaluated with two separate indicators: “How would you rate your relationship with your mother (or the woman who raised you) during the years you were growing up?” and “How would you rate your relationship with your father (or the man who raised you) during the years you were growing up?” Scores range from 1 (excellent) to 5 (poor).
3.2. Qualitative data
The second author conducted 40 in-depth, face-to-face interviews. All interviews were semi-structured; however, the specific content of the interview varied based on each subject's personal experiences and history. The sample was recruited using a web posting on the New York City/New Jersey area craigslist.org that resulted in 15 interviews, and word of mouth/snowball sampling which resulted in 25 interviews. The web posting sought to recruit persons for whom being overweight or obese was an important part of their life. The query specified that the researcher was interested both in people who were currently overweight as well as those who had been overweight at one time. The sample is disproportionately Jewish (63%) and female (78%) and ranges in age from 20 to 64. The sample is disproportionately white (36 out of 40). It is also a predominantly middle to upper-middle class sample. All participants graduated from high school, and all but two also graduated from college (Jaffe, 2008).
4. Analytic Plan
4.1 Quantitative data
The quantitative analysis has four steps. First, we contrast the psychosocial, demographic, socioeconomic, and early life characteristics of persons currently classified as underweight, normal weight, overweight, obese I, obese II/III, and those who did not report their weight. Second, we evaluate the extent to which BMI category affects five psychosocial outcomes, after controlling for potential confounding factors including demographic and socioeconomic characteristics. Third, we examine the extent to which the association between BMI and psychological well-being varies on the basis of one's young adult (age 21) BMI. Finally, we evaluate whether the statistical associations among early BMI, adult BMI, and the psychosocial outcomes is confounded by early parental relationships.
4.2. Qualitative data
The second author read each interview transcript three times, and identified six themes: (a) former weight; (b) dieting; (c) moral concerns; (d) health; (e) psychological well-being; (f) aging; and (g) beauty concerns. Coding was done manually; no computer softwares were used. Several quotes fell into more than one category, and were placed in as many categories as was appropriate. Coding decisions were reviewed by the first author; none were disputed. Responses pertaining to former weight and psychological well-being provide the data for this manuscript. Respondents were classified based on their weight trajectory, and we contrast persons who were: (a) consistently overweight or obese over the life course; (b) persons who were normal weight in early life and become overweight or obese as adults; and (c) persons who were overweight or obese in early life but who lost considerable weight during adulthood.
Although these data are from a highly selective, geographically narrow sample, we believe that processes and interpretations revealed in the qualitative interviews provide a useful source for illuminating the patterns documented in the quantitative data. The striking consistency in the narratives offered by persons within each of the three weight trajectory groups suggests that similar patterns also would be evidenced in a nationally representative sample of persons who fall in each of the three categories of consistently overweight; transitioned from normal weight to overweight, and transitioned from overweight to normal weight.
5. Results
5.1 Quantitative data
5.1.1 Bivariate analysis
Table 1 presents descriptive statistics (i.e., means and proportions) for all variables included in the analysis, by BMI category. We performed a factorial ANOVA and post-hoc comparisons across the six weight categories; the right hand column denotes statistically significant contrasts between specific weight categories.
Table 1.
Means (and Standard Deviations) or Proportions, Midlife in the United States (MIDUS) 1995 (N = 3,511)
| Total Sample | Underweighta (<18.5) | Normalb (18.5 – 24.9) | Overweightc (25 – 29.9) | Obese Id (30 – 34.9) | Obese II/IIIe (35+) | Did not report weight | F-statistic (df=5) | Significant Subgroup Differences | |
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Dependent Variables Positive mood (standardized) | 0 (1.00 | −.10 (1.05) | .01 (1.01) | .03 (.97) | .03 (.98) | −.13 (1.09) | −.20 (1.0) | 2.29* | |
| Negative mood (standardized) | 0 (1.00) | .13 (.98) | .02 (.99) | −.08 (.92) | −.03 (1.0) | .22 (1.19) | .24 (1.15) | 6.04*** | be, ce, cf, de, df |
| Perceived daily discrimination (Range: 1 to 4) | 1.44 (.58) | 1.42 (.52) | 1.40 (.56) | 1.42 (.55) | 1.46 (.58) | 1.62 (.61) | 1.48 (.72) | 6.55*** | be, ce, de |
| Self-acceptance (Range: 3 to 21) | 16.48 (3.51) | 15.95 (3.02) | 16.63 (3.56) | 16.61 (3.49) | 16.42 (3.43) | 15.88 (3.61) | 15.74 (3.51) | 3.78** | be, ce |
| Self-satisfaction (1=very satisfied) | .58 | .57 | .59 | .59 | .57 | .47 | .44 | 5.15*** | be, bf, ce, cf |
| Demographic Characteristics Sex (1 = female) | .49 | .79 | .60 | .36 | .44 | .63 | .60 | 41.76*** | ab, ac, ad, bc, bd, ce, cf, de, df |
| Race (1 = black) | .06 | .03 | .04 | .06 | .08 | .12 | .08 | 5.15*** | ae, bd. be, ce, |
| Age (in years) | 46.8 (13.2) | 41.0 (13.1) | 44.73 (13.21) | 47.85 (13.4) | 49.71 (11.97) | 47.34 (11.87) | 45.22 (13.56) | 15.94*** | ac, ad, ae, bc, bf, be, df |
| Currently married | .64 | .44 | .60 | .68 | .68 | .63 | .58 | 6.78*** | ab, ac, ad, ae, bc, bd |
| Formerly married | .23 | .37 | .24 | .22 | .23 | .23 | .24 | 1.96 | ac |
| Never married | .13 | .19 | .16 | .10 | .09 | .14 | .18 | 5.49*** | bc, bd |
| Has children (1=yes) | .81 | .74 | .76 | .83 | .86 | .81 | .80 | 7.04*** | bc, bd |
| Socioeconomic Status <12 years education | .09 | .082 | .068 | .082 | .13 | .09 | .071 | 4.04* | bd, cd |
| 13–15 years education | .30 | .36 | .31 | .28 | .29 | .33 | .33 | 1.33 | |
| 16+ years education | .33 | .32 | .38 | .34 | .25 | .23 | .33 | 8.40*** | bd, be, cd, ce |
| Currently employed | .71 | .63 | .72 | .71 | .71 | .69 | .71 | .1.58 | |
| Early Life Characteristics Normal/underweight at age 21 | .79 | 1.00 | .96 | .79 | .56 | .37 | .90 | 16.5*** | ac, ad, ae, bc, bd, be, cd, ce, cf, df, ef |
| Did not report age 21 weight | .04 | 0 | .003 | .005 | .002 | .002 | .81 | 1757*** | af, bf, cf, df, ef |
| Relationship quality with mother when growing up (1=excellent; 5 = poor) | 2.19 (1.10) | 2.39 (1.19) | 2.26 (1.13) | 2.13 (1.07) | 2.12 (1.04) | 2.15 (1.19) | 2.36 (1.15) | 3.29** | bc |
| Relationship quality with mother when growing up (1=excellent; 5 = poor) | 2.57 (1.18) | 2.32 (1.19) | 2.59 (1.21) | 2.54 (1.13) | 2.57 (1.23) | 2.44 (1.23) | 2.10 (1.22) | 1.67 | |
| N | 3511 | 74 | 1177 | 1303 | 526 | 272 | 158 | ||
| % | 100 | 2.1 | 33.5 | 37.1 | 15 | 7.7 | 4.5 | ||
Notes: Asterisks denote significance level of F-statistic, where
p < .05.
p < .01.
p < .001.
Post-hoc comparisons were conducted using ANOVA; significant (p > .05) subgroup differences are denoted as ab: underweight versus normal; ac: underweight versus overweight; ad: underweight versus obese I; ae: underweight versus obese II/III; af: underweight versus weight missing; bc: normal versus overweight; bd: normal versus obese I; be: normal versus obese II/III; bf: normal versus weight missing; cd: overweight versus obese I; ce: overweight versus obese II; cf: overweight versus missing; de: obese I versus obese II/III; df: obese I versus weight missing; ef: obese II/III versus weight missing.
Roughly 37 percent of the MIDUS sample is overweight (BMI of 25 to 29.9), and an additional 23 percent are obese (BMI of 30 or higher). These proportions are comparable to national estimates for the 1990s showing that 18 to 25 percent of the U.S. population were obese, and 50–60 percent were overweight or obese (Ogden et al., 2004). The average age is 46.8 years, and men and women each account for one half of the sample. The sample is biased positively in terms of education; one third have graduated from college while an additional 30 percent has at least some college. Only six percent of the analytic sample is African American; by contrast, 12 percent of the overall U.S. population is African American (U.S. Census Bureau, 2006).
We do not find significant mean differences across the six weight categories in terms of positive mood, yet obese II/III fare significantly worse than others in terms of the four other outcomes. Persons in the obese II/III category report significantly more frequent negative mood and perceived daily discrimination than normal weight, overweight or obese I persons. They also report significantly lower levels of self-acceptance and self-satisfaction than normal weight or overweight persons, although they do not differ from obese I persons in this regard. We found no systematic relationship between body weight and early parent-child relationships.
Current body weight is strongly related to retrospective reports of weight at age 21. The proportion reporting they were normal weight in young adulthood decreases monotonically, as adult weight increases. All currently underweight persons (100 percent) and nearly all normal weight (96 percent) adults report weights that placed them in the “normal/underweight” category at age 21, while this proportion declines to 79 percent among currently overweight persons, 56 percent among obese I persons, and just 37 percent among obese II/IIII persons.
Consistent with epidemiological studies, African Americans are over-represented among persons classified as obese, especially the extremely obese; blacks account for 6 percent of the overall MIDUS sample, yet they comprise 12 percent of obese II/III respondents. Obesity and overweight risk is inversely related to socioeconomic status. The association between age and body weight is curvilinear; overweight and obese I persons are significantly older than “normal” weight persons. BMI is not associated with marital status in a systematic fashion.
5.1.2. Multivariate analysis
Next, we evaluate whether BMI is significantly related to the five psychosocial outcomes, after adjusting for demographic, family, and socioeconomic characteristics. Table 2 shows adjusted coefficients for each weight status variable; the left-hand panel displays OLS regression coefficients for continuous outcomes, and the right-hand panel displays logistic regression results (i.e., odds ratios) for the dichotomous outcome.
Table 2.
Summary of Regression Analyses Predicting Psychosocial Outcomes in the MIDUS, by Body Mass Index (N = 3,511)
| OLS Regression | Logistic Regression | ||||
|---|---|---|---|---|---|
|
| |||||
| Positive Mood (Standardized) | Negative Mood (Standardized) | Perceived Daily Discrimination | Self-Acceptance | Self-Satisfaction (1=Very Satisfied) | |
|
|
|||||
| Body Mass Index Underweight | −.036 (.12) | −.064 (.12) | −.031 (.84) | −.33 (.41) | 1.14 |
| Overweight | −.038 (.04) | −.014 (.040) | .038 (.022) | −.15 (.14) | .87 |
| Obese I | −.050 (.05) | .021 (.052) | .084** (.028) | −.26 (.18) | .79* |
| Obese II/III | −. 19** (.07) | .219*** (.066) | .183*** (.037) | −.65** (.23) | .56*** |
| Did not report weight | −22** (.08) | .15 (.083) | .039 (.046) | −.67* (.29) | .62** |
| Intercept | −.53 (.092) | .830 (.091) | 1.80 (.050) | 14.89 (.32) | 1.02 |
| Adjusted R2 | .028 | .064 | .132 | .055 | |
| Chi-squre; DF | 122.3; 14 | ||||
| N | 3501 | 3498 | 3511 | 3496 | 3511 |
Notes:
p < .05.
p < .01.
p < .001.
Unstandardized regression coefficients (and standard errors) are presented for OLS regression. Odds ratios are presented for logistic regression. All models are adjusted for sex, race, age, marital status, parental status, education, and employment status.
Extremely obese persons are disadvantaged on all five outcomes. Obese II/III persons report positive mood scores that are roughly .2 standard deviations lower, and negative mood scores that are .2 standard deviations higher than normal weight persons, as well as significantly more frequent interpersonal discrimination (b=.18, p < .001), and significantly lower levels of self-acceptance (b=−.65, p < .001). Obese II/III persons are roughly half as likely as normal weight persons to say they are “very satisfied” with themselves. Obese I persons fare worse than normal weight persons on just two dimensions; they report more frequent interpersonal discrimination (b= .084, p < .01), and are about 20 percent less likely to say they are “very satisfied” with themselves. Persons who did not report their weight have significantly lower levels of positive mood and self-acceptance, and are less likely to say they are “very satisfied” with themselves, compared to normal weight persons.
Next, we assess whether the association between adult BMI and the outcomes is contingent upon BMI at age 21. For each outcome, we evaluated a two-way interaction between each adult and age 21 BMI category. We did not evaluate a separate interaction term for persons in the “underweight” category, because 100 percent of persons in the underweight category were also “normal/underweight” at age 21. Rather, we merged the underweight and normal weight persons into a single category for this part of the analysis. A statistically significant interaction terms indicates that the impact of adult weight varies based on one's youthful weight.
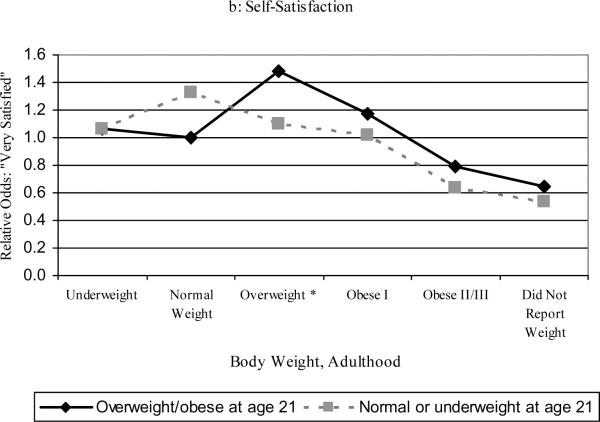
Only one of the five models yielded a statistically significant interaction term: the model for self-satisfaction. Further, the effect of only one of the BMI categories (i.e., currently overweight) is moderated by youthful body weight. Figure 2a displays odds ratios for the adult by youthful BMI categories, adjusted for demographic and socioeconomic characteristics, and Figure 2b is further adjusted for early relationships with parents. The omitted category (OR=1.0) includes persons who were normal weight both in adolescence and in adulthood.
Persons who are currently overweight and also were overweight in young adulthood have the highest odds of rating themselves as “very satisfied” with one 's self. These odds are significantly higher than for persons who are currently overweight yet were slender in adolescence (expB of 1.44 versus 1.13, respectively). Regardless of one's weight at age 21, the odds that one is “very satisfied” with oneself decline monotonically as one's weight increases beyond “overweight,” underscoring the powerful stigma of obesity. Persons who did not report their weight are about as likely as obese II/III to report being “very satisfied” with themselves.
We also explored whether these patterns would attenuate when a potential source of both self-evaluations and early weight are controlled: early parent-child relationship quality. Results are plotted in Figure 2b. The inclusion of these measures does not substantially alter the results plotted in Figure 2a. However, maternal and paternal relationships each have a significant effect on self-satisfaction; retrospective reports of problematic childhood relationships are associated with lower odds of self-satisfaction in adulthood. In sum, higher BMI is associated with a less positive self-concept, and having an adult BMI slightly above the cultural “ideal” (that is, being overweight) is more distressing for those who enjoyed a normal or slim body weight during their formative years – relative to those who have been consistently overweight.
5.2. Qualitative findings
We now compare and contrast the narratives of persons who have experienced considerable weight changes over the life course, and those who have been persistently overweight or obese. We are not evaluating hypotheses; rather, we seek to offer insights into the ways that body weight changes might affect self-concept. Consistent with the results of the quantitative analysis, we find that persons who have been above “normal” weight since their formative years accept their weight as an integral part of their identity. By contrast, those who either gained or lost considerable weight over the life course struggle with the implications of this change for their self-concept. Those who experienced substantial changes in body weight report uncertainty as to whether their self-concept should reflect the weight that they currently are, or the weight that they believe to be a reflection of who they are, where the latter typically reflected one's body weight during their formative years Nearly all persons whose weight changed dramatically recounted experiences reflecting their body weight during adolescence, and emphasized the importance of that weight to their current self-concept.
Maureen, age 40, is morbidly obese and “easily 300 pounds.” She has been overweight since childhood and says that her weight is an integral and enduring feature of her self-concept: “I'm always aware of it…it's part of my ego, if you will, of who I am because I know I'm heavy.” Maureen learned as a young teenager that she was overweight; her mother wouldn't allow her to wear a bikini because she was bigger than her best friend. As an adult, she is regularly reminded that she is obese by both family members and strangers.
By contrast, her peers who gained excessive weight in adulthood struggle with the knowledge that their current BMI places them in the category of overweight or obese. Roberta, a 60 year old college administrator who says she went from being a “stick” to a size 12, admits that she has not accepted that she is now overweight. Darlene, a 57 year old administrative assistant, reports a similar experience. She recalls that as a teenager she struggled with being underweight, especially because a curvaceous figure was in vogue at that time. However, she gained weight after her pregnancies and is now about 162 pounds and 5'2” (BMI = 30),= yet she is unable to let go of her former identity: “I still think of myself as that thin person and then you look in the mirror and you see this other person and you're like, what the heck happened?” Both Darlene and Roberta mentioned that they receive jarring reminders of their weight today, when they buy clothing or when they're weighed at a doctor's appointment.
The open-ended interviews also reveal that losing weight, like gaining weight, is often accompanied by at least some psychological distress or readjustment. Both those who lose and gain weight wrestle with whether their identity is that of a “fat” or a “thin” person. Ellen, an advertising executive in New York who dropped from 230 pounds to 110 pounds, recalled a recent clothes shopping trip. She was browsing in the women's department (the term used to describe sizes 18 plus) because that was where she “was used to shopping.” She was reminded of her recent weight loss when a saleswoman redirected her to the petite's department.
Similarly, Christopher, a 56 year old teacher and part-time actor, recounts that 15 years after he lost 63 pounds, he was surprised to realize he was no longer obese. He recalls learning he was no longer obese when a stranger in an elevator called him “skinny.”As Christopher told us: “I think most [formerly obese] people identify somehow as heavy. Like we're just here visiting in a skinny body. Most people who lose weight don't ever enjoy it because they never really think they're thin.” Christopher still worries about his weight on a daily basis. Thus, despite his drastic weight loss, he does not confidently hold a “thin” self-concept.
These persistent fears of weight gain are reasonable; empirical studies document that formerly overweight people typically regain at least part of their weight loss (Brownell and Rodin, 1994). This was the experience of Priya, a 28 year old Indian-American whose weight has fluctuated dramatically since she was a child. She is currently obese, at 5'8” and 225 pounds. Priya explains: “It's like you spend six years becoming fat …and suddenly it's gone. You don't realize it's gone until pretty much all of it's gone so here you are slim, but you don't know slim. You haven't been treated slim, you've never interacted as a slim person, you've been fat. So I didn't realize I was slim until I got fat again.” Priya has described a process reported by nearly every participant in the qualitative sample who experienced significant weight change: one's body weight can change more quickly than one's body image or self-concept. The body weight that one experienced during adolescence often makes an indelible imprint on one's self-concept, and that imprint does not easily fade even upon severe weight loss (or gain) in adulthood.
6. Discussion
Our study reveals the toll that overweight and obesity takes on psychological well-being. In our quantitative analyses, we found that obese II/III persons category fare worse than normal weight persons on each of the five psychological outcomes. Persons whose BMI is 35 or above report significantly more frequent negative mood and unkind treatment by strangers, less frequent good mood, lower levels of self-acceptance, and a lower likelihood of being “very satisfied” with one's self. The psychological toll associated with excessive weight also emerges among those who are obese I, although this subgroup fares worse than normal weight persons on just two outcomes: discrimination and self-satisfaction. One reason why obese persons may offer critical self-evaluations is that they know their weight puts them in a social category deemed unattractive and morally unacceptable by most Americans (Puhl and Heuer, 2009), thus they engage in “self-stigmatization” (Corrigan and Calabrese, 2005).
Our primary aim was to explore whether changes in one's weight between age 21 and adulthood have distinctive consequences for psychological health. Our work was motivated by two theoretical frameworks that generated competing hypotheses: temporal comparison theory suggests that weight loss would confer psychological advantages and weight gain psychological decrements (relative to stable weight), whereas stigma theories suggest a more complex set of associations. Obesity and changes in body weight may engender strategies that either heighten or minimize the effects of body weight (e.g., Crocker and Major, 1989; Thoits, 2011). Overall, our quantitative analyses provided only limited evidence that weight change effects psychological well-being, above and beyond the effect of one's current weight. The effects of adult body weight on psychosocial well-being were contingent upon early adulthood weight for just one outcome (self-satisfaction), and one weight category (overweight). Overweight adults who were also overweight in adolescence were significantly more likely than overweight adults who had been thin adolescents to say they were “very satisfied” with themselves.
These findings have several important implications. First, changes in one's weight matter psychologically only for those at the lower bounds of the high BMI spectrum (i.e., overweight). For obese persons, early adult BMI does not moderate the effects of adult BMI on self-satisfaction. Obese II/III persons fare worse than persons at all other points on the BMI spectrum, regardless of their weight in early adulthood. Morbid obesity can be considered a “master status” (Goffman, 1963): it is highly visible; “obtrusive” in that it may interfere with daily functioning (Jenkins, 2004); and elicits negative treatment from individuals and social institutions (Carr and Friedman, 2005). These chronic strains associated with extreme obesity may be sufficiently powerful to erase the self-knowledge that one was once a “thin” person. Further, the tremendous weight loss required for obese II/III persons to become “normal” weight may be so daunting that these individuals may give up on ever returning to a lower weight. Obese II/III persons may not believe that their “possible self” – or who they could become in the future – will represent an improvement over who they are today, and that pessimistic perception could be distressing (Granberg, 2006). Given the multiple stressors facing obese II/III persons, they may be less likely than their overweight or obese I peers to use strategies such as deflection to minimize the stigma associated with their weight (Crocker and Major, 1989; Thoits, 2011).
By contrast, persons who are overweight may face fewer external assaults on their physical and emotional well-being, in part because their weight is statistically normative (Flegal et al., 2010). Yet even for overweight persons, weight change may still take an emotional toll because it forces a shift in identity. As our qualitative interviews revealed, weight change – whether gain or loss – poses emotional challenges. Overweight and obese persons who were thin during adolescence had difficulty accepting their current high BMIs, and viewed their physical exterior as discrepant with the thin person they believed themselves to be. In their narratives, they consistently described what they looked like and how they felt during adolescence and early adulthood, even though they were not prompted to do so. Normal weight adults who were formerly overweight or obese say they never “learned” how to interact with their social worlds as a slim person, and thus cannot easily negotiate encounters such as being described as “skinny.” This process has been described as “identity lag,” or a cognitive obstacle whereby one's internalized identity lags behind physical change (Granberg, 2011).
Further, formerly overweight and obese persons recounted their worries that their status as a thin person is temporary. Given how easy weight gain is, most fear that it is just a matter of time before they cycle back to their former high weight. Yet most say that they still identify as “fat” regardless of how the outside world sees them. By contrast, persons who were overweight or obese continually since adolescence have a well-defined body image: women like Maureen know that they are “fat.” Although interviews with Maureen revealed that her self-concept had suffered through years of verbal slights from friends and family, her body image was unambiguous: she says her weight is “part of her ego.”
Taken together, our findings offer modest support for recent writings on temporal comparisons and self-concept. Recent studies have found that persons who denigrate their former self may enjoy self-esteem benefits because they view themselves as improving over time, as they transition from “chump” to “champ” (Wilson and Ross, 2001). Taylor and Brown (1988: 196) have suggested that people are the happiest when they believe that “the present is better than the past and that the future will be even better.” The corollary of this argument is that persons who have gotten “worse” on some criteria may be particularly self-critical, because they view themselves as being on a trajectory of decline. As our quantitative analyses and open-ended interviews reveal, persons who became overweight in adulthood were less likely to offer positive self-assessments compared to those who had always been overweight.
7. Limitations and future directions
Our study has several limitations. First, the MIDUS data are cross-sectional, so we cannot ascertain causal order. For example, we do not know whether BMI is a cause or consequence of psychological well-being; weight change may be triggered by depressive and anxiety symptoms (Anderson et al., 2006). Retrospective reports of weight also may be biased by one's current mood. Future studies could use the 1995 and 2004 waves of the MIDUS to better evaluate the possibility of an endogenous relationship between body weight and psychosocial well-being.
Second, our measure of weight trajectory does not pinpoint the precise age at which one gained or lost significant weight. Rather, we compare self-reported weight at age 21 with current weight. The long-term consequences of early-life obesity and changes in weight may be conditional on the age of onset of obesity, or the age when one's weight changed considerably. The extent to which one adopts the identity of a “fat” person may depend both on the age at which one became obese and the duration of this experience. Moreover, experiences of obesity at age 21 are more recent for younger persons and may have a more powerful impact on their psychological well-being. We implicitly address this concern by controlling age in all analyses. However, a more detailed analysis would require assessment of three-way interaction terms of current weight by youthful weight by current age. Such an analysis is precluded by sample size; we would not have adequate numbers of persons in all cells to estimate such models.
Third, we operationalized body weight using BMI only and did not capture other aspects of size or appearance that may affect psychological well-being or interpersonal interactions, such as whether one's weight reflects lean muscle versus fat. MIDUS investigators did not collect a measure of muscularity versus fat, using methods such as a skinfold caliper device or bioelectrical impedance analysis. This is potentially problematic because BMI is a weak proxy for body fat among normal and overweight people, although it is a reasonable approximation among obese persons (Romero-Corral et al., 2008).We urge researchers to consider a broader range of indicators, including waist circumference, waist-hip ratio, muscularity, and adiposity as each may reflect psychosocial outcomes in distinctive ways.
Fourth, we did not assess whether the psychological consequences of weight change were conditional upon other personal characteristics such as gender, race, or social class. The extent to which a characteristic such as obesity is devalued is contingent upon social context (Crocker and Major, 1989). Obese persons belonging to subgroups where obesity is less acceptable and normative may be particularly susceptible to self-criticism. Whites, highly educated persons, younger persons, and those with richer economic resources are more likely to value slimness and to internalize negative attitudes about obesity (Crandall and Martinez, 1996). Definitions of physical attractiveness also are tied more closely to slenderness for women (Friedman et al., 2002). In supplementary analyses, we evaluated whether the psychosocial consequences of BMI differed by gender, and found no evidence of a statistically significant moderation effect. This is surprising, given research suggesting that body weight is more salient to the self-concept of women versus men (Heo et al., 2005). We suspect that three-way interaction terms of BMI, gender and race are needed; prior work suggests that body weight has a statistically significant effect on white but not black women's psychological well-being (Scheiman, McMullen and Swan, 2007). However, sample size precludes us from conducting this fine-grained analysis.
Finally, the qualitative sample may be biased by self-selection. As a result, it is not comparable to the MIDUS along key psychological and demographic dimensions. Persons who agreed to participate in the study are those for whom body weight and changes therein are a particularly salient component of their self-concept. The sample is also heavily white, upper middle-class, female and Jewish, and all reside in the greater New York area. These subgroups may be particularly susceptible to the pressures of living up to a “thin” ideal, thus the psychological toll of obesity may be particularly acute for them. We encourage researchers to strive toward mixed-methods work where carefully chosen subsets of random-sample surveys also participate in cognitive interviewing, focus groups, or semi-structured interviews, to reveal the processes through which body weight changes affect self-concept and well-being.
Despite these limitations, our study shows that extreme obesity carries profound psychological costs, and that in some cases these costs are contingent upon one's weight trajectory. Future studies should explore further how temporal comparisons and stigmatization processes shape weight-related health behaviors. Efforts to manage one's weight through healthy diet and exercise could be shaped by one's beliefs about the duration and permanence of one's current weight. Those who view obesity as part of their “ego” may fail to engage in weight loss efforts, if they view such efforts as futile. Yet, formerly thin persons who have not accepted that they are now overweight or obese also may rebuff weight loss efforts, if they are in denial about their size. We look forward to seeing a new generation of research that conceptualizes body weight not as a personal “state,” but a “trait” that may wax and wane over the life course.
Research Highlights
Obese persons report more sadness and discrimination than normal weight persons.
Obese persons report lower self-acceptance than their thinner counterparts.
The persistently overweight have better self-esteem than those who recently became overweight.
Weight self-concept reflects both youthful weight and current weight.
Figures 1a and 1b.
Relative Odds of Reporting that One is “Very Satisfied” with One's Self, by Current BMI and BMI at Age 21 in the MIDUS
Note: Odds ratios in Figure 1a are adjusted for demographic and socioeconomic characteristics. Odds ratios in Figure 1b are also adjusted for childhood relationship characteristics. The interaction term was statistically significant for overweight persons only.
Acknowledgements
We received helpful comments from the anonymous reviewers, editors, and participants at the Obesity and Families conference held at Brigham Young University in May 2010. The MIDUS study is supported by the National Institute on Aging (P01-AG020166; Carol D. Ryff, Principal Investigator) and the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. A public use version of the Midlife Development in the United States (MIDUS) survey is available from the Inter-University Consortium for Political and Social Research (ICPSR) at the University of Michigan (www.icpsr.umich.edu).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This research was supported by a grant from the National Institute on Aging (P01-AG020166).
A second wave of MIDUS data also was collected in 2004. Despite the advantages of using the most recent wave of data, we use the earlier (1995) wave in order to: (a) minimize the duration of the recall period between the date of interview and when the respondent was age 21; and (b) to ensure that the sample includes sizeable proportions of young adults ages 25–44, a time when body weight may be particularly important to one's self concept – and prior to the onset of menopause, as well as later life health-related weight declines.
References
- Albert S. Temporal comparison theory. Psychological Review. 1977;84:485–503. [Google Scholar]
- Anderson SE, Cohen P, Naumova E, Must A. Association of depression and anxiety disorders with weight change in a prospective community based study of children followed up in adulthood. Archives of Pediatric Adolescent Medicine. 2006;160:285–291. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- Banis H, Varni J, Wallender J, Korsch B. Psychological and social adjustment of obese children and their families. Child Care Health and Development. 1988;14:157–73. doi: 10.1111/j.1365-2214.1988.tb00572.x. [DOI] [PubMed] [Google Scholar]
- Brim OG, Ryff CD, Kessler RC. The MIDUS national survey: an overview. In: Brim OG, Ryff CD, Kessler RC, editors. How healthy are we?: a national study of well-being at midlife. University of Chicago Press; Chicago: 2004. pp. 1–36. [Google Scholar]
- Brownell T, Rodin J. The dieting maelstrom: is it possible and advisable to lose weight? American Psychologist. 1994;49:781–791. doi: 10.1037//0003-066x.49.9.781. [DOI] [PubMed] [Google Scholar]
- Carr D, Friedman M. Is obesity stigmatizing? Body weight, perceived discrimination and psychological well-being in the United States. Journal of Health and Social Behavior. 2005;46:244–259. doi: 10.1177/002214650504600303. [DOI] [PubMed] [Google Scholar]
- Carr D, Friedman M. Body weight and interpersonal relationships. Social Psychology Quarterly. 2006;69:127–49. [Google Scholar]
- Carr D, Friedman MA, Jaffe K. Understanding the relationship between obesity and positive and negative affect: the role of psychosocial mechanisms. Body Image. 2007;4:165–177. doi: 10.1016/j.bodyim.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Cash TF, Counts B, Huffine CE. Current and vestigial effects of overweight among women: fear of fat, attitudinal body image, and eating behaviors. Journal of Psychopathology and Behavioral Assessment. 1990;12:157–67. [Google Scholar]
- Centers for Disease Control . CDC Growth Charts for the United States: Methods and Development. CDC; Washington, DC: 2000. (Series Report 11, No. 246). [Google Scholar]
- Christoffel KK, Forsyth BW. Mirror image of environmental deprivation: Severe childhood obesity of psychosocial origin. Child Abuse & Neglect. 1989;13:249–256. doi: 10.1016/0145-2134(89)90011-2. [DOI] [PubMed] [Google Scholar]
- Cooley CH. Human Nature and the Social Order. Free Press; New York: 1956. [Google Scholar]
- Corrigan PW, Calabrese JD. Strategies for assessing and diminishing self-stigma. In: Corrigan PW, editor. On the stigma of mental illness: Practical strategies for research and social change. American Psychological Association; Washington, DC: 2005. pp. 239–56. [Google Scholar]
- Crandall CS, Martinez R. Culture, ideology, and anti-fat attitudes. Personality and Social Psychology Bulletin. 1996;22:1165–76. [Google Scholar]
- Crocker J, Major B. Social stigma and self-esteem: the self-protective properties of stigma. Psychological Review. 1989;96:608–30. [Google Scholar]
- Faith MS, Calamaro CJ, Dolan MS, Pietrobelli A. Mood disorders and obesity. Current Opinion in Psychiatry. 2004;17:9–13. [Google Scholar]
- Faith MS, Flint J, Fairburn CG, Goodwin GM, Allison DB. Gender differences in the relationship between psychological well-being and relative body weight: results from a British population-based sample. Obesity Research. 2001;9:647–50. doi: 10.1038/oby.2001.86. [DOI] [PubMed] [Google Scholar]
- Festinger L. A theory of social comparison processes. Human Relations. 1954;7:117–140. [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin CL. Prevalence and trends in obesity among U.S. adults, 1999–2008. Journal of American Medical Association. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Friedman KE, Reichmann SK, Constanzo PR, Musante GJ. Body image partially mediates the relationship between obesity and psychological distress. Obesity Research. 2002;10:33–41. doi: 10.1038/oby.2002.5. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. Prentice-Hall; Englewood Cliffs, NJ: 1963. [Google Scholar]
- Granberg E. 'Is that all there is?' Possible selves, self-change, and weight loss. Social Psychology Quarterly 69, 109–126.Granberg, E., 2011. `Now my `old' self is thin': Stigma exits after weight loss. Social Psychology Quarterly. 2006;74:29–52. [Google Scholar]
- Han E, Norton EC, Powell LM. Direct and indirect effects of body weight on adult wages. Economics & Human Biology. 2011;9:381–392. doi: 10.1016/j.ehb.2011.07.002. [DOI] [PubMed] [Google Scholar]
- Heo M, Pietrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in U.S. adults: comparison and moderation by sex, age, and race. International Journal of Obesity. 2005;30:513–519. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- Istvan J, Zavela K, Weidner G. Body weight and psychological distress in NHANES I. International Journal of Obesity. 1992;16:999–1003. [PubMed] [Google Scholar]
- Jaffe K. Unpublished doctoral dissertation. Department of Sociology, Rutgers University; New Brunswick, NJ: 2008. Forming fat identities. [Google Scholar]
- Jenkins K. Body weight change and physical functioning among young old adults. Journal of Aging and Health. 2004;16:248–266. doi: 10.1177/0898264303262626. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Christensen H, Jacomb PA, Rodgers B, Parslow RA. Association of obesity with anxiety, depression, and emotional well-being: a community survey. Australia and New Zealand Journal of Public Health. 2003;27:434–40. doi: 10.1111/j.1467-842x.2003.tb00423.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–230. [PubMed] [Google Scholar]
- Koch D. Waaler revisited: The anthropometrics of mortality. Economics & Human Biology. 2011;9 doi: 10.1016/j.ehb.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Link BG, Streuning E, Cullen FT, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. American Sociological Review. 1989;54:400–23. [Google Scholar]
- Lissau I, Sorensen TIA. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet. 1994;343:324–27. doi: 10.1016/s0140-6736(94)91163-0. [DOI] [PubMed] [Google Scholar]
- Lumeng JC, Gannon G, Cabral H, Frank DA, Zuckerman B. Association between clinically meaningful behavior problems and overweight in children. Pediatrics. 2003;112:1138–45. doi: 10.1542/peds.112.5.1138. [DOI] [PubMed] [Google Scholar]
- Mroczek DK. Positive and negative affect at midlife. In: Brim OG, Ryff CD, Kessler RC, editors. How healthy are we?: a national study of well-being at midlife. University of Chicago Press; Chicago: 2004. pp. 205–226. [Google Scholar]
- National Heart, Lung, and Blood Institute [NHLBI] Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Author; Bethesda, MD: 1998. [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of American Medical Association. 2004;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Palta M, Prineas RJ, Berman R, Hannan P. Comparison of self-reported and measured height and weight. American Journal of Epidemiology. 1982;115:223–30. doi: 10.1093/oxfordjournals.aje.a113294. [DOI] [PubMed] [Google Scholar]
- Puhl R, Brownell KD. Ways of coping with obesity stigma: review and conceptual analysis. Eating Behaviors. 2003;4:53–78. doi: 10.1016/s1471-0153(02)00096-x. [DOI] [PubMed] [Google Scholar]
- Puhl R, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Puhl R, Latner JD. Stigma, obesity, and the health of the nation's children. Psychological Bulletin. 2007;133:557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- Rhee K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. The ANNALS of the American Academy of Political and Social Science. 2008;615:11–37. [Google Scholar]
- Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis Sert-Kuniyoshi, F.H., Lopez-Jimenez F. Accuracy of body mass index in diagnosing obesity in the adult general population. International Journal of Obesity. 2008;32:959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M, Pearlin LI. Social class and self-esteem among children and adults. American Journal of Sociology. 1978;84:53–78. [Google Scholar]
- Ryff CD. Happiness is everything, or is it? explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57:1069–1081. [Google Scholar]
- Schieman S, McMullen T, Swan M. Relative body weight and psychological distress in late life observations of gender and race comparisons. Journal of Aging and Health. 2007;19:286–312. doi: 10.1177/0898264307299300. [DOI] [PubMed] [Google Scholar]
- Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutrition. 2002;5:561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Pollack HA. Social marginalization of overweight children. Archives of Pediatrics and Adolescent Medicine. 2003;157:746–53. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- Taylor S, E., Brown JD. Illusion and well-being: a social psychological perspective on mental health. Psychological Bulletin. 1988;103:193–210. [PubMed] [Google Scholar]
- Thoits PA. Resisting the stigma of mental illness. Social Psychology Quarterly. 2011;74:6–28. [Google Scholar]
- U.S. Census Bureau . Statistical Abstract of the United States: 2006. Washington, D.C.: 2006. [Google Scholar]
- Viner RM, Cole TJ. Adult socioeconomic, educational, social and psychological outcomes of childhood obesity: a national birth cohort study. British Medical Journal. 2005;330:354. doi: 10.1136/bmj.38453.422049.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, Sarwer DB, Fabricatore AN, Crerand CE, Lipschutz PE, Faulconbridge L, Raper SE, Williams NN. Comparison of psychosocial status in treatment-seeking women with class III vs. class I–II obesity. Obesity. 2006;14(supplement):90S–98S. doi: 10.1038/oby.2006.288. [DOI] [PubMed] [Google Scholar]
- Wilson AE, Ross MR. From chump to champ: people's appraisals of their earlier and present selves. Journal of Personality and Social Psychology. 2001;80:572–584. doi: 10.1037//0022-3514.80.4.572. [DOI] [PubMed] [Google Scholar]
- Yan LL, Daviglus ML, Liu K, Stamler J, Wang R, Pirzada A, Garside DB, Dyer AR, Van Horn L, Liao Y, Fries JF, Greenland P. Midlife body mass index and hospitalization and mortality in older age. Journal of the American Medical Association. 2006;295:190–198. doi: 10.1001/jama.295.2.190. [DOI] [PubMed] [Google Scholar]
- Zagorsky J. Health and wealth: the late 20th century obesity epidemic in the U.S. Economics & Human Biology. 2005;3:296–313. doi: 10.1016/j.ehb.2005.05.003. [DOI] [PubMed] [Google Scholar]